Abstract
Transcatheter arterial chemoembolization is a technique for provoking ischemia and cytotoxic activity by selectively injecting microspheres containing chemotherapy drugs into vessels supplying a tumor. An 87-year-old female patient on palliative treatment for hepatocellular carcinoma and with indications for chemoembolization underwent preparatory angiography, which revealed celiac trunk occlusion. The treatment option chosen was selective catheterization of the hepatic artery proper to release the chemotherapy agent via an alternative route through the superior mesenteric artery with communication using the pancreaticoduodenal arcade. Studies have reported evidence showing increased survival after chemoembolization and also reduced tumor growth rate. However, difficulties with accessing and catheterizing the artery feeding the tumor via the alternative access make the procedure a challenge, because of the tortuosity of the pancreaticoduodenal arcade.
Keywords:
chemoembolization; hepatocellular carcinoma; palliative treatment
Resumo
A quimioembolização arterial transcateter consiste em promover isquemia e ação citotóxica por meio da injeção de microesferas contendo quimioterápicos aplicada seletivamente nos vasos que nutrem o tumor. Paciente do sexo feminino, com 87 anos, em tratamento paliativo para carcinoma hepatocelular com indicação de quimioembolização, foi submetida a angiografia pré-procedimento, a qual identificou oclusão do tronco celíaco. A opção foi a cateterismo seletiva da artéria hepática própria por uma via alternativa para lançamento do agente quimioterápico, através da artéria mesentérica superior com comunicação utilizando a arcada pancreatoduodenal. Evidências de aumento da sobrevida demonstrados em estudos após a quimioembolização foram relatados, bem como redução da taxa de crescimento tumoral; entretanto, dificuldades em acessar e cateterizar a artéria nutrícia tumoral através do acesso alternativo tornam o procedimento um desafio, devido à tortuosidade da arcada pancreatoduodenal.
Palavras-chave:
quimioembolização; carcinoma hepatocelular; tratamento paliativo
INTRODUCTION
Hepatocellular carcinoma (HCC) is the most common primary liver tumor, with elevated morbidity and mortality rates all over the world.11 Gaba RC, Lokken RP, Hickey RM, et al. Quality improvement guidelines for transarterial chemoembolization and embolization of hepatic malignancy. J Vasc Interv Radiol. 2017;28(9):1210-23. http://dx.doi.org/10.1016/j.jvir.2017.04.025. PMid:28669744.
http://dx.doi.org/10.1016/j.jvir.2017.04...
Although surgical resection is a curative treatment, few cases are candidates for hepatectomy, because of advanced multifocal disease, extrahepatic tumoral invasion, deterioration of liver function, portal hypertension, and poor functional status.11 Gaba RC, Lokken RP, Hickey RM, et al. Quality improvement guidelines for transarterial chemoembolization and embolization of hepatic malignancy. J Vasc Interv Radiol. 2017;28(9):1210-23. http://dx.doi.org/10.1016/j.jvir.2017.04.025. PMid:28669744.
http://dx.doi.org/10.1016/j.jvir.2017.04...
,22 Kwon JW, Chung JW, Song S-Y, et al. Transcatheter arterial chemoembolization for hepatocellular carcinomas in patients with celiac axis occlusion. J Vasc Interv Radiol. 2002;13(7):689-94. http://dx.doi.org/10.1016/S1051-0443(07)61845-4. PMid:12119327.
http://dx.doi.org/10.1016/S1051-0443(07)...
Liver transplantation is another effective option for curative treatment, but it is limited to the following cases: one tumor less than 5 cm in diameter or three tumors less than 3 cm in diameter (Milan Criteria), in addition to difficulties with finding donors.11 Gaba RC, Lokken RP, Hickey RM, et al. Quality improvement guidelines for transarterial chemoembolization and embolization of hepatic malignancy. J Vasc Interv Radiol. 2017;28(9):1210-23. http://dx.doi.org/10.1016/j.jvir.2017.04.025. PMid:28669744.
http://dx.doi.org/10.1016/j.jvir.2017.04...
