Abstract
Helicobacter pylori (HP) is a vital element in the etiology of peptic ulcers and gastric cancer. This research aimed to determine the frequency, distribution, and determinants of HP infection in adults and adolescents with gastric symptoms in district Haripur, Khyber Pakhtunkhwa, Pakistan. This cross-sectional study was performed from June 2018 to June 2020 at the Medical Laboratory Technology Department, The University of Haripur, Pakistan. Presence of HP was a research variable, while sex, age groups, education status, overcrowding, dining habits, milk intake, drinking water source and animal contact were grouping variables. Immuno-chromatographic technique (ICT) was used to for serological detection of HP antibodies. All variables were represented by frequency and percentage with 95%CI. Prevalence of HP and its distribution by eight socio-demographic variables was testified by the chi-square goodness-of-fit test while association was testified by chi-square test of association. Out of total 1160 cases, 557 (48%) were positive for HP. Population prevalence was higher in men, in the age group 20-40 years, illiterate, family size ≤ 10 persons, taking restaurant food, using tetra pack, using municipal water, and having animal contact. The observed prevalence of HP was similar to its expected prevalence in the population. The observed distribution of HP in the sample was different from its expected distribution in population by eight socio-demographic variables. Presence of HP was associated with all eight socio-demographic variables besides age groups.
Keywords:
Helicobacter pylori; prevalence; hematemesis; dyspepsia; Pakistan; Haripur
Resumo
Helicobacter pylori (HP) é um elemento vital na etiologia de úlceras pépticas e câncer gástrico. Esta pesquisa teve como objetivo determinar a frequência, distribuição e determinantes da infecção por HP em adultos e adolescentes com sintomas gástricos no distrito de Haripur, Khyber Pakhtunkhwa, Paquistão. Este estudo transversal foi realizado de junho de 2018 a junho de 2020 no Departamento de Tecnologia de Laboratórios Médicos da Universidade de Haripur, Paquistão. A presença de HP foi uma variável de pesquisa, enquanto sexo, faixas etárias, escolaridade, superlotação, hábitos alimentares, ingestão de leite, fonte de água potável e contato com animais foram variáveis de agrupamento. A técnica imunocromatográfica (TIC) foi utilizada para a detecção sorológica de anticorpos para HP. Todas as variáveis foram representadas por frequência e percentual com IC 95%. A prevalência de HP e sua distribuição por oito variáveis sociodemográficas foi comprovada pelo teste de ajuste do qui-quadrado, enquanto a associação foi verificada pelo teste de associação do qui-quadrado. Do total de 1.160 casos, 557 (48%) foram positivos para HP. A prevalência populacional foi maior em homens, na faixa etária de 20 a 40 anos, analfabetos, família ≤ 10 pessoas, consumindo comida de restaurante, usando tetra pack, usando água municipal e tendo contato com animais. A prevalência observada de HP foi semelhante à sua prevalência esperada na população. A distribuição observada de HP na amostra foi diferente de sua distribuição esperada na população por oito variáveis sociodemográficas. A presença de HP foi associada a todas as oito variáveis sociodemográficas além das faixas etárias.
Palavras-chave:
Helicobacter pylori; prevalência; hematemesis; dispepsia; Paquistão; Haripur
1. Introduction
1.1 Background
Helicobacter pylori (HP) bacterium is a major cause of type B gastritis and is strongly associated with peptic and duodenal ulcers, and even stomach cancer (Smolka and Backert, 2012SMOLKA, A.J. and BACKERT, S., 2012. How Helicobacter pylori infection controls gastric acid secretion. Journal of Gastroenterology, vol. 47, no. 6, pp. 609-618. http://dx.doi.org/10.1007/s00535-012-0592-1. PMid:22565637.
http://dx.doi.org/10.1007/s00535-012-059...
). The gram-negative bacterium HP is formerly known as Campylobacter pylori, predominantly colonizing the stomach’s linings (Salih, 2009SALIH, B.A., 2009. Helicobacter pylori infection in developing countries: the burden for how long? Saudi Journal of Gastroenterology, vol. 15, no. 3, pp. 201-207. http://dx.doi.org/10.4103/1319-3767.54743. PMid:19636185.
http://dx.doi.org/10.4103/1319-3767.5474...
; Coelho and Coelho, 2021COELHO, L.G.V. and COELHO, M.C.F., 2021. Helicobacter pylori and colorectal neoplasms: a concise review. Arquivos de Gastroenterologia, vol. 58, no. 1, pp. 114-119. http://dx.doi.org/10.1590/s0004-2803.202100000-19. PMid:33909789.
http://dx.doi.org/10.1590/s0004-2803.202...
). HP has affected about half of the world’s population (Torres et al., 2000TORRES, J., PÉREZ-PÉREZ, G., GOODMAN, K.J., ATHERTON, J.C., GOLD, B.D., HARRIS, P.R., GARZA, A.M., GUARNER, J. and MUÑOZ, O., 2000. A comprehensive review of the natural history of Helicobacter pylori infection in children. Archives of Medical Research, vol. 31, no. 5, pp. 431-469. http://dx.doi.org/10.1016/S0188-4409(00)00099-0. PMid:11179581.
http://dx.doi.org/10.1016/S0188-4409(00)...
; Coelho et al., 2021COELHO, M.C.F., RIBEIRO, H.G., GOMES, C.G.D.O., MARINHO, F.P., BARBOSA, A.J. and COELHO, L.G.V., 2021. Helicobacter pylori chronic gastritis on patients with premalignant conditions: OLGA and OLGIM evaluation and serum biomarkers performance. Arquivos de Gastroenterologia, vol. 58, no. 1, pp. 39-47. http://dx.doi.org/10.1590/s0004-2803.202100000-08. PMid:33909795.
http://dx.doi.org/10.1590/s0004-2803.202...
). The prevalence of HP infection shows variations with socioeconomic status as in developed countries, it is low like Australia 23%, Germany 39% and England 41%, in contrast to less developed countries, like Pakistan 92%, Bangladesh 90%, India 79% and Nepal 57% (Muhammad et al., 2012MUHAMMAD, J.S., ZAIDI, S.F. and SUGIYAMA, T., 2012. Epidemiological ins and outs of helicobacter pylori: a review. Journal of the Pakistan Medical Association, vol. 62, no. 9, pp. 955-959. PMid:23139983.).
HP has a narrow host range more or less solely in humans and some non-human primates. Despite several studies on the risk factors for acquiring HP infection, the exact mechanisms whereby this bacterium is acquired remained mostly unknown (Hanafiah et al., 2020HANAFIAH, A., RAZAK, S.A., NEOH, H.-M., ZIN, N.M. and LOPES, B.S., 2020. The heterogeneic distribution of Helicobacter pylori cag pathogenicity island reflects different pathologies in multiracial Malaysian population. The Brazilian Journal of Infectious Diseases, vol. 24, no. 6, pp. 545-551. http://dx.doi.org/10.1016/j.bjid.2020.10.005. PMid:33157035.
http://dx.doi.org/10.1016/j.bjid.2020.10...
). The frequent routes of transmission are oral-oral, gastro-oral, fecal-oral, iatrogenic and intra-familial (Eslick et al., 1999ESLICK, G.D., LIM, L.L.-Y., BYLES, J.E., XIA, H.H.-X. and TALLEY, N.J., 1999. Association of Helicobacter pylori infection with gastric carcinoma: a meta-analysis. American Journal of Gastroenterology, vol. 94, no. 9, pp. 2373-2379. http://dx.doi.org/10.1111/j.1572-0241.1999.01360.x. PMid:10483994.
http://dx.doi.org/10.1111/j.1572-0241.19...
; Hedayati et al., 2021HEDAYATI, M.A., AHMADI, S., SERVATYARI, K. and SHEIKHESMAEILI, F., 2021. PREX2 gene’s expression in gastric antral epithelial cells of patients with H. pylori infection. Arquivos de Gastroenterologia, vol. 58, no. 3, pp. 353-358. http://dx.doi.org/10.1590/s0004-2803.202100000-59. PMid:34705970.
http://dx.doi.org/10.1590/s0004-2803.202...
; Bastán et al., 2021BASTÁN, J.E.P., PONCE, R.H. and HERNÁNDEZ, B.R., 2021. Caracterización clínico epidemiológica de la infección por Helicobacter pylori en pacientes con úlcera péptica. Revista Cubana de Medicina General Integral, vol. 37, no. 1, p. e1288.).
Despite high virulence, pathogenicity, and prevalence, in most individuals, HP infection remains asymptomatic. Simultaneously, few develop symptoms in later stages (Ahmad et al., 2003AHMAD, A., GOVIL, Y. and FRANK, B.B., 2003. Gastric mucosa-associated lymphoid tissue lymphoma. American Journal of Gastroenterology, vol. 98, no. 5, pp. 975-986. http://dx.doi.org/10.1111/j.1572-0241.2003.07424.x. PMid:12809817.
http://dx.doi.org/10.1111/j.1572-0241.20...
) like dyspepsia, epigastric pain, belching, and heartburn, while untreated patients may lead to type B gastritis, peptic or duodenal ulcer, and even stomach cancer (Chang and Parsonnet, 2010CHANG, A.H. and PARSONNET, J., 2010. Role of bacteria in oncogenesis. Clinical Microbiology Reviews, vol. 23, no. 4, pp. 837-857. http://dx.doi.org/10.1128/CMR.00012-10. PMid:20930075.
http://dx.doi.org/10.1128/CMR.00012-10...
).
There is a need for epidemiological studies that are primarily designed to estimate the different risk factors contributing to HP infection progression in our population. Doing so will help the healthcare professionals understand the disease burden in our population and facilitate the policymakers to consider health issues due to HP during policy formulation and budgetary allocation. Therefore, this study was designed to determine the frequency, distribution, and determinants of HP infection in adults and adolescents with gastric symptoms.
1.2. Research problems & knowledge gaps
Epidemiological inquiry gives us the overall and group-wise burden of a disease or a health-related event so that resources may be allocated accordingly to manage it. It further gives us the causes/ determinants of the disease, so that preventive measures may be recommended to control it in a specified population.
For our population, we are unaware of the frequency of HP infection, its distribution by eight socio-demographic factors, and its association to eight factors; this unawareness of 17 pieces of information are our 17 research problem. There is a paucity of relevant research documents available for our population, so these 17 are our knowledge gaps. These 17 research problems are expanded as 17 research questions (RQs), 17 research objectives (ROs), and 17 research hypotheses (RHs) as follows.
1.3. Research questions
We have tried to answer the following research questions in three groups.
RQ 1: What is the prevalence of HP infection in adults and adolescents with gastric symptoms in district Haripur, Pakistan? (H01)
RQs 2-9: What is the distribution of HP infection by eight socio-demographic factors in adults and adolescents with gastric symptoms in district Haripur, Pakistan? (H02-H09)
RQs 10-17: Is there association between the presence of HP infection and eight socio-demographic factors in adults and adolescents with gastric symptoms in district Haripur, Pakistan? (H010-H017)
1.4. Research Objectives (ROs)
We had the following objectives in three groups.
