Abstract
OBJECTIVES:
This cross-sectional study aimed to evaluate the influence of Primary Headache (PH) on efficacy of a Temporomandibular Disorders (TMD) conservative therapy and its association with the presence of self-reported parafunctional habits.
SAMPLE AND METHODS:
Sample was composed of 400 medical records, divided into four groups: I) Muscular TMD (n=64); II) Muscular TMD+PH (n=48); III) Muscular TMD+Articular TMD (n=173); IV) Muscular TMD+Articular TMD+PH (n=115). All groups had undergone a TMD therapy for three months with a stabilization appliance and counseling for habits and behavioral changes, with no specific headache management. Current pain intensity and existence or not of self-reported bruxism were assessed. Repeated measures ANOVA and Chi-Square test followed by Odds were used for statistical analysis, with a significance level of 5%.
RESULTS:
results of this study showed that: (1) A conservative therapy with stabilization appliance and counseling for habits and behavioral changes was effective in the TMD pain relief; (2) Groups with an additional diagnosis of PH had worsened the pain improvement significantly; and (3) no association between the presence of self-reported bruxism and PH was found.
CONCLUSIONS:
this study could elucidate the important effect that headache may have on the TMD management.
Facial pain; Temporomandibular joint disorders; Headache; Therapy
INTRODUCTION
Primary headache (PH) and chronic orofacial pain are common symptoms in the general population88- Ciancaglini R, Radaelli G. The relationship between headache and symptoms of temporomandibular disorder in the general population. J Dent. 2001;29(2):93-8., and the presence of headache in patients reporting temporomandibular disorders (TMD) have a high prevalence of 50 to 80%66- Bendtsen L, Jensen R. Tension-type headache. Neurol Clin. 2009;27(2):525-35. , 88- Ciancaglini R, Radaelli G. The relationship between headache and symptoms of temporomandibular disorder in the general population. J Dent. 2001;29(2):93-8. , 2828- Mitrirattanakul S, Merrill RL. Headache impact in patients with orofacial pain. J Am Dent Assoc. 2006;137(9):1267-74., whereas these numbers in patients without TMD are only 13 to 23%1919- Gonçalves DA, Speciali JG, Jales LC, Camparis CM, Bigal ME. Temporomandibular symptoms, migraine, and chronic daily headaches in the population. Neurology. 2009;73(8):645-6. , 3333- Wiendels NJ, Knuistingh Neven A, Rosendaal FR, Spinhoven P, Zitman FG, Assendelft WJ, et al. Chronic frequent headache in the general population: prevalence and associated factors. Cephalalgia. 2006;26(12):1434-42..
Primary headache individuals could experience more severe and frequent symptoms of TMD, and vice-versa22- Alencar F Jr, Becker A. Evaluation of different occlusal splints and counselling in the management of myofascial pain dysfunction. J Oral Rehabil. 2009;36(2):79-85. , 33- Arima T, Svensson P, Arendt-Nielsen L. Experimental grinding in healthy subjects: a model for postexercise jaw muscle soreness? J Orofac Pain. 1999;13(2):104-14.. The relationship between these two entities, however, is not well established in the literature yet55- Ballegaard V, Thede-Schmidt-Hansen P, Svensson P, Jensen R. Are headache and temporomandibular disorders related? A blinded study. Cephalalgia. 2008;28(8):832-41. , 1919- Gonçalves DA, Speciali JG, Jales LC, Camparis CM, Bigal ME. Temporomandibular symptoms, migraine, and chronic daily headaches in the population. Neurology. 2009;73(8):645-6..
Some studies have shown that TMD therapy reduces the complaint of headache in both intensity and frequency3030- Nilsson H, Vallon D, Ekberg EC. Long-term efficacy of resilient appliance therapy in TMD pain patients: a randomised, controlled trial. J Oral Rehabil. 2011;38(10):713-21., nevertheless, to the best of our knowledge, the impact of PH on TMD therapy efficacy has not been published yet.
Furthermore, some studies have confirmed that the presence of parafunctional habits, i.e., activities of the masticatory muscles, as clenching and grinding, has an important role in TMD pain, whereas patients with sleep bruxism have an increased risk for the occurrence of myofascial pain1515- Fernandes G, Franco AL, Siqueira JT, Goncalves DA, Camparis CM. Sleep bruxism increases the risk for painful temporomandibular disorder, depression and non-specific physical symptoms. J Oral Rehabil. 2012;39(7):538-44.. This association with headache is not well defined2929- Nagamatsu-Sakaguchi C, Minakuchi H, Clark GT, Kuboki T. Relationship between the frequency of sleep bruxism and the prevalence of signs and symptoms of temporomandibular disorders in an adolescent population. Int J Prosthodont. 2008;21(4):292-8..
Based on the above, this study aimed to evaluate the influence of the presence of PH on the efficacy of a TMD conservative therapy and the association with the presence of self-reported parafunctional habits. The null hypothesis is that the presence of primary headaches does not influence negatively the efficacy of TMD management.
SAMPLE AND METHODS
This study was approved by the Institutional Ethics Committee, under protocol #105/2010.
Sample
This cross-sectional study performed 1,200 evaluations in medical records from an Orofacial Pain Clinic, from 1996 to 2009. The sample was composed of 400 medical records, initially selected according to the following criteria:
Inclusion:
1. Medical records of adults aged 18 years or more with:
2. Presence of myofascial pain with or without the presence of muscular trigger points by manual palpation, according to the American Academy of Orofacial Pain (AAOP)1111- De Leeuw R, Klasser GD (editors). Orofacial pain: guidelines for assessment, diagnosis, and management. Chicago: Quintessence; 2008.;
Exclusion:
1. