Abstract
OBJECTIVE:
To determine how early musculoskeletal disorders (MSDs) develop in dental professionals and to explore the potential differences among distinct dental specialties.
MATERIAL AND METHODS:
271 dental postgraduates majoring in five dental specialties were recruited, i.e., orthodontics, prosthodontics, endodontics, periodontics and alveolar surgery. 254 age-matched non-dental postgraduates served as the control. The standardized Nordic questionnaire on MSDs and a self-report questionnaire regarding correlative factors (only for dental postgraduates) were answered through emails. Reliability of responses was assessed applying test-retest method.
RESULTS:
The intraclass correlation coefficient of participants' answers ranged from 0.89 to 0.96. Dental postgraduates had significantly higher prevalence of MSDs than the control group, especially at neck, upper back and lower back. In all dental specialties included, high prevalence of MSDs was reported at neck (47.5%-69.8%), shoulders (50.8%-65.1%), lower back (27.1%-51.2%) and upper back (25.6%-46.5%), with lower prevalence at elbows (5.1%-18.6%), hips (3.4%-16.3%) and ankles (5.1%-11.6%). Periodontics students reported the worst MSDs in most body regions except wrists and knees, which were more prevalent for prosthodontic and alveolar surgery students, respectively. Furthermore, year of clinical work, clinical hours per week and desk hours per week were found as risk factors for MSDs, whereas physical exercise and rest between patients as protective factors.
CONCLUSIONS:
High and specialty-related MSDs afflict dental professionals even since very early stage of careers. Prevention aimed at the specialty-related characteristics and the risk/protective factors revealed in this study should be introduced to dental personnel as early as possible.
Occupational health; Musculoskeletal diseases; Specialty; Dentists; Dental education
INTRODUCTION
The nature of dental clinical work could predispose dentists to diverse occupational hazards88- Fasunloro A, Owotade FJ. Occupational hazards among clinical dental staff. J Contemp Dent Pract. 2004;5:134-52., among which musculoskeletal disorders (MSDs) have been most frequently reported22- Akesson I, Johnsson B, Rylander L, Moritz U, Skerfving S. Musculoskeletal disorders among female dental personnel: clinical examination and a 5-year follow-up study of symptoms. Int Arch Occup Environ Health. 1999;72:395-403. , 33- Anton D, Rosecrance J, Merlino L, Cook T. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am J Ind Med. 2002;42:248-57. , 99- Finsen L, Christensen H, Bakke M. Musculoskeletal disorders among dentists and variation in dental work. Appl Ergon. 1998;29:119-25. , 1717- Oberg T, Oberg U. Musculoskeletal complaints in dental hygiene: a survey study from a Swedish county. J Dent Hyg. 1993;67:257-61.. In typical clinical settings, dental practitioners frequently adopt unfavorable postures characterized by neck flexion, side bend and rotation, and shoulder abduction for better view and easier access to the oral cavity2020- Smith CA, Sommerich CM, Mirka GA, George MC. An investigation of ergonomic interventions in dental hygiene work. Appl Ergon. 2002;33:175-84.. This static and awkward posture as well as repetitive movements, high prehension forces, and long work duration has been identified as the biomechanical risk factor associated with the development of MSDs among dentists1919- Sanders M, Turcotte C. Ergonomic strategies for dental professionals. Work. 1997;8:55-72., which compromises their health and even causes dropout from dental careers88- Fasunloro A, Owotade FJ. Occupational hazards among clinical dental staff. J Contemp Dent Pract. 2004;5:134-52..
