Abstract
Current cross-sectional study was carried out between September 2019 to January 2020 at the Department of Pathology, Mardan Medical Complex (MMC), Mardan, and District Headquarter Hospital North Waziristan, Khyber Pakhtunkhwa (KP), Pakistan. The objectives of the current study were to determine the prevalence of leishmaniasis and its associated risk factors in selected districts of KP province, Pakistan. Altogether, three hundred and seventy-four (n=374) leishmaniosis patients were included in the current study. Skin specimen from the ulcer border were collected. The slides were stained by Giemsa stain and examined for the presence of amastigote. The prevalence of leishmania infected patients in different region of KP were as follows: North Waziristan region 53.7 (n=201) District Mardan 34.7% (n=130); District Nowshera 6.7% (n=25), District Swabi 1.1% (n=4) and other Districts i.e. Dir, Malakand, Buner and Bajawarr were 3.7% (n=14). The frequency of leishmaniasis were more in male and majority of the infected patients were in the age group of <10 years. Among n=374 patients 95.7% (n= 358) had cutaneous leishmaniasis while 3% (n= 11) had mucocutaneous type of infection and 1.3% (n= 5) patients had both cutaneous and mucocutaneous infection. Upon treatment by Sodium stibogluconate (SSG) 97% (n=362) showed clinical signs of complete or partial recovery of their skin lesions. Conclusively, highest incidence of leishmania infection occurred during short study period and majority of the cases showed positive response to treatment.
Keywords:
cutaneous leishmaniasis; mucocutaneus leishmaniasis; treatment; KP; Pakistan
Resumo
O estudo transversal atual foi realizado entre setembro de 2019 e janeiro de 2020 no Departamento de Patologia Mardan Medical Complex (MMC), Mardan, e no District Headquarter Hospital North Waziristan, Khyber Pakhtunkhwa (KP), Paquistão. Os objetivos do presente estudo foram determinar a prevalência da leishmaniose e seus fatores de risco associados em distritos selecionados da província de KP, Paquistão. Ao todo, 374 (n = 374) pacientes com leishmaniose foram incluídos no presente estudo. Amostras de pele da borda da úlcera foram coletadas. As lâminas foram coradas pelo corante Giemsa e examinadas quanto à presença de amastigotas. As prevalências de pacientes infectados por leishmania em diferentes regiões de KP foram as seguintes: região do Waziristão Norte 53,7 (n = 201), distrito Mardan 34,7% (n = 130); distrito Nowshera 6,7% (n = 25), distrito Swabi 1,1% (n = 4) e outros distritos, ou seja, Dir, Malakand, Buner e Bajawarr foram 3,7% (n = 14). A frequência de leishmaniose foi maior no sexo masculino e a maioria dos pacientes infectados estava na faixa etária < 10 anos. Entre n = 374 pacientes, 95,7% (n = 358) tinham leishmaniose cutânea enquanto 3% (n = 11) tinham infecção do tipo mucocutâneo e 1,3% (n = 5) pacientes tinham infecção cutânea e mucocutânea. Após tratamento com estibogluconato de sódio (SSG), 97% (n = 362) apresentaram sinais clínicos de recuperação completa ou parcial de suas lesões cutâneas. Conclusivamente, a maior incidência de infecção por leishmania ocorreu durante o curto período de estudo e a maioria dos casos apresentou resposta positiva ao tratamento.
Palavras-chave:
leishmaniose cutânea; leishmaniose mucocutânea; tratamento; KP; Paquistão
1. Introduction
Leishmaniasis is a vector born protozoon infection caused by different species. The most common form is cutaneous leishmaniasis (CL). The leishmanial infections are considered as endemic in more than ninety countries of the world (Torres-Guerrero et al., 2017TORRES-GUERRERO, E., QUINTANILLA-CEDILLO, M.R., RUIZ-ESMENJAUD, J. and ARENAS, R., 2017. Leishmaniasis: a review. F1000 Research, vol. 6, p. 750. http://dx.doi.org/10.12688/f1000research.11120.1. PMid:28649370.
http://dx.doi.org/10.12688/f1000research...
