Abstract
Objective
To evaluate the efficacy of Profluss® on prostatic chronic inflammation (PCI).
Materials and Methods
We prospectively enrolled 168 subjects affected by LUTS due to bladder outlet obstruction submitted to 12 cores prostatic biopsy for suspected prostate cancer + 2 cores collected for PCI valuation. First group consisted of 108 subjects, with histological diagnosis of PCI associated with BPH and high grade PIN and/or ASAP, randomly assigned to 1:1 ratio to daily Profluss® (group I) for 6 months or to control group (group Ic). Second group consisted of 60 subjects, with histological diagnosis of BPH, randomly assigned to 1:1 ratio to daily Profluss® + α-blockers treatment (group II) for 3 months or to control group (group IIc). After 6 months first group underwent 24 cores prostatic re-biopsy + 2 cores for PCI while after 3 months second group underwent two-cores prostatic for PCI. Specimens were evaluated for changes in inflammation parameters and for density of T-cells (CD3, CD8), B-cells (CD20) and macrophages (CD68).
Results
At follow-up there were statistical significant reductions of extension and grading of flogosis, mean values of CD20, CD3, CD68 and mean PSA value in group I compared to Ic, while extension and grading of flogosis in group II were inferior to IIc but not statistical significant. A statistically significant reduction in the density of CD20, CD3, CD68, CD8 was demonstrated in group II in respect to control IIc.
Conclusions
Serenoa repens+Selenium+Lycopene may have an anti-inflammatory activity that could be of interest in the treatment of PCI in BPH and/or PIN/ASAP patients.
Phytotherapy; Serenoa; Inflammation; Prostatitis; Prostatic Hyperplasia
INTRODUCTION
Benign prostatic hyperplasia (BPH) is a common cause of bothersome lower urinary tract symptoms in man, representing a growing entity in terms of healthcare costs and morbidity.
Approximately 50% of men aged between 50 and 60 years, 60% of men aged between 60 and 70 years, and up to 90% of men aged > 80 years have some degree of benign prostatic enlargement (BPE) (11. Berry SJ, Coffey DS, Walsh PC, Ewing LL: The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132: 474-9.).
Medical therapies can provide adequate alleviation of BPE symptoms (LUTS): The two primary classes of oral medications that are prescribed for the treatment of symptoms are alpha-blockers and 5-alpha-reductase inhibitors (5ARIs). Despite medical therapy improves LUTS, some adverse events (ejaculatory dysfunction, loss of libido, erectile dysfunction) are caused by the treatment, worsening an already compromised sexual function (22. Miner M, Rosenberg MT, Perelman MA: Treatment of lower urinary tract symptoms in benign prostatic hyperplasia and its impact on sexual function. Clin Ther. 2006; 28: 13-25.).
The aetiology of BPH is still far from being fully understood but multiple partially overlapping and complementary theories have been proposed (33. Tang J, Yang J: Etiopathogenesis of benign prostatic hypeprlasia. Indian J Urol. 2009; 25: 312-7.). There are some evidences that prostatic inflammation could be a key component in BPE and BPH progression.
Two of the major clinical studies on BPH (MTOPS and Reduce study) recently demonstrated the link between histological prostatic inflammation and prostate enlargement or symptoms scores (44. Roehrborn CG, Kaplan SA, Noble WD: The impact of acute or chronic inflammation in baseline biopsy on the risk of clinical progression of BPE: Results from the MTOPS study. AUA Meeting 2005. J Urol, suppl., 2005; 173: 346, abstract 1277.,55. Nickel JC, Roehrborn CG, O'Leary MP, Bostwick DG, Somerville MC, Rittmaster RS: The relationship between prostate inflammation and lower urinary tract symptoms: examination of baseline data from the REDUCE trial. Eur Urol. 2008; 54: 1379-84.). Numerous major key players in chronic inflammation have been studied in BPH: varieties of growth factors and cytokines have been shown to be involved both in the inflammatory process and in the epithelial/stromal prostatic cells interactions (66. Kramer G, Mitteregger D, Marberger M: Is benign prostatic hyperplasia (BPH) an immune inflammatory disease? Eur Urol. 2007; 51: 1202-16.). These mediators are released in the prostatic gland by inflammatory cells that can be found on most of the surgery-derived BPH specimens (77. Di Silverio F, Gentile V, De Matteis A, Mariotti G, Giuseppe V, Luigi PA, et al.: Distribution of inflammation, pre-malignant lesions, incidental carcinoma in histologically confirmed benign prostatic hyperplasia: a retrospective analysis. Eur Urol. 2003; 43: 164-75.).
