Abstracts
Although basal ganglia calcifications were described a long time ago,1,3,11 the association of leukoencephalopathy, cerebral calcifications, and cysts (LCC) is a very rare entity described in 1996.5 We present a new case of LCC and discuss clinical, neuroradiologic, and histopathologic findings regarding this association.
Leukoencephalopathy; cerebral calcifications; brain cysts; epilepsy
Mesmo que as calcificaçãoes dos núcleos da base tenham sido descritas há muito tempo atrás1,3,11 a associação com leucoencefalopatia, calcificações cerebrais e cistos (LCC) é uma entidade muito rara descrita em 1996.5 Nós apresentamos um caso novo de LCC e discutimos os achados clínicos, neurorradiológicos e histopatológicos relacionados a essa entidade.
Leucoencefalopatia; calcificação cerebral; cisto cerebral; epilepsia
CASE REPORT
The rare association of leukoencephalopathy, cerebral calcifications, and cysts: case report
A associação rara de leucoencefalopatia, calcificações cerebrais e cistos: relato de caso
Gustavo Rassier IsolanI; Lucas Scotta CabralII; Cláudio Galvão de Castro JúniorIII; Ápio Cláudio AntunesIV; Gilberto SchwartsmannIII; Frederico Soares FalcettaV
IDivison of Neurosurgery, Division of Neurology HCPA/UFRGS. Graduate Program: Surgery, HCPA/UFRGS
IIDivision of Neurology, HCPA/UFRGS
IIIDivison of Oncology, HCPA/UFRGS
IVDivison of Neurosurgery, HCPA, UFRGS
VMedical School, UFRGS
Corresponding author Corresponding author: Gustavo Rassier Isolan Hospital de Clínicas de Porto Alegre Departamento de Neurologia Rua Ramiro Barcelos, 2350 CEP 90440-050, Porto Alegre, RS, Brasil Tel.: (+55)(51)2101-8182 - Fax: (+55)(51)3388-5085 E-mail: gisolan@yahoo.com.br
ABSTRACT
Although basal ganglia calcifications were described a long time ago,1,3,11 the association of leukoencephalopathy, cerebral calcifications, and cysts (LCC) is a very rare entity described in 1996.5 We present a new case of LCC and discuss clinical, neuroradiologic, and histopathologic findings regarding this association.
Keywords: Leukoencephalopathy, cerebral calcifications, brain cysts, epilepsy.
RESUMO
Mesmo que as calcificaçãoes dos núcleos da base tenham sido descritas há muito tempo atrás1,3,11 a associação com leucoencefalopatia, calcificações cerebrais e cistos (LCC) é uma entidade muito rara descrita em 1996.5 Nós apresentamos um caso novo de LCC e discutimos os achados clínicos, neurorradiológicos e histopatológicos relacionados a essa entidade.
Unitermos: Leucoencefalopatia, calcificação cerebral, cisto cerebral, epilepsia.
