Abstracts
BACKGROUND: Considering the paucity of information presently available concerning inferior phrenic arteries, a more definitive study seemed appropriate and necessary, both for its potential clinical applications and to provide additional data to contemporary anatomical literature. OBJECTIVE: Most anatomical textbooks of gross anatomy offer very little information concerning the anatomy and distribution of the inferior phrenic artery (IPA). For that reason, the origin of the IPA has been studied and the available literature has been reviewed. METHODS: Thirty-two human adult cadavers preserved in formalin obtained from the departments of Anatomy, Kasturba Medical College, Manipal and Mangalore were dissected and the origin of the IPA was studied. RESULTS: The IPA had its usual origin from the abdominal aorta in 28 cases but in the remaining four cases, two were arising from the celiac trunk, one from the left gastric artery and one from the right renal artery. CONCLUSION: The IPA usually originates from the aorta or celiac artery, and less frequently from the renal, hepatic or left gastric arteries. The IPA is a major source of collateral or parasitized arterial supply to hepatocellular carcinoma, second only to the hepatic artery. Literature on the IPA origin and clinical implications of variation in its origin have been reviewed in this article.
Inferior phrenic arteries; hepatocellular carcinoma; embolization; vascular variations
CONTEXTO: Considerando a escassez de informações atualmente disponíveis sobre artérias frênicas inferiores, umestudo mais definitivo nos pareceu apropriado e necessário, tanto por suas potenciais aplicações clínicas quanto para fornecer dados adicionais à literatura anatômica contemporânea. OBJETIVO: A maioria dos livros-texto de anatomia oferece muito poucas informações referentes à anatomia e distribuição da artéria frênica inferior (AFI). Por este motivo, a origem da AFI foi investigada e a literatura disponível foi revisada. MÉTODOS: Trinta e dois cadáveres humanos adultos preservados em formol e obtidos dos departamentos de anatomia do Kasturba Medical College, Manipal and Mangalore foram dissecados, e a origem da AFI foi investigada. RESULTADOS: A AFI teve sua origem habitual na aorta abdominal em 28 casos; no entanto, nos quatro casos restantes, duas originavam-se do tronco celíaco, uma da artéria gástrica esquerda e uma da artéria renal direita. CONCLUSÃO: A AFI geralmente origina-se da aorta ou artéria celíaca, e menos freqüentemente das artérias renal, hepática ou gástrica esquerda. A AFI é a maior fonte de fornecimento arterial colateral ou parasitado para carcinoma hepatocelular, ficando atrás somente da artéria hepática. A literatura sobre a origem da AFI e as implicações clínicas de variação em sua origem foram revisadas neste artigo.
Artérias frênicas inferiores; carcinoma hepatocelular; embolização; variações vasculares
ORIGINAL ARTICLE
The origin of the inferior phrenic artery: a study in 32 South Indian cadavers with a review of the literature
Origem da artéria frênica inferior: estudo em 32 cadáveres da Índia do Sul com revisão da literatura
Thejodhar PulakuntaI; Bhagath Kumar PotuI; Vasavi Rakesh GorantlaI; Muddanna S. RaoI; Sampath MadhyasthaII; Venkata Ramana VollalaIII
IDepartment of Anatomy, Kasturba Medical College, Manipal, Karnataka, India
IIDepartment of Anatomy, Kasturba Medical College, Mangalore, Karnataka, India
IIIDepartment of Anatomy, Melaka Manipal Medical College, Manipal, Karnataka, India
Correspondence Correspondence: Bhagath Kumar.Potu Department of Anatomy, Center for Basic Sciences Kasturba Medical College 576104 Manipal, Karnataka India Tel.: + 91 820 2922327 Email: potu_kumar2000@yahoo.co.in
ABSTRACT
BACKGROUND: Considering the paucity of information presently available concerning inferior phrenic arteries, a more definitive study seemed appropriate and necessary, both for its potential clinical applications and to provide additional data to contemporary anatomical literature.
OBJECTIVE: Most anatomical textbooks of gross anatomy offer very little information concerning the anatomy and distribution of the inferior phrenic artery (IPA). For that reason, the origin of the IPA has been studied and the available literature has been reviewed.