; WHO, 2019WORLD HEALTH ORGANIZATION – WHO, 2019. Global leprosy update, 2018: moving towards a leprosyfree world. Weekly Epidemiological Record, vol. 94, no. 35-36, pp. 389-412.). Cutaneous leishmaniasis causes skin lesions, mainly ulcer on the body surfaces, with lifelong scares and serious disabilities whereas, in mucocutaneous leishmaniasis (MCL) complete or partial destruction of the mucus membrane of the mouth, nose and throat occurs (WHO, 2019WORLD HEALTH ORGANIZATION – WHO, 2019. Global leprosy update, 2018: moving towards a leprosyfree world. Weekly Epidemiological Record, vol. 94, no. 35-36, pp. 389-412.). The diagnosis of leishmaniasis is generally based on clinical signs and symptoms, microscopic detection of the parasites and tissue culture. The reported causative agent of anthroponotic CL in Pakistan is mainly Leishmania tropica (L. tropica) seen in urban areas whereas for zoonotic CL is Leishmania major (L. major) more common in rural areas (Afghan et al., 2011AFGHAN, A.K., KASSI, M., KASI, P.M., AYUB, A., KAKAR, N. and MARRI, S.M., 2011. Clinical manifestations and distribution of cutaneous leishmaniasis in Pakistan. Journal of Tropical Medicine, vol. 2011, p. 359145. http://dx.doi.org/10.1155/2011/359145. PMid:22174721.
http://dx.doi.org/10.1155/2011/359145...
; Postigo, 2010POSTIGO, J.A.R., 2010. Leishmaniasis in the world health organization eastern mediterranean region. International Journal of Antimicrobial Agents, vol. 36, suppl. 1, pp. S62-S65. http://dx.doi.org/10.1016/j.ijantimicag.2010.06.023. PMid:20728317.
http://dx.doi.org/10.1016/j.ijantimicag....
). Globally, approximately 1.5 million new cases of CL are emerging annually and around 350 million people are at risk (Hawash et al., 2018HAWASH, Y.A., ISMAIL, K.A., ABDEL-WAHAB, M.M. and KHALIFA, M., 2018. Diagnosis, treatment and clinical features of cutaneous leishmaniasis in Saudi Arabia. Korean Journal of Parasitology, vol. 56, no. 3, pp. 229-236. http://dx.doi.org/10.3347/kjp.2018.56.3.229. PMid:29996626.
http://dx.doi.org/10.3347/kjp.2018.56.3....
). According to WHO, an estimated more than 90% cases of CL occurs in Afghanistan, Iran, Algeria, Brazil, Saudi Arabia, Syria, Pakistan, and Columbia (WHO, 2010WORLD HEALTH ORGANIZATION – WHO, 2010. Control of the leishmaniases: report of a meeting of the WHO Expert Commitee on the Control of Leishmaniases, Geneva, 22-26 March 2010. Geneva: WHO. WHO Technical Report Series.).
Cutaneous leishmaniasis is considered as a major public health concern in Pakistan. Although, CL is endemic in all Pakistan, but majority of the patients are continuously reported in KP province bordering the neighboring Afghanistan and especially from districts where refugees are residing (Afghan et al., 2011AFGHAN, A.K., KASSI, M., KASI, P.M., AYUB, A., KAKAR, N. and MARRI, S.M., 2011. Clinical manifestations and distribution of cutaneous leishmaniasis in Pakistan. Journal of Tropical Medicine, vol. 2011, p. 359145. http://dx.doi.org/10.1155/2011/359145. PMid:22174721.
http://dx.doi.org/10.1155/2011/359145...
). The major endemic areas of KP are southern region including Waziristan and other districts of KP like Mardan, Swabi, Nowshera, Dir, Buner, and Baja war. There is scarcity of data regarding prevalence of CL and its treatment efficacy in Pakistan, therefor this study was focused on current epidemiology, diagnosis, and treatment of this neglected diseases in the KP province of Pakistan.
2. Materials and Methods
2.1. Study design and setting
This cross-sectional study was carried out between September 2019 to January 2020 at the Department of Pathology, Mardan Medical Complex (MMC), Mardan and District Headquarter Hospital (DHQ), North Waziristan KP, Pakistan. The MMC is a 520 bedded largest referral tertiary care teaching hospital of the province. The hospital has emergency, intensive care unit and all the major and minor facilities with state of the art diagnostics and supportive services. The study population included patients of different age groups, with clinical signs and symptoms or with suspected leishmaniasis visited the MMC Mardan and DHQ North Waziristan. All those patients having coinfection or other skin disease were excluded from this study.
2.2. Clinical examination
Patients were clinically examined by a specialized dermatologist. Clinical examination involved affected tissues, characteristics of the lesions (size, site, appearance, and number). Furthermore, all the sociodemographic information’s including residence, animals in or near the house and history of the visit to endemic areas ( Last 1-3 months before appearance of the skin lesions ) were recorded.