RO 1: To determine the prevalence of HP infection in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (H01)
ROs 2-9: To determine the distribution of HP infection by eight socio-demographic factors in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (H02-H09)
ROs 10-17: To determine the association between the presence of HP infection and eight socio-demographic factors in adults and adolescents with gastric symptoms in district Haripur, Pakistan? (H010-H017)
1.5. Research (null) hypotheses
H01: The observed prevalence of HP infection is same as expected in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 1, RO 1)
H02: The observed distribution of HP infection is same as expected by sex in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 2, RO 2)
H03: The observed distribution of HP infection is same as expected by age groups in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 3, RO 3)
H04: The observed distribution of HP infection is same as expected by the education status in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 4, RO 4)
H05: The observed distribution of HP infection is same as expected by overcrowding in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 5, RO 5)
H06: The observed distribution of HP infection is same as expected by the dining habits in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 6, RO 6)
H07: The observed distribution of HP infection is same as expected by the milk consumption in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 7, RO 7)
H08: The observed distribution of HP infection is same as expected by the source of drinking water in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 8, RO 8)
H09: The observed distribution of HP infection is same as expected by animal contact in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 9, RO 9)
H010: The presence of HP infection is associated with sex in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 10, RO 10)
H011: The presence of HP infection is associated with age groups in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 11, RO 11)
H012: The presence of HP infection is associated with education status in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 12, RO 12)
H013: The presence of HP infection is associated with overcrowding in the population of adults and adolescents with gastric symptoms (RQ 13, RO 13)
H014: The presence of HP infection is associated with dining habits in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 14, RO 14)
H015: The presence of HP infection is associated with milk consumption in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 15, RO 15)
H016: The presence of HP infection is associated with the source of drinking water in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 16, RO 16)
H017: The presence of HP infection is associated with animal contact in adults and adolescents with gastric symptoms in district Haripur, Pakistan. (RQ 17, RO 17)
1.6. Significance and applicability
HP is a significant public health problem associated with peptic ulcer disease and gastric carcinoma and has a high global prevalence. By having identified the associated exposures as socio-demographic variables, we will recommend the strategy for its prevention and control at personal and community levels.
1.7. Operational definitions
Adult as defined by WHO: An adult is older than 19 years of age unless national law defines a person as an adult at an earlier age. Besides, as defined by WHO, adolescents are aged 10 to 19 years inclusive (WHO, 2013WORLD HEALTH ORGANIZATION – WHO, 2013 [viewed 20 October 2020]. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach [online]. WHO. Available from: https://www.who.int/publications/i/item/9789241505727.
https://www.who.int/publications/i/item/...
).
2. Material and Methods
2.1. Study design, settings & duration and ethical approval & consent
This cross-sectional study was carried out at the Department of Medical Laboratory Technology, The University of Haripur, Haripur, Pakistan, from June 2018 to June 2020. The data was collected from the Gastroenterology Outdoor Patient Department of District Headquarter Hospital, Haripur, Pakistan. Ethical approval was granted by the Departmental Bioethical Committee of The University of Haripur. Consent from the management of District Headquarter Hospital, Haripur, was taken to collect data. The consent of the patients/ guardians was taken before inclusion in the study.
2.2. Population, sample size, sampling technique & sample selection
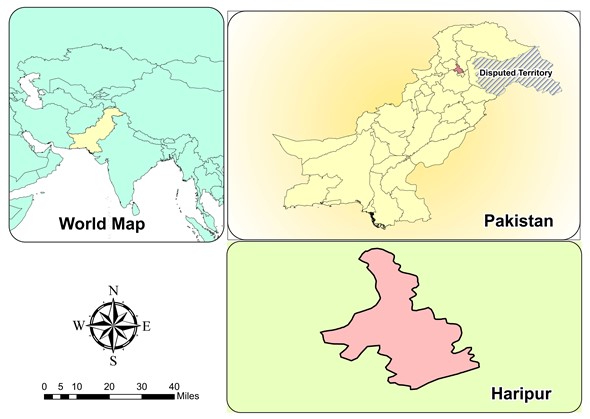
Living in the catchment area of District Headquarter Hospital, Haripur, a population of 50,000 adults and adolescents with gastric symptoms was considered to be at risk for HP infection, as shown in Figure 1.The sample size was calculated to be 1160 by online sample size calculator Raosoft® with a margin of error of 3.739%, confidence level of 99%, the population size of 50,000, and response distribution of 50% (Raosoft, 2004RAOSOFT, 2004 [viewed 20 October 2020]. Sample size calculator [online]. RAOSOFT. Available from: http://www.raosoft.com/samplesize.html
http://www.raosoft.com/samplesize.html...
). The sampling technique was consecutive non-probability. The inclusion criteria were the adults and adolescents presenting with the gastric symptoms, including hematemesis, dyspepsia, heartburn, vomiting, poor appetite, and irregular defecation frequency. The only exclusion criterion was refusal for inclusion.
2.3. Equipment and procedure of conduct
We conducted ICT as follows according to the producer’s instructions (CTK Biotech, 2020CTK BIOTECH, 2020 [viewed 13 November 2021]. H. pylori Ab combo rapid test CE [online]. CTK Biotech. Available from: https://ctkbiotech.com/product/h-pylori-ab-combo-rapid-test-ce/.
https://ctkbiotech.com/product/h-pylori-...
). About 03 ml of blood samples were collected in aseptic gel-vacutainers. In case of any delayed testing (up to 05 days), specimens were stored at 2-8◦C. Subsequently, serum was extracted by centrifugation at 3500 rpm for 05 minutes. HP antibodies were detected in serum by using pre-coated antigen strips (HP Ab Combo Rapid Test CE, CTK, Biotech Inc., Poway, CA, USA) based on double antigen lateral flow assay chromatographic technique. Around 35µl serum and 35µl commercially available sample diluent available with the kit were added together to avoid any air bubbles formed during the assay. The results were read after 15 minutes. The formation of the color band against the test area was considered positive. In contrast, no color band at the test area was considered a negative result.
2.4. Data collection plan
Data were collected for one research variable; the presence of HP (yes & no) and eight socio-demographic variables/ factors with attributes in brackets; sex (men & women), age groups (10-19, 20-40, 41-60 & 60+ years), education status (illiterate, primary, secondary & higher education), overcrowding (family members≤10 & family members>10), dining habits (restaurant & home-made), milk consumption (tetra pack & fresh milk), source of drinking water (municipal, streams/lakes & boring water), animal contact (yes & no). All variables were on a nominal scale except age groups and education status on the ordinal scale. For eight tests of association, presence of HP was a single dependent variable, while each of the eight socio-demographic variables was an independent variable.
2.5. Data analysis plan
2.5.1. Descriptive statistics & estimation of parameters
All the nine variables were described by frequency (count) and percentage for the sample and as confidence interval for proportion at 95% confidence level (CL) for the population using an online calculator “Statistics Kingdom” (https://www.statskingdom.com/proportion-confidence-interval-calculator.html).
2.5.2. Hypotheses testing
Here, we have used two types of statistical tests. One is the chi-square goodness-of-fit test, and the other is the chi-square test of association (Pagano and Gauvreau, 2018PAGANO, M. and GAUVREAU, K., 2018. Principles of biostatistics. New York: CRC Press.; Daniel and Cross, 2018DANIEL, W.W. and CROSS, C.L., 2018. Biostatistics: a foundation for analysis in the health sciences. Hoboken: John Wiley & Sons.; Zar, 1999ZAR, J.H., 1999. Biostatistical analysis. Hoboken: Prentice Hall.). Chi-square goodness-of-fit test is a univariate/ single variable test, which is used to testify H01 to H09, giving the significance of the difference between the observed (sample) and expected (population) prevalence/ distribution for different attributes of the same variable. Chi-square test of association is a bivariate test used to testify H10 to H017 to show an association between the two variables; here, presence of HP is a dependent variable, and each one of the eight socio-demographic variables is an independent variable. All these 17 tests are conducted at alpha 0.5 through an online statistical calculator (Social Science StatisticsSOCIAL SCIENCE STATISTICS, 2014 [viewed 13 November 2021]. Statistics Calculators [online]. Available from: https://www.socscistatistics.com/tests/.
https://www.socscistatistics.com/tests/...
). Observed and expected frequencies, their differences, chi-square statistic, degree of freedom, and level of significance are given for each.
3. Results
3.1. Descriptive statistics & estimation of parameters
3.1.1. Prevalence of HP in population (RQ 1, RO 1)
Out of the 1160 patients, 557 (48%) were positive for HP infection. Table 1 gives frequency and percentage of HP positive cases in the sample with their estimated prevalence in the population of 45.12%-50.88% at 95%CL and likewise for HP negative cases.
Frequency of HP in sample and population in adults and adolescents with gastric symptoms (RQ 1, RO 1) (n=1160).
3.1.2. Distribution of HP positive cases in population (RQs 2-9, ROs 2-9)
Here 557/1160 (48%) HP positive cases were distributed by eight socio-demographic variables with their estimated prevalence in the population at 95%CL in Table 2.
Distribution of HP positive cases by eight socio-demographic variables in adults and adolescents with gastric symptoms (n=557/1160, RQs 2-9, ROs 2-9).
3.2. Hypotheses testing
3.2.1. Observed versus expected prevalence of HP in population (RQ 1, RO 1, H01)
Here the observed prevalence of HP was compared to 50% expected prevalence in population through chi-square goodness-of-fit test at alpha 0.05, as in Table 3. H01 was accepted, showing that the observed prevalence of HP was similar to its expected prevalence in the population.
Comparison of frequency of HP between the sample and population in adults and adolescents with gastric symptoms (RQ1, RO1, H01, n=557/1160).
3.2.2. Observed versus expected distribution of HP positive cases by eight factors (RQs 2-9, ROs 2-9, H02-H09)
Here observed distribution of HP positive cases in sample was compared to the equal expected distribution in population by eight socio-demographic variables separately through chi-square goodness-of-fit test at alpha 0.05, as in Table 4. All hypotheses (H02-H09) were rejected, showing that the observed distribution of HP in sample was different from its expected distribution in population by eight socio-demographic variables.
Distribution of HP positive cases in sample versus equal expected distribution in population by eight socio-demographic variables in adults and adolescents with gastric symptoms (RQs 2-9, ROs 2-9, H02-H09, n=557).
3.3. Association of presence of HP and eight socio-demographic variables (RQs 10-17, ROs 10-17, H010-H017)
Seven out of eight hypotheses were rejected, showing an association between the presence of HP infection and seven socio-demographic variables, i.e., sex, education status, overcrowding, dining habits, milk consumption, and source of drinking water and animal contact. H011 was accepted, showing no association between the presence of HP infection and age groups, as given in Table 5.
Association of HP and eight socio-demographic variables in population in adults and adolescents with gastric symptoms (RQs 10-17, ROs 10-17, H010-H017, n=1160).
4. Discussion
4.1. Limitations & delimitations (weaknesses)
Our study was not community-based. It was a hospital-based one, including only adults and adolescents with gastric symptoms. So, it is not representative of the general community/ individuals without gastric symptoms.