The inflammatory cells may trigger a sophisticated and well-orchestrated inflammatory cascade, resulting in excessive oxidative stress, activation of the transcription factor nuclear factor-kappa B (NF-κB), production of several cytokines and overexpression of inducible-cyclooxygenase (COX-2), inducible-nitric-oxide-synthase (iNOS) and 5-lipoxygenase (5-LOX), leading, in turn, to the release of prostaglandins, nitrates, and leukotrienes. Furthermore, inflammatory cells produce growth factors, such as vascular endothelial growth factor (VEGF) and transforming growth factor-β (TGF-β), which may support fibromuscular growth in BPH (88. Sciarra A, Di Silverio F, Salciccia S, Autran Gomez AM, Gentilucci A, Gentile V: Inflammation and chronic prostatic diseases: evidence for a link? Eur Urol. 2007; 52: 964-72.).
Plant extracts have been used in the medical management of BPH-induced LUTS with the aim to relieve symptoms without adverse events related to treatment (99. Comhaire F, Mahmoud A: Preventing diseases of the prostate in the elderly using hormones and nutriceuticals. Aging Male. 2004; 7: 155-69.).
Serenoa Repens (SeR), derived from the berries of the saw palmetto tree, is the most popular naturally derived medication for BPH (1010. Suzuki M, Ito Y, Fujino T, Abe M, Umegaki K, Onoue S, et al.: Pharmacological effects of saw palmetto extract in the lower urinary tract. Acta Pharmacol Sin. 2009; 30: 227-81.). Several mechanisms of action have been proposed to explain its therapeutic efficacy, including inhibition of 5α-reductase and dihydrotestosterone binding to androgen receptors, a weak α1-adrenergic receptor antagonism, inhibition of growth factors-induced prostate cell proliferation and inhibition of COX-2 and 5-LOX (1111. Buck AC: Is there a scientific basis for the therapeutic effects of serenoa repens in benign prostatic hyperplasia? Mechanisms of action. J Urol. 2004; 172: 1792-9.).
Besides SeR, both lycopene (LY), a dietary carotenoid synthesized by plants, fruits,
and microorganisms with a strong antioxidant activity, and selenium (Se), an essential trace element
mainly functioning through seleno-proteins and able to promote an optimal antioxidant/oxidant
balance, have been shown to exert beneficial effects in BPH (1212. Diwadkar-Navsariwala V, Prins GS, Swanson SM, Birch LA, Ray VH, Hedayat S, et
al.: Selenoprotein deficiency accelerates prostate carcinogenesis in a transgenic model. Proc Natl
Acad Sci U S A. 2006; 103: 8179-84.
13. Schwarz S, Obermüller-Jevic UC, Hellmis E, Koch W, Jacobi G, Biesalski HK:
Lycopene inhibits disease progression in patients with benign prostate hyperplasia. J Nutr. 2008;
138: 49-53.
14. Kandaş NO, Randolph C, Bosland MC: Differential effects of selenium on benign
and malignant prostate epithelial cells: stimulation of LNCaP cell growth by noncytotoxic, low
selenite concentrations. Nutr Cancer. 2009; 61: 251-64.
15. Wertz K, Siler U, Goralczyk R: Lycopene: modes of action to promote prostate
health. Arch Biochem Biophys. 2004; 430: 127-34.-1616. Obermüller-Jevic UC, Olano-Martin E, Corbacho AM, Eiserich JP, van der Vliet A,
Valacchi G, et al.: Lycopene inhibits the growth of normal human prostate epithelial cells in vitro.
J Nutr. 2003; 133: 3356-60.).