Transcatheter arterial chemoembolization (TACE) is currently used as a palliative treatment for patients with tumors that cannot be resected33 Attia NM, Othman MH. Transcatheter arterial chemoembolization of hepatocellular carcinoma in patients with celiac axis occlusion using pancreaticoduodenal arcade as a challenging alternative route. Eur J Radiol Open. 2017;4:53-74. http://dx.doi.org/10.1016/j.ejro.2017.04.002. PMid:28516133.
http://dx.doi.org/10.1016/j.ejro.2017.04...
,44 Lencioni R, de Baere T, Soulen MC, Rilling WS, Geschwind JF. Lipiodol transarterial chemoembolization for hepatocellular carcinoma: A systematic review of efficacy and safety data. Hepatology. 2016;64(1):106-16. http://dx.doi.org/10.1002/hep.28453. PMid:26765068.
http://dx.doi.org/10.1002/hep.28453...
and also in cases of resectable tumors, to reduce tumor volume and dispersal of neoplastic cells during manipulation in surgical procedure.22 Kwon JW, Chung JW, Song S-Y, et al. Transcatheter arterial chemoembolization for hepatocellular carcinomas in patients with celiac axis occlusion. J Vasc Interv Radiol. 2002;13(7):689-94. http://dx.doi.org/10.1016/S1051-0443(07)61845-4. PMid:12119327.
http://dx.doi.org/10.1016/S1051-0443(07)...
The mechanism through which TACE achieves its objective is induction of ischemia in the tumor (generally by injection of gelfoam or microspheres) through the cytotoxic action of a chemotherapy agent selectively administered with the aim of provoking long-lasting intratumoral retention. This therapeutic method has a high positive response rate, retarding tumor progression and increasing survival. Once injected, the chemotherapy drug should ideally be retained in the tumor and released gradually to avoid systemic toxicity.55 Varela M, Real MI, Burrel M, et al. Chemoembolization of hepatocellular carcinoma with drug eluting beads: Efficacy and doxorubicin pharmacokinetics. J Hepatol. 2007;46(3):474-81. http://dx.doi.org/10.1016/j.jhep.2006.10.020. PMid:17239480.
http://dx.doi.org/10.1016/j.jhep.2006.10...
Currently, the drugs most often used are doxorubicin, combined or not with mitomycin or cisplatin, and irinotecan. There are two methods of chemoembolization in use: either conventional, using a chemotherapy mixture (with or without a liposoluble vehicle) combined with permanent or temporary emboligenic materials; or with granules loaded with a chemotherapy drug, using emboligenic microspheres.66 Basile A, Carrafiello G, Ierardi AM, Tsetis D, Brountzos E. Quality-improvement guidelines for hepatic transarterial chemoembolization. Cardiovasc Intervent Radiol. 2012;35(4):765-74. http://dx.doi.org/10.1007/s00270-012-0423-z. PMid:22648700.
http://dx.doi.org/10.1007/s00270-012-042...
Part I – Clinical situation
The patient was an 87-year-old female with hypertension and long-term diabetes. She had started seeing a hepatologist in 2009 because of a liver nodule found incidentally during a computed tomography examination of the abdomen, located in segment VI, with a diameter of approximately 2.6 cm, and no specific characteristics visible. During the initial investigation, renal and hepatic functions were normal, viral hepatitis serologies were negative, and alpha-fetoprotein was within normal limits. After 2 years, a control tomography showed a discrete enlargement in the nodule located in segment VI (2.8 cm) and a second nodule that had appeared in segment VII (0.9 cm).
During 2011, a repeat tomography showed that the nodule had enlarged further and, for the first time, a contrast uptake pattern was seen during the arterial phase, with washout during the other phases, compatible with a diagnosis of HCC, differentiating it from any type of benign lesion. In view of the patient’s comorbidities, the lesion was not biopsied and the patient was referred to our service for chemoembolization with doxorubicin, as a palliative measure, to prolong survival and quality of life.
Arteriography conducted preparatory to chemoembolization revealed obstruction of the celiac trunk, probably caused by atherosclerotic disease, making it a challenge to reach the tumor.
A total of four embolizations with doxorubicin were performed, in 2011, 2012, 2014, and, the most recent, in May of 2018. Control examinations showed an average regression of 30-40% in the diameter of the primary tumor. However, as the disease advanced, smaller-diameter satellite lesions began to appear, creating additional obstacles to palliative treatment. Nevertheless, after 9 years’ follow-up the patient still has preserved liver function and there is no evidence of thrombosis of the adjacent portal vein.
