ABSTRACT
Ménétrier's disease (MD) is included in the group of hypertrophic gastropathy; is a rare gastric hyperplasia that affects adults and children, with different behavior between these groups. We know that its etiology is related to allergens and co-infections. It's characterized by the hypertrophy of the gastric folds, with the appearance of cerebral convolutions on Upper Gastrointestinal Endoscopy (UGE) and, histologically, by the mucosal hypertrophy at the expense of foveolar hyperplasia and atrophy of the glands in body and fundus of the stomach. The UGE together with the gastric tissue biopsy confirms the diagnosis. What concerns us in the following case, however, is patient's long-lasting evolution, about eight years.
Key words:
pediatrics; gastropathy; endoscopy of the gastrointestinal tract; gastroenterology; histology
RESUMO
Inclui-se a doença de Ménétrier (DM) no grupo das gastropatias hipertóficas, sendo uma hiperplasia gástrica rara que acomete adultos e crianças, com comportamento distinto entre esses grupos. Sabemos que sua etiologia relaciona-se com alérgenos e coinfecções. Caracteriza-se pela hipertrofia das pregas gástricas, com aspecto de circunvoluções cerebrais à endoscopia digestiva alta (EDA) e, histologicamente, pelo alargamento da mucosa às custas de hiperplasia foveolar e hipotrofia das glândulas em corpo e fundo gástrico. A EDA, junto à biópsia gástrica, confirma o diagnóstico. O que nos intriga no caso a seguir é o tempo evolução arrastado da paciente, cerca de oito anos.
Unitermos:
pediatria; gastropatias; endoscopia do sistema digestório; gastroenterologia; histologia
INTRODUCTION
Ménétrier disease (MD) is a rare hyperplastic gastropathy, most commonly in the pediatric setting, observed in children under ten years of age. Described by Pierre Ménétrier in 1888, it was associated with protein loss and hypochlorhydria(11 Feldman M, Friedman LS, Brandt LJ. Sleisenger and Fortran's gastrointestinal and liver disease. vol. 1. 2006 ed. Philadelphia: Saunders Elsevier. pp. 557-63, 633-8, 1082-1083.). The clinical presentation is acute, and the patient may present weight loss, epigastralgy, nausea, vomiting, bleeding and diarrhea(22 Zeitune J, Monici L. Gastrites. Rev Bras Med. 2000; 57(12): 33-43.). At least 20% of the patients have protein-losing gastropathy with hypoalbuminemia(33 Komorowski RA, Caya JG. Hyperplastic gastropathy. Clinicopathologic correlation. Am J Surg Pathol. 1991 Jun; 15(6): 577-85. PubMed PMID: 2031530.), with subsequent edema in more than 90% of the cases, and varying severity(44 Dolores F, Bettencourt JD, Mendes A. Gastropatia hipertrófica exsudativa associada a infecção aguda a citomegalovirus. Rev Port Doenças Infecciosas. 1994; 7: 243-5.).
The disease is rare in children(55 Lambrecht NW. Ménétrier's disease of the stomach: a clinical challenge. Curr Gastroenterol Rep. 2011; 13: 513-7.), is more common in male and has a benign self-limiting course(66 Barberán AC, Hubrecht AS, Abás AH, Roig JR, Gratacós JM, Navarro JAI. Enfermedad de Ménétrier infantil e infección aguda por citomegalovirus. An Pediatr (Barc). 2006 Jan; 64(5): 478-80.). Its etiology is still not well understood, but it is known to include allergic, immunological, and infectious factors, with its development in some patients. The association with cytomegalovirus (CMV) infection is described in about 30% of the individuals affected(77 Proujansky R. Protein-losing enteropathy. In: Walker WA, Goulet O, Kleinman RE, Sherman PM, Shneider BL, Sanderson IR, editors. Pediatric gastrointestinal disease - pathophysiology, diagnosis, management. 4th ed. Canada, BC: Decker; 2004. p. 194-200.). Fieber(88 Fieber SS. Hypertrophic gastrites: report of two cases and analysis of fifty pathologically verified cases from literature. Gastroenterology. 1955; 28: 39-69. PubMed PMID: 13232174.), in 1955, listed a number of possible agents that would contribute to the pathophysiology of the disease and concluded that allergy was the most common in the cases evaluated in his study. H. pylori co-infection is also associated with MD by causing a rare gastric mucosal response to this aggression, impacting a prominent gastric foveolar proliferative phenomenon.
The diagnosis of MD is based on patient's clinical presentation, in which the initial approach is given by upper gastrointestinal endoscopy (UGE), whose role is to rule out other differential diagnoses, such as lymphomas and initial cancer and other infiltrative inflammatory diseases that may result in nonspecific gastric wall thickening, and therefore, the histopathological study of the gastric mucosa is confirmatory for the diagnosis.
Unlike in pediatric patients, in the adult, a clinical form of chronic evolution predominates, whose gastrectomy as a treatment is much more common than in children(99 Scharschimidt BF. The natural history of hypertrophic gastropathy (Ménétrier disease): report of a case with 16 years follow up and review of 120 cases from the literature. Am J Med. 1977; 63: 644-52.). Whereas in a pediatric approach, its evolution is mostly benign, with spontaneous healing using symptomatic medication, such as ranitidine(1010 Kang JY, Tang KF, Goh A, Sundran FX, Seah CS. Remission of Ménétrier's disease associated with ranitidine administration. Aust N Z J Med. 1990; 20: 716-7.).
The purpose of this article is to report a case of MD in pediatrics, in which the peculiarity occurs in the long-lasting of evolution of the disease in the patient in question, about 8 years, something unusual when treating this disease in children, emphasizing clinical, endoscopic and anatomopathological aspects, as well as echo-ultrasonography, as complementary propaedeutic, including current comments on the therapeutic approach.
CASE REPORT
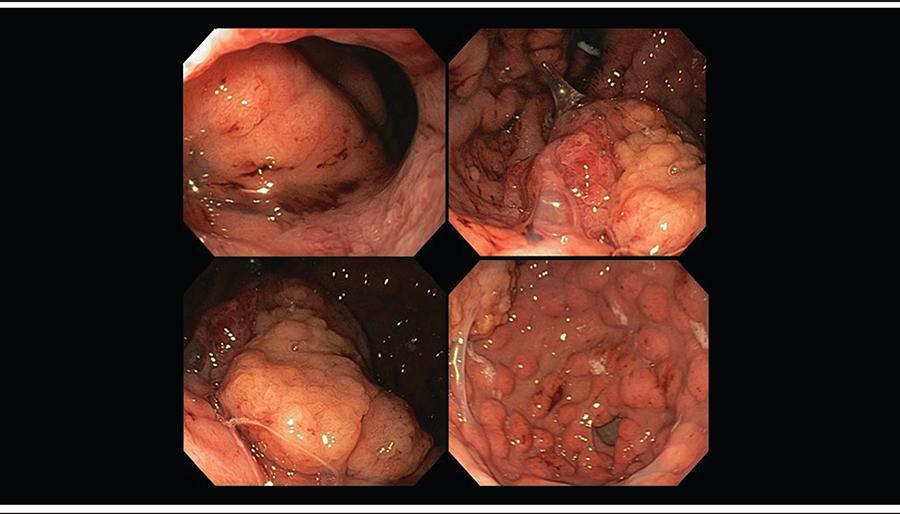
A female patient, born in Taubaté (SP) and from Teófilo Otoni (MG), 16 years old, report, at the age of 8 years, the onset of episodes of epigastric discomfort associated with intermittent nausea, vomiting and anasarca. The UGE performed in the city of origin at the age of 10 years showed giant hypertrophic gastritis with positive urease test, and the patient was treated for Helicobacter pylori infection. She was referred to the Gastroenterology Department of the Hospital das Clínicas of the Universidade Federal de Minas Gerais (UFMG) at age of 13 years for progressive control of the disease. Laboratory tests include 3.49 g/dl albumin [reference value (RV) 3.5 to 5 g/dl]; 13.4 g/dl hemoglobin (RV 11.5 to 14.8), 186 pg/ml vitamin B12 (RV 239 to 931 pg/ml) and serology for CMV with immunoglobulin class G (IgG) positive and class M (IgM) negative, asymptomatic, and no other changes on physical examination. The UGE showed hypertrophic gastric folds, clear mucoid gastric content in moderate quantity and voluminous polypoid formation, with irregular limits, with irregular and pale surface, friable at the touch of the endoscope and with softened consistency, located in the small curvature, close to the transition body-antrum, extending from the angular incisure to the greater curvature. In the other segments of the gastric body and fundus were observed important edema and enanthema, enlarged folds and several polyps up to 8 mm, with a regular reddish surface (Figure 1).
Overview of the body and fundus of the stomach, with hypertrophy of gastric folds, mucosal congestion and swelling, with presence of mucus
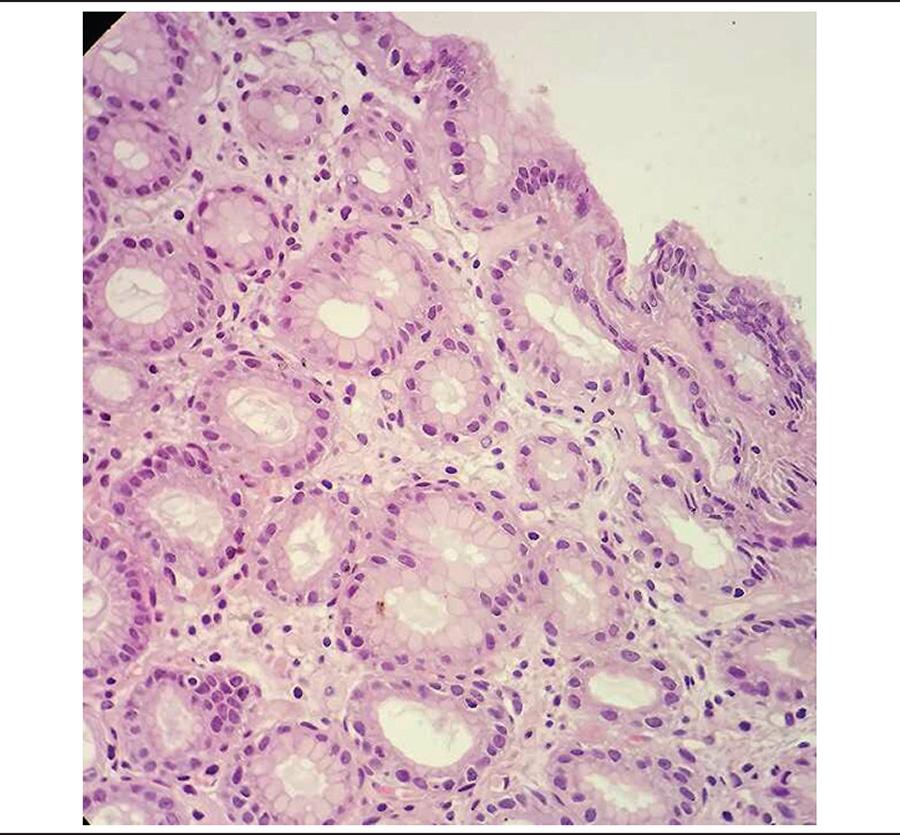
The histological study of the endoscopic biopsies demonstrated in the hyperplastic polypoid lesion the presence of foveolar hyperplasia cystically dilated, associated with a discrete mononuclear inflammatory infiltrate in the lamina propria, with no evidence of malignancy; atrophy of oxyntic glands and the remainder of the gastric mucosa presenting exuberant foveolar hyperplasia and discrete mononuclear inflammatory infiltrate in the lamina propria. The search for Helicobacter pylori was negative. The histological diagnosis was MD (Figure 2). The histological architecture of the gastric body in MD differs greatly when compared to that of the normal gastric body (Figure 3).
Body of the stomach affected by Ménétriér disease; hyperplasia of the gastric foveolar epithelium with mononuclear inflammatory infiltrates in the lamina propria and atrophy of oxyntic glands
Subsequent echoendoscopy had been performed as a complementary propaedeutic procedure in order to rule out other possible differential diagnoses or associated diseases, considering the patient's evolution of eight years, uncommon in MD cases (Figure 4).
High echoendoscopy evidencing polypoid lesion in the transitional body-antrum gastric zone and diffuse thickening of gastric folds with anechoic mucous cysts
A subsequent echoendoscopy was performed as a complementary propaedeutic in order to rule out other possible differential diagnoses or associated diseases, considering the 8-year evolution of the disease, uncommon in cases of MD.