4.2. Strengths of the study
4.2.1. Prevalence of HP in population
Pakistan is currently facing severe financial constraints and overburdened healthcare sector to cater massive influx of patients (Haqqi et al., 2021HAQQI, A., AWAN, U.A., ALI, M., SAQIB, M.A.N., AHMED, H. and AFZAL, M.S., 2021. COVID‐19 and dengue virus co‐epidemics in Pakistan: a dangerous combination for overburdened healthcare system. Journal of Medical Virology, vol. 93, no. 1, pp. 80-82. http://dx.doi.org/10.1002/jmv.26144. PMid:32510175.
http://dx.doi.org/10.1002/jmv.26144...
; Awan et al., 2021cAWAN, U.A., ZAHOOR, S., AYUB, A., AHMED, H., AFTAB, N. and AFZAL, M.S., 2021c. COVID‐19 and arboviral diseases: another challenge for Pakistan’s dilapidated healthcare system. Journal of Medical Virology, vol. 93, no. 7, pp. 4065-4067. http://dx.doi.org/10.1002/jmv.26668. PMid:33200437.
http://dx.doi.org/10.1002/jmv.26668...
; Qasim et al., 2020QASIM, M., AWAN, U.A., AFZAL, M.S., SAQIB, M.A.N., SIDDIQUI, S. and AHMED, H., 2020. Dataset of knowledge, attitude, practices and psychological implications of healthcare workers in Pakistan during COVID-19 pandemic. Data in Brief, vol. 32, p. 106234. http://dx.doi.org/10.1016/j.dib.2020.106234. PMid:32895632.
http://dx.doi.org/10.1016/j.dib.2020.106...
; Awan et al., 2021bAWAN, U.A., KHATTAK, A.A., AFZAL, M.S., KHAN, H.I., SAQIB, M.A.N. and AHMED, H., 2021b. COVID-19 and tuberculosis overlapping epidemics: a holistic review from Pakistan. Journal of Medical Virology, vol. 93, no. 5, pp. 2573-2575. http://dx.doi.org/10.1002/jmv.26714. PMid:33295641.
http://dx.doi.org/10.1002/jmv.26714...
; Awan et al., 2021aAWAN, U.A., KHATTAK, A.A., AFZAL, M.S., IQBAL, N. and NADEEM, M.F., 2021a. Emergence of SARS‐CoV‐2 variant: a wake‐up call for Pakistan’s overburdened healthcare system. Journal of Medical Virology, vol. 93, no. 5, pp. 2595-2598. http://dx.doi.org/10.1002/jmv.26825. PMid:33506951.
http://dx.doi.org/10.1002/jmv.26825...
; Alvi et al., 2021ALVI, M.Z.-U.-D., SATTAR, M., CHEEMA, F.A., AWAN, U.A., AFTAB, M.N., SHAH, Z.H. and AFZAL, M.S., 2021. COVID-19 and emergence of antimicrobial resistance: a most neglected aspect of health emergency in Pakistan. Diabetes & Metabolic Syndrome, vol. 15, no. 4, p. 102179. http://dx.doi.org/10.1016/j.dsx.2021.06.016. PMid:34186352.). Firstly, epidemiological research measures the prevalence of a disease in a specified population by selecting a representative sample from it, collecting and analyzing data for the sample, describing the sample using descriptive statistics, and infer these to describe the population through estimation of parameters (inferential statistics). Then sample statistics are compared to the population parameters to see if the frequency of the disease in the sample is similar to its prevalence in the population or otherwise through hypothesis testing (inferential statistics)? In our study, we have given frequency and percentage of HP positive cases in sample and confidence intervals (CI) for proportion for population and compared the frequency of HP positive cases in the samples versus population through hypothesis testing.
4.2.2. Observed versus expected distribution of HP in population
Secondly, epidemiological research measures prevalence of a disease in a specified population by socio-demographic variables/ attributes/ factors/ groups called the distribution of the disease. We have given distribution of HP in the sample as frequency and percentage, then in population as CI and then compared the distribution of HP positive cases in the sample (observed) versus population (expected) through hypothesis testing, all for eight socio-demographic groups. Very few studies have given CI for their populations. However, no study has compared the distribution of HP positive cases by socio-demographic groups in the sample versus population through hypothesis testing. This hypothesis testing would be an innovative addition to the global literature by us.
However, for the distribution of HP by socio-demographic variables/ groups/ factors, almost all studies have wrongly calculated percentages/ prevalence. For example, analysis of hypothetical data is here; a sample size of 400 persons, including 250 men and 150 women, have HP infection positive in 260 cases, so the overall frequency of positive cases will be 260 & overall percentage (prevalence) of positive cases will be 65% (260*100/400=65%). Whereas the frequency for negative cases will be 140 (400-260), and the percentage will be 35% (140*100/400=35%).
Now we come to the distribution of HP positive cases by sex. If out of 260 positive cases, there were 160 men and 100 women, then the ‘correct’ percentage (prevalence) will be 40% (160*100/400=40%) for men and 25% (100*100/400=25%) for women, the total frequency of positive cases to be 260/400 (65%). Nevertheless, almost all studies cited here have calculated HP positive percentage for 160 men out of a total of 250 men (and not out of total 400 cases) to be 64% and for 100 women out of a total of 150 women (and not out of total 400 cases) to be 66.66%, total 64+66.66=130.66%, which is impossible.
The paragraph above shows the distribution of HP positive cases by sex ‘only descriptively’ by frequency and percentage. This descriptive statistic is not valid to conclude that the prevalence of HP positive cases is higher in men than women or vice versa. For comparison, one has to use inferential statistics/ hypothesis testing. One has to put a hypothesis, use a test of significance of difference, and then develop the decision. Even then, there is no statistical test available to testify the frequency/ proportion/ prevalence/ distribution of HP positive cases or any other disease/ event in men versus women, i.e., by sex or by any other socio-demographic variable/ group/ factor. The test available is the chi-square goodness-of-fit test (Sharma et al., 1997SHARMA, T.K., YOUNG, E.L., MILLER, S. and CUTLER, A.F., 1997. Evaluation of a rapid, new method for detecting serum IgG antibodies to Helicobacter pylori. Clinical Chemistry, vol. 43, no. 5, pp. 832-836. http://dx.doi.org/10.1093/clinchem/43.5.832. PMid:9166238.
http://dx.doi.org/10.1093/clinchem/43.5....
; Rahman et al., 2008RAHMAN, S.H.Z., AZAM, M.G., RAHMAN, M.A., ARFIN, M.S., ALAM, M.M., BHUIYAN, T.M., AHMED, N., RAHMAN, M., NAHAR, S. and HASSAN, M.S., 2008. Non-invasive diagnosis of H pylori infection: evaluation of serological tests with and without current infection marker CIM. World Journal of Gastroenterology, vol. 14, no. 8, pp. 1231-1236. http://dx.doi.org/10.3748/wjg.14.1231. PMid:18300349.
http://dx.doi.org/10.3748/wjg.14.1231...
; Raj et al., 2017RAJ, P., THOMPSON, J.F. and PAN, D.H., 2017. Helicobacter pylori serology testing is a useful diagnostic screening tool for symptomatic inner city children. Acta Paediatrica, vol. 106, no. 3, pp. 470-477. http://dx.doi.org/10.1111/apa.13724. PMid:28024098.
http://dx.doi.org/10.1111/apa.13724...
), which compares the ‘observed frequencies’ (counts) of HP positive cases for men and women in ‘sample’ to the ‘expected frequencies’ of HP positive cases for men and women in ‘population’. The expected frequencies may be taken from literature or hypothetical from the researcher’s background knowledge regarding the specified population. No such hypothesis testing is there in any study cited here for HP positive cases. Even the global literature we have come across to distribute other diseases/ events is not based on such inferential analysis. So, this effort on our part will be an innovative addition to the global literature. We in our study have given observed frequencies, expected frequencies, their differences, square of their differences, chi-square values, all for each cell separately, degrees of freedom and p values for all the eight chi-square goodness-of-fit tests separately, which are valid, reliable, verifiable, repeatable and replicable.
The comparison to the cited studies for the distribution of HP positive cases would have been based on our study’s hypothesis results versus cited studies. However, the cited studies have no hypothesis tested for it, so we have compared percentages to percentages in the discussion.
4.2.3. Determinants of disease (association between variables)
Any finding/ decision/ conclusion given in a study should be valid, reliable, verifiable, repeatable, and replicable. Most of the studies have given only a p-value for the chi-square test of association. It is neither verifiable nor repeatable. We in our study have given observed frequencies, expected frequencies, their differences, square of their differences, chi-square values, all for each cell separately, degrees of freedom and p values for all the eight chi-square tests of association (Sharma et al., 1997SHARMA, T.K., YOUNG, E.L., MILLER, S. and CUTLER, A.F., 1997. Evaluation of a rapid, new method for detecting serum IgG antibodies to Helicobacter pylori. Clinical Chemistry, vol. 43, no. 5, pp. 832-836. http://dx.doi.org/10.1093/clinchem/43.5.832. PMid:9166238.
http://dx.doi.org/10.1093/clinchem/43.5....
; Rahman et al., 2008RAHMAN, S.H.Z., AZAM, M.G., RAHMAN, M.A., ARFIN, M.S., ALAM, M.M., BHUIYAN, T.M., AHMED, N., RAHMAN, M., NAHAR, S. and HASSAN, M.S., 2008. Non-invasive diagnosis of H pylori infection: evaluation of serological tests with and without current infection marker CIM. World Journal of Gastroenterology, vol. 14, no. 8, pp. 1231-1236. http://dx.doi.org/10.3748/wjg.14.1231. PMid:18300349.
http://dx.doi.org/10.3748/wjg.14.1231...
; Raj et al., 2017RAJ, P., THOMPSON, J.F. and PAN, D.H., 2017. Helicobacter pylori serology testing is a useful diagnostic screening tool for symptomatic inner city children. Acta Paediatrica, vol. 106, no. 3, pp. 470-477. http://dx.doi.org/10.1111/apa.13724. PMid:28024098.
http://dx.doi.org/10.1111/apa.13724...
; Nadeem et al., 2023NADEEM, M.F., KHATTAK, A.A., ZEESHAN, N., AWAN, U.A., ALAM, S., AHMED, W., GUL, S., AFROZ, A., SUGHRA, K., RASHID, U. and KHAN, M.A.U., 2023. Molecular epidemiology of Plasmodium species in conflicted Federally Administered Tribal Area (FATA) Pakistan. Brazilian Journal of Biology = Revista Brasileira de Biologia, vol. 83, p. e247219. http://dx.doi.org/10.1590/1519-6984.247219. PMid:34468526.
http://dx.doi.org/10.1590/1519-6984.2472...
) separately, which are valid, reliable, verifiable, repeatable and replicable and of course an innovative addition to the global literature. At times, authors have given decisions/ conclusions based on percentages; which are not valid. In such cases, we have applied the chi-square test of association for the cited studies from the available observed frequencies, and results for cited studies are shown in the discussion as chi-square/ Yate’s chi-square, degrees of freedom (d.f.), and p values for comparison.
