Abstract
The Brazilian Purpuric Fever (BPF) is a systemic disease with many clinical features of meningococcal sepsis and is usually preceded by purulent conjunctivitis. The illness is caused by Haemophilus influenza biogroup aegyptius, which was associated exclusively with conjunctivitis. In this work construction of the las gene, hypothetically responsible for this virulence, were fusioned with ermAM cassette in Neisseria meningitidis virulent strains and had its DNA transfer to non BPF H. influenzae strains. The effect of the las transfer was capable to increase the cytokines TNFα and IL10 expression in Hec-1B cells line infected with these transformed mutants (in eight log scale of folding change RNA expression). This is the first molecular study involving the las transfer to search an elucidation of the pathogenic factors by horizontal intergeneric transfer from meningococci to H. influenzae.
Brazilian purpuric fever; Haemophilus influenzae biogroup aegyptius; genetic transfer; Neisseria meningitidis; Haemophilus influenzae
RESEARCH PAPER
Inflammatory response of Haemophilus influenzae biotype aegyptius causing Brazilian Purpuric Fever
Gisele Cristiane Gentile Cury; Rafaella Fabiana Carneiro Pereira; Luciana Maria de Hollanda; Marcelo Lancellotti* Correspondence : M. Lancellotti Department of Biochemistry Institute of Biology Rua Monteiro Lobato s/n Caixa Postal 6109 13083-970 State University of Campinas Campinas, SP, Brazil E-mail: mlancell@unicamp.br
Biotechnology Laboratory, Department of Biochemistry, Institute of Biology, State University of Campinas, Campinas, SP, Brazil
Correspondence Correspondence : M. Lancellotti Department of Biochemistry Institute of Biology Rua Monteiro Lobato s/n Caixa Postal 6109 13083-970 State University of Campinas Campinas, SP, Brazil E-mail: mlancell@unicamp.br
ABSTRACT
The Brazilian Purpuric Fever (BPF) is a systemic disease with many clinical features of meningococcal sepsis and is usually preceded by purulent conjunctivitis. The illness is caused by Haemophilus influenza biogroup aegyptius, which was associated exclusively with conjunctivitis. In this work construction of the las gene, hypothetically responsible for this virulence, were fusioned with ermAM cassette in Neisseria meningitidis virulent strains and had its DNA transfer to non BPF H. influenzae strains. The effect of the las transfer was capable to increase the cytokines TNFα and IL10 expression in Hec-1B cells line infected with these transformed mutants (in eight log scale of folding change RNA expression). This is the first molecular study involving the las transfer to search an elucidation of the pathogenic factors by horizontal intergeneric transfer from meningococci to H. influenzae.
Key words: Brazilian purpuric fever, Haemophilus influenzae biogroup aegyptius, genetic transfer, Neisseria meningitidis, Haemophilus influenzae.
Introduction
The Brazilian Purpuric Fever (BPF) is a fulminant pedriac disease caused by Haemophilus influenzae biogroup aegyptius (Hae). BPF was first described just over a decade ago when an outbreak emerged in several locations in the Sao Paulo State, Brazil. The illness has many clinical features of meningococcal sepsis as high fever, vomiting, abdominal pain, rapid progression of petechiae and vascular collapse. These symptons generally manifest between 7-10 days after an episode of purulent conjunctivitis (1985; 1986; 1987a; 1987b).
Major outbreaks of BPF occurred from 1984 through 1990, and sporadic cases also have been reported in Australia (McIntyre and others 1987), USA (Virata and others 1998) and recently in 2007 in Amazonas region, Brazil (Santana-Porto and others 2009). However, the disease may be more common than expected. Since the clinical picture is very similar to the meningoccocal septicemia, possible cases of BPF could be misreported. Currently, BPF is a disease requiring mandatory reporting in Brazil, because BPF agents may potentially lead to new outbreaks.
Before the emerging of BPF, Hae was a bacterium only associated with conjunctivitis, pro,ducing seasonal and epidemic infection in hot climates (Pittman and Davis 1950). Little is known of the determinants of Hae virulence or the pathogenesis of infection in BPF. Potential virulence factors such as pilus proteins and lipopolysaccharide have been investigated in the infant rat model (Rubin and St Geme 1993) and in vitro with endothelial cells (Quinn and others 1995; Weyant and others 1994), but these factors have not been consistently associated with the pathogenesis of BPF. The invasive unique phenotype in Hae makes evident that this bacterium has virulence factors absent in the rest of Haemophilus strains.