Part II – What was done
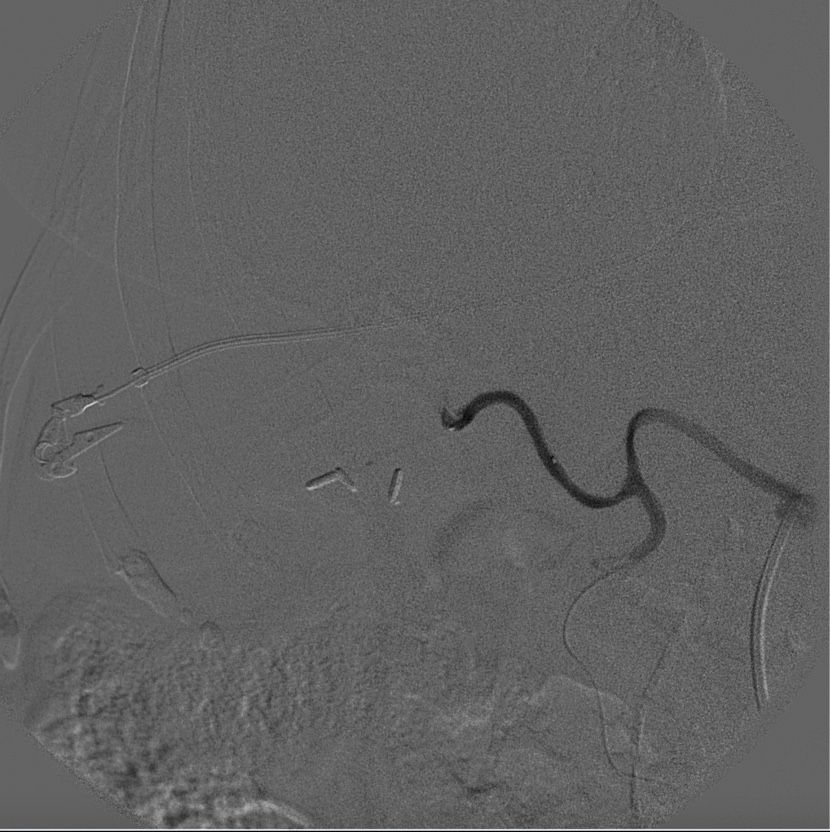
The procedures were all similar, but we will only describe the most recent, performed in 2018. With the patient under general anesthesia and aseptic technique, ultrasound-guided puncture of the right radial artery was performed, followed by placement of a 6F introducer specific for the radial artery, insertion of a 0.035 hydrophilic guidewire and multipurpose catheter, and catheterization of the abdominal aorta. Contrast imaging confirmed obstruction of the celiac trunk and patency of the superior mesenteric artery, an alternative route to access the liver (Figure 1). After catheterization of the superior mesenteric artery, the 0.035 guidewire was substituted for a 0.014 guidewire with microcatheter (Figure 2).
Catheterization of the pancreaticoduodenal arcade via the superior mesenteric artery and access to the hepatic artery proper.
The alternative route was, in the following order, via the inferior and superior pancreaticoduodenal arteries, the gastroduodenal artery, the hepatic artery proper, and the right hepatic artery. After superselective catheterization of the topography of segment VI (Figure 3), which was the site of the largest nodule and the greatest number of satellite nodules, 150-200 µm Hepaspheres™ (Merit Medical Systems, United States) loaded with doxorubicin were delivered. A control arteriography demonstrated satisfactory embolization of the target vessels (Figure 4).
DISCUSSION
Since the start of the century, diabetes mellitus has been considered a risk factor for emergence of several types of cancer. El-Serag et al. conducted a meta-analysis with 13 cohort studies and 13 case-control studies that linked the disease with a 2.5 times increased risk of appearance of hepatocarcinoma. Other studies confirmed these findings, attributing from 2 to 3 times increased risk and a considerable proportion of these studies only included patients with negative serology for viral hepatitis.77 Li X, Wang X, Gao P. Diabetes Mellitus and Risk of Hepatocellular Carcinoma. BioMed Res Int. 2017;20:5202684. http://dx.doi.org/10.1155/2017/5202684. PMid:29379799.
http://dx.doi.org/10.1155/2017/5202684...