4.2.4. Marwat’s Logical Trajectory of Research Process
Here in this project, we have followed the “Marwat’s Logical Trajectory of Research Process in Medical Sciences”, developed by Dr. Muhammad Marwat, our co-author. It is an eight-step innovative logical/ intellectual activity, including putting in order the research problems, knowledge gaps, research questions, research objectives, research hypotheses, data collection, data analysis, and data interpretation. Earlier, two research articles are published using this trajectory, available at https://www.gjms.com.pk/index.php/journal/article/view/751/747 and https://www.gjms.com.pk/index.php/journal/article/view/766/762
4.3. Interpretations & comparisons
Interpretations & comparisons are placed under three main headings following the aims of the current study; prevalence of HP infection, distribution of HP infection by eight socio-demographic variables and determinants of HP infection (association to eight socio-demographic variables) in our population and 17 subheadings as per our 17 hypotheses, comparing our findings to local, national, regional and global literature.
4.3.1. Prevalence of HP in population (RQ 1, RO 1, H01)
The prevalence of HP infection in our sample was 48%, and for our population, it was 45.12%-51.88% at 95% CL. Similar prevalence was given by Rasheed et al. from Islamabad, collecting asymptomatic cases of all ages from all over Pakistan, for 2002-2015, as 49.54% (1147/2315) (Rasheed et al., 2017RASHEED, F., YAMEEN, A., AHMAD, T. and BILAL, R., 2017. Rate of active Helicobacter pylori infection among symptomatic patients of Pakistan. The Malaysian Journal of Pathology, vol. 39, no. 1, pp. 69-72. PMid:28413207.). Similarly, Rastogi et al. (2015)RASTOGI, M., RASTOGI, D., SINGH, S., AGARWAL, A., PRIYADARSHI, B. and MIDDHA, T., 2015. Prevalence of Helicobacter pylori in asymptomatic adult patients in a tertiary care hospital: a cross sectional study. Biomedical Research, vol. 26, no. 1, pp. 117-122. from Kanpur, India in 2012-13 in asymptomatic adult individuals as 44.23% (92/208) and a global systematic review and meta-analysis by Hooi et al. (2017)HOOI, J.K., LAI, W.Y., NG, W.K., SUEN, M.M., UNDERWOOD, F.E., TANYINGOH, D., MALFERTHEINER, P., GRAHAM, D.Y., WONG, V.W., WU, J.C., CHAN, F.K.L., SUNG, J.J.Y., KAPLAN, G.G. and NG, S.C., 2017. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology, vol. 153, no. 2, pp. 420-429. http://dx.doi.org/10.1053/j.gastro.2017.04.022. PMid:28456631.
http://dx.doi.org/10.1053/j.gastro.2017....
including 184 studies from 62 countries for the duration 1970-2016 showing global prevalence as 48.46% (257,768/ 531,880).
Lower prevalence was noted by Khoder et al. (2019)KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044. PMid:30939800.
http://dx.doi.org/10.3390/pathogens80200...
from UAE in 2017-18 as 41.42% (145/350) in healthy asymptomatic individuals and a population-based cross-sectional study by Shu et al. (2019)SHU, L., ZHENG, P.-F., ZHANG, X.-Y. and FENG, Y.-L., 2019. Dietary patterns and Helicobacter pylori infection in a group of Chinese adults ages between 45 and 59 years old: an observational study. Medicine, vol. 98, no. 2, p. e14113. http://dx.doi.org/10.1097/MD.0000000000014113. PMid:30633225.
http://dx.doi.org/10.1097/MD.00000000000...
from Hangzhou city, Zhejiang province, China, including 3014 healthy 45-59 years adults in 2015-16, as 27.50% (829/3014).
Higher prevalence was reported by Rasheed et al. (2012)RASHEED, F., AHMAD, T. and BILAL, R., 2012. Prevalence and risk factors of Helicobacter pylori infection among Pakistani population. Pakistan Journal of Medical Sciences, vol. 28, no. 4, pp. 661-665. from Islamabad, Pakistan in 2008-2009 involving asymptomatic persons 2-70 years old as 74.4% (384/516), by Singh et al. (2002)SINGH, V., TRIKHA, B., NAIN, C.K., SINGH, K. and VAIPHEI, K., 2002. Epidemiology of Helicobacter pylori and peptic ulcer in India. Journal of Gastroenterology and Hepatology, vol. 17, no. 6, pp. 659-665. http://dx.doi.org/10.1046/j.1440-1746.2002.02746.x. PMid:12100610.
http://dx.doi.org/10.1046/j.1440-1746.20...
from Chandigarh, India in symptomatic cases as 61.25% (49/80), a meta-analysis by Moosazadeh et al. (2016)MOOSAZADEH, M., LANKARANI, K.B. and AFSHARI, M., 2016. Meta-analysis of the prevalence of Helicobacter pylori infection among children and adults of Iran. International Journal of Preventive Medicine, vol. 7, no. 1, p. 48. http://dx.doi.org/10.4103/2008-7802.177893. PMid:27076886.
http://dx.doi.org/10.4103/2008-7802.1778...
from Iran, including 21 articles (n=15,680) as 54.0% (95% CI: 53-55%) and by Assaad et al. (2018)ASSAAD, S., CHAABAN, R., TANNOUS, F. and COSTANIAN, C., 2018. Dietary habits and Helicobacter pylori infection: a cross sectional study at a Lebanese hospital. BMC Gastroenterology, vol. 18, no. 1, p. 48. http://dx.doi.org/10.1186/s12876-018-0775-1. PMid:29661143.
http://dx.doi.org/10.1186/s12876-018-077...
from Lebanon in 2016 including adults as 52.04% (n=153/294).
4.3.2. Distribution of HP positive cases by eight socio-demographic variables (RQs 2-9 & ROs 2-9, H02-H09)
4.3.2.1. (H02)
Regarding sex, the prevalence of HP in our population was higher for men 30.68% (95%CI 28.04-33.34%) than women 17.32% (95%CI 15.15-19.51%).
Similar to our study, a higher prevalence for men 28.42% (658/2315) than women 21.12% (489/2315) was noted by Rasheed et al. (2017)RASHEED, F., YAMEEN, A., AHMAD, T. and BILAL, R., 2017. Rate of active Helicobacter pylori infection among symptomatic patients of Pakistan. The Malaysian Journal of Pathology, vol. 39, no. 1, pp. 69-72. PMid:28413207. for the years 2002-2015 from Islamabad, by Rastogi et al. (2015)RASTOGI, M., RASTOGI, D., SINGH, S., AGARWAL, A., PRIYADARSHI, B. and MIDDHA, T., 2015. Prevalence of Helicobacter pylori in asymptomatic adult patients in a tertiary care hospital: a cross sectional study. Biomedical Research, vol. 26, no. 1, pp. 117-122. from Kanpur, India, men 29.32% (61/208) versus women 14.90% (31/208), by Khoder et al. (2019)KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044. PMid:30939800.
http://dx.doi.org/10.3390/pathogens80200...
from UAE, men 21.71% (76/350) versus women 19.71% (69/350) and by Shu et al. (2019)SHU, L., ZHENG, P.-F., ZHANG, X.-Y. and FENG, Y.-L., 2019. Dietary patterns and Helicobacter pylori infection in a group of Chinese adults ages between 45 and 59 years old: an observational study. Medicine, vol. 98, no. 2, p. e14113. http://dx.doi.org/10.1097/MD.0000000000014113. PMid:30633225.
http://dx.doi.org/10.1097/MD.00000000000...
from China, men 16.25% (490/3014) versus women 11.25% (339/3014).
Higher prevalence for women 31.63% (93/294) versus men 20.41% (60/294) was found by Assaad et al. (2018)ASSAAD, S., CHAABAN, R., TANNOUS, F. and COSTANIAN, C., 2018. Dietary habits and Helicobacter pylori infection: a cross sectional study at a Lebanese hospital. BMC Gastroenterology, vol. 18, no. 1, p. 48. http://dx.doi.org/10.1186/s12876-018-0775-1. PMid:29661143.
http://dx.doi.org/10.1186/s12876-018-077...
from Lebanon, by Zhu et al. (2014)ZHU, Y., ZHOU, X., WU, J., SU, J. and ZHANG, G., 2014. Risk factors and prevalence of Helicobacter pylori infection in persistent high incidence area of gastric carcinoma in Yangzhong city. Gastroenterology Research and Practice, vol. 2014, p. 481365. http://dx.doi.org/10.1155/2014/481365. PMid:24550981.
http://dx.doi.org/10.1155/2014/481365...
for the duration 2009-2011 from Yangzhong city, China women 36.70% (1446/5417) versus men 26.70% (1989/5417).
4.3.2.2. (H03)
Regarding age groups, the prevalence of HP in our sample and population was highest for the age group 21-40 years 18.7% (95%CL 16.47%-20.95%) and lowest for the age group 60+ years 4.82% (95%CL 3.6%-6.06%). Rasheed et al. (2017)RASHEED, F., YAMEEN, A., AHMAD, T. and BILAL, R., 2017. Rate of active Helicobacter pylori infection among symptomatic patients of Pakistan. The Malaysian Journal of Pathology, vol. 39, no. 1, pp. 69-72. PMid:28413207. for the years 2002-2015 from Islamabad showed the highest prevalence for age group 19-44 years 27.95% (647/2315), similar to our study, and lowest for age group 3-18 years 5.18% (120/2315), Rastogi et al. (2015)RASTOGI, M., RASTOGI, D., SINGH, S., AGARWAL, A., PRIYADARSHI, B. and MIDDHA, T., 2015. Prevalence of Helicobacter pylori in asymptomatic adult patients in a tertiary care hospital: a cross sectional study. Biomedical Research, vol. 26, no. 1, pp. 117-122. from Kanpur, India showed the highest prevalence for age group 19-39 years 31.73% (66/208) and lowest for the age group 60+ years 1.92% (4/208), both similar to our study. Here two groups of 19-29 and 30-39 years of cited study were merged to one group of 19-39 years for comparison to our group of 20-40 years and two groups of 60-69 and ≥70 years for comparison to our one group of 60+ years.
Zhu et al. (2014)ZHU, Y., ZHOU, X., WU, J., SU, J. and ZHANG, G., 2014. Risk factors and prevalence of Helicobacter pylori infection in persistent high incidence area of gastric carcinoma in Yangzhong city. Gastroenterology Research and Practice, vol. 2014, p. 481365. http://dx.doi.org/10.1155/2014/481365. PMid:24550981.
http://dx.doi.org/10.1155/2014/481365...
from Yang Zhong, China showed the highest prevalence for age group 40-59 years 53.20% (2882/5417) and lowest for the age group 30-39 years 4.94% (267/5417), both different from our study. Here two groups of cited study 40-49 and 50-59 years were merged into one group of 40-59 years for comparison to our group of 41-60 years.