The horizontal transfer of virulence genes has a major role in the evolution of bacterial pathogens and since the natural genetic exchange between Haemophilus influenzae and Neisseria meningitidis was already described (Kroll and others 1998), the highly virulent ``meningococcal'' phenotype in Hae may be result of the genetic transfer from the meningococcus to Hae-BPF. One possible explanation for the emergence of the invasive Hae strains is an occurrence of a genetic exchange of invasiveness genes between those two bacteria. Meningococcal conserved sequences were identified in the Hae strains associated with BPF determined as NMB0419 in N. meningitidis and bfp001 in Hae (Li and others 2003).
The lav gene is another proof of the lateral transfer between Haemophilus and Neisseria. This gene is predicted to encode a virulence-associated autotransporter and to be transferred from H. influenzae to Neisseria. Through homology and base sequences analysis, it was observed that a novel type of this autotransporter had emerged in Hae, which was described as las (Davis and others 2001).
In the present work, we aimed to analyze the role of the las gene as a virulence determinant in BPF. Constructions of the las gene from Hae were transfer to non BPF H. influenzae strains and the inflammatory effects were analyzed and measured in an endothelial cellular system in vitro. This work is the first molecular study involving the las transfer to search an elucidation of the pathogenic factors by horizontal intergeneric transfer between meningococci and H. influenzae.
Material and Methods
Bacterial conditions
The Neisseria meningitidis and Haemophilus influenzae strains used in this work (Table 1) were grown in chocolate agar at 37 °C with 5% CO2. When needed, culture media were supplemented with erythromycin at 2 mg/mL for N. meningitidis receptor strains or 1 µg/mL for H. influenzae receptor strains.
DNA techniques
Recombinant DNA protocols and transformation were performed as described previously (Hollanda and others; Lancellotti and others 2008). The oligonucleotides used are listed in Table 2. All the mutants obtained by homologous recombination were verified by PCR analysis using an oligonucleotide harboring the target gene and another harboring the cassette.
Construction of fusion mutation in las::ermAM
The las gene was amplified from Hae11116 strain using the template sequence from GenBank GI: 14994100. Initially, the upstream region of the start codon was amplified using the primers lasiF and lasiR (Table 2). The downstream region to start codon of las was also amplified using lasfF and lasfR primers (Table 2). The lasi and lasf amplicons were cloned in pGEMT Easy (Promega), originating the plasmids pLAN 75 and pLAN76, respectively. Both plasmids had one BamHI site, which was necessary to future insertions. In the BamHI site of pLAN75 was inserted the ermAM cassette to generate the pLAN77. A new amplification reaction was performed using the ERAM3 and lasiF primers using pLAN77 as template. The amplicon obtained was inserted in BamHI site of pLAN76 generating the transcriptional fusion vector pLAN78. Then, this vector was transformed in N. meningitidis B4 strain, originating the LG2 strain (Figure 1).
Genetic transfer assays of las gene from N. meningitidis to H. influezae
The fusioned mutant LG2 was used as DNA donor to performed in vitro transformation of H. influenzae RdKw20 and H. influenzae βlac strains. The transformation process was performed according specifications already described (Taha and others 1998) adapted for H. influenzae using the BHI liquid medium (supplemented with haemin and NAD at 10 µg/mL). The H. influenzae strains were growth in chocolate agar and suspensions of DO 600 in supplemented BHI were made. The 5 µg of DNA from LG2 strain was added in the bacterial suspensions and then incubated at 37 °C in atmosphere of 5% of CO2 by 5 hours. The suspensions were plated in chocolate agar with erythromycin.
Hec1b cell culture and adhesion assay
Hec1B cells line were grown in plastic flasks (25 cm2) with RPMI 1640 medium (Cultilab, Campinas, SP Brazil), supplemented with 2% L-glutamine, 120 µg/mL of garamycin and 10% inactivated fetal bovine serum (complete medium). The tests for adhesion in cells followed specifications already described (Pereira RFC 2011).
Production of inflammatory cytokines by real time PCR
For those strains that promoted morphological alterations in Hec1b cells were performed analysis of the cytokines (IL10 and TNFα) production. Total RNA was extracted using the Trizol Reagent (Invitrogen, Calsbag, CA, USA). RNA yield was estimated by Nanodrop (Thermo Scientific). A minimum amount of 0.2 ng of the RNA was submitted to reverse transcription followed by qRT PCR. Real-time PCR primers are listed in Table 2 and the reaction was performed using the StepONE Plus thermocycler (Applied Biosystems). Each 10 µL reaction contained 400 nM of each primer, 5 µL Master Mix and 1/60 000 Fast EVA Green Master Mix (both from Biotium), 0.25 uL of Super Script III Platinum One-Step qRT-PCR System (Invitrogen Calsbad, CA, USA) and the recommendations for cDNA production described in the kit were followed. Reactions were repeated on three different biological replicates using as endogenous control the GAPDH gene and fold expression changes were averaged. The data was analyzed by the comparative Ct method revised in (Schmittgen and Livak 2008).
