ABSTRACT
Purpose:
In this study we aimed to review urological soft tissue sarcomas of genitourinary tract that were diagnosed in our institution and their prognostic factors for survival.
Materials and Methods:
The clinical and pathological records of 31 patients who had diagnosis of soft tissue sarcomas primarily originating from the genitourinary tract between 2005-2011 were reviewed.
Results:
The most common site was kidney (17 cases, 54.8%), and most common diagnosis was leiomyosarcoma (11 cases, 35.4%). A total of 24 patients (77.4%) had surgical excision. The surgical margins were positive in 7 patients who presented with local recurrence after primary resection. Twelve patients developed metastatic disease. During follow-up (range 9-70 month), 26 of the 31 patients (88.9%) were alive. Significant survival differences were found according to histological type (p: 0.001), with lower survival rates for malignant fibrous histiocytoma. The tumor size, the presence of metastasis at the time of diagnosis and tumor localization were not statistically significant for overall survival.
Conclusions:
In our series, prostate sarcomas, paratesticular rhabdomyosarcoma and malignant fibrous histiocytoma had poor prognosis, especially in patients presenting with metastatic disease.
Keywords:
Genitourinary Tract Anomalies[Supplementary Concept]; Sarcoma; Survival
INTRODUCTION
Soft tissue sarcomas (STSs) are a diverse group of solid tumors that originate from embryonic mesenchymal cells which have various clinical and pathological characteristics (11. Russo P, Brady MS, Conlon K, Hajdu SI, Fair WR, Herr HW, et al. Adult urological sarcoma. J Urol. 1992;147:1032-6.). STSs of the genitourinary (GU) tract are uncommon, only accounting for 2.1% of all STSs and 1% to 2% of all malignant GU tumors (22. Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212-36., 33. Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, Ghafoor A, et al. Cancer statistics, 2005. CA Cancer J Clin. 2005;55:10-30. Erratum in: CA Cancer J Clin. 2005;55:259.). Due to low prevalence of urological STS, clinical research is limited with institution-based studies. The tumor stage, grade, size, and localization are found to be important prognostic factors for patient survival in STSs in several studies (44. Mondaini N, Palli D, Saieva C, Nesi G, Franchi A, Ponchietti R, et al. Clinical characteristics and overall survival in genitourinary sarcomas treated with curative intent: a multicenter study. Eur Urol. 2005;47:468-73.
5. Stojadinovic A, Leung DH, Allen P, Lewis JJ, Jaques DP, Brennan MF. Primary adult soft tissue sarcoma: time-dependent influence of prognostic variables. J Clin Oncol. 2002;20:4344-52.-66. Dotan ZA, Tal R, Golijanin D, Snyder ME, Antonescu C, Brennan MF, et al. Adult genitourinary sarcoma: the 25-year Memorial Sloan-Kettering experience. J Urol. 2006;176:2033-8.). In this study, we aimed to review urological STS that were diagnosed in our institution and their prognostic factors for survival.
MATERIALS AND METHODS
The clinical and pathological records of 31patients who had diagnosis of soft tissue sarcomas primarily originating from the genitourinary tract between 2005-2011 were reviewed. Sarcomas of the GU tract that arised from the kidney, ureter, bladder, prostate, and paratesticular region were included. Retroperitoneal sarcomas without a tight relationship to the kidney or to the adrenal gland were excluded. Female genital organ related sarcomas were excluded from this study. Characteristics of the patients including age, sex, tumor histology, tumor size, primary organ, metastasis at diagnosis, and status of surgical resection were examined. All histopathological findings were obtained from biopsy or surgically resected specimens from files of patients in the Department of Pathology. Local recurrence or metastasis was described as the first recurrence of disease at the primary tumor site or distant site detected by computed tomography. The clinical characteristics of the patients at the time of admission and follow-up were achieved from hospital records, directly from the patients or from their families. All patients underwent CT scan before surgery. Recurrence was defined as recurrent disease at a local or distant site.