4.3.2.3. (H04)
Regarding education status, the prevalence of HP in our sample and population was highest in the illiterate group 16.29% (95%CL 14.16%-18.42%) and lowest in the higher education group as 8.19% (95%CI 6.61-9.77%). Zhu et al. (2014)ZHU, Y., ZHOU, X., WU, J., SU, J. and ZHANG, G., 2014. Risk factors and prevalence of Helicobacter pylori infection in persistent high incidence area of gastric carcinoma in Yangzhong city. Gastroenterology Research and Practice, vol. 2014, p. 481365. http://dx.doi.org/10.1155/2014/481365. PMid:24550981.
http://dx.doi.org/10.1155/2014/481365...
from China showed the highest prevalence in primary as 33.67% (1824/5417) and the lowest in the illiterate group as 1.64% (89/5417), both different from our study. Ozaydin et al. from Turkey showed the highest prevalence in primary 39.35% (1801/4577) and lowest in the secondary group 7.76% (335/5417), both different from our study (Ozaydin et al., 2013OZAYDIN, N., TURKYILMAZ, S.A. and CALI, S., 2013. Prevalence and risk factors of helicobacter pylori in Turkey: a nationally-representative, cross-sectional, screening with the 13 C-Urea breath test. BMC Public Health, vol. 13, no. 1, p. 1215. http://dx.doi.org/10.1186/1471-2458-13-1215. PMid:24359515.
http://dx.doi.org/10.1186/1471-2458-13-1...
). Shu et al. from China showed the highest prevalence for secondary school of 17.19% (518/3014) and lowest for secondary school of 02.98% (90/3014) (Shu et al., 2019SHU, L., ZHENG, P.-F., ZHANG, X.-Y. and FENG, Y.-L., 2019. Dietary patterns and Helicobacter pylori infection in a group of Chinese adults ages between 45 and 59 years old: an observational study. Medicine, vol. 98, no. 2, p. e14113. http://dx.doi.org/10.1097/MD.0000000000014113. PMid:30633225.
http://dx.doi.org/10.1097/MD.00000000000...
). As the cited study had three groups, so illiterate and primary groups of our study were merged into one group (189+162=351, 30.25%) compared to the secondary school group of the cited study. Hence our study will show the highest prevalence for secondary school group 30.25%, while the cited study shows the highest prevalence for secondary school of 17.19%.
4.3.2.4. (H05)
Regarding overcrowding, the prevalence of HP in our sample and population was higher in smaller family size ≤10 group 26.9% (95% CL 24.35-29.45%) than larger family size >10 21.1% (95%CI 18.75-23.45%). Similar reports are by Khoder et al. (2019)KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044. PMid:30939800.
http://dx.doi.org/10.3390/pathogens80200...
from UAE with smaller family size (≤6 persons/house) 28.0% (98/350) versus larger family size (≥7 persons/house) 13.42% (47/350), by Zhu et al. from China, smaller family size (≤ 6) 71.67% (3382/5417) versus larger family size (≥7) as 0.98% (53/5417) (Zhu et al., 2014ZHU, Y., ZHOU, X., WU, J., SU, J. and ZHANG, G., 2014. Risk factors and prevalence of Helicobacter pylori infection in persistent high incidence area of gastric carcinoma in Yangzhong city. Gastroenterology Research and Practice, vol. 2014, p. 481365. http://dx.doi.org/10.1155/2014/481365. PMid:24550981.
http://dx.doi.org/10.1155/2014/481365...
). The family size of this cited study of 1, 2, 3, 4, 5 & 6 was merged into one group of ≤6 compared to our group of ≤10.
Opposite reported was by Rasheed et al. (2012)RASHEED, F., AHMAD, T. and BILAL, R., 2012. Prevalence and risk factors of Helicobacter pylori infection among Pakistani population. Pakistan Journal of Medical Sciences, vol. 28, no. 4, pp. 661-665. from Islamabad, Pakistan, in 2008-2009, showing a higher prevalence in a larger family size of ≥7 41.67% (215/516) versus the smaller family size of ≤6 as 32.75% (169/516).
4.3.2.5. (H06)
Regarding dining habits, the prevalence of HP in our sample and population was higher in the restaurant group 28.35% (95%CL 25.74-30.94%) than the home-made group 19.65% (95%CL 17.36-21.94%). Mhaskar et al. from Pune, Maharashtra State, India, during January 2008 and November 2010, including 350 symptomatic cases, showed higher prevalence for home-made group 28.28% (99/350) than restaurant group 26% (91/350), opposite to our findings (Mhaskar et al., 2013MHASKAR, R.S., RICARDO, I., AZLIYATI, A., LAXMINARAYAN, R., AMOL, B., SANTOSH, W. and BOO, K., 2013. Assessment of risk factors of Helicobacter pylori infection and peptic ulcer disease. Journal of Global Infectious Diseases, vol. 5, no. 2, pp. 60-67. http://dx.doi.org/10.4103/0974-777X.112288. PMid:23853433.
http://dx.doi.org/10.4103/0974-777X.1122...
). The frequency of outside food consumption from the cited study had four attributes of 1/week, 2/week, 3/week, and seldom. The first three attributes/groups were merged to compare to our restaurant group while rarely compared to our home-made group.
4.3.2.6. (H07)
Regarding milk consumption, the prevalence of HP in our sample and population was higher in tetra pack milk group 35.1% (95%CL 32.35%-37.85%) than fresh milk group 12.9% (95%CL 10.97-14.83%). No relevant studies were available to compare the internet in local, national, regional, and global literature.
4.3.2.7. (H08)
Regarding the source of drinking water, the prevalence of HP in our sample and population was highest in the municipal water group 24.9% (25%CL 22.41-27.39%) and lowest in boring water 8.2% (95%CL 6.62-9.78%). Rasheed et al. (2012)RASHEED, F., AHMAD, T. and BILAL, R., 2012. Prevalence and risk factors of Helicobacter pylori infection among Pakistani population. Pakistan Journal of Medical Sciences, vol. 28, no. 4, pp. 661-665. from Islamabad showed the highest prevalence of HP in well water (synonymous to our streams/lakes group) as 38.95% (201/516) and lowest for city water (synonymous to our municipal group) 14.92% (77/516), both different from our study.
4.3.2.8. (H09)
Regarding animal contact, the prevalence of HP in our sample and population was higher in the contact yes group 26.37% (95%CL 23.83-28.91%) than contact no group 21.63% (95%CL 19.26-24.0%). Similar reports are by Rasheed et al. (2012)RASHEED, F., AHMAD, T. and BILAL, R., 2012. Prevalence and risk factors of Helicobacter pylori infection among Pakistani population. Pakistan Journal of Medical Sciences, vol. 28, no. 4, pp. 661-665. from Islamabad in 2008-2009 with animal contact yes group 39.15% (202/516) versus no animal contact group 35.27% (182/516), by Khoder et al. (2019)KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044. PMid:30939800.
http://dx.doi.org/10.3390/pathogens80200...
from UAE with animal contact yes group as 35.42% (124/350) versus no animal contact group of 6% (21/350), by Elhariri et al. from Cairo with dogs contact yes group 27.78% (61/90) versus no dogs contact group 16.66% (29/90) (Elhariri et al., 2017ELHARIRI, M., ELHELW, R., HAMZA, D. and EL-MAHALLAWY, H.S., 2017. Serologic evidence and risk factors for Helicobacter pylori infection in animals and humans. Journal of Infection in Developing Countries, vol. 11, no. 5, pp. 414-419. http://dx.doi.org/10.3855/jidc.9339. PMid:30943179.
http://dx.doi.org/10.3855/jidc.9339...
).
4.3.3. Association of presence of HP and eight socio-demographic variables (RQs 10-17, ROs 10-17, H010-H017)
4.3.3.1. (H010)
The presence of HP infection was associated with sex in our population. A similar association was found by Khoder et al. (2019)KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044. PMid:30939800.
http://dx.doi.org/10.3390/pathogens80200...
from UAE (p=0.0014) and by Zhu et al. (2014)ZHU, Y., ZHOU, X., WU, J., SU, J. and ZHANG, G., 2014. Risk factors and prevalence of Helicobacter pylori infection in persistent high incidence area of gastric carcinoma in Yangzhong city. Gastroenterology Research and Practice, vol. 2014, p. 481365. http://dx.doi.org/10.1155/2014/481365. PMid:24550981.
http://dx.doi.org/10.1155/2014/481365...
from China (Yate’s χ2 value=4.9556, d.f. =1, p=0.0260 at alpha 0.05).
No association was reported by Rasheed et al. (2017)RASHEED, F., YAMEEN, A., AHMAD, T. and BILAL, R., 2017. Rate of active Helicobacter pylori infection among symptomatic patients of Pakistan. The Malaysian Journal of Pathology, vol. 39, no. 1, pp. 69-72. PMid:28413207. for the years 2002-2015 from Islamabad (p=0.124), by Rasheed et al. (2012)RASHEED, F., AHMAD, T. and BILAL, R., 2012. Prevalence and risk factors of Helicobacter pylori infection among Pakistani population. Pakistan Journal of Medical Sciences, vol. 28, no. 4, pp. 661-665. from Islamabad, Pakistan in 2008-2009 (p=0.622), by Santos et al. (2005)SANTOS, I.S., BOCCIO, J., SANTOS, A.S., VALLE, N.C.J., HALAL, C.S., BACHILLI, M.C. and LOPES, R.D., 2005. Prevalence of Helicobacter pylori infection and associated factors among adults in southern Brazil: a population-based cross-sectional study. BMC Public Health, vol. 5, no. 1, p. 118. http://dx.doi.org/10.1186/1471-2458-5-118. PMid:16283940.
http://dx.doi.org/10.1186/1471-2458-5-11...
from Brazil (n=363) (Yate’s χ2 value=2.5884, d.f.=1, p=0.1076), by Mabeku et al. (2018)MABEKU, L.B.K., NGAMGA, M.L.N. and LEUNDJI, H., 2018. Potential risk factors and prevalence of Helicobacter pylori infection among adult patients with dyspepsia symptoms in Cameroon. BMC Infectious Diseases, vol. 18, no. 1, p. 278. http://dx.doi.org/10.1186/s12879-018-3146-1. PMid:29907086.
http://dx.doi.org/10.1186/s12879-018-314...
from Cameroon (n=205) (Yate’s χ2 value=0.6953, d.f.=1, p=0.4043), by Mungazi et al. (2018)MUNGAZI, S.G., CHIHAKA, O.B. and MUGUTI, G.I., 2018. Prevalence of Helicobacter pylori in asymptomatic patients at surgical outpatient department: harare hospitals. Annals of Medicine and Surgery, vol. 35, pp. 153-157. http://dx.doi.org/10.1016/j.amsu.2018.09.040. PMid:30302246.
http://dx.doi.org/10.1016/j.amsu.2018.09...
from Harare, Zimbabwe (n=300) (p=0.076), by Assaad et al. (2018)ASSAAD, S., CHAABAN, R., TANNOUS, F. and COSTANIAN, C., 2018. Dietary habits and Helicobacter pylori infection: a cross sectional study at a Lebanese hospital. BMC Gastroenterology, vol. 18, no. 1, p. 48. http://dx.doi.org/10.1186/s12876-018-0775-1. PMid:29661143.
http://dx.doi.org/10.1186/s12876-018-077...
from Lebanon in 2016 (p=0.358), and by Shu et al. (2019)SHU, L., ZHENG, P.-F., ZHANG, X.-Y. and FENG, Y.-L., 2019. Dietary patterns and Helicobacter pylori infection in a group of Chinese adults ages between 45 and 59 years old: an observational study. Medicine, vol. 98, no. 2, p. e14113. http://dx.doi.org/10.1097/MD.0000000000014113. PMid:30633225.
http://dx.doi.org/10.1097/MD.00000000000...
from China (Yate’s χ2 value=12.5921, d.f.=1, p=0.000387 at alpha 0.05).