2.3. Sample collection
A total of three hundred and seventy-four (n=374) leishmaniosis patients were included in the current study. The patient information such as age, gender, and location of wounds were recorded using a questioner’s form. After disinfecting the skin, by 70% alcohol, the disposable surgical blades or needles were used for collecting skin specimen from the ulcer border and spread on two different slides.
2.4. Sample processing and microscopic examination
The prepared slides were air dried and fixed with methanol. The fixed slides were stained by Giemsa stain and examined under microscope for the presence of amastigote as described elsewhere (Saab et al., 2015SAAB, M., HAGE, H., CHARAFEDDINE, K., HABIB, R.H. and KHALIFEH, I., 2015. Diagnosis of cutaneous leishmaniasis: why punch when you can scrape? The American Journal of Tropical Medicine and Hygiene, vol. 92, no. 3, pp. 518-522. http://dx.doi.org/10.4269/ajtmh.14-0512. PMid:25561563.
http://dx.doi.org/10.4269/ajtmh.14-0512...
). The diagnostic criteria of CL and MCL were based on the presence of amastigote within the smear.
2.5. Patient’s treatment and follow up
All the laboratory confirmed cases were treated by intralesional or intramuscular Sodium stibogluconate (SSG); (Pentostam, Glaxo Smith Kline, Uxbridge, UK). The SSG was administered at a dose of 20mg/kg/day for 10-20 days. During intramuscular injections ulcerative lesions was observed for healing. The lesions resolution signs included size regression (Complete or partial scarring and re-epithelialization) and reduction in inflammatory signs (skin edema, erythema, and hardening).
2.6. Statistical analysis
The association of Leishmania infection with potential risk factors was observed by using SPSS. Odds ratios with 95% confidence interval were calculated and p value <0.05 were considered as significant. Lambda values were calculated using Pearson correlation.
2.7. Ethics statement
After the detailed explanation of the study purpose and procedures informed written consent were obtained from all the participants (>18years) and those under 18 years were obtained from the patient attendant or parents. The ethical permission was obtained from the ethical committee of hospital and Department of Medical Lab Technology, The University of Haripur.
3. Results
3.1. Study population and characteristics
Three hundred and seventy-four (n=374) patients with suspected CL and MCL were investigated. Living areas of the leishmanial infected patients were as follows: North Waziristan region 53.7% (n=201), District Mardan 34.7% (n=130), District Nowshera 6.7% (n=25), District Swabi 1.1% (n=4) and other Districts i.e., Dir, Malakand, Buner and Bajawarr were 3.7%(n=14). Gender wise male and female were 63.6%(n=238) and 36.4% (n=136) respectively. The frequency of leishmaniasis were more in male and majority of the infected patients were in the age group of <10 years. The overall frequency of leishmania infected patients and their clinical and demographic characteristics are shown in Table 1. All the cases were reported during the winter season. Moreover, 82.8% (n=310) patients have a close contact with domestic animals or nearby their houses.
Demographic and clinical features of leishmaniasis patients attending tertiary care teaching hospital Mardan Medical Complex (MMC), Mardan and District Headquarter Hospital North Waziristan, KP, Pakistan from September 2019 to January 2020.
3.2. Clinical characteristics
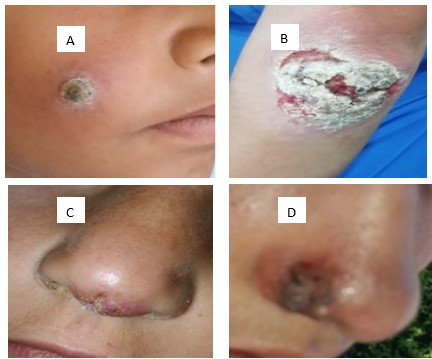
The leishmanial lesions were confined to patient skin and mucosal membrane with no other tissue involvement noticed. One hundred and twenty-two (32.6%) individuals have multiple lesions. The affected lesions were observed mainly on exposed body parts, the face, the lower limbs, and the upper limbs (30.5%, 25.2% and 32.6%) respectively (Figure 1; Table1).
Images of patients having cutaneous leishmaniasis (A and B), mucocutaneous leishmaniasis (C and D) attending tertiary care teaching hospital Mardan Medical Complex (MMC), Mardan, and District Headquarter Hospital North Waziristan, KP, Pakistan from September 2019 to January 2020.
3.3. Prevalence of leishmania infection
Among n=374 patients 95.7% (n= 358) had cutaneous leishmaniasis (scars on skin, legs, feet, neck and hands) while 3% (n= 11) had mucocutaneous type of infection (lesions on lips, nose and throat area) and 1.3%(n=5) patients had both cutaneous and mucocutaneous infection (lesions on skin, lips, nose, hands, thoracic cavity and feet) (Table 2).