Statistical analysis was done by using the Statistical Package for Social Sciences, ver. 13.0 for Windows, (SPSS, Chicago, IL). The crude probability of survival was estimated by using the Kaplan - Meier method and differences between patient groups were assessed by the log rank test. A P value < 0.05 was considered to be statistically significant.
RESULTS
The demographic characteristics of the patients are presented in Table-1. The mean age at diagnosis was 58 years (range, 19-81 years). Median follow-up was 61 months. Twenty two patients were male and 9 patients were female. The most common site was kidney (17 cases, 54.8%), followed by paratesticular region with 7 cases (7 cases, 22.5%), prostate (4 cases, 12.9%) and bladder (3 cases, 9.8%). The mean tumor diameter was 14 cm. The most common diagnosis was leiomyosarcoma (11 cases, 35.4%), followed by liposarcoma (8 cases, 25.8%), malignant fibrous histiocytoma, (4 cases,12.9%), malignant nerve sheath tumor (3 cases, 9.7%), rhabdomyosarcoma (2 cases,6.5%) and Kaposi sarcoma (2 cases, 6.5%). A total of 24 patients (77.4%) out of 31 patients had surgical excision. The surgical margins were positive in 7 patients who presented with local recurrence after primary resection. Twelve patients developed metastatic disease. There were lymph node metastasis in 2 patients and distant metastasis in 10 patients; lung, liver and bones were the most affected sites. At the end of the study period (range 9-70 month), 26 of the 31 patients (88.9%) were alive.
Distribution of 31 genitourinary sarcomas according to selected clinical and pathological characteristics.
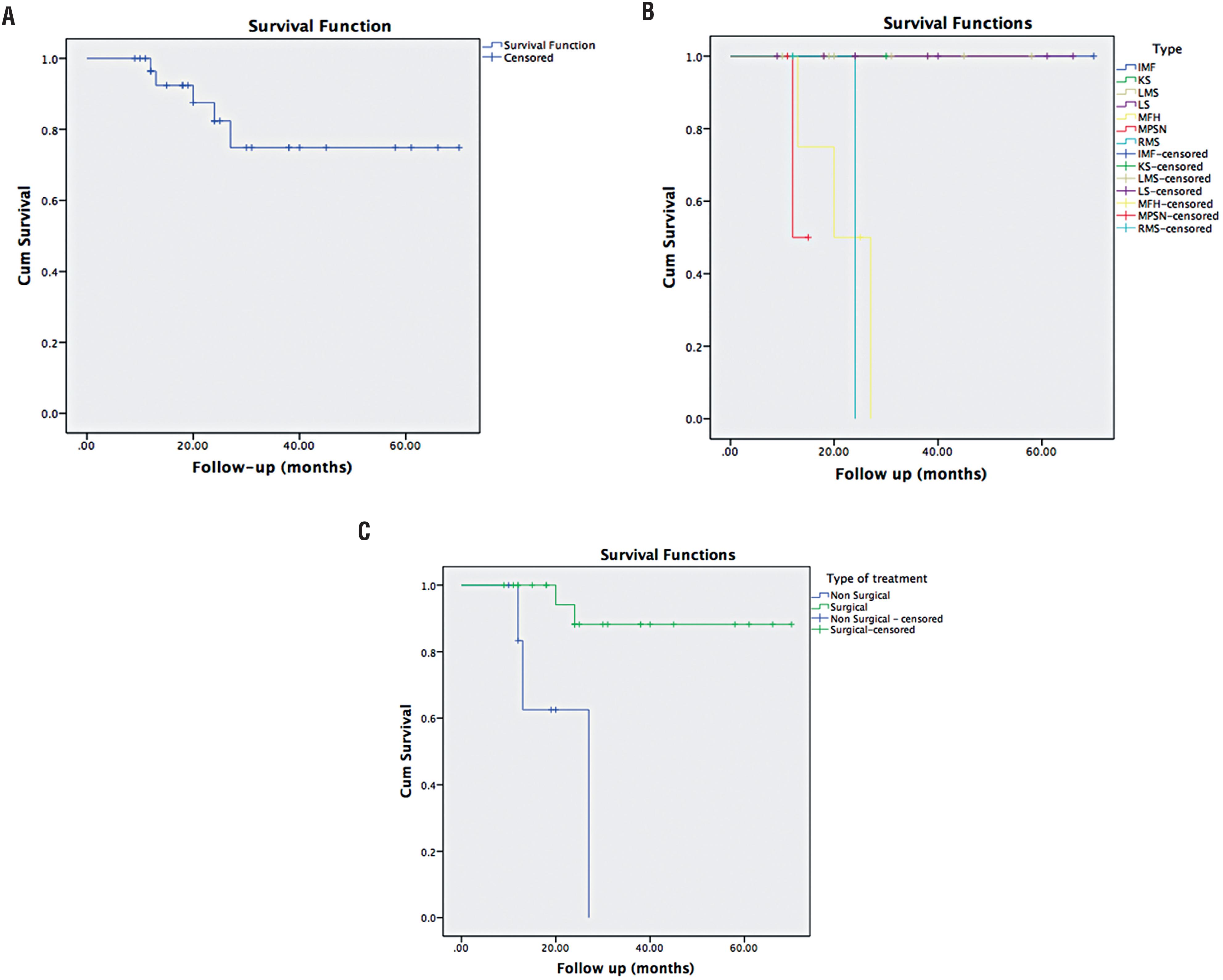
There were no significant differences in survival according to sex and age (p: 0.717, p: 0.107 respectively) (Figure-1A). Significant survival differences were found according to histological type (p: 0.001), with lower survival rates for malignant fibrous histiocytoma (Figure-1B). Leiomyosarcomas and liposarcomas had a better 5 years survival when compared to rhabdomyosarcomas and other types. The tumor size and the presence of metastasis at the time of diagnosis were not statistically significant for overall survival (p: 0.590, p: 0.500 respectively). There were no relation with tumor localization and survival (p: 0.449). The patients who underwent surgical resection had significantly higher rates of survival (p: 0.001), (Figure-1C).