METHODS: Thirty-two human adult cadavers preserved in formalin obtained from the departments of Anatomy, Kasturba Medical College, Manipal and Mangalore were dissected and the origin of the IPA was studied.
RESULTS: The IPA had its usual origin from the abdominal aorta in 28 cases but in the remaining four cases, two were arising from the celiac trunk, one from the left gastric artery and one from the right renal artery.
CONCLUSION: The IPA usually originates from the aorta or celiac artery, and less frequently from the renal, hepatic or left gastric arteries. The IPA is a major source of collateral or parasitized arterial supply to hepatocellular carcinoma, second only to the hepatic artery. Literature on the IPA origin and clinical implications of variation in its origin have been reviewed in this article.
Keywords: Inferior phrenic arteries, hepatocellular carcinoma, embolization, vascular variations.
RESUMO
CONTEXTO: Considerando a escassez de informações atualmente disponíveis sobre artérias frênicas inferiores, umestudo mais definitivo nos pareceu apropriado e necessário, tanto por suas potenciais aplicações clínicas quanto para fornecer dados adicionais à literatura anatômica contemporânea.
OBJETIVO: A maioria dos livros-texto de anatomia oferece muito poucas informações referentes à anatomia e distribuição da artéria frênica inferior (AFI). Por este motivo, a origem da AFI foi investigada e a literatura disponível foi revisada.
MÉTODOS: Trinta e dois cadáveres humanos adultos preservados em formol e obtidos dos departamentos de anatomia do Kasturba Medical College, Manipal and Mangalore foram dissecados, e a origem da AFI foi investigada.
RESULTADOS: A AFI teve sua origem habitual na aorta abdominal em 28 casos; no entanto, nos quatro casos restantes, duas originavam-se do tronco celíaco, uma da artéria gástrica esquerda e uma da artéria renal direita.
CONCLUSÃO: A AFI geralmente origina-se da aorta ou artéria celíaca, e menos freqüentemente das artérias renal, hepática ou gástrica esquerda. A AFI é a maior fonte de fornecimento arterial colateral ou parasitado para carcinoma hepatocelular, ficando atrás somente da artéria hepática. A literatura sobre a origem da AFI e as implicações clínicas de variação em sua origem foram revisadas neste artigo.
Palavras-chave: Artérias frênicas inferiores, carcinoma hepatocelular, embolização, variações vasculares.
Introduction
Although descriptions of the right inferior phrenic artery (RIPA) and left inferior phrenic artery (LIPA) are typically very brief and lacking in detail in anatomy textbooks, they have received increased attention in recent years in the clinical literature. This stems largely from the discovery of the involvement of the right (most frequently) or left inferior phrenic arteries in the arterial supply and growth of hepatocellular carcinoma (HCC).1,2 Indeed, the great importance of such knowledge lies in the fact that an unresectable HCC can be treated by transcatheter embolization of not only its typical blood supply, the right or left hepatic arteries, but also by embolization of a RIPA, if involved.1-4
Accordingly, with the appropriately targeted utilization of certain current cancer treatments hinging on a thorough knowledge of the origin of the IPA, our current study aimed at establishing this very fact. There are few publications concerning the role and detailed anatomy of the IPA with respect to their involvement in HCC1,2,5 and, similarly, few have been produced with direct focus on the elucidation of the origin and distribution of these arteries.1,2,6 Quain, quoted by Pick & Anson,7 was the first author to describe the origin of the IPA. Tanabe et al.1 referred only to general textbook descriptions of these arteries and Gokan et al.2 reported on frequency of origin of the RIPA in a study of 16 patients. A study of 74 cadavers by Adachi8 is the largest available concerning IPA. Modern anatomy textbooks offer few details of the anatomy of the inferior phrenic arteries.9-11 Because transcatheter embolization of HCC and other hepatic neoplasms often involves finding the root of the RIPA, the interventional radiologist or oncologist could potentially benefit from knowledge of common variations in origin of these vessels and their respective frequencies of occurrence. The importance of the IPA is not limited to the treatment of HCC. Practically any hepatic neoplasm (including metastatic disease to the liver) may receive blood supply from the IPA. In addition, there have been reports of gastric hemorrhage due to bleeding from the LIPA after treatment of the left gastric artery with embolization.12
Vascular variations are constantly observed in dissection of adult cadavers.13 The inferior phrenic arteries usually originate from the aorta or celiac artery, and less frequently from the renal, hepatic or left gastric arteries. The roentgenographic anatomy of the phrenic arteries has been described in detail by Kahn et al.14 They contribute to the arterial supply of the adrenal glands and are thus important in angiographic examinations for adrenal lesions.14,15
In general, these vessels, which supply the diaphragm, are of small caliber.13,16,17 The purpose of this study was to analyze the origin of the inferior phrenic arteries.