Echoendoscopy showed a marked thickening of the entire gastric wall, which measured 12 mm, mainly the mucous layer (8 mm), which is hypoechoic, with the presence of several cysts measuring 5 to 10 mm (normal wall thickness is up to 5 mm). The stratification of the gastric wall was preserved, with the submucosa and muscular layers identified. The gastric wall thickening was diffuse, from the cardia to the pylorus. The polypoid lesion measured, in its largest extensions, 5 × 3 cm with heterogeneous appearance. It is worth noting that it is another interesting aspect of the case, since cystic formations, such as those observed, are not typical of Ménétriér hypertrophic gastropathy.
The propaedeutic feature of the echoendoscopy assumes an important role in the case because of its atypical and long-lasting presentation (about 8 years), and is indicated as a complementary propaedeutic(1111 Andrade CS, Poças FC, Lago P, Soares J, Areias J. Pregas gástricas hipertróficas: doença de Ménétrier. J Port Gastrenterol. 2009; 16(1): 33-4.), with findings as MD when revealing a localized, hyperechoic mucosal layer thickening and/or one or more gastric folds of thickness greater than 10 mm, however the UGE and the anatomopathological study are the gold standard for the diagnosis of the disease.
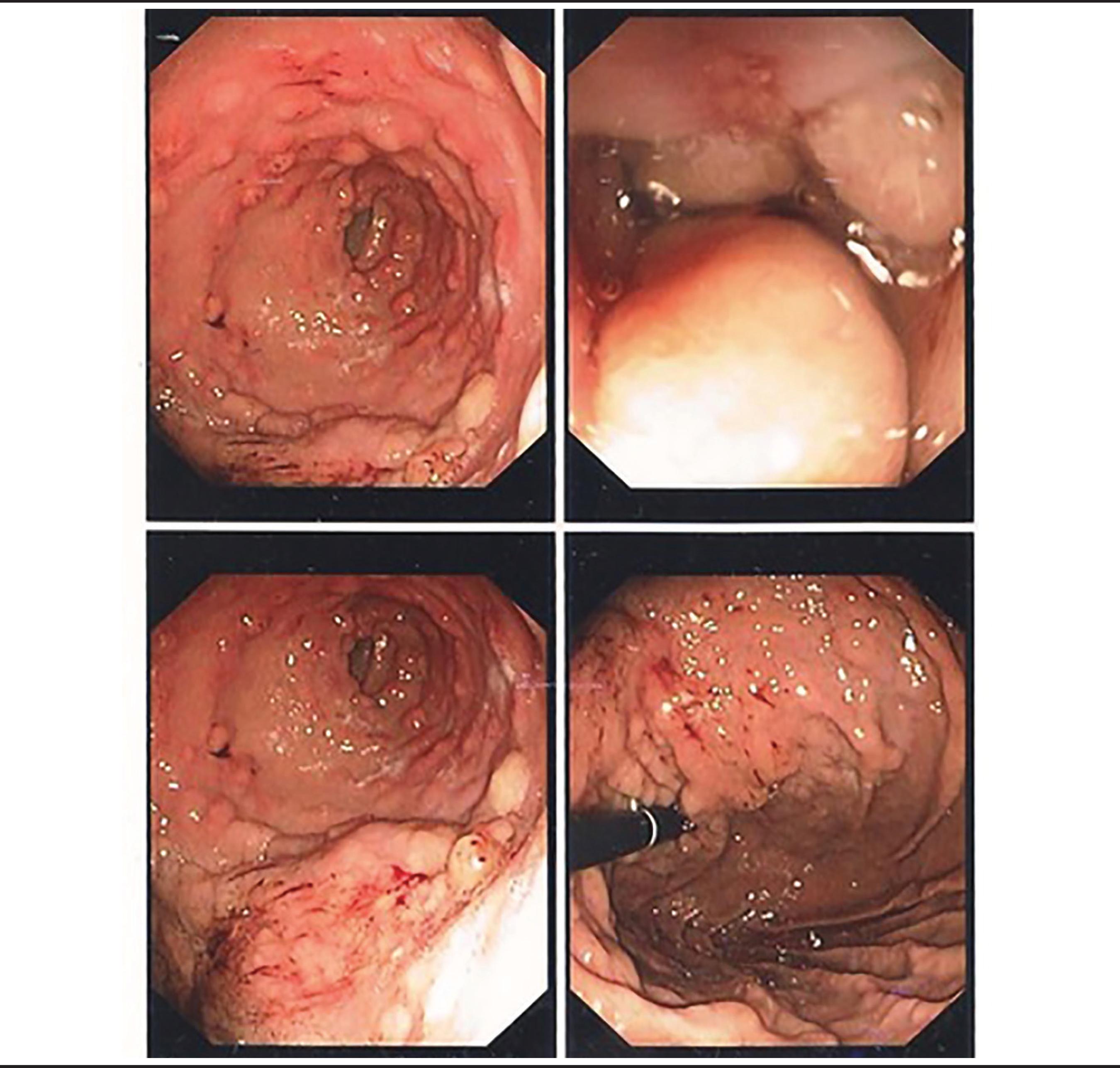
Even with the evolution of the disease for around 8 years, no specific therapeutic measures were performed and, due to the asymptomatic condition, the normal physical examination and the treatments used in the case of MD, therefore, a conservative approach was adopted, with endoscopic follow-up with a new UGE performed six months later aiming to control the disease, which showed diffuse the gastric folds thickening and elevated lesion in the body-antrum transition, consistent with the previous endoscopic findings (Figure 5) with no histopathological changes. Conservative management was maintained due to the permanence of patient's clinical stability, with no physical or symptomatic changes, with endoscopic follow-up in six months, with no specific therapeutic measures.