The aim of this study is to evaluate the efficacy of Profluss® ( SeR-Se-LY) in reducing chronic inflammation in patient with benign prostatic hyperplasia and/or PIN/ASAP.
MATERIALS AND METHODS
Study design, patients selection criteria and allocation
The “Flogosis And Profluss in Prostatic and Genital Disease” (FLOG) study was a multicentre study involving 9 urological Italian centres between January 2009 and December 2010 that analysed prospectively collected data of two category of patients affected by BPH and/or PIN/ASAP. The inclusion criteria for the first group were: presence of LUTS due to bladder outlet obstruction (BOO) secondary to clinical BPH, assessed by urodynamic and pressure flow evaluation, PSA > 4ng/mL and/or DRE abnormality and/or abnormal findings on transrectal ultrasound, 12 cores prostatic biopsy performed for suspected prostate cancer with two more cores collected from the left and right lobes (for chronic inflammation evaluation), histological diagnosis of prostatic chronic inflammation associated with BPH and high grade PIN and/or ASAP. Exclusion criteria were: treatment with NSAIDs or corticosteroids in the previous 6 months, urinary infection, treatment with finasteride or dutasteride, phytotherapy in the previous 6 months; diagnosis of prostatic cancer (PCa). Fourty patients were excluded after PCa was diagnosed and finally 108 patients were analysed in this study. Subjects were randomly assigned to 1:1 ratio to SeR 320mg+LY5mg+Se50mcg/day treatment (group I) for 6 months or to control group (group Ic) and then underwent 24 cores prostatic re-biopsy with two more needle biopsies (for chronic inflammation evaluation) collected from the left and right lobes in the same previous areas allowing similar histopathological analysis.
Inclusion criteria for second group were: presence of LUTS due to bladder outlet obstruction (BOO) secondary to clinical BPH, assessed by urodynamic and pressure flow evaluation, PSA > 4ng/mL and/or DRE abnormality and/or abnormal findings on transrectal ultrasound, 12 cores prostatic biopsy performed for suspected prostate cancer with two more cores collected from the left and right lobes (for chronic inflammation valuation), histological diagnosis of prostatic chronic inflammation associated with BPH and indication for surgical treatment. Exclusion criteria were: treatment with NSAIDs or corticosteroids in the previous 6 months; treatment with finasteride or dutasteride, phytotherapy in the previous 6 months, urinary infection, diagnosis of PCa. Sixty-six consecutive patients met inclusion criteria. Six patients dropped out for various reasons: 2 lost to follow-up and 4 excluded due to concomitant drug medication which was not allowed by the criteria we had established. Finally, a total of 60 patients were included in the analysis and they were enrolled and randomly assigned to 1:1 ratio to SeR 320mg+LY5mg+Se50mcg/day and α-blockers treatment (group II) for 3 months or to control group (group IIc). At month 3 two-cores prostatic biopsy was performed in the same areas of the previous allowing similar histopathological analysis and then underwent Transurethral Resection of Prostate (TURP).
Principles outlined in the Declaration of Helsinki were followed and all patients signed a written informed consent form.
Histopathological evaluation
Prostate specimens were fixed with 10% buffered formalin for 8-12 hours (biopsy), 12-24 hours (TURP) and sent for central review by a blinded pathologist.
Coloration of specimens was performed by hematoxylin-eosin. On the main representative area of each histological specimen, parameters of flogosis like extensions and grading of flogosis were evaluated, according to the score of Nickel (1717. Nickel JC, True LD, Krieger JN, Berger RE, Boag AH, Young ID: Consensus development of a histopathological classification system for chronic prostatic inflammation. BJU Int. 2001; 87: 797-805.).
On paraffin sections of 5 micron were assessed, by immunohistochemical technique using monoclonal antibodies (Dako company), B-lymphocytes (CD20), T-lymphocytes (CD3, CD8), and macrophages (CD68). The detection system was the universal kit LSAB of the Dako company. All the immunohistochemical procedures were performed using the automated immunostaining Optimax Plus system (Biogenex, San Ramon, USA).
The immunostaining specimens were assessed using the Axioplan Zeiss microscope with Axiovision software. For each specimen with positive immunostaining for CD20, CD3, CD8 and CD68, only the main representative areas were selected, using a zoom 10x.