Leishmaniasis lesion sites and other factors cross tabulation of leishmaniasis patients attending tertiary care teaching hospital Mardan Medical Complex (MMC), Mardan, and District Headquarter Hospital North Waziristan, KP, Pakistan from September 2019 to January 2020.
3.4. Prevalence of leishmania infection in various districts
Being highly endemic region, highest prevalence 53.7%(201/374) was reported from North Waziristan. Among patients from North Waziristan only one patient has travel history. Region wise variation was observed in incidence of leishmaniasis. In district Mardan one hundred and thirty (34.7%) of leishmaniasis cases were reported and 60.7% (n=79/130) of the patients had no travel history and their distribution in different areas of district Mardan were as follows; Lund Khwar; 67.1%(n=53/130), Karamar Shabaz Ghara ;20.2% (n=16/130),Takht Bhai; 6.3% (n=5/130), Babozai ;3.8%(n=3/130) and Jamal Gharay 2.5% (n=2/130). The remaining fifty-one (39.2%) have travel history outside the Mardan district. Their distribution according to their travel destinations were as follows; District Nowshera; 23.5%(n=12/51), Baluchistan; 21.5% (n=11/51), District Dir; 13.7% (n=7/51), Bajawarr 7.8% (n=4/51), Mohmand Agency; 3.9% (n=2/51) and district Hangu, Tank and Chakwal (Punjab province); 3.9% (n=2/51) respectively. Twenty-five (6.7%) patients with leishmaniasis cases were reported from district Nowshera and their distribution were as follows; Aza Khel; 76% (n=19/25), Nizam Pur; 16% (n=4/25) and Khair Abad; 8%(n=2/25). The cases reported from districts Swabi, Dir, Darghi, Bajawarr and Buner were 1.1% (n=4/374), 1.3% (5/374), 1.1% (4/374), 0.8% (3/374) and 0.6% (2/374) respectively.
3.5. Treatment and follow up
Three hundred and seventy-four (n=374) laboratory confirmed patients were treated with SSG injections. At the end of therapy, all the patients were followed up. Three hundred and sixty-two (97%) showed clinical signs of complete or partial recovery of their skin lesions. The remaining 3% (n=12/374) patients had no sign of recovery for their skin lesions.
4. Discussion
During the study period, three hundred and seventy-four (n=374) patients with active leishmanial skin lesions were identified. The number of cases detected relatively in short study period were comparatively highest than the previous reports (Abuzaid et al., 2017ABUZAID, A.A., ABDOON, A.M., ALDAHAN, M.A., ALZAHRANI, A.G., ALHAKEEM, R.F., ASIRI, A.M., ALZAHRANI, M.H. and MEMISH, Z.A., 2017. Cutaneous leishmaniasis in Saudi Arabia: a comprehensive overview. Vector Borne and Zoonotic Diseases, vol. 17, no. 10, pp. 673-684. http://dx.doi.org/10.1089/vbz.2017.2119. PMid:28806141.
http://dx.doi.org/10.1089/vbz.2017.2119...
; Hawash et al., 2018HAWASH, Y.A., ISMAIL, K.A., ABDEL-WAHAB, M.M. and KHALIFA, M., 2018. Diagnosis, treatment and clinical features of cutaneous leishmaniasis in Saudi Arabia. Korean Journal of Parasitology, vol. 56, no. 3, pp. 229-236. http://dx.doi.org/10.3347/kjp.2018.56.3.229. PMid:29996626.
http://dx.doi.org/10.3347/kjp.2018.56.3....
). Factors that contribute to increase prevalence might be growing population size, increasing urbanization, frequent population mobility, poverty, and poor health standards. Furthermore, the advancement in diseases diagnosis and awareness regarding early treatment may be additional factors. However, we observed highest prevalence from North Waziristan region, which is war effected zone from the last 10-12 years and majority of the residence are internally displaced.
The current study was carried out during the winter season. Previously, high prevalence has been reported during the winter season (Amin et al., 2013AMIN, T.T., AL-MOHAMMED, H.I., KALIYADAN, F. and MOHAMMED, B.S., 2013. Cutaneous leishmaniasis in Al Hassa, Saudi Arabia: epidemiological trends from 2000 to 2010. Asian Pacific Journal of Tropical Medicine, vol. 6, no. 8, pp. 667-672. http://dx.doi.org/10.1016/S1995-7645(13)60116-9. PMid:23790342.
http://dx.doi.org/10.1016/S1995-7645(13)...