While most musculoskeletal symptoms could be relieved by proper preventive strategies, especially before chronic damages have been done1818- Ranney D. Work-related chronic injuries of the forearm and hand: their specific diagnosis and management. Ergonomics. 1993;36:871-80., current studies indicate that effective preventive methods are still lacking44- Beach JC, DeBiase CB. Assessment of ergonomic education in dental hygiene curricula. J Dent Educ. 1998;62:421-5.. This could be caused by the inadequate understanding of MSDs per se. In fact, though numerous reports suggest its high prevalence88- Fasunloro A, Owotade FJ. Occupational hazards among clinical dental staff. J Contemp Dent Pract. 2004;5:134-52., few have explored how early MSDs develop in dental careers, which could hinder the application of preventive methods. Cumulative work duration of dental students, who are at the beginning of dental careers, is shorter than dentists. Nevertheless, the same clinical tasks, more uncomfortable postures due to their inexperience, lack of self-protect awareness11- Abreu MH, Lopes-Terra MC, Braz LF, Rimulo AL, Paiva SM, Pordeus IA. Attitudes and behavior of dental students concerning infection control rules: a study with a 10-year interval. Braz Dent J. 2009;20:221-5. , 2222- Yüzbasioglu E, Saraç D, Canbaz S, Saraç YS, Cengiz S. A survey of cross-infection control procedures: knowledge and attitudes of Turkish dentists. J Appl Oral Sci. 2009;17:565-9.and gradually cumulated exposure to clinical tasks could promote MSDs in the early period of careers. To help prevent MSDs and minimize the negative effect, further studies of the above issue are needed.
Moreover, working postures and duration which are causally related to MSDs vary in distinct specialties. For example, most orthodontic procedures only require a view of buccal surfaces of teeth (with lingual orthodontics as an exception) while the view of pulp cavity is required for endodontists. Another example, most tooth extraction is a short and brisk exertion of force, whereas prosthodontic treatment usually comprises longer and repeated motion. Hence, MSDs could vary among different specialties, which, to the best of our knowledge, has never been reported.
Therefore, we develop this survey to investigate MSDs in dental students of distinct specialties in China. The aim of this study is to evaluate MSDs in the early stage of dental careers and to explore the potential differences of MSDs among distinct specialties.
MATERIAL AND METHODS
Two groups, i.e., the dental and non-dental postgraduates were recruited from Sichuan University, China. The dental postgraduates (n=327) were volunteers recruited from 5 dental specialties, including orthodontics, prosthodontics, endodontics, periodontics and alveolar surgery. They had received general dental training in the last undergraduate year, and had sticked to their specialties as postgraduates for at least 1 year. The non-dental postgraduates (n=350) were volunteers proportionally recruited from 26 non-dental and non-medical specialties, including economics, literature, chemistry, and so on. All the subjects had no idea about the purpose of the investigation.
The standardized Nordic questionnaire1111- Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering- Sørensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233-7.was used to investigate the prevalence, frequency and impact of musculoskeletal symptoms in different anatomical regions. Briefly, the frequencies of MSDs were categorized as "never" (negative MSDs); or "everyday" (ED), at least once in the "last week" (LW), "last month" (LM) or "last year" (LY). Numbers of ED, LW, LM and LY were summed as positive MSDs, based on which the prevalence of MSDs was calculated. The impacts of MSDs were categorized as "no interference"(N), "work activities reduced"(W), "leisure activities reduced" (L), or "treatment sought" (T). An accompanying self-report questionnaire was designed to collect personal information of the dental postgraduates including specialty, gender, age, year of clinical work, etc. A small-scale pilot study has previously been done to evaluate the effectiveness and reliability of the accompanying questionnaire (data not shown). An email was sent to the students, asking them to fill in the informed consent form, and answer the standardized Nordic questionnaire, and the self-report questionnaire (for the dental postgraduates only). Three weeks later, the same questionnaires were emailed to 40 randomly selected subjects (20 dental and 20 non-dental postgraduates) to assess the reliability of the responses. Throughout the study, an official email account from the postgraduate institute has been used for contact, so that the identities of the researchers have been kept in dark to the students1515- Martins Junior RL, Kerber FC, Stuginski-Barbosa J. Attitudes of a group of Brazilian orthodontists towards the diagnosis and management of primary headache (migraine): an electronic-based survey. J Appl Oral Sci. 2011;19:674-8..
The chi-square test was utilized to examine the differences of MSDs prevalence between the dental and control group, and the differences among distinct dental specialties. The Wilcoxon rank-sum test was employed to compare the frequency and impact of MSDs among dental specialties. The logistic regression was used to reveal the association between prevalence of MSDs and exposure variables among dental postgraduates. All analyses were conducted using SPSS 13.0.