4.3.3.2. (H011)
There was no association between HP infection and age groups in our population. Similar finding was by Mabeku et al. (2018)MABEKU, L.B.K., NGAMGA, M.L.N. and LEUNDJI, H., 2018. Potential risk factors and prevalence of Helicobacter pylori infection among adult patients with dyspepsia symptoms in Cameroon. BMC Infectious Diseases, vol. 18, no. 1, p. 278. http://dx.doi.org/10.1186/s12879-018-3146-1. PMid:29907086.
http://dx.doi.org/10.1186/s12879-018-314...
from Cameroon (χ2 value=4.057, d.f.=3, p=0.398).
Many reports showed association like Rasheed et al. (2017)RASHEED, F., YAMEEN, A., AHMAD, T. and BILAL, R., 2017. Rate of active Helicobacter pylori infection among symptomatic patients of Pakistan. The Malaysian Journal of Pathology, vol. 39, no. 1, pp. 69-72. PMid:28413207. for the years 2002-2015 from Islamabad (p <0.5), Rasheed et al. (2012)RASHEED, F., AHMAD, T. and BILAL, R., 2012. Prevalence and risk factors of Helicobacter pylori infection among Pakistani population. Pakistan Journal of Medical Sciences, vol. 28, no. 4, pp. 661-665. from Islamabad in 2008-2009 (p=0.003), Khoder et al. (2019)KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044. PMid:30939800.
http://dx.doi.org/10.3390/pathogens80200...
from UAE (p=0.032), Zhu et al. (2014)ZHU, Y., ZHOU, X., WU, J., SU, J. and ZHANG, G., 2014. Risk factors and prevalence of Helicobacter pylori infection in persistent high incidence area of gastric carcinoma in Yangzhong city. Gastroenterology Research and Practice, vol. 2014, p. 481365. http://dx.doi.org/10.1155/2014/481365. PMid:24550981.
http://dx.doi.org/10.1155/2014/481365...
for the duration 2009-2011 from China (χ2 value=118.46, d.f.=3, p <0.00001 at alpha 0.05), Santos et al. (2005)SANTOS, I.S., BOCCIO, J., SANTOS, A.S., VALLE, N.C.J., HALAL, C.S., BACHILLI, M.C. and LOPES, R.D., 2005. Prevalence of Helicobacter pylori infection and associated factors among adults in southern Brazil: a population-based cross-sectional study. BMC Public Health, vol. 5, no. 1, p. 118. http://dx.doi.org/10.1186/1471-2458-5-118. PMid:16283940.
http://dx.doi.org/10.1186/1471-2458-5-11...
from Brazil (χ2 value=14.06, d.f.=3, p=0.0028) and Mungazi et al. (2018)MUNGAZI, S.G., CHIHAKA, O.B. and MUGUTI, G.I., 2018. Prevalence of Helicobacter pylori in asymptomatic patients at surgical outpatient department: harare hospitals. Annals of Medicine and Surgery, vol. 35, pp. 153-157. http://dx.doi.org/10.1016/j.amsu.2018.09.040. PMid:30302246.
http://dx.doi.org/10.1016/j.amsu.2018.09...
from Harare, Zimbabwe (p=0.012).
4.3.3.3. (H012)
There was association between the presence of HP infection and education status. Similar report was by Santos et al. (2005)SANTOS, I.S., BOCCIO, J., SANTOS, A.S., VALLE, N.C.J., HALAL, C.S., BACHILLI, M.C. and LOPES, R.D., 2005. Prevalence of Helicobacter pylori infection and associated factors among adults in southern Brazil: a population-based cross-sectional study. BMC Public Health, vol. 5, no. 1, p. 118. http://dx.doi.org/10.1186/1471-2458-5-118. PMid:16283940.
http://dx.doi.org/10.1186/1471-2458-5-11...
from Brazil (χ2 value=14.5184, d.f.=3, p=0.0022). Many reports of no association were from Rasheed et al. (Khoder et al., 2019KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044. PMid:30939800.
http://dx.doi.org/10.3390/pathogens80200...
) from Islamabad, Pakistan in 2008-2009 (p=0.720), Zhu et al. (2014)ZHU, Y., ZHOU, X., WU, J., SU, J. and ZHANG, G., 2014. Risk factors and prevalence of Helicobacter pylori infection in persistent high incidence area of gastric carcinoma in Yangzhong city. Gastroenterology Research and Practice, vol. 2014, p. 481365. http://dx.doi.org/10.1155/2014/481365. PMid:24550981.
http://dx.doi.org/10.1155/2014/481365...
from China (χ2 value=3.6003, d.f.=3, p=0.3079 at alpha 0.05) and Mungazi et al. (2018)MUNGAZI, S.G., CHIHAKA, O.B. and MUGUTI, G.I., 2018. Prevalence of Helicobacter pylori in asymptomatic patients at surgical outpatient department: harare hospitals. Annals of Medicine and Surgery, vol. 35, pp. 153-157. http://dx.doi.org/10.1016/j.amsu.2018.09.040. PMid:30302246.
http://dx.doi.org/10.1016/j.amsu.2018.09...
from Harare, Zimbabwe (p=0.105).
4.3.3.4. (H013)
There was association between the presence of HP infection and overcrowding. Similar reports are from Rasheed et al. (2012)RASHEED, F., AHMAD, T. and BILAL, R., 2012. Prevalence and risk factors of Helicobacter pylori infection among Pakistani population. Pakistan Journal of Medical Sciences, vol. 28, no. 4, pp. 661-665. from Islamabad in 2008-2009 (p=0.025) and Santos et al. (2005)SANTOS, I.S., BOCCIO, J., SANTOS, A.S., VALLE, N.C.J., HALAL, C.S., BACHILLI, M.C. and LOPES, R.D., 2005. Prevalence of Helicobacter pylori infection and associated factors among adults in southern Brazil: a population-based cross-sectional study. BMC Public Health, vol. 5, no. 1, p. 118. http://dx.doi.org/10.1186/1471-2458-5-118. PMid:16283940.
http://dx.doi.org/10.1186/1471-2458-5-11...
from Brazil (Yate’s χ2 value=4.8974, d.f.=1, p=0.0268).
Reports of no association were from Khoder et al. (2019)KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044. PMid:30939800.
http://dx.doi.org/10.3390/pathogens80200...
from UAE (p=0.676), Zhu et al. (2014)ZHU, Y., ZHOU, X., WU, J., SU, J. and ZHANG, G., 2014. Risk factors and prevalence of Helicobacter pylori infection in persistent high incidence area of gastric carcinoma in Yangzhong city. Gastroenterology Research and Practice, vol. 2014, p. 481365. http://dx.doi.org/10.1155/2014/481365. PMid:24550981.
http://dx.doi.org/10.1155/2014/481365...
from China (Yate’s χ2 value=0.0072, d.f.=1, p=0.9325 at alpha 0.05), Mabeku et al. (2018)MABEKU, L.B.K., NGAMGA, M.L.N. and LEUNDJI, H., 2018. Potential risk factors and prevalence of Helicobacter pylori infection among adult patients with dyspepsia symptoms in Cameroon. BMC Infectious Diseases, vol. 18, no. 1, p. 278. http://dx.doi.org/10.1186/s12879-018-3146-1. PMid:29907086.
http://dx.doi.org/10.1186/s12879-018-314...
from Cameroon (Yate’s χ2 value=2.6, d.f.=1, p=0.1068), and Mungazi et al. (2018)MUNGAZI, S.G., CHIHAKA, O.B. and MUGUTI, G.I., 2018. Prevalence of Helicobacter pylori in asymptomatic patients at surgical outpatient department: harare hospitals. Annals of Medicine and Surgery, vol. 35, pp. 153-157. http://dx.doi.org/10.1016/j.amsu.2018.09.040. PMid:30302246.
http://dx.doi.org/10.1016/j.amsu.2018.09...
from Harare, Zimbabwe (p=0.08).
4.3.3.5. (H014)
There was association between the presence of HP infection and dining habits. A similar report was by Mhaskar et al. (2013)MHASKAR, R.S., RICARDO, I., AZLIYATI, A., LAXMINARAYAN, R., AMOL, B., SANTOSH, W. and BOO, K., 2013. Assessment of risk factors of Helicobacter pylori infection and peptic ulcer disease. Journal of Global Infectious Diseases, vol. 5, no. 2, pp. 60-67. http://dx.doi.org/10.4103/0974-777X.112288. PMid:23853433.
http://dx.doi.org/10.4103/0974-777X.1122...
from Pune, Maharashtra State, India (Yate’s χ2 value=30.987, d.f.=1, p< 0.05).
4.3.3.6. (H015)
There was association between the presence of HP infection and milk consumption. No relevant studies were available to compare in local, national, regional, and global literature.
4.3.3.7. (H016)
There was association between HP infection and drinking water sources. A similar report was by Khoder et al. (2019)KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044. PMid:30939800.
http://dx.doi.org/10.3390/pathogens80200...
from UAE (p=0.001). In contrast, no association was from Rasheed et al. from Islamabad, Pakistan, in 2008-2009 (p=0.885) and (Khoder et al., 2019KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044. PMid:30939800.
http://dx.doi.org/10.3390/pathogens80200...
).
4.3.3.8. (H017)
There was association between the presence of HP infection and animal contact. A similar report was by Rasheed et al. (2012)RASHEED, F., AHMAD, T. and BILAL, R., 2012. Prevalence and risk factors of Helicobacter pylori infection among Pakistani population. Pakistan Journal of Medical Sciences, vol. 28, no. 4, pp. 661-665. from Islamabad in 2008-2009 (p=0.004). Opposing reports of no association were from Khoder et al. (Sharma et al., 1997SHARMA, T.K., YOUNG, E.L., MILLER, S. and CUTLER, A.F., 1997. Evaluation of a rapid, new method for detecting serum IgG antibodies to Helicobacter pylori. Clinical Chemistry, vol. 43, no. 5, pp. 832-836. http://dx.doi.org/10.1093/clinchem/43.5.832. PMid:9166238.
http://dx.doi.org/10.1093/clinchem/43.5....
) from UAE (p=0.445), Elhariri et al. (2017)ELHARIRI, M., ELHELW, R., HAMZA, D. and EL-MAHALLAWY, H.S., 2017. Serologic evidence and risk factors for Helicobacter pylori infection in animals and humans. Journal of Infection in Developing Countries, vol. 11, no. 5, pp. 414-419. http://dx.doi.org/10.3855/jidc.9339. PMid:30943179.
http://dx.doi.org/10.3855/jidc.9339...
from Cairo (Yate’s χ2 value=0.9183, d.f.=1, p=0.338) and Mungazi et al. (Daniel and Cross, 2018DANIEL, W.W. and CROSS, C.L., 2018. Biostatistics: a foundation for analysis in the health sciences. Hoboken: John Wiley & Sons.) from Harare, Zimbabwe (p=0.119).