Statistical analysis
The data from each assay were statistically analyzed using Turkey's test compared with a control sample and p < 0.05 was considered significant. All experiments were performed in triplicate and the data shown in the graphs and in the table represent the means ± standard errors.
Results
For the production of the las::ermAM gene aiming the detection of the las transfer was used the template strain Hae11116 (GenBank GI: 14994100). The construction of pLAN78 and the correct insertion of each construction component were verified using ermAM's and las's primers. This construction was used in the transformation of B4 strain for the achievement of the mutant B4 LG2.
The artificial horizontal transfer from N. meningitidis to H. influenzae strains was performed using the DNA extracted from strain LG2 and the strains Rd and βlac were used as receptors, originating the mutants Rd LG2 and βlac LG2. The transference process was verified by erythromycin resistant transformants at 1g/mL. Also, analyses for las::ermAM insertion were made using the primer lasi and ERAM1 (data not shown).
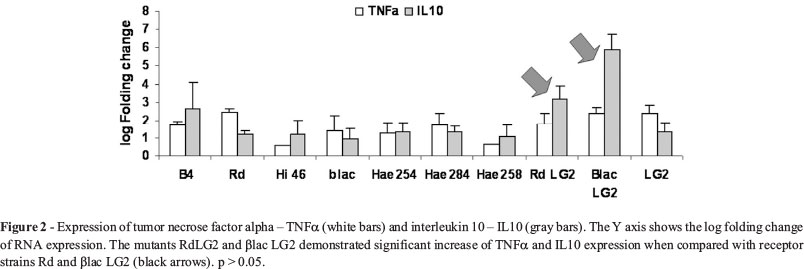
H. influenzae and N. meningitidis transformants and their wild types, three Hae-BPF strains (Hae 254/86, Hae 284/86 and Hae 258/86) and one typical H. influenzae (Hi 46) strain were analyzed in inducing expression of cytokines TNFα and IL10 in Hec-1-B cells. The in vitro assays showed that the insertion of the foreign construction in the N. meningitidis B4 donor strain did not influence the cytokines production when the B4 mutant LG2 infected Hec-1B cells. There was an increase in the expression of these inflammatory cytokines in Hec-1B cells when infected with the transformed strains βlac and Rd. Still, the levels of IL10 expression in the infection with the mutants were higher than in the presence of the Hae-BPF strains (Figure 2).
Discussion
The use of the increase of cytokines in septic shock characterization is normally done in N. meningitidis pathologies. The implication of TNFα and interleukines, such as IL10, in meningococci sepsis is well described by many authors (Bjerre and others 2004; Brandtzaeg and others 2001; Jacobs and Tabor 1990). In this work the use the Hec-1-B cells line, which had already used as model of TNFα verification in meningococcal infection (Pereira RFC 2011; Taha 2000), for the immunological analysis in the transfer process of the las gene from meningoccci strains to H. influenzae not associated with the purpura fulminans process. Nevertheless, the study of the immune response of H. influenzae biotype aegyptius causing the Brazilian purpuric fever had never been described before in vitro. The strains involved in the first BPF outbreak Hae254, Hae258 and Hae284 were able to activate the expression of IL10 and TNFα in Hec-1B cells. Though, the expression profile was lower than that observed in the transformants (Figure 2). The differential cytokines production is an important result still in study by our group. Whereas the invasive phenotype is unique in Hae strains within the Haemophilus genre, the use of a transcriptions fusion, as mimicking models of bacterial genetic transfer, is a useful and neglected tool in the search of Hae's virulence factors.
Nevertheless, the effect of the genetic transfer of the intergeneric of las gene open a new discussion about its implication in BPF physiopathology. Since the gene las was proved to have differences between lav from H. influenzae (Davis and others 2001), it is possible that this gene is associated with Hae virulence. The present work do not touch the details of the ancestrality of las gene described (Davis and others 2001), However, the role of las in the transfer of pathogenic characteristics in NTHi strains was evidenced with production of IL10 and TNFα in cells infected with the βlacLG2 and RdLG2 mutants (Figure 2).