Subsequently the positive cells were counted in three fields with lens 20x, within this area, the medium value was considered as expression of B and T lymphocyte density and as expression of the macrophages density present in the specimen.
Statistical analysis
Baseline characteristics are presented as frequencies of occurrence or mean and standard deviation as appropriate. Statistical differences among groups of frequencies were tested by Chi-square test. Given the not normal distribution of continuous data, we tested differences among independent samples by Mann-Whitney U-test.
All statistical tests were two-tailed and p-value < 0.05 were considered significant. Data were entered into Microsoft Excel for Windows (Microsoft Corporation, Redmond, WA). Statistical analysis was performed using SPSS for Windows release 17.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Clinical results
Baseline demographic and clinical characteristics of patients analyzed are listed in Table-1. No differences in terms of parameters collected, such as age, prostate volume, PSA values, urodynamic findings and other general health status variants were observed between groups.
- Baseline clinical and histopathological characteristics of population and comparision of groups at inclusion.
Histopathological findings and results
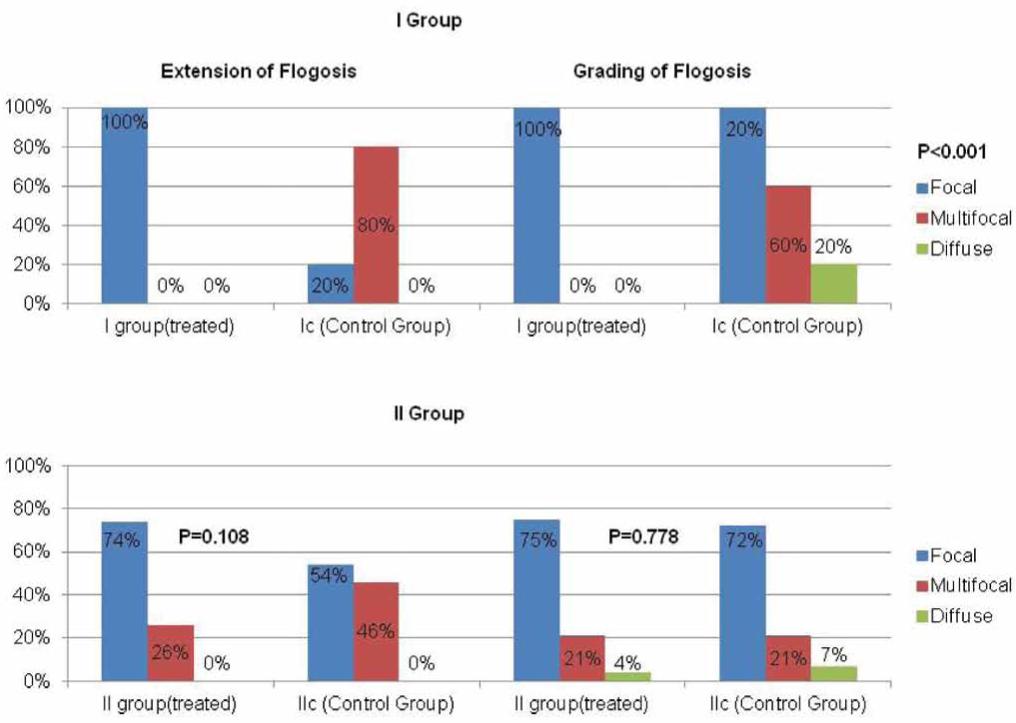
At 6-month histopathological evaluation, a significant difference of flogosis was demonstrated between Groups I and Ic, with a reduction both of extension (P < 0.001) and grading (P < 0.001) of flogosis among treated patients (Figure-1).
Extension and grading of flogosis on surgical specimens of patients treated with (Profluss®) and control group with PIN/ASAP (I Group) and BPH (II Group).
Histopathological evaluation performed at 3 months in patients enrolled in Group II revealed no significant difference of extension and grading of flogosis in respect to group control IIc (Figure-1). However, a slight reduction of extension and grading could be observed in the treated group.
