Abstracts
This study evaluated the prevalence of nontuberculous mycobacterium (NTM) in relation to the total number of cases of mycobacterial infections detected in patients admitted at the University Hospital of Santa Maria from 2008 to 2010. From the positive samples for the genus Mycobacterium, 67% belonged to the Mycobacterium tuberculosis complex (MTBC) and 33% of them were classified as NTM. This investigation aims to contribute to the epidemiology of mycobacterioses, inasmuch as patients infected by NTM require distinctive treatment and monitoring in comparison with those infected by MTBC.
nontuberculous mycobacteria; Mycobacterium tuberculosis; classification; phenotyping; South of Brazil
Foi avaliada a prevalência de micobactérias não tuberculosas (MNT) em relação ao total de casos de micobacterioses identificadas em pacientes do Hospital Universitário de Santa Maria, entre os anos de 2008 e 2010. Entre as amostras positivas para o gênero Mycobacterium, 67% eram do complexo Mycobacterium tuberculosis (CMTB) e 33% foram classificadas como MNT. Este estudo procura contribuir com a epidemiologia das micobacterioses, uma vez que os pacientes infectados por MNT necessitam de tratamento e acompanhamento diferenciado dos infectados pelo CMTB.
micobactéria não tuberculosa; Mycobacterium tuberculosis; classificação; fenotipagem; Sul do Brasil
LABORATORY MEDICINE
BRIEF COMMUNICATION
Identification of mycobacteria isolated at University Hospital of Santa Maria, Rio Grande do Sul, Brazil
Identificação de micobactérias isoladas no Hospital Universitário de Santa Maria, Rio Grande do Sul, Brasil
Vanessa Albertina AgerttI; Tanise Vendruscolo DalmolinII; Pauline Cordenonsi BonezIII; Caren Rigon MizdalIII; Jaciane Baggiotto MarquesIII; Vanessa da Costa FloresIV; Adelinde SallaV; Marli Matiko Anraku de CamposVI
IMaster's degree in Pharmaceutical Sciences; attending post-graduation in Pharmaceutical Sciences at Universidade Federal de Santa Maria (UFSM)
IIGraduating student in Pharmacy at UFSM
IIIPharmacist; attending post-graduation in Pharmaceutical Sciences at UFSM
IVPharmacist; specialist in Clinical and Laboratory analysis; attending post-graduation in Pharmaceutical Sciences at UFSM
VPharmacist at the Clinical Analysis Laboratory from University Hospital of Santa Maria
VIDoctor in Pharmacy (Clinical Analysis); associate professor at UFSM
Correspondence Mailing address Vanessa Albertina Agertt Avenida Roraima, 1000, Camobi; CEP: 97105-970; Santa Maria-RS, Brazil; e-mail: vaagertt@gmail.com.
ABSTRACT
This study evaluated the prevalence of nontuberculous mycobacterium (NTM) in relation to the total number of cases of mycobacterial infections detected in patients admitted at the University Hospital of Santa Maria from 2008 to 2010. From the positive samples for the genus Mycobacterium, 67% belonged to the Mycobacterium tuberculosis complex (MTBC) and 33% of them were classified as NTM. This investigation aims to contribute to the epidemiology of mycobacterioses, inasmuch as patients infected by NTM require distinctive treatment and monitoring in comparison with those infected by MTBC.
Key words: nontuberculous mycobacteria; Mycobacterium tuberculosis; classification; phenotyping; South of Brazil.
RESUMO
Foi avaliada a prevalência de micobactérias não tuberculosas (MNT) em relação ao total de casos de micobacterioses identificadas em pacientes do Hospital Universitário de Santa Maria, entre os anos de 2008 e 2010. Entre as amostras positivas para o gênero Mycobacterium, 67% eram do complexo Mycobacterium tuberculosis (CMTB) e 33% foram classificadas como MNT. Este estudo procura contribuir com a epidemiologia das micobacterioses, uma vez que os pacientes infectados por MNT necessitam de tratamento e acompanhamento diferenciado dos infectados pelo CMTB.
Palavras-chave: Unitermos: micobactéria não tuberculosa; Mycobacterium tuberculosis; classificação; fenotipagem; Sul do Brasil.
Introduction
The genus Mycobacterium comprises species from the mycobacterium tuberculosis complex (MTBC) and other species denominated nontuberculous mycobacterium (NTM)(8). The protocols for tuberculosis treatment (TB) and infections caused by NTM differ from each other. Thus, the differential diagnosis of tuberculosis and NTM is crucial in order to establish a suitable treatment(5, 15).