Still, it is very important to reinforce that the gene acquisition was mediated by an environmental action. The BPF outbreak occurred in the Southest Brazilian region where the primitive agriculture was performed with a great emission of carbon dust from sugar cane burn. The atmosphere is similar to the one described to N. meningitidis using nanostructures mimicking the action of dust and particles formed by silica and carbon in atmosphere (Hollanda and others; Mattos and others). Thereby, the involvement of environment mimicked through the use of nanoparticles is one of the focus in our group research.
Recently the whole genome of Hae254/86 (also described as F3031) was sequenced and deposited in GenBank (accession no. FQ670178). The genomes of 254/86, F3047 a nontybeable H. influenzae that causes otitis and other five H. influenzae strains also non-invasive were compared. It was observed that more than 75% of the Hae 254/86 genome is similar among this H. influenzae strains (Strouts and others). The genome of the strain Hae 258/86 was sequenced as well as it's assembling and annotation is in process currently by our research group. Despite the fact that 254/86, 258/86 and all the other strains isolated from the Brazilian outbreak belong to the same clonal group (Brenner and others 1988), the strains are genetically distinct and the complete genome sequence of more than one strain of this clone will be a very helpful tool to better define the virulence determinants in the unique BPF clinical picture.
Also, new strategies to study this interesting bacterium must be considered and the search for new virulence variants. The emergence of a new outbreak in Brazil (Santana-Porto and others 2009) might be an indicative of omitted cases, reinforcing the importance of new studies about its pathogenicity and prophylaxis.
In conclusion, the las gene could be a possible predominant virulence gene involved in the pathology caused by H. influenzae biogroup aegyptius - BPF. This is the first molecular study involving the las transfer to search an elucidation of the pathogenic factors by horizontal intergeneric transfer from meningococci to H. influenzae. Also, the effect of the las transfer was capable to increase the cytokines TNFα and IL10 expression in Hec-1B cells line infected with these transformed mutants. These results reinforced the hypothesis of the real involving of las gene in H. influenzae biotype aegyptius causing the brazilian purpuric fever.
Acknowledgments
All the authors declare have no conflicts of interest in this work. This work was supported by FAPESP (number 2008/56777-5) and CNPq (number 575313/2008-0). Thanks for the English revision for Julia N. Varela.
Submitted: January 17, 2014
Approved: April 17, 2014
All the content of the journal, except where otherwise noted, is licensed under a Creative Commons License CC BY-NC.
- (1985) Preliminary report: epidemic fatal purpuric fever among children-Brazil. MMWR Morb Mortal Wkly Rep 34:217-219.
- (1986) Brazilian purpuric fever: Haemophilus aegyptius bacteremia complicating purulent conjunctivitis. MMWR Morb Mortal Wkly Rep 35:553-554.
- (1987a) Brazilian purpuric fever: epidemic purpura fulminans associated with antecedent purulent conjunctivitis. Brazilian Purpuric Fever Study Group. Lancet 2:757-761.
- (1987b) Haemophilus aegyptius bacteraemia in Brazilian purpuric fever. Brazilian Purpuric Fever Study Group. Lancet 2:761-763.
- Bjerre A, Brusletto B, Hoiby EA, Kierulf P, Brandtzaeg P (2004) Plasma interferon-gamma and interleukin-10 concentrations in systemic meningococcal disease compared with severe systemic Gram-positive septic shock. Crit Care Med 32:433-438.
- Brandtzaeg P, Bjerre A, Ovstebo R, Brusletto B, Joo GB, Kierulf P (2001) Neisseria meningitidis lipopolysaccharides in human pathology. J Endotoxin Res 7:401-420.
- Brenner DJ, Mayer LW, Carlone GM, Harrison LH, Bibb WF, Brandileone MC, Sottnek FO, Irino K, Reeves MW, Swenson JM and others (1988) Biochemical, genetic, and epidemiologic characterization of Haemophilus influenzae biogroup aegyptius (Haemophilus aegyptius) strains associated with Brazilian purpuric fever. J Clin Microbiol 26:1524-1534.
- Davis J, Smith AL, Hughes WR, Golomb M (2001) Evolution of an autotransporter: domain shuffling and lateral transfer from pathogenic Haemophilus to Neisseria J Bacteriol 183:4626-4635.
- Hollanda LM, Cury GC, Pereira RF, Ferreira GA, Sousa A, Sousa EM, Lancellotti M (2011) Effect of mesoporous silica under Neisseria meningitidis transformation process: environmental effects under meningococci transformation. J Nanobiotechnology 9:28.