A significant reduction of total interstitial mononuclear cells, B lymphocytes, T lymphocytes and macrophages in Group I compared with control group (Ic) was observed at 6-month evaluation (P < 0.001) (Table-2).
- Total number of infiltrates, inflammatory cells markers included in the study and serum PSA with average findings in PIN/ASAP patients at 6-month evaluation.
Among patients with BPH (Group II), total interstitial mononuclear cells, B lymphocytes, T lymphocytes and macrophages were significantly reduced at 3 month evaluation compared with control group (P < 0.001) (Table-3).
- Total number of infiltrates, inflammatory cells markers included in the study and serum PSA with average findings in BPH patients at 3-month evaluation.
According with the reduction of extension and grade of flogosis in Group I, mean PSA values was significantly lower than in control group (P < 0.0001) (Table-2).
No statistical significant reduction of PSA value was demonstrated between Groups II and IIc (Table-3).
DISCUSSION
Almost all surgery-derived BPH specimens show inflammatory infiltrates at histological examination (1818. Kohnen PW, Drach GW: Patterns of inflammation in prostatic hyperplasia: a histologic and bacteriologic study. J Urol. 1979; 121: 755-60.,1919. Nickel JC, Downey J, Young I, Boag S: Asymptomatic inflammation and/or infection in benign prostatic hyperplasia. BJU Int. 1999; 84: 976-81.); yet most of these patients neither have clinical signs of infection nor any correlation with bacterial or other foreign antigens.
In a study by Robert et al. it was found that most patients, treated by surgery for complicated and/or symptomatic BPH, had inflammatory cells infiltrating BPH tissues: 81% had T-lymphocytes markers, 52% had B-lymphocytes markers, and 82% had macrophages markers (2020. Robert G, Descazeaud A, Nicolaïew N, Terry S, Sirab N, Vacherot F, et al.: Inflammation in benign prostatic hyperplasia: a 282 patients' immunohistochemical analysis. Prostate. 2009; 69: 1774-80.). Therefore, in patients with high-grade prostatic inflammation IPSS score and prostate volume were significantly higher. These findings were confirmed by Mishra et al. (2121. Mishra VC, Allen DJ, Nicolaou C, Sharif H, Hudd C, Karim OM, et al.: Does intraprostatic inflammation have a role in the pathogenesis and progression of benign prostatic hyperplasia? BJU Int. 2007; 100: 327-31.), who compared pathology specimens in 374 patients who underwent transurethral resection of the prostate (TURP) for either LUTS or urinary retention. They found 70% of men with urinary retention have acute and/or chronic inflammation versus 45% of men without LUTS.
These data may support the hypothesis that an anti-inflammatory therapy may act to relief BPH symptoms and may also condition prostate tissue growth (2222. Sebastiano C, Vincenzo F, Tommaso C, Giuseppe S, Marco R, Ivana C, et al.: Dietary patterns and prostatic diseases. Front Biosci (Elite Ed). 2012; 4: 195-204.).
Among all phytotherapics, the lipidosterolic extract of Serenoa repens, a compound used to relief symptoms of BPH, had shown an anti-inflammatory activity modifying the production of leukotrienes and 5 hydroxyeicosatetraenoic acid, via the inhibition of the oxidative enzyme 5 lypoxygenase rather than phospholipase A2 or cell viability. Since the infiltration of inflammatory cells appears to have a role in BPH, inhibition of the production of chemotactic leukotrienes and other 5 lypoxygenase metabolites by Serenoa repens could be useful in BPH treatment (2323. Vela Navarrete R, Garcia Cardoso JV, Barat A, Manzarbeitia F, López Farré A: BPH and inflammation: pharmacological effects of Permixon on histological and molecular inflammatory markers. Results of a double blind pilot clinical assay. Eur Urol. 2003; 44: 549-55.).
Serenoa Repens, in a multicenter, open pilot study, was also evaluated for its effects on inflammatory markers. Tumor necrosis factor-α and IL-1b were dramatically lower in the Serenoa repens-treated group; both biological markers have been used as indicators of prostatic inflammation in cases of chronic prostatitis (2323. Vela Navarrete R, Garcia Cardoso JV, Barat A, Manzarbeitia F, López Farré A: BPH and inflammation: pharmacological effects of Permixon on histological and molecular inflammatory markers. Results of a double blind pilot clinical assay. Eur Urol. 2003; 44: 549-55.).