Methods
Thirty-two human adult cadavers preserved in formalin, obtained from the departments of anatomy, Kasturba Medical College, Manipal and Mangalore were dissected and the origin of the inferior phrenic artery was studied. The ages of the cadavers ranged between 28-56 years. To dissect the abdominal aorta, the pancreas was removed with the aid of scissors. All the ganglions and the nervous tissue around the arteries were removed with the aid of a pincer and scissors to allow observing the disposition of these inferior phrenic arteries. After resection of tissues subjacent to the diaphragmatic crura and adherent tissues all along the median arcuate ligament, these structures were exposed, allowing observation of the origin of the IPA.
Results
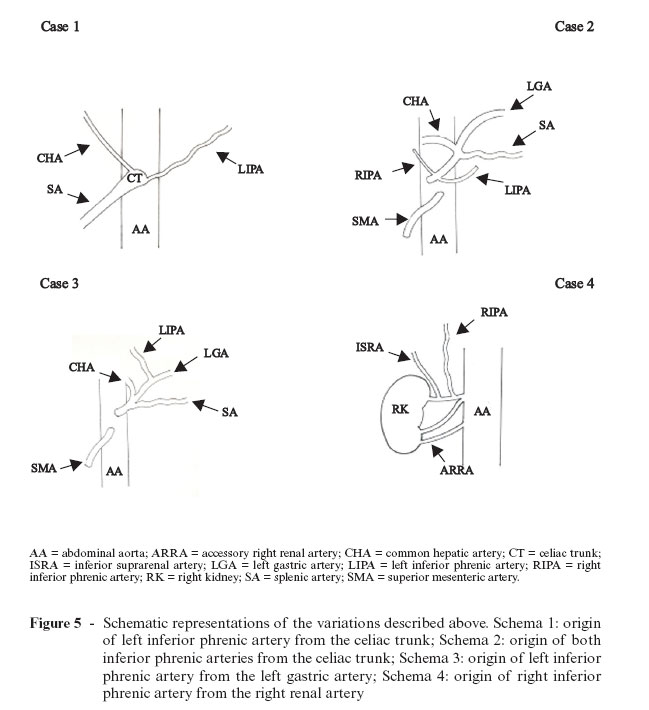
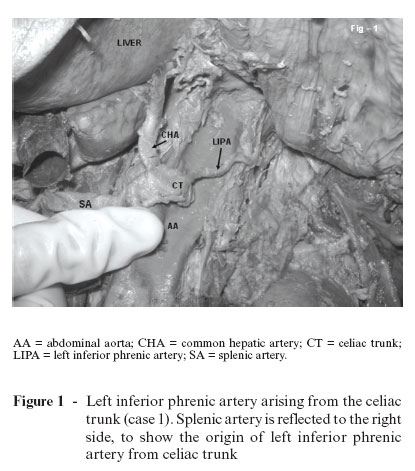
The inferior phrenic artery showed a variant origin in four out of 32 cases. It was seen to arise directly from the celiac trunk in two cases (Figures 1 and 2) and there was one case arising from the left gastric artery (Figure 3) and another from the right renal artery (Figure 4). The observations have been tabulated below in Table 1 and Figure 5.
Discussion
Considering the paucity of information presently available concerning these arteries, a more definitive study seemed appropriate and necessary, both for its potential clinical applications and to provide additional data to contemporary anatomical literature. In describing the origins of the IPA, the fourth edition of Mastery of Surgery11 gives only brief mention of the aorta or celiac trunk, or the right renal artery as sources of the IPA.