The study protocol has been approved by West China Hospital of Stomatology Institute Review Board in Jul. 2012. The Approval ID is WCHSIRB-D-2012-033.
RESULTS
A total of 288 dental postgraduates and 279 other postgraduates responded respectively. The researchers excluded 17 responses of dental students and 25 responses from the control group due to previous injuries/diseases which could induce musculoskeletal symptoms, inadequate clinical hours per week (<4 hours), information loss or misunderstanding of questions. Altogether, 254 questionnaires of the control group and 271 questionnaires of the dental group (2.78±1.57 years of clinical experience) including 58 from students in orthodontics, 59 in prosthodontics, 68 in endodontics, 43 in periodontics and 43 in alveolar surgery, were subjected to statistical analysis. In the reliability test, responses of participants showed a high consistency. The intraclass correlation coefficient (ICC) ranged from 0.89 to 0.96.
MSDs of dental personnel and other professionals
In general, 85.6% dental postgraduates experienced positive MSDs in at least one anatomic region, which was significantly higher than other professionals (70.4%). With regarding to specific regions, dental postgraduates experienced more MSDs in neck, upper back and lower back, while less in ankles with significance (P<0.05). No differences were observed in other regions (Figure 1).
Musculoskeletal disorders (MSDs) prevalence at various anatomical regions in the dental and non-dental postgraduate groups. MSDs prevalence is calculated as the ratio of positive MSDs (ED+LW+LM+LY) number to the total number *P<0.05
Body locations of musculoskeletal symptoms in distinct dental specialties
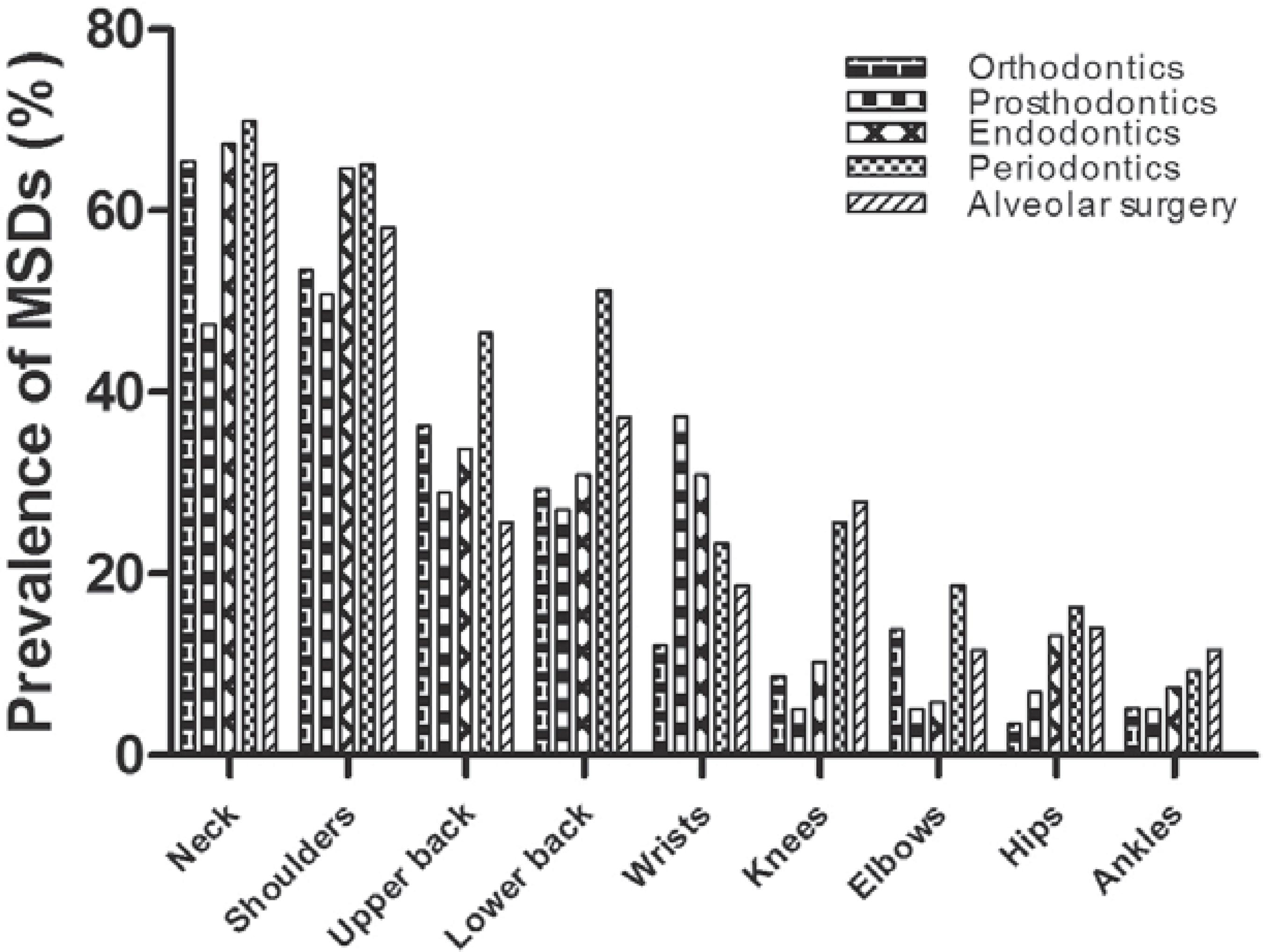