; Haouas et al., 2015HAOUAS, N., AMER, O., ISHANKYTY, A., ALAZMI, A. and ISHANKYTY, I., 2015. Profile and geographical distribution of reported cutaneous leishmaniasis cases in northwestern Saudi Arabia, from 2010 to 2013. Asian Pacific Journal of Tropical Medicine, vol. 8, no. 4, pp. 287-291. http://dx.doi.org/10.1016/S1995-7645(14)60332-1. PMid:25975500.
http://dx.doi.org/10.1016/S1995-7645(14)...
). However, another study reported its high prevalence in the summer (Bousslimi et al., 2010BOUSSLIMI, N., AOUN, K., BEN-ABDA, I., BEN-ALAYA-BOUAFIF, N., RAOUANE, M. and BOURATBINE, A., 2010. Epidemiologic and clinical features of cutaneous leishmaniasis in southeastern Tunisia. The American Journal of Tropical Medicine and Hygiene, vol. 83, no. 5, pp. 1034-1039. http://dx.doi.org/10.4269/ajtmh.2010.10-0234. PMid:21036833.
http://dx.doi.org/10.4269/ajtmh.2010.10-...
). This seasonal variation among different studies might be due to local climate and its effects on the activities on the host vector. It has also been observed that the insect is more active during humid environments and bread in spaces where sufficient moisture is available (Chaves and Pascual, 2006CHAVES, L.F. and PASCUAL, M., 2006. Climate cycles and forecasts of cutaneous leishmaniasis, a nonstationary vector-borne disease. PLoS Medicine, vol. 3, no. 8, p. e295. http://dx.doi.org/10.1371/journal.pmed.0030295. PMid:16903778.
http://dx.doi.org/10.1371/journal.pmed.0...
).
Gender wise male were more infected, as they are more exposed to environment and majority of them have either ground sleeping habits or close contact with the animals. Domestic animals can serve as a reservoir for the parasite and transmission may occur from animal to sand fly to human. These finding are consistence with the previous reports (Mumtaz et al., 2016MUMTAZ, S., MUNIR, A.H., ASGHAR, M. and NAHEED, N., 2016. Frequency and types of leishmaniasis in Khyber Pakhtunkhwa (KPK). Journal of Medical Sciences, vol. 24, pp. 136-140.; Farahmand et al., 2011FARAHMAND, M., NAHREVANIAN, H., SHIRAZI, H.A., NAEIMI, S. and FARZANEHNEJAD, Z., 2011. An overview of a diagnostic and epidemiologic reappraisal of cutaneous leishmaniasis in Iran. The Brazilian Journal of Infectious Diseases, vol. 15, no. 1, pp. 17-21. http://dx.doi.org/10.1016/S1413-8670(11)70134-9. PMid:21412584.
http://dx.doi.org/10.1016/S1413-8670(11)...
). Patients having age <10 years and male were more infected. Similar patron has been observed previously (Abuzaid et al., 2017ABUZAID, A.A., ABDOON, A.M., ALDAHAN, M.A., ALZAHRANI, A.G., ALHAKEEM, R.F., ASIRI, A.M., ALZAHRANI, M.H. and MEMISH, Z.A., 2017. Cutaneous leishmaniasis in Saudi Arabia: a comprehensive overview. Vector Borne and Zoonotic Diseases, vol. 17, no. 10, pp. 673-684. http://dx.doi.org/10.1089/vbz.2017.2119. PMid:28806141.
http://dx.doi.org/10.1089/vbz.2017.2119...
; Mumtaz et al., 2016MUMTAZ, S., MUNIR, A.H., ASGHAR, M. and NAHEED, N., 2016. Frequency and types of leishmaniasis in Khyber Pakhtunkhwa (KPK). Journal of Medical Sciences, vol. 24, pp. 136-140.; Farahmand et al., 2011FARAHMAND, M., NAHREVANIAN, H., SHIRAZI, H.A., NAEIMI, S. and FARZANEHNEJAD, Z., 2011. An overview of a diagnostic and epidemiologic reappraisal of cutaneous leishmaniasis in Iran. The Brazilian Journal of Infectious Diseases, vol. 15, no. 1, pp. 17-21. http://dx.doi.org/10.1016/S1413-8670(11)70134-9. PMid:21412584.
http://dx.doi.org/10.1016/S1413-8670(11)...
). This increase prevalence of Leishmania infection in younger population might be due to increase exposure to infectious sandfly bites. The proven risk factors for leishmaniasis in our study were male gender, young age, frequent travel, and rural residence.