In countries with low or average income levels, in which over 90% of the cases of TB occur, the diagnosis is reached through acid-alcohol resistant bacilli smear(12). To date, the diagnosis that confirms tuberculosis is conducted through culture of lesion sample with isolation and identification of the bacilli(2). Several laboratories do not perform this identification procedure due to the lack of resources to apply molecular techniques or the considerable time allocated for phenotypic methods. This study is based on patients admitted at the University Hospital of Santa Maria (UHSM), which currently does not conduct the differential diagnosis of mycobacterioses as standard procedure, but exclusively in cases of treatment failure. Therefore, the objective of the present research was to assess the prevalence of NTM in relation to the total number of cases of identified mycobacterium in patients admitted at the UHSM from 2008 to 2010.
Methods
This study was conducted with positive samples for mycobacterium detected through AARB analysis and originally from the clinical analysis laboratory of the University Hospital of Santa Maria (UHSM), located in Santa Maria, RS, Brazil, from January 2008 to December 2010. The information on the positive samples included gender, isolated site and results from sputum smear and culture. Both procedures were routinely applied by the CAL-UHSM and standardized according to the guidelines described in the Bacteriology Manual of Tuberculosis proposed by the Ministry of Health(4).
171 pulmonary and extra-pulmonary positive samples for mycobacterium were categorized by phenotypic methods. The classification of NTM and MTBC was carried out at the Mycobacteriology laboratory of the Clinical and Toxicological Analysis Department of UFSM in order to assess growth time, pigment production and growth in the presence of inhibitor agent(4). The Certificate for Ethical Appreciation (Certificado de Apresentação para Apreciação ética [CAAE]) number 0104.0.243.000-11 was issued and the research project was submitted to the Ethics Committee in Research from UFSM.
Results
The mycobacterium were classified into four groups:
I - photochromogenic;
II - scotochromogenic;
III - non-chromogenic;
IV - rapid growth.
The specimens identified as group III were isolated from M. tuberculosis complex through susceptibility to para-aminobenzoic acid (PABA).
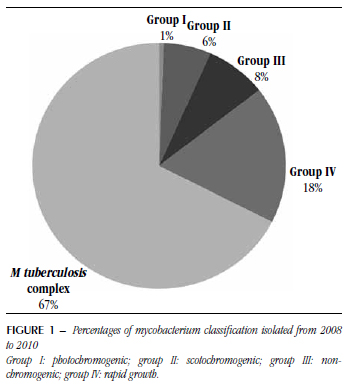
4,603 samples were analyzed herein, from which 194 were positive for smear and culture. From the positive samples for Mycobacterium, 67% were from M. tuberculosis complex and 33% of them were classified as NTM, as shown in Figure 1.
70% of 194 samples of isolated bacterium were from male patients, from which 67% were from MTBC and 33% were NTM. In NTM isolates, 70% were from male patients. In Figure 2, the occurrence of MTBC and NTM is demonstrated in relation to the isolation sites of positive samples.
Discussion
The clinically significant species of the genus Mycobacterium have doubled in the last 15 years(9). As mycobacterioses are not mandatorily notified in Brazil, the high incidence of these diseases reported in some studies is not corroborated by official records(3). The investigations in this area are scarce and the available ones differ as to the analyzed population and type of clinical sample, hence the difficulty in comparing yielded results(16).
From the studies that revealed the percentage of NTM, those conducted in Rio de Janeiro(7, 14) yielded results similar to the present investigation (33%), with 45% and 34.3% of NTM(1). However, they were carried out from 2000 to 2002. A more recent study was conducted in São José do Rio Preto-SP from 1996 to 2005(13), which showed the incidence of 24.4% of NTM, corroborating our results.
According to Matos et al.(10), a study developed in Bahia-Brazil evinced a higher prevalence of NTM among male patients (68.4%), which was also confirmed herein (70%). However, the percentage of NTM isolated from 1998 to 2003 was 8.2%, contrasting with our study (33%). This discrepancy may have occurred owing to the fact that more accurate procedures for the differentiation of colonies infected by NTM were applied in this investigation such as the use of criteria proposed by the American Thoracic Society (ATS)(6). The fact that cases of contamination or colonization were not assessed may have contributed to the overestimation of prevalence values, hence the importance of evaluating both laboratory and clinical findings. The different incidences surveyed herein, including the research group, may have arisen due to the fact that the study was carried out with respiratory and other site samples, which had not occurred in all cited studies. Another plausible explanation is the geographic distribution of NMT species in such a large country as Brazil with several environmental factors(1, 11), which also justifies the age differences in the studied population. Older individuals are prone to preexisting pulmonary diseases, which is a major factor in colonization and/or NMT infection.
Studies solely based on NMT classification (Figure 1) without the identification of the corresponding species were not found, which hindered comparisons. Notwithstanding, as the objective of the present investigation was to raise awareness about the existence of NMT in the region of Santa Maria, we believe this goal was achieved as demonstrated by the yielded results. There were no differences between the type of sample in which MTBC bacilli and NMT were isolated, although there was a higher occurrence in the sputum samples. This result may account for the fact that this kind of sample is common among medical investigations, inasmuch as it is not an invasive procedure.