It has been hypothesized that SeR, Ly, and Se, administered together, might amplify their therapeutic efficacy on the proliferative and inflammatory component of BPH (2424. Magri V, Trinchieri A, Perletti G, Marras E: Activity of Serenoa repens, lycopene and selenium on prostatic disease: evidences and hypotheses. Arch Ital Urol Androl. 2008; 80: 65-78.).
The efficacy of this association was recently confirmed in an in vitro and in vivo comparison study performed on rats with partial bladder outlet obstruction: prostate pro-inflammatory phenotype, as well as hyperplasia, was reduced more efficiently than the single compounds (2525. Bonvissuto G, Minutoli L, Morgia G, Bitto A, Polito F, Irrera N, et al.: Effect of Serenoa repens, lycopene, and selenium on proinflammatory phenotype activation: an in vitro and in vivo comparison study. Urology. 2011; 77: 248.e9-16.).
Analyzing specimens from patients with high grade PIN and/or ASAP, a statistical significant reduction in the extension, and in the grading of the inflammatory cells infiltrate was demonstrated in the patients treated with SeR+Ly+Se (Group I).
Therefore, it was confirmed by immune-histochemical technique using monoclonal antibodies, that mononuclear cell infiltration (B-lymphocytes CD20, T-lymphocytes CD3-CD8 and macrophages CD68) is the most common pattern. SeR+Ly+Se combination therapy resulted in a statistical significant reduction of this inflammatory infiltrate.
The inflammatory infiltrates are responsible for the secretion of cytokines, which are involved in the paracrine and autocrine regulation of stromal and epithelial cell growth. This mechanism has been considered to influence the development of prostate cancer and BPH (2626. De Nunzio C, Kramer G, Marberger M, Montironi R, Nelson W, Schröder F, et al.: The controversial relationship between benign prostatic hyperplasia and prostate cancer: the role of inflammation. Eur Urol. 2011; 60: 106-17.): SeR+Se+Ly association acting on these pathway may be considered to chemoprevent both conditions.
According with the reduction of extension, grade of flogosis and CD20, CD3, CD8,CD68, mean PSA values decreased from 5.62 ± 1.04 to 4.16 ± 0.89 (p < 0.001), suggesting that PSA value could be an useful marker of prostate inflammation. This result was underlined also in a study from Li Gui-Zhong et al. Thus, if an elevated PSA level is considered in association with histological inflammation with detailed grading in a high number of biopsy specimens, it might prevent unnecessary repeated biopsies (2727. Gui-Zhong L, Libo M, Guanglin H, Jianwei W: The correlation of extent and grade of inflammation with serum PSA levels in patients with IV prostatitis. Int Urol Nephrol. 2011; 43: 295-301.).
The aim of the analysis performed in the Group II was to verify whether in patients with bladder outlet obstruction, waiting for TURP, SeR+Se+LY association determined the same effects observed in Group I.
Comparing the results with control group, there were no statistically significant differences in terms of reducing the extension and grading of inflammation.
As reported in several studies, the extent of inflammation and grade correlated positively with the serum PSA level (2828. Ozden C, Ozdal OL, Guzel O, Han O, Seckin S, Memis A: The correlation between serum prostate specific antigen levels and asymptomatic inflammatory prostatitis. Int Urol Nephrol. 2007; 39: 859-63.,2929. Kandirali E, Boran C, Serin E, Semercioz A, Metin A: Association of extent and aggressiveness of inflammation with serum PSA levels and PSA density in asymptomatic patients. Urology. 2007; 70: 743-7.). Probably in the Group II we have selected patients with lower extension and grade of flogosis: this finding is also supported by the fact that between the two subsets there were no statistical significant differences in terms of total PSA.