CASE REPORT
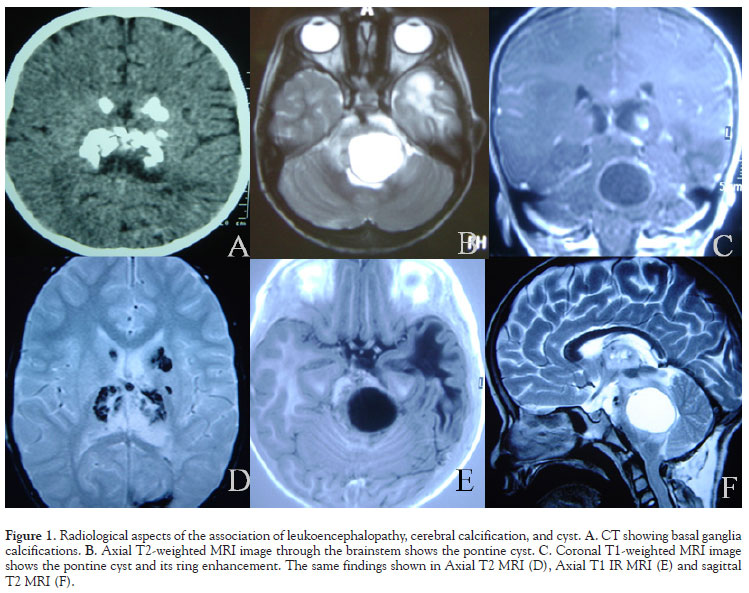
A 9-year-old male was admitted to our hospital for the evaluation of generalized tonic-clonic seizures, one year ago, and for a balance disorder one month ago. There were no complications during pregnancy. His parents were healthy and not consanguineous. No abnormality was found on general physical and ophthalmologic examinations. Neurologic evaluation showed dysbasia. Complete blood count, sedimentation rate, liver and renal function tests, serum thyroid and parathyroid hormones, calcium, phosphate, alkaline phosphatase, and lactate levels were within normal limits. Serological tests for cytomegalovirus, Toxoplasma gondii, and HIV 1 and 2 were all negative. Cervical, thoracic, and abdominal CT examinations showed no abnormality. Interictal Scalp EEG was normal. The initial CT showed numerous foci of calcifications scattered through the basal ganglia. In MRI, abnormally increased signal intensity was noted in the left temporal and occipital lobes white matter whereas the cortical gray matter was spared. A large pontine cyst was present. Cyst intensity was higher than that of the CSF on T2-weighted, T1-weighted and fluid-attenuated inversion recovery images. Contrast-enhanced scans showed ring enhancement of the cyst wall. A telovelar approach to the fourth ventricle was performed and a supracollicular puncture was done and the intracystic xantochromic fluid drained. The balance disturbance improved in the immediate postoperative period. Two months later the patient was readmitted to our clinic because of a CSF leak. A new MRI showed enlargement of the cyst and hydrocephalus. Based on these new findings a ventricular-peritoneal shunt was performed and one week later the pontine cyst was reoperated, but this time with aggressive resection of part of this wall, which was very adherent to the brainstem tissue, followed by cyst drainage. The intra-operative facial nerve monitoring with mapping of the floor of the fourth ventricle was used in this second operation and a supracollicular approach was performed. A shunt was introduced into the cystic cavity communicating it with the subdural space. The CSF leak resolved and the symptoms improved. The histopathologic examination of the cyst wall was inconclusive. The seizures are controlled with carbamazepine.
DISCUSSION
Leukoencephalopathy, cerebral calcifications and cysts (LCC) is a relatively new entity described in the medical literature. Regarding the clinical significance of each component of this syndrome, it has only really been realized that the triad might have distinct radiopathologic features. Despite the pioneering description of perivascular calcifications in the basal ganglia by Virchow,11 Bamberger,1 and Frietzche's3 first ever radiologic characterization of cysts, LCC only came to our attention after MRI became widely used. LCC was originally described by Labrune et al. in 1996;5 since then, approximately a dozen cases have been reported in the current medical literature.2,4,6,7,8,9
Reinterpretations of older reports linked this entity to Coats' disease, and raised the hypothesis that it would have to be inherited in autosomal recessive fashion.10 Later it was reported that at least some patients with Coats' disease can present brain calcifications, bringing these entities even closer.4 However, there is consistent evidence of the post-natal development of pathological hallmarks.7
There have been quite a few advances in the pathological characterization of LCC. On histopathological examination, angiomatous-like rearrangements of the microvessels are prominent. They are associated with Rosenthal fibers, intense gliosis, and microcalcifications; these were hypothesized by Labrune et al as secondary changes.