Kaplan-Meier analysis of overall survival in overall cases (A), according to histological subtype (B) according to presence vs. absence of surgical resection (C).
DISCUSSION
The infrequency of GU STSs is the main problem for clinical research while data in the literature are limited (77. Lee G, Lee SY, Seo S, Jeon S, Lee H, Choi H, et al. Prognostic factors and clinical outcomes of urological soft tissue sarcomas. Korean J Urol. 2011;52:669-73.). In the literature, liposarcoma (LS) represents the most common soft tissue sarcoma of retroperitoneum (88. Bautista N, Su W, O’Connell TX. Retroperitoneal soft-tissue sarcomas: prognosis and treatment of primary and recurrent disease. Am Surg. 2000;66:832-6.). The biological behavior and prognosis of LS are usually more favorable compared to most of STS but the prognosis can vary widely depending on tumor characteristics, especially histological subtype and tumor grade (99. Nijhuis PH, Sars PR, Plaat BE, Molenaar WM, Sluiter WJ, Hoekstra HJ. Clinico-pathological data and prognostic factors in completely resected AJCC stage I-III liposarcomas. Ann Surg Oncol. 2000;7:535-43.). In our study, 6 patients had perirenal and renal LS. Renal LSs were found in renal parenchyma without being in renal lipomatous tissue. While 4 patients had no evidence of local recurrence, one patient had a local recurrence and one patient had an adrenal metastasis. One patient had a bladder LS. Primary LS of the urinary bladder is a very rare entity with a poor prognosis that usually presents as a large tumor mass (1010. Veiga González M, Fresno Forcelledo MF, Pérez del Río MJ, Madrigal Rosales B, Vara Gastrodeza A, Herrero Zapatero A. [Primary round-cell liposarcoma of the bladder]. Arch Esp Urol. 1998;51:925-8.). Our patient had no evidence of disease in 66 months follow-up. One patient had a paratesticular LS and had lung metastasis.