Shoulders (50.8%-65.1%), neck (47.5%-69.8%), upper back (25.6%-46.5%) and lower back (27.1%-51.2%) were the regions most commonly reported with MSDs. In these four regions, periodontic students reported the highest prevalence, while prosthodontic students reported the lowest, though no significant differences were observed. All specialties reported low MSDs in elbows (5.1%-18.6%), hips (3.4%-16.3%) and ankles (5.1%-11.6%), and no significant differences among specialties were detected (Figure 2, Table 1).
Musculoskeletal disorders (MSDs) prevalence at various regions in different dental specialties
However, differences were observed in wrists and knees. These two regions were thus further analyzed to detect where the difference existed at an adjusted significance level (α') of 0.0052 according to the formula (m=k*(k-1)/2, α'=1- , k=5 that represented five specialties) 1414- Li X. Medical statistics. 2nd ed. Beijing: Higher Education Press; 2008. . Prosthodontic students had the highest rate of wrist symptom (22, 37.3%), significantly higher than orthodontic students (7, 12.1%). The highest prevalence of knee disorders was reported by alveolar surgery students (12, 27.9%), significantly higher than prosthodontic students (3, 5.1%) (Table 2).
Frequency and impact of musculoskeletal symptoms
The four regions reported with high rate of MSDs (neck, shoulders, upper back and lower back) and the two regions detected with differences among specialties were further analyzed. The suffering of MSDs among dental specialties was summarized in Figure 3. The frequencies were categorized as "everyday" (ED), at least once in the "last week" (LW), "last month" (LM) or "last year" (LY). The influences were categorized as "no interference" (N), "work activities reduced" (W), "leisure activities reduced" (L), or "treatment sought" (T). Consistent with our findings of the prevalence, periodontic students reported more severe symptoms in neck, upper back and lower back. In terms of wrists and knees, more severe symptoms were reported by prosthodontic students and alveolar students, respectively.