Control gastrointestinal endoscopy evidencing hypertrophy of gastric mucosa folds, diffuse polypoid lesions and elevated lesion in body-antrum transitional zone
DISCUSSION
The diagnosis of MD is based on clinical data, notably hypoalbuminemia, associated with the presence of thickened gastric folds found in the UGE, with compatible biopsies. Associations with Helicobacter pylori infection, as observed in the patient, allergic processes and medications acting on E2 prostaglandin molecules may be related to the disease, and the CMV coinfection should be considered in pediatric cases with MD, mainly in those who present abrupt gastrointestinal protein loss(1212 Volonaki E, Haliotis F, Vliet-Constantinidou C, Avlonitis S, Roma E. Cytomegalovirus infection in a child with Menetrier's disease: a case report. Ann Gastroenterol. 2007; 20(3): 223-5.), although several pathophysiological mechanisms are involved in the disease. Rare cases have been described in which the diagnosis was defined by the identification of inclusion bodies in gastric tissue biopsies, suggesting an association of the infant form with CMV infection(1313 Coad NAG, Shah KJ. Menetrier's disease in childhood associate with cytomegalovirus infection: a case report and review of the literature. Br J Radiol. 1986 Oct; 59(702): 615-20.). It is known, however, that the observation of cytomegalic inclusion bodies comprises neither the only possibility nor the most sensitive, when compared with other CMV diagnostic methods, such as serology and immunohistochemistry.
The most interesting and atypical nuance of the case occurs in the time of evolution, of about eight years, which is quite unusual. In most cases of MD in childhood, the evolution of the disease occurs with spontaneous remission, unlike that observed in the adult patient. The evolution to atrophic gastritis may be the precursor of dysplastic and neoplastic transformations; meanwhile, the evolution for healing and recovery of the mucosa is correlated with absence of symptoms. In the case presented, the gastric mucosa is impaired even with the long-lasting 8-year of evolution, but with no signs of malignancy or dysplasia, and the patient remained asymptomatic.