Leiomyosarcoma (LMS) make up 50-60% of all renal sarcomas, therefore, it is the most common histologic subtype (1111. Beccia DJ, Elkort RJ, Krane RJ. Adjuvant chemotherapy in renal leiomyosarcoma. Urology. 1979;13:652-4.). Renal LMS has a very poor prognosis, which results in death of the majority of patients within two years (1212. Srinivas V, Sogani PC, Hajdu SI, Whitmore WF Jr. Sarcomas of the kidney. J Urol. 1984;132:13-6.). However, radical surgery seems to offer the best chance of cure. The role of adjuvant chemotherapy and / or radiotherapy remains controversial due to the paucity of data on the treatment of this rare renal neoplasm. While local recurrence is common, low-grade LMS tends to pursue a more indolent course. Four of our patients had LMS of the kidney. All patients had no evidence of local recurrence but distant metastasis was noted in adrenal and lymph node during of follow-up. Two of our patients had perirenal LMS. Their origin has been suggested as coming from the interlacing bundles of smooth muscle in the inner layer of the renal capsule (1313. Ng WD, Chan KW, Chan YT. Primary leiomyosarcoma of renal capsule. J Urol. 1985;133:834-5.) and in the form of a mass attached to the cortical surface of the kidney. One of these patients had distant metastasis in liver and bone. Three of our patients had LMS of the prostate. LMS is the most common primary sarcoma of the prostate in adults and accounts for 38-52% of primary prostatic sarcomas (1414. Sexton WJ, Lance RE, Reyes AO, Pisters PW, Tu SM, Pisters LL. Adult prostate sarcoma: the M. D. Anderson Cancer Center Experience. J Urol. 2001;166:521-5.). It has an aggressive clinical course (1515. Cheville JC, Dundore PA, Nascimento AG, Meneses M, Kleer E, Farrow GM, et al. Leiomyosarcoma of the prostate. Report of 23 cases. Cancer. 1995;76:1422-7.). Due to the rarity of prostatic LMS, definite treatment recommendations are yet to be established. Multimodality treatment combinations including surgery, preoperative or postoperative radiation therapy and neoadjuvant or adjuvant chemotherapy has been used (1414. Sexton WJ, Lance RE, Reyes AO, Pisters PW, Tu SM, Pisters LL. Adult prostate sarcoma: the M. D. Anderson Cancer Center Experience. J Urol. 2001;166:521-5., 1515. Cheville JC, Dundore PA, Nascimento AG, Meneses M, Kleer E, Farrow GM, et al. Leiomyosarcoma of the prostate. Report of 23 cases. Cancer. 1995;76:1422-7.). Up to a third of patients have demonstrable metastases at presentation, usually to the lung, and sometimes to the liver (1414. Sexton WJ, Lance RE, Reyes AO, Pisters PW, Tu SM, Pisters LL. Adult prostate sarcoma: the M. D. Anderson Cancer Center Experience. J Urol. 2001;166:521-5., 1515. Cheville JC, Dundore PA, Nascimento AG, Meneses M, Kleer E, Farrow GM, et al. Leiomyosarcoma of the prostate. Report of 23 cases. Cancer. 1995;76:1422-7.). In our series, three patients, who had LMS, received adjuvant radiotherapy and multi-agent chemotherapy. All of them had distant metastasis in lung and bone.