Frequency and impact of Musculoskeletal disorders (MSDs) in different dental specialties The frequencies were categorized as "everyday" (ED), at least once in the "last week" (LW), "last month" (LM) or "last year” (LY). The impacts were categorized as "no interference" (N), "work activities reduced" (W), "leisure activities reduced" (L), or "treatment sought" (T) .a, b, c and d, compared to orthodontists, prosthodontics, endodontics and alveolar surgery respectively (P<0.05)
Risk factors for musculoskeletal symptoms
Tables 3 and 4 summarized variables that were associated with the prevalence of MSDs significantly. Year of clinical work and exercise time per week correlated with the presence of MSDs in orthodontic, prosthodontic and periodontic students. Those students with more than four years of clinical experience (OR: 3.46, 95%CI: 1.27-9.42; OR: 2.71, 95% CI: 1.49-4.93) were more likely to develop MSDs, and those students with less than two years of clinical experience reported fewer symptoms (OR: 0.64, 95% CI: 0.43-0.95). Work time per week was also influential. Orthodontic students who undertook 16-20 hours of clinical work per week (OR: 2.62, 95% CI: 1.34-5.14) suffered a higher prevalence, which was the same case for endodontic students (OR: 3.11, 95% CI: 1.50-6.37). Rest between patients and physical exercise showed protective effect from the development of MSDs. Periodic rest negatively associated with MSDs in prosthodontics (OR: 1.41, 95% CI: 1.26-1.59) and alveolar surgery (OR: 2.14, 95% CI: 1.48-3.11). 6-8 hours spent on exercise per week (OR: 0.53, 95% CI: 0.30-0.94) reduced the prevalence of MSDs, and weekly exercise less than 1 hour (OR: 1.83, 95% CI: 1.13-2.95) was significantly associated with higher prevalence. In combination of data regarding periodontics and alveolar surgery, it was indicated that female students may have a higher risk to develop MSDs (OR: 1.37, 95%CI: 1.04-1.73; OR: 1.15, 95%CI: 1.07-1.26).
DISCUSSION
This study, to the best of our knowledge, is the first that reports different disease patterns of MSDs suffered by dental professionals of distinct specialties, particularly with a focused scrutiny on the early development of MSDs.
There are 85.6% dental postgraduates complaining at least one anatomic region with musculoskeletal symptoms, significantly higher than the control group (70.4%). Together with higher prevalence in neck, upper back and lower back reported by dental postgraduates, it is suggested that, compared to the general population, higher MSDs afflict dental personnel. This could mainly be due to the more uncomfortable postures they assume to undertake during work.
The prevalence of MSDs in dental postgraduates in our study is similar to the results of other findings regarding dentists22- Akesson I, Johnsson B, Rylander L, Moritz U, Skerfving S. Musculoskeletal disorders among female dental personnel: clinical examination and a 5-year follow-up study of symptoms. Int Arch Occup Environ Health. 1999;72:395-403. , 33- Anton D, Rosecrance J, Merlino L, Cook T. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am J Ind Med. 2002;42:248-57. , 88- Fasunloro A, Owotade FJ. Occupational hazards among clinical dental staff. J Contemp Dent Pract. 2004;5:134-52.. However, their clinical experience (2.78±1.57 years) is much shorter, suggesting that the progression and deterioration of MSDs spark from the very beginning of the practitioners' career life. Ergonomic studies demonstrate that protection and treatment should begin early before musculoskeletal injuries become persistent1818- Ranney D. Work-related chronic injuries of the forearm and hand: their specific diagnosis and management. Ergonomics. 1993;36:871-80.. Thus, more concerns should be put on the prevention in the early stages of dental careers.
The comparison regarding MSDs among different dental specialties provides more fresh and in-depth understandings to this issue. It is interesting that prosthodontic students experience more suffering of wrist symptoms while fewer in almost all other body regions (Table 1). This discrepancy may be due to the nature of prosthodontic work. Compared with other specialties, prosthodontic students may assign relatively less time for intraoral operation, as they have more off-chair work to do, e.g., making the temporary crown and choosing the color for porcelain. This advantage may more or less relieve them of the burden from the long-term awkward posture in chair-side operation. On the other hand, more frequent use of vibrating instruments, as indicated to be a risk factor for wrist injuries in previous studies1212- Lake J. Musculoskeletal dysfunction associated with the practice of dentistry - proposed mechanisms and management: literature review. Univ Tor Dent J. 1995;9:7,9-11., probably subjects them to higher risk of wrist disorders.
