Abstract
The development of infiltrative bladder carcinoma in patients previously treated with radical prostatectomy due to prostate adenocarcinoma represents a challenging perspective. Radical cystectomy remains the best option for invasive bladder cancer, however, there are few reports about the best approach to such individuals. Nevertheless, despite possible technical difficulties found during surgery, the orthotopic urinary shunt is a reasonable option in selected cases.
bladder cancers; prostatic neoplasms; urinary diversion
CASE REPORT
Cystectomy with orthotopic reconstruction following radical retropubic prostatectomy
Ari Miotto Jr; Marcos Dall'Oglio; Miguel Srougi
Division of Urology, Paulista School of Medicine, Federal University of São Paulo, UNIFESP, and Syrian-Lebanese Hospital, São Paulo, SP, Brazil
Correspondence Correspondence to Dr. Miguel Srougi Rua Barata Ribeiro, 414 / 7º andar São Paulo, SP, 01308-000, Brazil Fax: + 55 11 3257-8002 E-mail: srougi@attglobal.net
ABSTRACT
The development of infiltrative bladder carcinoma in patients previously treated with radical prostatectomy due to prostate adenocarcinoma represents a challenging perspective. Radical cystectomy remains the best option for invasive bladder cancer, however, there are few reports about the best approach to such individuals. Nevertheless, despite possible technical difficulties found during surgery, the orthotopic urinary shunt is a reasonable option in selected cases.
Key words: bladder cancers; prostatic neoplasms; urinary diversion
INTRODUCTION
A subgroup of the population of patients who undergo radical prostatectomy can develop other malignant neoplasias in pelvic organs, including invasive bladder carcinoma (1). Cystectomy in this group of patients is the treatment of choice, however, the preservation of bodily image through the confection of an orthotopic neobladder remains a matter of discussion (1).
We present a case report of radical cystectomy with ileal neobladder in the late post-operative period of a radical prostatectomy.
CASE REPORT
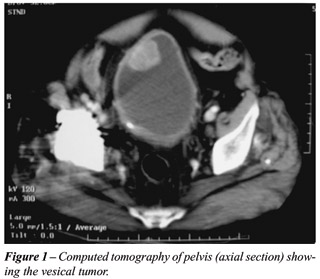
A 78-year old male patient underwent prostatovesiculectomy and bilateral iliac lymphadenectomy 6 years earlier, whose pathological examination revealed prostate adenocarcinoma Gleason 3 + 2, stage T2b. Post-operative outcome was satisfactory, remaining with urinary continence and preserved sexual potency, and current PSA < 0.04. During the follow-up, he presented an episode of painless macroscopic hematuria, undergoing an urethrocystoscopy that evidenced a vesical tumor. The transrectal resection of the bladder tumor confirmed the diagnosis of transitional cell carcinoma (TCC) with invasion of the muscular layer. The systemic staging through computerized tomography of abdomen (Figure-1) and thorax, and bone scintigraphy discarded metastatic disease.
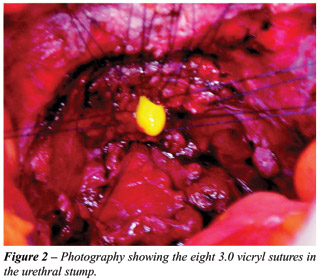
Consequently to such result, the patient underwent radical cystectomy that evolved without abnormalities, with no need of blood transfusion. The freezing biopsy of urethral margin and distal ureters was performed, revealing margins free from neoplastic involvement. The reconstruction of urinary transit was performed through orthotopic ileal neobladder modified by Srougi et al. (2) and urethro-ileal anastomosis with 8 separate Vicryl 3-0 sutures (Figure-2). The pathological examination evidenced high-grade TCC, infiltrative in muscular wall, stage T2b. The patient was released from the hospital on the tenth post-operative day, with removal of stents and double-J catheter on the twentieth day. Currently he is on the 30th post-operative day, with diurnal urinary continence, and presenting nocturnal enuresis.
DISCUSSION
Approximately 2% of patients undergoing radical prostatectomy will require cystectomy due to infiltrative bladder neoplasia and among these, only one third will have reconstruction of the urinary tract through confection of an orthotopic ileal neobladder (1).
Studies demonstrate a higher risk of surgical complications in cases where any treatment had been performed previously to cystectomy; 44% following radical prostatectomy and 65% following radiotherapy. However, when only major complications are analyzed, the numbers are equivalent to patients who did not receive previous treatment, with reintervention being necessary in approximately 9% of complications (3). In the case reported we did not have transoperative difficulties, however the dissection of the vesico-urethral anastomosis had to be meticulous, with the possibility of using a flexible cystoscope to help obtain a better preservation of the urethral stump (1). Preservation of the neurovascular bundle is impaired by the loss of anatomic planes due to the previous surgery (1). Mean blood loss ranges between 275 and 3500 mL (3), and in this case it was 500 mL with no need of blood transfusion.
Schuster et al. (1) believe that patients undergoing cystectomy following radical prostatectomy lose lower quantities of blood than those undergoing cystectomy following radiotherapy, with a largest extravesical dissemination of the tumor occurring in these cases and consequently presenting higher technical difficulty, higher surgical time and lower possibility of orthotopic reconstruction. Despite a little expressive experience, such data demonstrate that the prognosis is better in cases of cystectomy following prostatectomy radical (1). Concerning the absence of blood transfusion in this case, we attribute it to a meticulous dissection, additionally there is a lower risk of locally advanced diseased in post-radical prostatectomy cases (30%) when compared with post-radiotherapy cases (60%) (1). On the other hand, in relation to the form of reconstruction of the urinary transit, there seems to be no increase in complications initially, thus favoring the preservation of bodily image and a prompt return to social life.
Received: January 21, 2004
Accepted after revision: March 24, 2004
- 1. Schuster TG, Marcovich R, Sheffield J, Montie JE, Lee CT: Radical cystectomy for bladder cancer after definitive prostate cancer treatment. Urology. 2003; 61: 342-7.
- 2. Srougi M, Sakai AT, D'Império M: Radical Cystectomy. In: Srougi M, Simon SD (eds.), Urological Cancer. São Paulo, Platina. 1990; pp. 255-79. [
- 3. Kukarni JN, Pramesh CS, Rathi S, Pantvaidya GH: Long-term results of orthotopic neobladder reconstruction after radical cystectomy. BJU Int. 2003; 91: 485-8.
Publication Dates
-
Publication in this collection
01 June 2004 -
Date of issue
Apr 2004
History
-
Received
21 Jan 2004 -
Accepted
24 Mar 2004