Malignant fibrous histiocytoma (MFH) is rare in the urinary tract and mostly it is located in the kidneys and consists of 0.23-0.67% of all bladder tumors. In our series, the tumors were localized in kidney, prostate, and bladder. MFH usually spreads fast. The size, depth and histologic features of the tumor are important factors for metastasis (1616. Kunze E, Theuring F, Krüger G. Primary mesenchymal tumors of the urinary bladder. A histological and immunohistochemical study of 30 cases. Pathol Res Pract. 1994;190:311-32.). Despite this treatment, 3-year survival is approximately 40% (1717. Celik O, Turk H, Budak S, Ilbey YO. Rare type of bladder cancer: malign fibrous histiocytoma. Arch Ital Urol Androl. 2014;86:158-9.). In our series a patient, who had MFH, underwent surgery, received adjuvant radiotherapy and multiagent chemotherapy, but died 20 months after initial diagnosis.
Two patients in our series had paratesticular rhabdomyosarcoma (RMS), which can arise from the epididymis, the mesenchymal layers surrounding the testis and its true appendages, and the spermatic cord. It is the most common primary paratesticular malignant neoplasm diagnosed in patients aged 7 years to 36 years, with a mean age of 10 years (1818. Moroni M, Nesi G, Travaglini F, Rizzo M, Amorosi A, Dominici A. Rhabdomyosarcoma of the spermatic cord. A case report with review of the literature. Urol Int. 2003;71:114-7.). With regard to pathological sub classification, these tumors were of embryonal and pleomorphic type, respectively. The patients in our series were treated by radical orchiectomy. Retroperitoneal lymphadenectomy or chemotherapy was not performed. One of our cases was found to have embryonal RMS. Although he underwent radical orchiectomy and had post-operative chemotherapy, he had distant metastasis in lung and liver. Another case had no evidence of local recurrence.
Malignant peripheral nerve sheath tumors (MPNST) are confirmed only by histological and immunohistochemically evaluation (1919. Williams SB, Szlyk GR, Manyak MJ. Malignant peripheral nerve sheath tumor of the kidney. Int J Urol. 2006;13:74-5.). Involvement of the kidney is uncommon, and it is very difficult to differentiate with other kidney sarcomas from MPNSTs clinically or upon gross examination (2020. Khandelwal A, Gupta A, Khandelwal K. Malignant peripheral nerve sheath tumor of kidney. Iran J Kidney Dis. 2011;5:373., 2121. Grobmyer SR, Reith JD, Shahlaee A, Bush CH, Hochwald SN. Malignant Peripheral Nerve Sheath Tumor: molecular pathogenesis and current management considerations. J Surg Oncol. 2008;97:340-9.). Current treatment for MPNST in the genitourinary system involves surgical excision and adjuvant chemotherapy. This combined modality approach results in a 5-year survival rate of 40-69% with complete resection of localized disease (2222. Voznesensky MA, Yamase H, Taylor JA 3rd. Malignant peripheral nerve sheath tumor of the renal pelvis. Urol Int. 2009;83:370-2.). Two patients out of three had a poor outcome: one was dead from the disease and the other is alive with the metastatic disease.
In conclusion, genitourinary sarcomas are a rare group of tumors, some patients with localized resectable masses may have a favorable prognosis. Complete surgical resection is the best chance for survival. Prostate sarcomas, paratesticular RMS, and MFH had a poor prognosis, especially in patients presenting with metastatic disease and combined multimodality approach is the treatment of choice all of them; unfortunately, it provides limited therapeutic benefit.
REFERENCES
-
1Russo P, Brady MS, Conlon K, Hajdu SI, Fair WR, Herr HW, et al. Adult urological sarcoma. J Urol. 1992;147:1032-6.
-
2Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212-36.
-
3Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, Ghafoor A, et al. Cancer statistics, 2005. CA Cancer J Clin. 2005;55:10-30. Erratum in: CA Cancer J Clin. 2005;55:259.
-
4Mondaini N, Palli D, Saieva C, Nesi G, Franchi A, Ponchietti R, et al. Clinical characteristics and overall survival in genitourinary sarcomas treated with curative intent: a multicenter study. Eur Urol. 2005;47:468-73.