The English edition of Gray's Anatomy10 gives a slightly more complete account, claiming origins from the aorta or celiac trunk, variably from common trunks, and possibly from the renal artery. The American edition of Gray's Anatomy9 gives the most complete textbook account, claiming origins from both the celiac trunk and aorta, as well as describing common trunk origins and mentioning alternative origins, including the renal or accessory renal arteries, the left gastric, hepatic, and gonadal arteries. Interestingly, none of these references provide statistical information regarding origin of either the RIPA or LIPA.
In their analysis of the inferior phrenic arterial involvement in HCC, Tanabe et al.1 refer to other authors concerning the origins of the IPA, citing aortic and celiac trunk origins. The computed tomography (CT) study by Gokan et al.2 described these arteries with slightly greater detail and included actual percentages. They found that the most frequent origins were from the aorta and celiac trunk, with 46% of specimens presenting an aortic origin, most commonly on the right side, and a celiac origin, most commonly on the left (52%). They also observed the RIPA arising from the right renal artery in 9% of cases studied. They mentioned alternative origins as well (left gastric, hepatic, superior mesenteric, and spermatic), stating that such origins occurred with < 4% frequency on either the right or left sides. Anatomical studies by Anson & McVay18 provided illustrations that depicted the IPA situated at various levels vertically, but originating only from the aorta or celiac trunk. No numerical data were provided in their study. In an examination of 68 Japanese cadavers, Piao et al.6 found the majority of the IPA arising from the aorta (61.6%), with 28.2% of the IPA originating from the celiac trunk, and the remainder originating from either renal, left gastric, or middle adrenal arteries. Pick & Anson7 gave an impressive account of their findings concerning various aspects of the inferior phrenic arteries in their dissection of 200 cadavers. Regarding origins, they found aortic and celiac sources to be the most common (45.1 and 47.8%, respectively). They claimed common trunks variably for both as well, and even a common origin with the right internal spermatic artery. They found that < 7% arose variably from the renal (5.8%), left gastric (2.3%), or hepatic arteries (0.3%). This work is by far the most complete account to date of the IPA origins.
However, in the current study the origin of the IPA arteries from the celiac trunk was observed in two cases (6.25%), one from the left gastric artery (3.125%) and one from the right renal artery (3.125%) out of the 32 cadavers. In the remaining 28 cases it had its normal origin from the abdominal aorta. Loukas et al.19 reported that, out of 300 cadavers they studied, the right IPA originated from: a) celiac trunk in 40% of the specimens; b) aorta in 38%; c) renal in 17%; d) left gastric in 3%; and e) hepatic artery proper in 2% of the specimens. The left IPA originated from: a) celiac trunk in 47%; b) aorta in 45%; c) renal in 5%; d) left gastric in 2%; and e) hepatic artery proper in 1% of the specimens. The current study showed similar findings, except for the fact that the frequency of the IPA originating from the celiac trunk was much lesser.
The IPA is a major source of collateral or parasitized arterial supply to HCC, second only to the hepatic artery.19 The right IPA was always associated with HCC and served as the major collateral artery adjunct to the hepatic artery. These findings could have major implications in the transcatheter embolization of HCC patients. The knowledge of this type of variation shows that surgeons must be cautious to avoid unintentional sectioning of small-caliber arteries, as it may occur during celiac artery decompression in compression syndrome of the celiac trunk by the median arcuate ligament.
Presence of a supernumerary renal artery (as observed in case 4) is due to the abnormal disappearance or lack of formation of the lateral mesonephric arteries and their connecting channels.20,21
We hope this study has provided valuable data to researchers, clinicians and anatomists alike by enhancing the understanding of both the specific anatomy of the inferior phrenic arteries and their potential significance in supplying HCC and any number of other tumors, primary or metastatic, to the liver, such as cholangiocarcinoma, hepatoblastoma and subcapsular adenoma.22 For the clinician, in particular, treatments such as transcatheter embolization of HCC call for extensive knowledge of all possible variations of these vessels, particularly their origins, and it is conceivable that the application of this data will prove useful in the discussion and treatment of other hepatic, suprarenal or even diaphragmatic lesions unforeseen at the present time.19
Acknowledgements
We would like to thank Dr. Narga Nair, Professor and Head of the Department of Anatomy, KMC, Manipal for her support. We would also like to thank Mr. Nagaraj, Senior Artist, Center for Basic Sciences, KMC, Manipal for his assistance with the illustrations. A special thanks to Dr. Marios Loukas, MD, PhD, Department of Anatomy, American University of the Caribbean, Jordan Road, Cupecoy, Lowlands, Saint Maarten, Netherlands Antilles for his help.