The complex process of carcinogenesis involves several stages, that can be summarized as follows: endogenous hyperinsulinemia (insulin resistance), exogenous hyperinsulinemia (treatment with insulin or secretagogues), hyperglycemia, increased proinflammatory state and oxidative stress make damage to the genetic code more likely, increased angiogenesis and cell proliferation and reduced apoptosis rate.88 Mantovani A, Targher G. Type 2 diabetes mellitus and risk of hepatocellular carcinoma: spotlight on nonalcoholic fatty liver disease. Ann Transl Med. 2017;5(13):270. http://dx.doi.org/10.21037/atm.2017.04.41. PMid:28758096.
http://dx.doi.org/10.21037/atm.2017.04.4...
Therefore, since diabetes is a risk factor for hepatic neoplasms and our patient had negative serology for viral hepatitis, the fact that she had had diabetes for a long time supports the likelihood of a relationship between the two diseases.
In order to perform selective chemoembolization of HCC, it is necessary to catheterize the hepatic arteries via the celiac trunk, in order to determine which vessels lead to the lesion. This involves conducting an anatomovascular study of the tumor using the conventional arteriography technique with contrast to observe the origin of the HCC and the tortuosity of adjacent vessels and arteries, in addition to detecting anatomic variations, stenoses, transmural atherosclerotic disease, and possible occlusions of the celiac trunk and superior mesenteric artery. A microcatheter is inserted through the catheter to administer the injection of granules containing chemotherapy agents only into the vessels feeding the tumor, thereby avoiding necrosis of healthy tissue. At the end of TACE, control angiography is performed to confirm total devascularization of the target site.66 Basile A, Carrafiello G, Ierardi AM, Tsetis D, Brountzos E. Quality-improvement guidelines for hepatic transarterial chemoembolization. Cardiovasc Intervent Radiol. 2012;35(4):765-74. http://dx.doi.org/10.1007/s00270-012-0423-z. PMid:22648700.
http://dx.doi.org/10.1007/s00270-012-042...
In the case described here, the traditional access via the celiac trunk was not possible. Compression by the median arcuate ligament of the diaphragm tends to be identified as the cause of the majority of celiac axis occlusions. However, using imaging methods we identified that there was an intimate relationship with an atherosclerotic process. According to clinical trials, catheterization of arteries occluded by extrinsic compression is easier than catheterization of arteries occluded intrinsically, such as by atherosclerosis.22 Kwon JW, Chung JW, Song S-Y, et al. Transcatheter arterial chemoembolization for hepatocellular carcinomas in patients with celiac axis occlusion. J Vasc Interv Radiol. 2002;13(7):689-94. http://dx.doi.org/10.1016/S1051-0443(07)61845-4. PMid:12119327.
http://dx.doi.org/10.1016/S1051-0443(07)...
When the usual access cannot be obtained, an alternative approach is possible via the superior mesenteric artery to the hepatic artery proper, by dilation of the pancreaticoduodenal arcade and the gastroduodenal artery99 Yoo RE, Kim HC, Chung JW. Microcatheter looping technique for catheterization of the proper hepatic artery through pancreaticoduodenal arcades and gastroduodenal artery in celiac axis occlusion. Gastrointest Interv. 2013;2(2):118-20. http://dx.doi.org/10.1016/j.gii.2013.10.001.
http://dx.doi.org/10.1016/j.gii.2013.10....
(Figure 5).
Schematic diagram illustrating arteries related to the tumor and the alternative route employed during the procedure.
Recent studies have found significant results in terms of increased survival of patients with HCC after chemoembolization. A systematic review conducted in 2016 by Lencioni et al., including 10,108 patients in 101 studies, evaluated that this treatment resulted in a tumor response rate of 52.5% and mean survival of 19.4 months, with 70.3% at 1 year, 40.4% at 3 years, and 34.4% at 5 years.44 Lencioni R, de Baere T, Soulen MC, Rilling WS, Geschwind JF. Lipiodol transarterial chemoembolization for hepatocellular carcinoma: A systematic review of efficacy and safety data. Hepatology. 2016;64(1):106-16. http://dx.doi.org/10.1002/hep.28453. PMid:26765068.
http://dx.doi.org/10.1002/hep.28453...