Analyzing the inflammatory infiltrate, surprisingly it has been documented a statistical significant reduction of CD20, CD3, CD8, CD68. In the study by Vela Navarrete et al., SeR alone showed a reduction of the biological markers (TNFα and IL-1β): however, the histological findings resulted in a reduction only in the number of lymphocytes B (CD20) (2323. Vela Navarrete R, Garcia Cardoso JV, Barat A, Manzarbeitia F, López Farré A: BPH and inflammation: pharmacological effects of Permixon on histological and molecular inflammatory markers. Results of a double blind pilot clinical assay. Eur Urol. 2003; 44: 549-55.).
Possible limits of this research could be represented by the lack of placebo controlling. A multicentre and randomized, double-blinded, placebo-controlled study could fill this gap and offer results that better clarify the activity of this category of treatment.
CONCLUSIONS
Our data support the anti-inflammatory activity of the combination of SeR+Se+LY in patients with histological inflammation detected on biopsy specimens. Patients with bladder outlet obstruction could benefit from this therapy on the inflammatory component of BPH. More data supporting these findings may confirm these evidences.
CONFLICT OF INTEREST
None declared.
Authors are grateful to University of Catania, University of Firenze, University of Roma Torvergata, University of Messina, Hospital of Bronte (Catania), Hospital “Buccheri La Ferla” (Palermo), Hospital of Napoli, Hospital of Avellino, and Israelitic Hospital (Rome) to have been part of the study. Authors also wish to thank Stefano Marventano for editing the manuscript.
REFERENCES
-
1Berry SJ, Coffey DS, Walsh PC, Ewing LL: The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132: 474-9.
-
2Miner M, Rosenberg MT, Perelman MA: Treatment of lower urinary tract symptoms in benign prostatic hyperplasia and its impact on sexual function. Clin Ther. 2006; 28: 13-25.
-
3Tang J, Yang J: Etiopathogenesis of benign prostatic hypeprlasia. Indian J Urol. 2009; 25: 312-7.
-
4Roehrborn CG, Kaplan SA, Noble WD: The impact of acute or chronic inflammation in baseline biopsy on the risk of clinical progression of BPE: Results from the MTOPS study. AUA Meeting 2005. J Urol, suppl., 2005; 173: 346, abstract 1277.
-
5Nickel JC, Roehrborn CG, O'Leary MP, Bostwick DG, Somerville MC, Rittmaster RS: The relationship between prostate inflammation and lower urinary tract symptoms: examination of baseline data from the REDUCE trial. Eur Urol. 2008; 54: 1379-84.
-
6Kramer G, Mitteregger D, Marberger M: Is benign prostatic hyperplasia (BPH) an immune inflammatory disease? Eur Urol. 2007; 51: 1202-16.
-
7Di Silverio F, Gentile V, De Matteis A, Mariotti G, Giuseppe V, Luigi PA, et al.: Distribution of inflammation, pre-malignant lesions, incidental carcinoma in histologically confirmed benign prostatic hyperplasia: a retrospective analysis. Eur Urol. 2003; 43: 164-75.
-
8Sciarra A, Di Silverio F, Salciccia S, Autran Gomez AM, Gentilucci A, Gentile V: Inflammation and chronic prostatic diseases: evidence for a link? Eur Urol. 2007; 52: 964-72.
-
9Comhaire F, Mahmoud A: Preventing diseases of the prostate in the elderly using hormones and nutriceuticals. Aging Male. 2004; 7: 155-69.
-
10Suzuki M, Ito Y, Fujino T, Abe M, Umegaki K, Onoue S, et al.: Pharmacological effects of saw palmetto extract in the lower urinary tract. Acta Pharmacol Sin. 2009; 30: 227-81.
-
11Buck AC: Is there a scientific basis for the therapeutic effects of serenoa repens in benign prostatic hyperplasia? Mechanisms of action. J Urol. 2004; 172: 1792-9.
-
12Diwadkar-Navsariwala V, Prins GS, Swanson SM, Birch LA, Ray VH, Hedayat S, et al.: Selenoprotein deficiency accelerates prostate carcinogenesis in a transgenic model. Proc Natl Acad Sci U S A. 2006; 103: 8179-84.