- Jacobs RF, Tabor DR (1990) The immunology of sepsis and meningitis-cytokine biology. Scand J Infect Dis Suppl 73:7-15.
- Kroll JS, Wilks KE, Farrant JL, Langford PR (1998) Natural genetic exchange between Haemophilus and Neisseria: intergeneric transfer of chromosomal genes between major human pathogens. Proc Natl Acad Sci U S A 95:12381-2385.
- Lancellotti M, Pace F, Stehling EG, Villares MC, Brocchi M, Silveira WD (2008) Ribotyping, biotyping and capsular typing of Haemophilus influenzae strains isolated from patients in Campinas, southeast Brazil. Braz J Infect Dis 12:430-437.
- Li MS, Farrant JL, Langford PR, Kroll JS (2003) Identification and characterization of genomic loci unique to the Brazilian purpuric fever clonal group of H. influenzae biogroup aegyptius: functionality explored using meningococcal homology. Mol Microbiol 47:1101-1111.
- Mattos IB, Alves DA, Hollanda LM, Ceragiogli HJ, Baranauskas V, Lancellotti M Effects of multi-walled carbon nanotubes (MWCNT) under Neisseria meningitidis transformation process. J Nanobiotechnology 9:53.
- McIntyre P, Wheaton G, Erlich J, Hansman D (1987) Brasilian purpuric fever in central Australia. Lancet 2:112.
- Overbergh L, Kyama CM, Valckx D, Debrock S, Mwenda JM, Mathieu C, D'Hooghe T (2005) Validation of real-time RT-PCR assays for mRNA quantification in baboons. Cytokine 31:454-458.
- Pereira RFC AD, Jacinto RK, Hollanda LM, Verinaud LMC, Machado CML and Lancellotti M (2011) Effects of Neisseria meningitidis Infection in Tumor Glioblastoma Cell Line NG97: Respiratory Pathogen Inducing Apoptosis. J Bacteriol Parasitol 2:5.
- Pittman M, Davis DJ (1950) Identification of the Koch-Weeks bacillus (Hemophilus aegyptius). J Bacteriol 59:413-426.
- Quinn FD, Weyant RS, Worley MJ, White EH, Utt EA, Ades EA (1995) Human microvascular endothelial tissue culture cell model for studying pathogenesis of Brazilian purpuric fever. Infect Immun 63:2317-2322.
- Rubin LG, St Geme JW, 3rd (1993) Role of lipooligosaccharide in virulence of the Brazilian purpuric fever clone of Haemophilus influenzae biogroup aegyptius for infant rats. Infect Immun 61:650-655.
- Santana-Porto EA, Oliveira AA, da-Costa MR, Pinheiro A, Oliveira C, Lopes ML, Pereira LE, Sacchi C, Araujo WN, Sobel J (2009) Suspected Brazilian purpuric fever, Brazilian Amazon region. Emerg Infect Dis 15:675-676.
- Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc 3:1101-1108.
- Strouts FR, Power P, Croucher NJ, Corton N, van Tonder A, Quail MA, Langford PR, Hudson MJ, Parkhill J, Kroll JS and others Lineage-specific virulence determinants of Haemophilus influenzae biogroup aegyptius Emerg Infect Dis 18:449-457.
- Taha MK (2000) Neisseria meningitidis induces the expression of the TNF-alpha gene in endothelial cells. Cytokine 12:21-25.
- Taha MK, Morand PC, Pereira Y, Eugene E, Giorgini D, Larribe M, Nassif X (1998) Pilus-mediated adhesion of Neisseria meningitidis: the essential role of cell contact-dependent transcriptional upregulation of the PilC1 protein. Mol Microbiol 28:1153-1163.
- Virata M, Rosenstein NE, Hadler JL, Barrett NL, Tondella ML, Mayer LW, Weyant RS, Hill B, Perkins BA (1998) Suspected Brazilian purpuric fever in a toddler with overwhelming Epstein-Barr virus infection. Clin Infect Dis 27:1238-1240.
- Weyant RS, Quinn FD, Utt EA, Worley M, George VG, Candal FJ, Ades EW (1994) Human microvascular endothelial cell toxicity caused by Brazilian purpuric fever-associated strains of Haemophilus influenzae biogroup aegyptius J Infect Dis 169:430-433.
Correspondence
Publication Dates
-
Publication in this collection
13 Feb 2015 -
Date of issue
Dec 2014
History
-
Received
17 Jan 2014 -
Accepted
17 Apr 2014