Hypertrophy of the gastric mucosa, the main characteristic of the disease, occurs by the local increase of the transforming growth factor alpha (TGF-α), the epidermal growth factor receptor (EGFR) and the transforming growth factor-β2(44 Dolores F, Bettencourt JD, Mendes A. Gastropatia hipertrófica exsudativa associada a infecção aguda a citomegalovirus. Rev Port Doenças Infecciosas. 1994; 7: 243-5.) receptor II, which promote the proliferation of gastric epithelial cells and increase mucus secretion rich in proteins, and the proliferation of foveolar epithelium is more prominent in adults than in children. The majority of patients may still have elevated serum levels of immunoglobulin class E (IgE) and moderate eosinophilia, suggesting an allergic response as a predisposing factor and/or possible viral infection(1414 Jacobe S, Lam A, Elliott E. Transient hypertrophic gastropathy. J Pediatr Gastroenterol Nutr. 1998 Feb; 26(2): 211-5.). A percentage of the affected individuals evolve to atrophic gastritis and remission of symptoms. In adults, it is considered a preneoplastic condition. On the other hand, MD in child evolves with spontaneous remission, most of the time. The presence of hyperplastic polyps, as in the case of the patient in question, increases the risk of neoplastic transformation, and 2% to 15% of these lesions are associated with adenocarcinoma in MD. There is no specific pharmacological treatment, but it is known that the use of anticholinergic drugs improves the serum albumin level. The use of rituximab, antibody inhibitor of epidermal growth factor receptor, and corticosteroid therapy has also been shown to be valuable for controlling symptoms. In case of symptomatic persistence, total gastrectomy is indicated(1515 Searcy RM, Malagelada JR. Ménétrier disease and idiopathic hypertrophic gastropathy. Ann Intern Med. 1984 Apr; 100(4): 565-70.).
Faced with this condition of diffuse hypertrophy of the superficial layer of the gastric mucosa, we must consider other diseases as the most probable differential diagnoses for diffuse stomach wall thickening(1616 Souza LRMF, Nogueira JR, Ferme AL, Goldman SM, D'lppolito G, Szejnfeld J. Doença de Ménétrier na infância: relato de caso. Rev Imagem. 2005; 27(3): 213-6.).
In cases of gastric folds thickening observed in the UGE, echoendoscopy may clearly identify the different layers of the gastric wall and evaluate not only the structure of each one, but also determine which ones are involved and complement the endoscopic findings(1717 Gómez, Martín A, Otero R, William, Arbelaez M, Victor, & Rodríguez, Jesús. (2005). Ecoendoscopia: Indicaciones de la A a la Z. Revista Colombiana de Gastroenterologia, 20(2), 34-64. Retrieved March 25, 2017), however, its use is operator-dependent for good visualization of the gastric layers and its use is not determinant to establish the diagnosis of MD, which, as previously stated, has the UGE together with the anatomopathological study as the gold standard.
An interesting perspective of echoendoscopy is that it may also exclude a thickening of vascular origin and thus, avoiding biopsies that would involve a high risk of hemorrhagic complications. The European Society of Gastrointestinal Endoscopy recommends that echoendoscopy precede the biopsy decision in all cases of gastric folds thickening that may suggest the existence of large subepithelial vessels.
Hyperplastic folds and MD tipically present gastric mucosa thickening, whereas malignant diseases, such as lymphomas, compromise all layers of the gastric wall(1818 Rösch T, Classen M. Gastroenterologic. Endosonograpy. New York: Thieme Stuttgart; 1992.). Therefore, some differential diagnoses may be chosen according to the anatomopathological characteristics (Table), however, in pediatric cases, we consider as the main differential diagnosis the hypertrophic gastropathy(1919 Occena RO, Taylor SF, Robinson CC, Sokol RJ. Association of cytomegalovirus with Ménétrier's disease in childhood: report of two new cases with a review of literature. J Pediatr Gastroenterol Nutr. 1993; 17: 217-24.).
CONCLUSION
MD, even though it is an uncommon gastropathy in pediatric patients, is a diagnosis that can not be excluded, due to its repercussion on the patient's quality of life. It is essential to the professional that assists these patients the good knowledge of this disease so as not to neglect therapies and to establish reliability of diagnosis. Thus, knowing the endoscopic presentations of the different hypertrophic gastropathy and their clinical and epidemiological presentation, as well as knowing their anatomopathological aspects, are essential for the pathologist practioner to perform diagnostic biopsies increasingly accurate.
ACKNOWLEDGEMENTS
To the Endoscopy department of the Instituto Alfa de Gastroenterologia of the Hospital das Clínicas at the UFMG and to the department of Pathological Anatomy of the Faculdade de Medicina at the UFMG.
REFERENCES
-
1Feldman M, Friedman LS, Brandt LJ. Sleisenger and Fortran's gastrointestinal and liver disease. vol. 1. 2006 ed. Philadelphia: Saunders Elsevier. pp. 557-63, 633-8, 1082-1083.