There is some predilection for the development of parenchymal cysts in the supratentorial compartment and cerebellum. As other pathological conditions - like leukoencepahlopathies and tumors - the expanding structure could be the sum of various fluid-containing small cysts,2 or simply the end effect of increased fluid content on the white matter.6 This is supported by ADC studies showing increased diffusibility and no diffusion restriction.8
It is suggested that an energy dysfunction stimulates cyst formation. This is indicated by spectroscopy studies performed by Nagae-Poetscher et al, which revealed an isolated lactate peak. The presence and significance of demyelization, however, remain controversial. Their study also showed reduced N-acetylaspartate and choline content. Nonetheless, the small sample size, the discordant creatine levels and the acquisition protocols preclude a clear answer to this question.7
In the great majority of reported cases, the onset was in childhood and adolescence. However, an adult-onset form is also suggested.9 The recognized clinical manifestations of LCC include cognitive decline, cerebellar signs and convulsive seizures, although any combination of pyramidal, extrapyramidal and cerebellar signs is possible according to lesion topography.
Overall, progressive calcifications in the basal nuclei, cerebellum and subcortical white matter are very accurately outlined by computed tomography. Diffuse white matter abnormalities and cysts are best appreciated on T2-weighted sequences; there is relative sparing of U-shaped fibers. Contrast-enhanced MRI presents with high signal intensities adjacent to cysts and calcifications, sometimes with mass effect, suggesting blood-brain barrier disruption.9
Little is known about the prognosis; the clinical course is thought to be slowly progressive. There is no proven specific therapy for LCC, other than the suggested symptomatic approach.
Received June 11, 2010; accepted July 16, 2010.
Medical School - HCPA/UFRGS
- 1. Bamberger PH. Beobach tungen und Bermerkungen bei Himkrankheiten. Verh Phys Med Gesellsch Wrzburg 1855;6:325-8.
- 2. Ben-Zeev B, Gross V, Kushnir T, et al. Vacuolating megalencephalic leukodystrophy in 12 Israel patients. J Child Neurol 2001;16:93-9.
- 3. Fritzsche R. Eine familiir auftretende Form von Oligophrenie mit rijntgenologisch nachweisbaren symmetrischen Kalkablagerungen im Gehim, besonders in den Stammganglien. Schweiz Arch Neural Psych. 1935;35:1-29.
- 4. Goutieres F, Dollfus H, Becquet F, Dufier JL. Extensive brain calcification in two children with bilateral Coats' disease. Neuropediatrics 1999;30:19-21.
- 5. Labrune P, Lacroix C, Goutieres F, et al. Extensive brain calcifications, leukodystrophy, and formation of parenchymal cysts: a new progressive disorder due to diffuse cerebral microangiopathy. Neurology 1996;46:1297-301.
- 6. Lohle PNM, van Mameren H, Zwindermann KH, et al. On the pathogenesis of brain tumour cysts: a volumetric study of tumour, oedema and cyst. Neuroradiology 2000;42:639-42.
- 7. Nagae-Poetscher LM, Bibat G, Philippart M, et al. Leukoencephalopathy, cerebral calcifications, and cysts: New observations. Neurology 2004;62:1206-9.
- 8. Pierpaoli C, Righini A, Linfante I, Tao-Cheng JH, Alger JR, Di Chiro G. Histopathologic correlates of abnormal water diffusion in cerebral ischemia: diffusion-weighted MR imaging and light and electron microscopic study. Radiology 1993;189:439-48.
- 9. Sener U, Zorlu Y, Men S et al. Leukoencephalopathy, Cerebral Calcifications, and Cysts. AJNR Am J Neuroradiol. 2006;27:200-3.
- 10. Tolmie JL, Browne BH, McGettrick PM, Stephenson JB. A familial syndrome with Coats' reaction retinal angiomas, hair and nail defects and intracranial calcification. Eye 1988;2:297-303.
- 11. Virchow R. Kalk metastases. Virchows Arch Path Anat. 1855;8: 103-13.
Corresponding author:
Publication Dates
-
Publication in this collection
20 Jan 2011 -
Date of issue
Sept 2010
History
-
Received
11 June 2010 -
Accepted
16 July 2010