All the suspected patients were diagnosed as CL and MCL on clinical presentation and microscopic examination as described elsewhere (Akilov et al., 2007AKILOV, O.E., KHACHEMOUNE, A. and HASAN, T., 2007. Clinical manifestations and classification of Old World cutaneous leishmaniasis. International Journal of Dermatology, vol. 46, no. 2, pp. 132-142. http://dx.doi.org/10.1111/j.1365-4632.2007.03154.x. PMid:17269962.
http://dx.doi.org/10.1111/j.1365-4632.20...
). The CL lesions were limited to skin whereas in case of MCL mucosal involvement were observed which are in consistence with the previous reports (Hawash et al., 2018HAWASH, Y.A., ISMAIL, K.A., ABDEL-WAHAB, M.M. and KHALIFA, M., 2018. Diagnosis, treatment and clinical features of cutaneous leishmaniasis in Saudi Arabia. Korean Journal of Parasitology, vol. 56, no. 3, pp. 229-236. http://dx.doi.org/10.3347/kjp.2018.56.3.229. PMid:29996626.
http://dx.doi.org/10.3347/kjp.2018.56.3....
; Zakai, 2014ZAKAI, H.A., 2014. Cutaneous leishmaniasis in Saudi Arabia: current status. Journal of Advanced Laboratory Research in Biology, vol. 5, no. 2, pp. 29-35.). We observed high prevalence of CL in this study, similar patron was also observed previously from Pakistan (Khan et al., 2016KHAN, N.H., BARI, A., HASHIM, R., KHAN, I., MUNEER, A., SHAH, A., WAHID, S., YARDLEY, V., O’NEIL, B. and SUTHERLAND, C.J., 2016. Cutaneous leishmaniasis in Khyber Pakhtunkhwa province of Pakistan: clinical diversity and species-level diagnosis. The American Journal of Tropical Medicine and Hygiene, vol. 95, no. 5, pp. 1106-1114. http://dx.doi.org/10.4269/ajtmh.16-0343. PMid:27601518.
http://dx.doi.org/10.4269/ajtmh.16-0343...
).
The SSG treatment was effective in 97% (n=362/374) patients who showed clinical signs of complete or partial recovery of their skin lesions. This treatment efficacy is comparatively high, then the previous report (Hawash et al., 2018HAWASH, Y.A., ISMAIL, K.A., ABDEL-WAHAB, M.M. and KHALIFA, M., 2018. Diagnosis, treatment and clinical features of cutaneous leishmaniasis in Saudi Arabia. Korean Journal of Parasitology, vol. 56, no. 3, pp. 229-236. http://dx.doi.org/10.3347/kjp.2018.56.3.229. PMid:29996626.
http://dx.doi.org/10.3347/kjp.2018.56.3....
). Previously, its lower efficacy has been reported elsewhere (Franke et al., 1990FRANKE, E.D., WIGNALL, F.S., CRUZ, M.E., ROSALES, E., TOVAR, A.A., LUCAS, C.M., LLANOS-CUENTAS, A. and BERMAN, J.D., 1990. Efficacy and toxicity of sodium stibogluconate for mucosal leishmaniasis. Annals of Internal Medicine, vol. 113, no. 12, pp. 934-940. http://dx.doi.org/10.7326/0003-4819-113-12-934. PMid:2173461.
http://dx.doi.org/10.7326/0003-4819-113-...
; Wortmann et al., 2002WORTMANN, G., MILLER, R.S., OSTER, C., JACKSON, J. and ARONSON, N., 2002. A randomized, double-blind study of the efficacy of a 10-or 20-day course of sodium stibogluconate for treatment of cutaneous leishmaniasis in United States military personnel. Clinical Infectious Diseases, vol. 35, no. 3, pp. 261-267. http://dx.doi.org/10.1086/341406. PMid:12115091.
http://dx.doi.org/10.1086/341406...
). The variation in drug efficacy might be due to causative leishmania species, duration and severity of the lesions, therapeutic regimen, and the individual health status (Decuypere et al., 2012DECUYPERE, S., VANAERSCHOT, M., BRUNKER, K., IMAMURA, H., MÜLLER, S., KHANAL, B., RIJAL, S., DUJARDIN, J.-C. and COOMBS, G.H., 2012. Molecular mechanisms of drug resistance in natural Leishmania populations vary with genetic background. PLoS Neglected Tropical Diseases, vol. 6, no. 2, p. e1514. http://dx.doi.org/10.1371/journal.pntd.0001514. PMid:22389733.
http://dx.doi.org/10.1371/journal.pntd.0...
).