Immunochromatographic test (ICT) is a rapid, inexpensive, widely used, and highly sensitive screening tool for the qualitative detection of antibodies (IgG, IgM, and IgA) against HP in human serum, plasma, or whole blood (CTK Biotech, 2020CTK BIOTECH, 2020 [viewed 13 November 2021]. H. pylori Ab combo rapid test CE [online]. CTK Biotech. Available from: https://ctkbiotech.com/product/h-pylori-ab-combo-rapid-test-ce/.
https://ctkbiotech.com/product/h-pylori-...
). It has been used in many investigational studies. Sharma et al. used it in Detroit, USA, in 1997 (n=96), showing 95% sensitivity, 77% specificity, 86% positive predictive value, and 91% negative predictive value in fresh serum (Sharma et al., 1997SHARMA, T.K., YOUNG, E.L., MILLER, S. and CUTLER, A.F., 1997. Evaluation of a rapid, new method for detecting serum IgG antibodies to Helicobacter pylori. Clinical Chemistry, vol. 43, no. 5, pp. 832-836. http://dx.doi.org/10.1093/clinchem/43.5.832. PMid:9166238.
http://dx.doi.org/10.1093/clinchem/43.5....
). Rahman et al. from Bangladesh used it in their study from June 2004-January 2005 (n=82) and reported 90.1% specificity, 80.9% sensitivity, 93.2% positive predictive value, 73.9% negative predictive value, and 87.8% accuracy (Rahman et al., 2008RAHMAN, S.H.Z., AZAM, M.G., RAHMAN, M.A., ARFIN, M.S., ALAM, M.M., BHUIYAN, T.M., AHMED, N., RAHMAN, M., NAHAR, S. and HASSAN, M.S., 2008. Non-invasive diagnosis of H pylori infection: evaluation of serological tests with and without current infection marker CIM. World Journal of Gastroenterology, vol. 14, no. 8, pp. 1231-1236. http://dx.doi.org/10.3748/wjg.14.1231. PMid:18300349.
http://dx.doi.org/10.3748/wjg.14.1231...
). Another recent study by Raj et al. from Bronx, NY, USA in 2009-2013 reported 88.4% sensitivity and 93.4% specificity against histology (Raj et al., 2017RAJ, P., THOMPSON, J.F. and PAN, D.H., 2017. Helicobacter pylori serology testing is a useful diagnostic screening tool for symptomatic inner city children. Acta Paediatrica, vol. 106, no. 3, pp. 470-477. http://dx.doi.org/10.1111/apa.13724. PMid:28024098.
http://dx.doi.org/10.1111/apa.13724...
).
5. Conclusions and Recommendations
About half the population (45-51%) of adults and adolescents with gastric symptoms was infected with HP with similar observed and expected prevalence. Distribution was different in sample and population by sex, age groups, education status, overcrowding, dining habits, milk consumption, drinking water source, and animal contact. HP infection in the population was associated with sex, education status, overcrowding, dining habits, milk consumption, drinking water source, and animal contact but not to age groups. This association does not mean that these are risk factors. It merely shows that these variables are seen more often than merely due to chance with the presence of HP infection. Cross-sectional inquiry lacks temporality, so it cannot tell which variable is exposure (risk factor) and which one is the outcome (disease). Still, it helps us which variable may be taken as exposure (speculated risk factor) and which one as the outcome (disease) in generating/ formulating hypothesis for verification through analytical observational (case-control and cohort) designs to cope further into the cause-n-effect relationship.
We will suggest more work for our population as a case-control design, whereby the relationship of the presence of HP infection with each of these socio-demographic, dietary, and lifestyle variables is evaluated by odds ratio and further as a cohort design to be assessed as a relative risk so that risk factors can be defined and preventive/ control interventions/ measures can be recommended.
6. Ethical Approval
Ethical approval was granted by the Departmental Bioethical Committee of The University of Haripur, Haripur, Pakistan. Consent from the management of District Headquarter Hospital, Haripur, was taken to collect data. The consent of the patients/guardians was taken before inclusion in the study.
References
- AHMAD, A., GOVIL, Y. and FRANK, B.B., 2003. Gastric mucosa-associated lymphoid tissue lymphoma. American Journal of Gastroenterology, vol. 98, no. 5, pp. 975-986. http://dx.doi.org/10.1111/j.1572-0241.2003.07424.x PMid:12809817.
» http://dx.doi.org/10.1111/j.1572-0241.2003.07424.x - ALVI, M.Z.-U.-D., SATTAR, M., CHEEMA, F.A., AWAN, U.A., AFTAB, M.N., SHAH, Z.H. and AFZAL, M.S., 2021. COVID-19 and emergence of antimicrobial resistance: a most neglected aspect of health emergency in Pakistan. Diabetes & Metabolic Syndrome, vol. 15, no. 4, p. 102179. http://dx.doi.org/10.1016/j.dsx.2021.06.016. PMid:34186352.
- ASSAAD, S., CHAABAN, R., TANNOUS, F. and COSTANIAN, C., 2018. Dietary habits and Helicobacter pylori infection: a cross sectional study at a Lebanese hospital. BMC Gastroenterology, vol. 18, no. 1, p. 48. http://dx.doi.org/10.1186/s12876-018-0775-1 PMid:29661143.
» http://dx.doi.org/10.1186/s12876-018-0775-1 - AWAN, U.A., KHATTAK, A.A., AFZAL, M.S., IQBAL, N. and NADEEM, M.F., 2021a. Emergence of SARS‐CoV‐2 variant: a wake‐up call for Pakistan’s overburdened healthcare system. Journal of Medical Virology, vol. 93, no. 5, pp. 2595-2598. http://dx.doi.org/10.1002/jmv.26825 PMid:33506951.
» http://dx.doi.org/10.1002/jmv.26825 - AWAN, U.A., KHATTAK, A.A., AFZAL, M.S., KHAN, H.I., SAQIB, M.A.N. and AHMED, H., 2021b. COVID-19 and tuberculosis overlapping epidemics: a holistic review from Pakistan. Journal of Medical Virology, vol. 93, no. 5, pp. 2573-2575. http://dx.doi.org/10.1002/jmv.26714 PMid:33295641.
» http://dx.doi.org/10.1002/jmv.26714 - AWAN, U.A., ZAHOOR, S., AYUB, A., AHMED, H., AFTAB, N. and AFZAL, M.S., 2021c. COVID‐19 and arboviral diseases: another challenge for Pakistan’s dilapidated healthcare system. Journal of Medical Virology, vol. 93, no. 7, pp. 4065-4067. http://dx.doi.org/10.1002/jmv.26668 PMid:33200437.
» http://dx.doi.org/10.1002/jmv.26668 - BASTÁN, J.E.P., PONCE, R.H. and HERNÁNDEZ, B.R., 2021. Caracterización clínico epidemiológica de la infección por Helicobacter pylori en pacientes con úlcera péptica. Revista Cubana de Medicina General Integral, vol. 37, no. 1, p. e1288.
- CHANG, A.H. and PARSONNET, J., 2010. Role of bacteria in oncogenesis. Clinical Microbiology Reviews, vol. 23, no. 4, pp. 837-857. http://dx.doi.org/10.1128/CMR.00012-10 PMid:20930075.
» http://dx.doi.org/10.1128/CMR.00012-10 - COELHO, L.G.V. and COELHO, M.C.F., 2021. Helicobacter pylori and colorectal neoplasms: a concise review. Arquivos de Gastroenterologia, vol. 58, no. 1, pp. 114-119. http://dx.doi.org/10.1590/s0004-2803.202100000-19 PMid:33909789.
» http://dx.doi.org/10.1590/s0004-2803.202100000-19 - COELHO, M.C.F., RIBEIRO, H.G., GOMES, C.G.D.O., MARINHO, F.P., BARBOSA, A.J. and COELHO, L.G.V., 2021. Helicobacter pylori chronic gastritis on patients with premalignant conditions: OLGA and OLGIM evaluation and serum biomarkers performance. Arquivos de Gastroenterologia, vol. 58, no. 1, pp. 39-47. http://dx.doi.org/10.1590/s0004-2803.202100000-08 PMid:33909795.
» http://dx.doi.org/10.1590/s0004-2803.202100000-08 - CTK BIOTECH, 2020 [viewed 13 November 2021]. H. pylori Ab combo rapid test CE [online]. CTK Biotech. Available from: https://ctkbiotech.com/product/h-pylori-ab-combo-rapid-test-ce/
» https://ctkbiotech.com/product/h-pylori-ab-combo-rapid-test-ce/ - DANIEL, W.W. and CROSS, C.L., 2018. Biostatistics: a foundation for analysis in the health sciences Hoboken: John Wiley & Sons.
- ELHARIRI, M., ELHELW, R., HAMZA, D. and EL-MAHALLAWY, H.S., 2017. Serologic evidence and risk factors for Helicobacter pylori infection in animals and humans. Journal of Infection in Developing Countries, vol. 11, no. 5, pp. 414-419. http://dx.doi.org/10.3855/jidc.9339 PMid:30943179.
» http://dx.doi.org/10.3855/jidc.9339 - ESLICK, G.D., LIM, L.L.-Y., BYLES, J.E., XIA, H.H.-X. and TALLEY, N.J., 1999. Association of Helicobacter pylori infection with gastric carcinoma: a meta-analysis. American Journal of Gastroenterology, vol. 94, no. 9, pp. 2373-2379. http://dx.doi.org/10.1111/j.1572-0241.1999.01360.x PMid:10483994.
» http://dx.doi.org/10.1111/j.1572-0241.1999.01360.x - HANAFIAH, A., RAZAK, S.A., NEOH, H.-M., ZIN, N.M. and LOPES, B.S., 2020. The heterogeneic distribution of Helicobacter pylori cag pathogenicity island reflects different pathologies in multiracial Malaysian population. The Brazilian Journal of Infectious Diseases, vol. 24, no. 6, pp. 545-551. http://dx.doi.org/10.1016/j.bjid.2020.10.005 PMid:33157035.
» http://dx.doi.org/10.1016/j.bjid.2020.10.005 - HAQQI, A., AWAN, U.A., ALI, M., SAQIB, M.A.N., AHMED, H. and AFZAL, M.S., 2021. COVID‐19 and dengue virus co‐epidemics in Pakistan: a dangerous combination for overburdened healthcare system. Journal of Medical Virology, vol. 93, no. 1, pp. 80-82. http://dx.doi.org/10.1002/jmv.26144 PMid:32510175.
» http://dx.doi.org/10.1002/jmv.26144 - HEDAYATI, M.A., AHMADI, S., SERVATYARI, K. and SHEIKHESMAEILI, F., 2021. PREX2 gene’s expression in gastric antral epithelial cells of patients with H. pylori infection. Arquivos de Gastroenterologia, vol. 58, no. 3, pp. 353-358. http://dx.doi.org/10.1590/s0004-2803.202100000-59 PMid:34705970.