-
2Zeitune J, Monici L. Gastrites. Rev Bras Med. 2000; 57(12): 33-43.
-
3Komorowski RA, Caya JG. Hyperplastic gastropathy. Clinicopathologic correlation. Am J Surg Pathol. 1991 Jun; 15(6): 577-85. PubMed PMID: 2031530.
-
4Dolores F, Bettencourt JD, Mendes A. Gastropatia hipertrófica exsudativa associada a infecção aguda a citomegalovirus. Rev Port Doenças Infecciosas. 1994; 7: 243-5.
-
5Lambrecht NW. Ménétrier's disease of the stomach: a clinical challenge. Curr Gastroenterol Rep. 2011; 13: 513-7.
-
6Barberán AC, Hubrecht AS, Abás AH, Roig JR, Gratacós JM, Navarro JAI. Enfermedad de Ménétrier infantil e infección aguda por citomegalovirus. An Pediatr (Barc). 2006 Jan; 64(5): 478-80.
-
7Proujansky R. Protein-losing enteropathy. In: Walker WA, Goulet O, Kleinman RE, Sherman PM, Shneider BL, Sanderson IR, editors. Pediatric gastrointestinal disease - pathophysiology, diagnosis, management. 4th ed. Canada, BC: Decker; 2004. p. 194-200.
-
8Fieber SS. Hypertrophic gastrites: report of two cases and analysis of fifty pathologically verified cases from literature. Gastroenterology. 1955; 28: 39-69. PubMed PMID: 13232174.
-
9Scharschimidt BF. The natural history of hypertrophic gastropathy (Ménétrier disease): report of a case with 16 years follow up and review of 120 cases from the literature. Am J Med. 1977; 63: 644-52.
-
10Kang JY, Tang KF, Goh A, Sundran FX, Seah CS. Remission of Ménétrier's disease associated with ranitidine administration. Aust N Z J Med. 1990; 20: 716-7.
-
11Andrade CS, Poças FC, Lago P, Soares J, Areias J. Pregas gástricas hipertróficas: doença de Ménétrier. J Port Gastrenterol. 2009; 16(1): 33-4.
-
12Volonaki E, Haliotis F, Vliet-Constantinidou C, Avlonitis S, Roma E. Cytomegalovirus infection in a child with Menetrier's disease: a case report. Ann Gastroenterol. 2007; 20(3): 223-5.
-
13Coad NAG, Shah KJ. Menetrier's disease in childhood associate with cytomegalovirus infection: a case report and review of the literature. Br J Radiol. 1986 Oct; 59(702): 615-20.
-
14Jacobe S, Lam A, Elliott E. Transient hypertrophic gastropathy. J Pediatr Gastroenterol Nutr. 1998 Feb; 26(2): 211-5.
-
15Searcy RM, Malagelada JR. Ménétrier disease and idiopathic hypertrophic gastropathy. Ann Intern Med. 1984 Apr; 100(4): 565-70.
-
16Souza LRMF, Nogueira JR, Ferme AL, Goldman SM, D'lppolito G, Szejnfeld J. Doença de Ménétrier na infância: relato de caso. Rev Imagem. 2005; 27(3): 213-6.
-
17Gómez, Martín A, Otero R, William, Arbelaez M, Victor, & Rodríguez, Jesús. (2005). Ecoendoscopia: Indicaciones de la A a la Z. Revista Colombiana de Gastroenterologia, 20(2), 34-64. Retrieved March 25, 2017
-
18Rösch T, Classen M. Gastroenterologic. Endosonograpy. New York: Thieme Stuttgart; 1992.
-
19Occena RO, Taylor SF, Robinson CC, Sokol RJ. Association of cytomegalovirus with Ménétrier's disease in childhood: report of two new cases with a review of literature. J Pediatr Gastroenterol Nutr. 1993; 17: 217-24.
-
20Hugh WJ, Coffey RJ, Washington MK. Ménétrier's disease: It's mimickers and pathogrnrsis. J Pathol Trans Med. 2016; 50: 10-6.
Publication Dates
-
Publication in this collection
Mar-Apr 2017
History
-
Received
02 Sept 2016 -
Reviewed
24 Jan 2017 -
Accepted
15 Mar 2017