Manuscript received May 21, 2007, accepted for publication Jun 08, 2007.
- 1. Tanabe N, Iwasaki T, Chida N, et al. Hepatocellular carcinomas supplied by inferior phrenic arteries. Acta Radiol. 1998;39:443-6.
- 2. Gokan T, Hashimoto T, Matsui S, Kushihashi T, Nobusawa H, Munechika H. Helical CT demonstration of dilated right inferior phrenic arteries as extrahepatic collateral arteries of hepatocellular carcinomas. J Comput Assist Tomogr. 2001;25:68-73.
- 3. Chung JW, Park JH, Han JK, Choi BI, Kim TK, Han MC. Transcatheter oily chemoembolization of the inferior phrenic artery in hepatocellular carcinoma: the safety and potential therapeutic role. J Vasc Interv Radiol. 1998;9:495-500.
- 4. Duprat G, Charnsangavej C, Wallace S, Carrasco CH. Inferior phrenic artery embolization in the treatment of hepatic neoplasms. Acta Radiol. 1988;29:427-9.
- 5. Andrews JC, Williams DM, Cho KJ, Knol JA, Wahl RL, Ensminger WD. Unsatisfactory hepatic perfusion after placement of an implanted pump and catheter system: angiographic correlation. Radiology. 1989;173:779-81.
- 6. Piao DX, Ohtsuka A, Murakami T. Typology of abdominal arteries, with special reference to inferior phrenic arteries and their esophageal branches. Acta Med Okayama. 1998;52:189-96.
- 7. Pick JW, Anson BJ. The inferior phrenic artery: origin and suprarenal branches. Anat Rec. 1940;78:413-27.
- 8. Adachi B. Das arteriensystem der japaner. Kyoto: Kaierlich-Japanichen Universitat; 1928;1:29-41.
- 9. Gray H. Anatomy of the human body. 30th ed. Baltimore: Williams & Wilkins; 1985. p. 746-7.
- 10. Gray H. Gray's anatomy. 38th ed. London: Churchill Livingstone; 1999. p. 1558.
- 11. Baker RJ, Fischer JE. Mastery of surgery. 4th ed. In: Philadelphia: Lippincott, Williams & Wilkins; 2001; p. 691692.
- 12. Northrop CH, Studley MA, Smith GR. Hemorrhage from the gastroesophageal junction. A cryptic angiographic diagnosis. Radiology. 1975;117(3 Pt 1):531-2.
- 13. Lipshutz B. A composite study of the coeliac trunkartery. Am. Surg. 1917;65:159-69.
- 14. Kahn PC. Selective angiography of inferior phrenic arteries. Radiology. 1967;88:1-8.
- 15. Kahn PC, Nickrosz LV. Selective angiography of adrenal glands. Am J Roentgenol Radium Ther Nucl Med. 1967;101:739-49.
- 16. Michels NA. The hepatic, cystic and retroduodenal arteries and their relations to the biliary ducts. Ann. Surg. 1951;133:503-24.
- 17. Michels NA. Collateral arterial pathways to the liver after ligation of the hepatic artery and removal of the celiac axis. Cancer. 1953;6:708-24.
- 18. Anson BJ, McVay CB. The topographical positions and the mutual relations of the visceral branches of the abdominal aorta: a study of 100 consecutive cadavers. Anat Rec. 1936;67:7-15.
- 19. Loukas M, Hullett J, Wagner T. Clinical anatomy of the inferior phrenic artery. Clin. Anat. 2005;18:357-65.
- 20. Moore KL. The developing human. Philadelphia: WB Saunders; 1973. p. 221.
- 21. Gray H. Gray's anatomy. 37th ed. Edinburgh: Churchill Livingstone; 1989. p. 256-8; 1407-9.
- 22. Cotran RS, Kumar V, Robbins SL. Robbins pathologic basis of disease. 5th ed. Philadelphia: WB Saunders; 1994. p. 831-71.
Publication Dates
-
Publication in this collection
17 Jan 2008 -
Date of issue
Sept 2007
History
-
Received
21 May 2007 -
Accepted
08 June 2007