Observational studies conducted on a global scale concluded that, to date, approximately half of patients with HCC have been given TACE at some point of their treatment. Meta-analysis studies have identified an evident increase in survival among patients treated with TACE using lipiodol, cisplatin, or doxorubicin, when compared with conservative treatment.44 Lencioni R, de Baere T, Soulen MC, Rilling WS, Geschwind JF. Lipiodol transarterial chemoembolization for hepatocellular carcinoma: A systematic review of efficacy and safety data. Hepatology. 2016;64(1):106-16. http://dx.doi.org/10.1002/hep.28453. PMid:26765068.
http://dx.doi.org/10.1002/hep.28453...
In a safety review, a total of 214 deaths were recorded in a study with 34,137 patients who underwent 50,953 transcatheter arterial chemoembolizations, resulting in an overall mortality rate of 0.6%, while the most common adverse events were liver failure (n = 59), followed by infectious complications (n = 20), gastrointestinal bleeding (n = 17), and rupture of intraperitoneal tumors (n = 8).44 Lencioni R, de Baere T, Soulen MC, Rilling WS, Geschwind JF. Lipiodol transarterial chemoembolization for hepatocellular carcinoma: A systematic review of efficacy and safety data. Hepatology. 2016;64(1):106-16. http://dx.doi.org/10.1002/hep.28453. PMid:26765068.
http://dx.doi.org/10.1002/hep.28453...
In a study conducted by Kwon et al., it did not prove possible to catheterize the hepatic artery proper via the alternative access in 8% of the patients. Problems mentioned were difficulties with manipulation of the catheter because of the tortuosity of the aorta, the small caliber and tortuosity of the pancreaticoduodenal arcade and the acute angle between the hepatic artery proper and the gastroduodenal artery. These cases were managed with percutaneous ethanol injection, systemic chemotherapy, and surgical operations. In one of these cases, vascular dissection of the celiac trunk was described; however, since this was not a major complication, the patient underwent TACE successfully and at the next session the rupture had resolved.22 Kwon JW, Chung JW, Song S-Y, et al. Transcatheter arterial chemoembolization for hepatocellular carcinomas in patients with celiac axis occlusion. J Vasc Interv Radiol. 2002;13(7):689-94. http://dx.doi.org/10.1016/S1051-0443(07)61845-4. PMid:12119327.
http://dx.doi.org/10.1016/S1051-0443(07)...
In another case report, published by Geiger et al.1010 Geiger MA, Callaert J, Deloose K, Bosiers M. Percutaneous retrograde crossing of a near-occluded celiac trunk via the superior mesenteric artery as an adjuvant maneuver for antegrade stenting. J Vasc Bras. 2016;15(1):61-5. http://dx.doi.org/10.1590/1677-5449.002415.
http://dx.doi.org/10.1590/1677-5449.0024...
, a patient with stenosis of the celiac trunk had a 6 x 15 mm stent deployed successfully via the superior mesenteric artery, which furnished the vascular surgeon with a new access route to the hepatic arteries and the possibility of less invasive, although difficult to execute, treatment.1010 Geiger MA, Callaert J, Deloose K, Bosiers M. Percutaneous retrograde crossing of a near-occluded celiac trunk via the superior mesenteric artery as an adjuvant maneuver for antegrade stenting. J Vasc Bras. 2016;15(1):61-5. http://dx.doi.org/10.1590/1677-5449.002415.
http://dx.doi.org/10.1590/1677-5449.0024...
We conclude that this was a challenging case in which obstruction of the celiac trunk – the traditional access route to the hepatic arteries, led us to employ an alternative route with greater tortuosity and technical difficulty, but which successfully achieved the objective. Another relevant detail of this case is the survival of the patient who, despite being in her ninth decade of life and undergoing palliative treatment, has satisfactory quality of life.
-
How to cite: Moraes AO, Nascimento EA, Zubiolo TFM, et al. Transcatheter arterial chemoembolization of hepatocellular carcinoma in a patient with celiac trunk occlusion: a therapeutic challenge. J Vasc Bras. 2019;18: e20180090. https://doi.org/10.1590/1677-5449.180090
-
Financial support: None.