-
13Schwarz S, Obermüller-Jevic UC, Hellmis E, Koch W, Jacobi G, Biesalski HK: Lycopene inhibits disease progression in patients with benign prostate hyperplasia. J Nutr. 2008; 138: 49-53.
-
14Kandaş NO, Randolph C, Bosland MC: Differential effects of selenium on benign and malignant prostate epithelial cells: stimulation of LNCaP cell growth by noncytotoxic, low selenite concentrations. Nutr Cancer. 2009; 61: 251-64.
-
15Wertz K, Siler U, Goralczyk R: Lycopene: modes of action to promote prostate health. Arch Biochem Biophys. 2004; 430: 127-34.
-
16Obermüller-Jevic UC, Olano-Martin E, Corbacho AM, Eiserich JP, van der Vliet A, Valacchi G, et al.: Lycopene inhibits the growth of normal human prostate epithelial cells in vitro. J Nutr. 2003; 133: 3356-60.
-
17Nickel JC, True LD, Krieger JN, Berger RE, Boag AH, Young ID: Consensus development of a histopathological classification system for chronic prostatic inflammation. BJU Int. 2001; 87: 797-805.
-
18Kohnen PW, Drach GW: Patterns of inflammation in prostatic hyperplasia: a histologic and bacteriologic study. J Urol. 1979; 121: 755-60.
-
19Nickel JC, Downey J, Young I, Boag S: Asymptomatic inflammation and/or infection in benign prostatic hyperplasia. BJU Int. 1999; 84: 976-81.
-
20Robert G, Descazeaud A, Nicolaïew N, Terry S, Sirab N, Vacherot F, et al.: Inflammation in benign prostatic hyperplasia: a 282 patients' immunohistochemical analysis. Prostate. 2009; 69: 1774-80.
-
21Mishra VC, Allen DJ, Nicolaou C, Sharif H, Hudd C, Karim OM, et al.: Does intraprostatic inflammation have a role in the pathogenesis and progression of benign prostatic hyperplasia? BJU Int. 2007; 100: 327-31.
-
22Sebastiano C, Vincenzo F, Tommaso C, Giuseppe S, Marco R, Ivana C, et al.: Dietary patterns and prostatic diseases. Front Biosci (Elite Ed). 2012; 4: 195-204.
-
23Vela Navarrete R, Garcia Cardoso JV, Barat A, Manzarbeitia F, López Farré A: BPH and inflammation: pharmacological effects of Permixon on histological and molecular inflammatory markers. Results of a double blind pilot clinical assay. Eur Urol. 2003; 44: 549-55.
-
24Magri V, Trinchieri A, Perletti G, Marras E: Activity of Serenoa repens, lycopene and selenium on prostatic disease: evidences and hypotheses. Arch Ital Urol Androl. 2008; 80: 65-78.
-
25Bonvissuto G, Minutoli L, Morgia G, Bitto A, Polito F, Irrera N, et al.: Effect of Serenoa repens, lycopene, and selenium on proinflammatory phenotype activation: an in vitro and in vivo comparison study. Urology. 2011; 77: 248.e9-16.
-
26De Nunzio C, Kramer G, Marberger M, Montironi R, Nelson W, Schröder F, et al.: The controversial relationship between benign prostatic hyperplasia and prostate cancer: the role of inflammation. Eur Urol. 2011; 60: 106-17.
-
27Gui-Zhong L, Libo M, Guanglin H, Jianwei W: The correlation of extent and grade of inflammation with serum PSA levels in patients with IV prostatitis. Int Urol Nephrol. 2011; 43: 295-301.
-
28Ozden C, Ozdal OL, Guzel O, Han O, Seckin S, Memis A: The correlation between serum prostate specific antigen levels and asymptomatic inflammatory prostatitis. Int Urol Nephrol. 2007; 39: 859-63.
-
29Kandirali E, Boran C, Serin E, Semercioz A, Metin A: Association of extent and aggressiveness of inflammation with serum PSA levels and PSA density in asymptomatic patients. Urology. 2007; 70: 743-7.
Publication Dates
-
Publication in this collection
Mar-Apr 2013
History
-
Received
10 Oct 2012 -
Accepted
15 Jan 2013