Despite the generally low prevalence of knee disorders in other studies1313- Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: a review. Ind Health. 2007;45:611- 21., alveolar surgery students have significantly higher prevalence in knees compared to other specialties in our investigation. It is observed that when performing dentoalveolar surgeries, like tooth extraction, students usually stand to facilitate their operations. Moreover, they may well take more time to finish an extraction due to inexperience, which puts them long in an unfavorable standing posture. Knee joints would be more vulnerable to chronic injuries when keeping stance is combined with large cumulative loads1616- Newell TM, Kumar S. Comparison of instantaneous and cumulative loads on the low back and neck in orthodontists. Clin Biomech (Bristol, Avon). 2005;20:130-7.. This could account for the vulnerability of knees among alveolar surgery students. However, experienced alveolar surgeons tend to sit whenever possible, which is also suggested to be a more protective posture55- Belenky M. Human-centered ergonomics: proprioceptive pathway to occupational health and peak performance in dental practice. In: Murphy DC, editor. Human-centered ergonomics. Ergonomics and the dental care worker. Waldorf: American Public Health Association; 1998. p.275-99.. It indicates that harmful postures are not always inevitable, thus further highlights the importance of corresponding training for the prevention of MSDs.
Periodontic students suffer the most serious MSDs in neck, shoulders, upper back and lower back. Long work duration and repetitive movements of periodontal treatments could be the main reasons that predisposes them to higher risk of MSDs. Interestingly, though using ultrasonic instruments for tooth cleaning frequently, periodontic students do not experience severe wrist symptoms as prosthodontic students do. Prehension force, which serves as a risk factor for MSDs66- Bramson JB, Smith S, Romagnoli G. Evaluating dental office ergonomic. Risk factors and hazards. J Am Dent Assoc. 1998;129:174-83., may explain this difference, as ultrasonic periodontal instruments do not require consistent firm grasp while high-speed handpieces do, which are more frequently used by prosthodontists.
Only a few variables of potential correlative factors are found significantly associated with MSDs. The differences among distinct specialties exist, but are not obvious. Clinical time and desk time positively correlate to musculoskeletal disorders, whereas physical exercise and rest between patients play a protective role, which is in accordance with previous studies concerning dentists99- Finsen L, Christensen H, Bakke M. Musculoskeletal disorders among dentists and variation in dental work. Appl Ergon. 1998;29:119-25. , 1010- Hayes MJ, Smith DR, Cockrell D. Prevalence and correlates of musculoskeletal disorders among Australian dental hygiene students. Int J Dent Hyg. 2009;7:176-81.. Female students are shown to present higher risk of MSDs than male, especially those who specialize in alveolar surgery. This could be due to the fact that surgeries like tooth extraction demand high and continuous prehension forces and, therefore, female students have to struggle harder to exert the required strength. Moreover, young women have less physical exercise than young men. No significant association is detected between MSDs and some suspicious risk factors, such as poor illumination satisfaction. Briefly, development of MSDs in dental students is related to multiple factors, mainly consistent with those of dentists. It indicates that, even though the accumulation of exposure to these factors is low in the early training years, their influences are still significant. Thus, prevention aimed at these factors should be explored.
Based on our findings, clinical supervisors should put more emphasis on musculoskeletal health according to the specific disease patterns of MSDs in distinct specialties, as numerous pedagogies have been shown to improve self-protection awareness77- Conrado CA, Maciel SM, Oliveira MR. A school-based oral health educational program: the experience of Maringa- PR, Brazil. J Appl Oral Sci. 2004;12:27-33. , 2121- Sposto MR, Santos SG, Domaneschi C, Navarro CM, Onofre MA. [Evaluation of the dental students' knowledge on HIV infection. Analysis before and after an informative lecture]. J Appl Oral Sci. 2003;11:125-32.. In addition, more physical exercises and less desk time could help dental personnel stay away from MSDs. Lastly and in the long run, working environment and dental instruments should keep having improvements.
Nevertheless, there are some limitations in this study. Firstly, though 271 dental postgraduates were recruited, each specialty only had a sample size of 43-68. Secondly, as most data are collected by self-report questionnaires, memorial mistakes could hardly be avoided. Therefore, prospective studies with larger sample sizes are necessary in the future.
CONCLUSION
High MSDs afflict dental professionals since early training years, which are specialty specific. Thus, protection against MSDs of dental practitioners should be taken at the early stage of careers, precisely, while still as dental students. Moreover, the preventive methods should match the nature of clinical task in distinct specialties.
This work was supported by National Nature Science Foundation of China No, 11002095 (to Dr. Yu Li) and Innovating Training Project (No. 20120610081) of Sichuan University.