Taken together, higher prevalence has been observed in study population and the number of cases is rising all the year around, especially in winter season. All the leishmanial lesions were confined to the patient skin and mucosal membrane with no other tissue involvement noticed. The SSG regimen proved effective in treating 97% cases. A large-scale national level epidemiological studies are needed to estimate its exact prevalence throughout the country and to combat this disease.
References
- ABUZAID, A.A., ABDOON, A.M., ALDAHAN, M.A., ALZAHRANI, A.G., ALHAKEEM, R.F., ASIRI, A.M., ALZAHRANI, M.H. and MEMISH, Z.A., 2017. Cutaneous leishmaniasis in Saudi Arabia: a comprehensive overview. Vector Borne and Zoonotic Diseases, vol. 17, no. 10, pp. 673-684. http://dx.doi.org/10.1089/vbz.2017.2119 PMid:28806141.
» http://dx.doi.org/10.1089/vbz.2017.2119 - AFGHAN, A.K., KASSI, M., KASI, P.M., AYUB, A., KAKAR, N. and MARRI, S.M., 2011. Clinical manifestations and distribution of cutaneous leishmaniasis in Pakistan. Journal of Tropical Medicine, vol. 2011, p. 359145. http://dx.doi.org/10.1155/2011/359145 PMid:22174721.
» http://dx.doi.org/10.1155/2011/359145 - AKILOV, O.E., KHACHEMOUNE, A. and HASAN, T., 2007. Clinical manifestations and classification of Old World cutaneous leishmaniasis. International Journal of Dermatology, vol. 46, no. 2, pp. 132-142. http://dx.doi.org/10.1111/j.1365-4632.2007.03154.x PMid:17269962.
» http://dx.doi.org/10.1111/j.1365-4632.2007.03154.x - AMIN, T.T., AL-MOHAMMED, H.I., KALIYADAN, F. and MOHAMMED, B.S., 2013. Cutaneous leishmaniasis in Al Hassa, Saudi Arabia: epidemiological trends from 2000 to 2010. Asian Pacific Journal of Tropical Medicine, vol. 6, no. 8, pp. 667-672. http://dx.doi.org/10.1016/S1995-7645(13)60116-9 PMid:23790342.
» http://dx.doi.org/10.1016/S1995-7645(13)60116-9 - BOUSSLIMI, N., AOUN, K., BEN-ABDA, I., BEN-ALAYA-BOUAFIF, N., RAOUANE, M. and BOURATBINE, A., 2010. Epidemiologic and clinical features of cutaneous leishmaniasis in southeastern Tunisia. The American Journal of Tropical Medicine and Hygiene, vol. 83, no. 5, pp. 1034-1039. http://dx.doi.org/10.4269/ajtmh.2010.10-0234 PMid:21036833.
» http://dx.doi.org/10.4269/ajtmh.2010.10-0234 - CHAVES, L.F. and PASCUAL, M., 2006. Climate cycles and forecasts of cutaneous leishmaniasis, a nonstationary vector-borne disease. PLoS Medicine, vol. 3, no. 8, p. e295. http://dx.doi.org/10.1371/journal.pmed.0030295 PMid:16903778.
» http://dx.doi.org/10.1371/journal.pmed.0030295 - DECUYPERE, S., VANAERSCHOT, M., BRUNKER, K., IMAMURA, H., MÜLLER, S., KHANAL, B., RIJAL, S., DUJARDIN, J.-C. and COOMBS, G.H., 2012. Molecular mechanisms of drug resistance in natural Leishmania populations vary with genetic background. PLoS Neglected Tropical Diseases, vol. 6, no. 2, p. e1514. http://dx.doi.org/10.1371/journal.pntd.0001514 PMid:22389733.
» http://dx.doi.org/10.1371/journal.pntd.0001514 - FARAHMAND, M., NAHREVANIAN, H., SHIRAZI, H.A., NAEIMI, S. and FARZANEHNEJAD, Z., 2011. An overview of a diagnostic and epidemiologic reappraisal of cutaneous leishmaniasis in Iran. The Brazilian Journal of Infectious Diseases, vol. 15, no. 1, pp. 17-21. http://dx.doi.org/10.1016/S1413-8670(11)70134-9 PMid:21412584.
» http://dx.doi.org/10.1016/S1413-8670(11)70134-9 - FRANKE, E.D., WIGNALL, F.S., CRUZ, M.E., ROSALES, E., TOVAR, A.A., LUCAS, C.M., LLANOS-CUENTAS, A. and BERMAN, J.D., 1990. Efficacy and toxicity of sodium stibogluconate for mucosal leishmaniasis. Annals of Internal Medicine, vol. 113, no. 12, pp. 934-940. http://dx.doi.org/10.7326/0003-4819-113-12-934 PMid:2173461.