-
The study was carried out at Hospital Maringá, Setor de Hemodinâmica, Maringá, PR, Brazil.
REFERÊNCIAS
-
1Gaba RC, Lokken RP, Hickey RM, et al. Quality improvement guidelines for transarterial chemoembolization and embolization of hepatic malignancy. J Vasc Interv Radiol. 2017;28(9):1210-23. http://dx.doi.org/10.1016/j.jvir.2017.04.025 PMid:28669744.
» http://dx.doi.org/10.1016/j.jvir.2017.04.025 -
2Kwon JW, Chung JW, Song S-Y, et al. Transcatheter arterial chemoembolization for hepatocellular carcinomas in patients with celiac axis occlusion. J Vasc Interv Radiol. 2002;13(7):689-94. http://dx.doi.org/10.1016/S1051-0443(07)61845-4 PMid:12119327.
» http://dx.doi.org/10.1016/S1051-0443(07)61845-4 -
3Attia NM, Othman MH. Transcatheter arterial chemoembolization of hepatocellular carcinoma in patients with celiac axis occlusion using pancreaticoduodenal arcade as a challenging alternative route. Eur J Radiol Open. 2017;4:53-74. http://dx.doi.org/10.1016/j.ejro.2017.04.002 PMid:28516133.
» http://dx.doi.org/10.1016/j.ejro.2017.04.002 -
4Lencioni R, de Baere T, Soulen MC, Rilling WS, Geschwind JF. Lipiodol transarterial chemoembolization for hepatocellular carcinoma: A systematic review of efficacy and safety data. Hepatology. 2016;64(1):106-16. http://dx.doi.org/10.1002/hep.28453 PMid:26765068.
» http://dx.doi.org/10.1002/hep.28453 -
5Varela M, Real MI, Burrel M, et al. Chemoembolization of hepatocellular carcinoma with drug eluting beads: Efficacy and doxorubicin pharmacokinetics. J Hepatol. 2007;46(3):474-81. http://dx.doi.org/10.1016/j.jhep.2006.10.020 PMid:17239480.
» http://dx.doi.org/10.1016/j.jhep.2006.10.020 -
6Basile A, Carrafiello G, Ierardi AM, Tsetis D, Brountzos E. Quality-improvement guidelines for hepatic transarterial chemoembolization. Cardiovasc Intervent Radiol. 2012;35(4):765-74. http://dx.doi.org/10.1007/s00270-012-0423-z PMid:22648700.
» http://dx.doi.org/10.1007/s00270-012-0423-z -
7Li X, Wang X, Gao P. Diabetes Mellitus and Risk of Hepatocellular Carcinoma. BioMed Res Int. 2017;20:5202684. http://dx.doi.org/10.1155/2017/5202684 PMid:29379799.
» http://dx.doi.org/10.1155/2017/5202684 -
8Mantovani A, Targher G. Type 2 diabetes mellitus and risk of hepatocellular carcinoma: spotlight on nonalcoholic fatty liver disease. Ann Transl Med. 2017;5(13):270. http://dx.doi.org/10.21037/atm.2017.04.41 PMid:28758096.
» http://dx.doi.org/10.21037/atm.2017.04.41 -
9Yoo RE, Kim HC, Chung JW. Microcatheter looping technique for catheterization of the proper hepatic artery through pancreaticoduodenal arcades and gastroduodenal artery in celiac axis occlusion. Gastrointest Interv. 2013;2(2):118-20. http://dx.doi.org/10.1016/j.gii.2013.10.001
» http://dx.doi.org/10.1016/j.gii.2013.10.001 -
10Geiger MA, Callaert J, Deloose K, Bosiers M. Percutaneous retrograde crossing of a near-occluded celiac trunk via the superior mesenteric artery as an adjuvant maneuver for antegrade stenting. J Vasc Bras. 2016;15(1):61-5. http://dx.doi.org/10.1590/1677-5449.002415
» http://dx.doi.org/10.1590/1677-5449.002415
Publication Dates
-
Publication in this collection
30 May 2019 -
Date of issue
2019
History
-
Received
15 Oct 2018 -
Accepted
25 Feb 2019