REFERENCES
-
1- Abreu MH, Lopes-Terra MC, Braz LF, Rimulo AL, Paiva SM, Pordeus IA. Attitudes and behavior of dental students concerning infection control rules: a study with a 10-year interval. Braz Dent J. 2009;20:221-5.
-
2- Akesson I, Johnsson B, Rylander L, Moritz U, Skerfving S. Musculoskeletal disorders among female dental personnel: clinical examination and a 5-year follow-up study of symptoms. Int Arch Occup Environ Health. 1999;72:395-403.
-
3- Anton D, Rosecrance J, Merlino L, Cook T. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am J Ind Med. 2002;42:248-57.
-
4- Beach JC, DeBiase CB. Assessment of ergonomic education in dental hygiene curricula. J Dent Educ. 1998;62:421-5.
-
5- Belenky M. Human-centered ergonomics: proprioceptive pathway to occupational health and peak performance in dental practice. In: Murphy DC, editor. Human-centered ergonomics. Ergonomics and the dental care worker. Waldorf: American Public Health Association; 1998. p.275-99.
-
6- Bramson JB, Smith S, Romagnoli G. Evaluating dental office ergonomic. Risk factors and hazards. J Am Dent Assoc. 1998;129:174-83.
-
7- Conrado CA, Maciel SM, Oliveira MR. A school-based oral health educational program: the experience of Maringa- PR, Brazil. J Appl Oral Sci. 2004;12:27-33.
-
8- Fasunloro A, Owotade FJ. Occupational hazards among clinical dental staff. J Contemp Dent Pract. 2004;5:134-52.
-
9- Finsen L, Christensen H, Bakke M. Musculoskeletal disorders among dentists and variation in dental work. Appl Ergon. 1998;29:119-25.
-
10- Hayes MJ, Smith DR, Cockrell D. Prevalence and correlates of musculoskeletal disorders among Australian dental hygiene students. Int J Dent Hyg. 2009;7:176-81.
-
11- Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering- Sørensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233-7.
-
12- Lake J. Musculoskeletal dysfunction associated with the practice of dentistry - proposed mechanisms and management: literature review. Univ Tor Dent J. 1995;9:7,9-11.
-
13- Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: a review. Ind Health. 2007;45:611- 21.
-
14- Li X. Medical statistics. 2nd ed. Beijing: Higher Education Press; 2008.
-
15- Martins Junior RL, Kerber FC, Stuginski-Barbosa J. Attitudes of a group of Brazilian orthodontists towards the diagnosis and management of primary headache (migraine): an electronic-based survey. J Appl Oral Sci. 2011;19:674-8.
-
16- Newell TM, Kumar S. Comparison of instantaneous and cumulative loads on the low back and neck in orthodontists. Clin Biomech (Bristol, Avon). 2005;20:130-7.
-
17- Oberg T, Oberg U. Musculoskeletal complaints in dental hygiene: a survey study from a Swedish county. J Dent Hyg. 1993;67:257-61.
-
18- Ranney D. Work-related chronic injuries of the forearm and hand: their specific diagnosis and management. Ergonomics. 1993;36:871-80.
-
19- Sanders M, Turcotte C. Ergonomic strategies for dental professionals. Work. 1997;8:55-72.
-
20- Smith CA, Sommerich CM, Mirka GA, George MC. An investigation of ergonomic interventions in dental hygiene work. Appl Ergon. 2002;33:175-84.
-
21- Sposto MR, Santos SG, Domaneschi C, Navarro CM, Onofre MA. [Evaluation of the dental students' knowledge on HIV infection. Analysis before and after an informative lecture]. J Appl Oral Sci. 2003;11:125-32.
-
22- Yüzbasioglu E, Saraç D, Canbaz S, Saraç YS, Cengiz S. A survey of cross-infection control procedures: knowledge and attitudes of Turkish dentists. J Appl Oral Sci. 2009;17:565-9.
Publication Dates
-
Publication in this collection
Jul-Aug 2013
History
-
Received
08 Mar 2013 -
Reviewed
31 May 2013 -
Accepted
20 June 2013