» http://dx.doi.org/10.7326/0003-4819-113-12-934 - HAOUAS, N., AMER, O., ISHANKYTY, A., ALAZMI, A. and ISHANKYTY, I., 2015. Profile and geographical distribution of reported cutaneous leishmaniasis cases in northwestern Saudi Arabia, from 2010 to 2013. Asian Pacific Journal of Tropical Medicine, vol. 8, no. 4, pp. 287-291. http://dx.doi.org/10.1016/S1995-7645(14)60332-1 PMid:25975500.
» http://dx.doi.org/10.1016/S1995-7645(14)60332-1 - HAWASH, Y.A., ISMAIL, K.A., ABDEL-WAHAB, M.M. and KHALIFA, M., 2018. Diagnosis, treatment and clinical features of cutaneous leishmaniasis in Saudi Arabia. Korean Journal of Parasitology, vol. 56, no. 3, pp. 229-236. http://dx.doi.org/10.3347/kjp.2018.56.3.229 PMid:29996626.
» http://dx.doi.org/10.3347/kjp.2018.56.3.229 - KHAN, N.H., BARI, A., HASHIM, R., KHAN, I., MUNEER, A., SHAH, A., WAHID, S., YARDLEY, V., O’NEIL, B. and SUTHERLAND, C.J., 2016. Cutaneous leishmaniasis in Khyber Pakhtunkhwa province of Pakistan: clinical diversity and species-level diagnosis. The American Journal of Tropical Medicine and Hygiene, vol. 95, no. 5, pp. 1106-1114. http://dx.doi.org/10.4269/ajtmh.16-0343 PMid:27601518.
» http://dx.doi.org/10.4269/ajtmh.16-0343 - MUMTAZ, S., MUNIR, A.H., ASGHAR, M. and NAHEED, N., 2016. Frequency and types of leishmaniasis in Khyber Pakhtunkhwa (KPK). Journal of Medical Sciences, vol. 24, pp. 136-140.
- POSTIGO, J.A.R., 2010. Leishmaniasis in the world health organization eastern mediterranean region. International Journal of Antimicrobial Agents, vol. 36, suppl. 1, pp. S62-S65. http://dx.doi.org/10.1016/j.ijantimicag.2010.06.023 PMid:20728317.
» http://dx.doi.org/10.1016/j.ijantimicag.2010.06.023 - SAAB, M., HAGE, H., CHARAFEDDINE, K., HABIB, R.H. and KHALIFEH, I., 2015. Diagnosis of cutaneous leishmaniasis: why punch when you can scrape? The American Journal of Tropical Medicine and Hygiene, vol. 92, no. 3, pp. 518-522. http://dx.doi.org/10.4269/ajtmh.14-0512 PMid:25561563.
» http://dx.doi.org/10.4269/ajtmh.14-0512 - TORRES-GUERRERO, E., QUINTANILLA-CEDILLO, M.R., RUIZ-ESMENJAUD, J. and ARENAS, R., 2017. Leishmaniasis: a review. F1000 Research, vol. 6, p. 750. http://dx.doi.org/10.12688/f1000research.11120.1 PMid:28649370.
» http://dx.doi.org/10.12688/f1000research.11120.1 - WORLD HEALTH ORGANIZATION – WHO, 2010. Control of the leishmaniases: report of a meeting of the WHO Expert Commitee on the Control of Leishmaniases, Geneva, 22-26 March 2010 Geneva: WHO. WHO Technical Report Series.
- WORLD HEALTH ORGANIZATION – WHO, 2019. Global leprosy update, 2018: moving towards a leprosyfree world. Weekly Epidemiological Record, vol. 94, no. 35-36, pp. 389-412.
- WORTMANN, G., MILLER, R.S., OSTER, C., JACKSON, J. and ARONSON, N., 2002. A randomized, double-blind study of the efficacy of a 10-or 20-day course of sodium stibogluconate for treatment of cutaneous leishmaniasis in United States military personnel. Clinical Infectious Diseases, vol. 35, no. 3, pp. 261-267. http://dx.doi.org/10.1086/341406 PMid:12115091.
» http://dx.doi.org/10.1086/341406 - ZAKAI, H.A., 2014. Cutaneous leishmaniasis in Saudi Arabia: current status. Journal of Advanced Laboratory Research in Biology, vol. 5, no. 2, pp. 29-35.
Publication Dates
-
Publication in this collection
08 Aug 2022 -
Date of issue
2024
History
-
Received
25 Feb 2021 -
Accepted
22 July 2021