In spite of the study limitations, we may conclude that the prevalence of NMT at UHSM is high and may be responsible for the treatment failure among some patients with only MTBC. This study contributes to the epidemiology of mycobacterioses, insofar as patients infected by NMT require distinctive treatment and monitoring in comparison with those infected by MTBC.
First submission on 26/06/12;
last submission on 13/12/12;
accepted for publication on 17/01/13;
published on 20/04/13
- 1. BARRETO, A. M. W.; CAMPOS, C. E. D. C. Micobactérias não tuberculosas no Brasil. Bol Pneumo San, v. 8, p. 23-32, 2000.
-
2BRASIL. Ministério da Saúde. Secretaria de Vigilância em Saúde. Centro de referência Professor Hélio Fraga. Sociedade Brasileira de Pneumologia e Tisiologia. Controle da tuberculose: uma proposta de integração ensino-serviço 5. ed. Rio de Janeiro: FUNASA/CRPHF/SBPT, 2002. Disponível em: <http://www.saude.mt.gov.br/upload/documento/81/controle-da-tuberculose-uma-proposta-de-integracao-ensino-servico-%5B81-080909-SES-MT%5D.pdf>. Acesso em: jun. 2012.
-
3BRASIL. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Manual nacional de vigilância laboratorial da tuberculose e outras micobactérias/Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Vigilância Epidemiológica. Brasília: Ministério da Saúde, 2008. 436 p.
-
4______. Ministério da Saúde. Secretaria de Vigilância em Saúde. Programa Nacional de Controle da Tuberculose. Manual de Recomendações para o Controle da Tuberculose no Brasil, 2010. Disponível em: <http://portal.saude.gov.br/portal/arquivos/pdf/manual_tuberculose.pdf>. Acesso em: jun. 2012.
- 5. ______. Secretaria Estadual da Saúde. Coordenadoria de Controle de Doenças. Micobacterioses: recomendações para o diagnóstico e tratamento. São Paulo: Secretaria Estadual da Saúde de São Paulo, 2005. Disponível em: . Acesso em: jun. 2012.
-
6_______. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Medical Section of the American Lung Association. Am J Respir Crit Care Med, v. 156, p. 1-25, 1997. Disponível em: <http://www.ncbi.nlm.nih.gov/pubmed/9279284>. Acesso em: jun. 2012.
- 7. FERREIRA, R. M. et al. Non-tuberculous mycobacteria I: one year clinical isolates identification in Tertiary Hospital Aids Reference Center, Rio de Janeiro, Brazil, in pre highly active antiretroviral therapy era. Mem Inst Oswaldo Cruz, v. 97, n. 5, p.725-9, 2002.
- 8. GRIFFITH, D. E.; AKSAMIT, T.; BROWN-ELLIOTT, B. A. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med, v. 175, n. 4, p. 367-416, 2007.
- 9. HALL, L.; ROBERTS, G. D. Non-molecular identification of nontuberculous mycobacteria in the clinical microbiology laboratory: What's the real deal? Clin Microbiol News, v. 28, n. 10, p. 73-80, 2006.
- 10. MATOS, E. D. et al. Nontuberculosis mycobacteria at a multiresistant tuberculosis reference center in Bahia: Clinical epidemiological aspects. Brazilian J Infec Dis, v. 8, n. 4, p. 296-304, 2004.
- 11. O'BRIEN, R. J.; GEITER, L. J.; SNIDER, D. E. The epidemiology of nontuberculous mycobacterial diseases in the United States. Results from a national survey. Am Rev Respir Dis, v. 135, p. 1007-14, 1987.
- 12. PAI, M.; KALANTRI, S.; DHEDA, K. New tools and emerging technologies for the diagnosis of tuberculosis. Part II. Active tuberculosis and drug resistance. Expert Rev Mol Diagn, v. 6, p. 423-42, 2006.
- 13. PEDRO, H. S. P. et al. Nontuberculous mycobacteria isolated in São José do Rio Preto, Brazil between 1996 and 2005. J Bras Pneumol, v. 34, n. 11, p. 950-5, 2008.
- 14. SENNA, S. G. et al. Identificação e análise de MNTs causadoras de infecção no Hospital Universitário - HUCFF/UFRJ no Rio de Janeiro. J Bras Pneumol, v. 32, n. 3, p. 135-58, 2006.
- 15. SONG, S. et al. Electrospray ionization-tandem mass spectrometry analysis of the mycolic acid profiles for the identification of common clinical isolates of mycobacterial species. J Microbiol Method, v. 77, p. 165-177, 2009.
- 16. UEKI, S. Y. et al. Micobactérias não tuberculosas: diversidade das espécies no estado de São Paulo. J Bras Patol Med Lab, v. 41, n. 1, p. 1-8, 2005.
Publication Dates
-
Publication in this collection
24 June 2013 -
Date of issue
Apr 2013
History
-
Received
26 June 2012 -
Accepted
17 Jan 2013 -
Reviewed
13 Dec 2012