» http://dx.doi.org/10.1590/s0004-2803.202100000-59 - HOOI, J.K., LAI, W.Y., NG, W.K., SUEN, M.M., UNDERWOOD, F.E., TANYINGOH, D., MALFERTHEINER, P., GRAHAM, D.Y., WONG, V.W., WU, J.C., CHAN, F.K.L., SUNG, J.J.Y., KAPLAN, G.G. and NG, S.C., 2017. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology, vol. 153, no. 2, pp. 420-429. http://dx.doi.org/10.1053/j.gastro.2017.04.022 PMid:28456631.
» http://dx.doi.org/10.1053/j.gastro.2017.04.022 - KHODER, G., MUHAMMAD, J.S., MAHMOUD, I., SOLIMAN, S.S.M. and BURUCOA, C., 2019. Prevalence of Helicobacter pylori and its associated factors among healthy asymptomatic residents in the United Arab Emirates. Pathogens, vol. 8, no. 2, p. 44. http://dx.doi.org/10.3390/pathogens8020044 PMid:30939800.
» http://dx.doi.org/10.3390/pathogens8020044 - MABEKU, L.B.K., NGAMGA, M.L.N. and LEUNDJI, H., 2018. Potential risk factors and prevalence of Helicobacter pylori infection among adult patients with dyspepsia symptoms in Cameroon. BMC Infectious Diseases, vol. 18, no. 1, p. 278. http://dx.doi.org/10.1186/s12879-018-3146-1 PMid:29907086.
» http://dx.doi.org/10.1186/s12879-018-3146-1 - MHASKAR, R.S., RICARDO, I., AZLIYATI, A., LAXMINARAYAN, R., AMOL, B., SANTOSH, W. and BOO, K., 2013. Assessment of risk factors of Helicobacter pylori infection and peptic ulcer disease. Journal of Global Infectious Diseases, vol. 5, no. 2, pp. 60-67. http://dx.doi.org/10.4103/0974-777X.112288 PMid:23853433.
» http://dx.doi.org/10.4103/0974-777X.112288 - MOOSAZADEH, M., LANKARANI, K.B. and AFSHARI, M., 2016. Meta-analysis of the prevalence of Helicobacter pylori infection among children and adults of Iran. International Journal of Preventive Medicine, vol. 7, no. 1, p. 48. http://dx.doi.org/10.4103/2008-7802.177893 PMid:27076886.
» http://dx.doi.org/10.4103/2008-7802.177893 - MUHAMMAD, J.S., ZAIDI, S.F. and SUGIYAMA, T., 2012. Epidemiological ins and outs of helicobacter pylori: a review. Journal of the Pakistan Medical Association, vol. 62, no. 9, pp. 955-959. PMid:23139983.
- MUNGAZI, S.G., CHIHAKA, O.B. and MUGUTI, G.I., 2018. Prevalence of Helicobacter pylori in asymptomatic patients at surgical outpatient department: harare hospitals. Annals of Medicine and Surgery, vol. 35, pp. 153-157. http://dx.doi.org/10.1016/j.amsu.2018.09.040 PMid:30302246.
» http://dx.doi.org/10.1016/j.amsu.2018.09.040 - NADEEM, M.F., KHATTAK, A.A., ZEESHAN, N., AWAN, U.A., ALAM, S., AHMED, W., GUL, S., AFROZ, A., SUGHRA, K., RASHID, U. and KHAN, M.A.U., 2023. Molecular epidemiology of Plasmodium species in conflicted Federally Administered Tribal Area (FATA) Pakistan. Brazilian Journal of Biology = Revista Brasileira de Biologia, vol. 83, p. e247219. http://dx.doi.org/10.1590/1519-6984.247219 PMid:34468526.
» http://dx.doi.org/10.1590/1519-6984.247219 - OZAYDIN, N., TURKYILMAZ, S.A. and CALI, S., 2013. Prevalence and risk factors of helicobacter pylori in Turkey: a nationally-representative, cross-sectional, screening with the 13 C-Urea breath test. BMC Public Health, vol. 13, no. 1, p. 1215. http://dx.doi.org/10.1186/1471-2458-13-1215 PMid:24359515.
» http://dx.doi.org/10.1186/1471-2458-13-1215 - PAGANO, M. and GAUVREAU, K., 2018. Principles of biostatistics New York: CRC Press.
- QASIM, M., AWAN, U.A., AFZAL, M.S., SAQIB, M.A.N., SIDDIQUI, S. and AHMED, H., 2020. Dataset of knowledge, attitude, practices and psychological implications of healthcare workers in Pakistan during COVID-19 pandemic. Data in Brief, vol. 32, p. 106234. http://dx.doi.org/10.1016/j.dib.2020.106234 PMid:32895632.
» http://dx.doi.org/10.1016/j.dib.2020.106234 - RAHMAN, S.H.Z., AZAM, M.G., RAHMAN, M.A., ARFIN, M.S., ALAM, M.M., BHUIYAN, T.M., AHMED, N., RAHMAN, M., NAHAR, S. and HASSAN, M.S., 2008. Non-invasive diagnosis of H pylori infection: evaluation of serological tests with and without current infection marker CIM. World Journal of Gastroenterology, vol. 14, no. 8, pp. 1231-1236. http://dx.doi.org/10.3748/wjg.14.1231 PMid:18300349.
» http://dx.doi.org/10.3748/wjg.14.1231 - RAJ, P., THOMPSON, J.F. and PAN, D.H., 2017. Helicobacter pylori serology testing is a useful diagnostic screening tool for symptomatic inner city children. Acta Paediatrica, vol. 106, no. 3, pp. 470-477. http://dx.doi.org/10.1111/apa.13724 PMid:28024098.
» http://dx.doi.org/10.1111/apa.13724 - RAOSOFT, 2004 [viewed 20 October 2020]. Sample size calculator [online]. RAOSOFT. Available from: http://www.raosoft.com/samplesize.html
» http://www.raosoft.com/samplesize.html - RASHEED, F., AHMAD, T. and BILAL, R., 2012. Prevalence and risk factors of Helicobacter pylori infection among Pakistani population. Pakistan Journal of Medical Sciences, vol. 28, no. 4, pp. 661-665.
- RASHEED, F., YAMEEN, A., AHMAD, T. and BILAL, R., 2017. Rate of active Helicobacter pylori infection among symptomatic patients of Pakistan. The Malaysian Journal of Pathology, vol. 39, no. 1, pp. 69-72. PMid:28413207.
- RASTOGI, M., RASTOGI, D., SINGH, S., AGARWAL, A., PRIYADARSHI, B. and MIDDHA, T., 2015. Prevalence of Helicobacter pylori in asymptomatic adult patients in a tertiary care hospital: a cross sectional study. Biomedical Research, vol. 26, no. 1, pp. 117-122.
- SALIH, B.A., 2009. Helicobacter pylori infection in developing countries: the burden for how long? Saudi Journal of Gastroenterology, vol. 15, no. 3, pp. 201-207. http://dx.doi.org/10.4103/1319-3767.54743 PMid:19636185.
» http://dx.doi.org/10.4103/1319-3767.54743 - SANTOS, I.S., BOCCIO, J., SANTOS, A.S., VALLE, N.C.J., HALAL, C.S., BACHILLI, M.C. and LOPES, R.D., 2005. Prevalence of Helicobacter pylori infection and associated factors among adults in southern Brazil: a population-based cross-sectional study. BMC Public Health, vol. 5, no. 1, p. 118. http://dx.doi.org/10.1186/1471-2458-5-118 PMid:16283940.
» http://dx.doi.org/10.1186/1471-2458-5-118 - SHARMA, T.K., YOUNG, E.L., MILLER, S. and CUTLER, A.F., 1997. Evaluation of a rapid, new method for detecting serum IgG antibodies to Helicobacter pylori. Clinical Chemistry, vol. 43, no. 5, pp. 832-836. http://dx.doi.org/10.1093/clinchem/43.5.832 PMid:9166238.
» http://dx.doi.org/10.1093/clinchem/43.5.832 - SHU, L., ZHENG, P.-F., ZHANG, X.-Y. and FENG, Y.-L., 2019. Dietary patterns and Helicobacter pylori infection in a group of Chinese adults ages between 45 and 59 years old: an observational study. Medicine, vol. 98, no. 2, p. e14113. http://dx.doi.org/10.1097/MD.0000000000014113 PMid:30633225.
» http://dx.doi.org/10.1097/MD.0000000000014113 - SINGH, V., TRIKHA, B., NAIN, C.K., SINGH, K. and VAIPHEI, K., 2002. Epidemiology of Helicobacter pylori and peptic ulcer in India. Journal of Gastroenterology and Hepatology, vol. 17, no. 6, pp. 659-665. http://dx.doi.org/10.1046/j.1440-1746.2002.02746.x PMid:12100610.
» http://dx.doi.org/10.1046/j.1440-1746.2002.02746.x - SMOLKA, A.J. and BACKERT, S., 2012. How Helicobacter pylori infection controls gastric acid secretion. Journal of Gastroenterology, vol. 47, no. 6, pp. 609-618. http://dx.doi.org/10.1007/s00535-012-0592-1 PMid:22565637.
» http://dx.doi.org/10.1007/s00535-012-0592-1 - SOCIAL SCIENCE STATISTICS, 2014 [viewed 13 November 2021]. Statistics Calculators [online]. Available from: https://www.socscistatistics.com/tests/
» https://www.socscistatistics.com/tests/ - TORRES, J., PÉREZ-PÉREZ, G., GOODMAN, K.J., ATHERTON, J.C., GOLD, B.D., HARRIS, P.R., GARZA, A.M., GUARNER, J. and MUÑOZ, O., 2000. A comprehensive review of the natural history of Helicobacter pylori infection in children. Archives of Medical Research, vol. 31, no. 5, pp. 431-469. http://dx.doi.org/10.1016/S0188-4409(00)00099-0 PMid:11179581.
» http://dx.doi.org/10.1016/S0188-4409(00)00099-0 - WORLD HEALTH ORGANIZATION – WHO, 2013 [viewed 20 October 2020]. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach [online]. WHO. Available from: https://www.who.int/publications/i/item/9789241505727
» https://www.who.int/publications/i/item/9789241505727 - ZAR, J.H., 1999. Biostatistical analysis Hoboken: Prentice Hall.
- ZHU, Y., ZHOU, X., WU, J., SU, J. and ZHANG, G., 2014. Risk factors and prevalence of Helicobacter pylori infection in persistent high incidence area of gastric carcinoma in Yangzhong city. Gastroenterology Research and Practice, vol. 2014, p. 481365. http://dx.doi.org/10.1155/2014/481365 PMid:24550981.
» http://dx.doi.org/10.1155/2014/481365
Publication Dates
-
Publication in this collection
17 June 2022 -
Date of issue
2024
History
-
Received
19 Feb 2021 -
Accepted
13 Nov 2021