-
5Stojadinovic A, Leung DH, Allen P, Lewis JJ, Jaques DP, Brennan MF. Primary adult soft tissue sarcoma: time-dependent influence of prognostic variables. J Clin Oncol. 2002;20:4344-52.
-
6Dotan ZA, Tal R, Golijanin D, Snyder ME, Antonescu C, Brennan MF, et al. Adult genitourinary sarcoma: the 25-year Memorial Sloan-Kettering experience. J Urol. 2006;176:2033-8.
-
7Lee G, Lee SY, Seo S, Jeon S, Lee H, Choi H, et al. Prognostic factors and clinical outcomes of urological soft tissue sarcomas. Korean J Urol. 2011;52:669-73.
-
8Bautista N, Su W, O’Connell TX. Retroperitoneal soft-tissue sarcomas: prognosis and treatment of primary and recurrent disease. Am Surg. 2000;66:832-6.
-
9Nijhuis PH, Sars PR, Plaat BE, Molenaar WM, Sluiter WJ, Hoekstra HJ. Clinico-pathological data and prognostic factors in completely resected AJCC stage I-III liposarcomas. Ann Surg Oncol. 2000;7:535-43.
-
10Veiga González M, Fresno Forcelledo MF, Pérez del Río MJ, Madrigal Rosales B, Vara Gastrodeza A, Herrero Zapatero A. [Primary round-cell liposarcoma of the bladder]. Arch Esp Urol. 1998;51:925-8.
-
11Beccia DJ, Elkort RJ, Krane RJ. Adjuvant chemotherapy in renal leiomyosarcoma. Urology. 1979;13:652-4.
-
12Srinivas V, Sogani PC, Hajdu SI, Whitmore WF Jr. Sarcomas of the kidney. J Urol. 1984;132:13-6.
-
13Ng WD, Chan KW, Chan YT. Primary leiomyosarcoma of renal capsule. J Urol. 1985;133:834-5.
-
14Sexton WJ, Lance RE, Reyes AO, Pisters PW, Tu SM, Pisters LL. Adult prostate sarcoma: the M. D. Anderson Cancer Center Experience. J Urol. 2001;166:521-5.
-
15Cheville JC, Dundore PA, Nascimento AG, Meneses M, Kleer E, Farrow GM, et al. Leiomyosarcoma of the prostate. Report of 23 cases. Cancer. 1995;76:1422-7.
-
16Kunze E, Theuring F, Krüger G. Primary mesenchymal tumors of the urinary bladder. A histological and immunohistochemical study of 30 cases. Pathol Res Pract. 1994;190:311-32.
-
17Celik O, Turk H, Budak S, Ilbey YO. Rare type of bladder cancer: malign fibrous histiocytoma. Arch Ital Urol Androl. 2014;86:158-9.
-
18Moroni M, Nesi G, Travaglini F, Rizzo M, Amorosi A, Dominici A. Rhabdomyosarcoma of the spermatic cord. A case report with review of the literature. Urol Int. 2003;71:114-7.
-
19Williams SB, Szlyk GR, Manyak MJ. Malignant peripheral nerve sheath tumor of the kidney. Int J Urol. 2006;13:74-5.
-
20Khandelwal A, Gupta A, Khandelwal K. Malignant peripheral nerve sheath tumor of kidney. Iran J Kidney Dis. 2011;5:373.
-
21Grobmyer SR, Reith JD, Shahlaee A, Bush CH, Hochwald SN. Malignant Peripheral Nerve Sheath Tumor: molecular pathogenesis and current management considerations. J Surg Oncol. 2008;97:340-9.
-
22Voznesensky MA, Yamase H, Taylor JA 3rd. Malignant peripheral nerve sheath tumor of the renal pelvis. Urol Int. 2009;83:370-2.
Publication Dates
-
Publication in this collection
Jan-Feb 2019
History
-
Received
22 Jan 2018 -
Accepted
13 May 2018 -
Published
10 June 2018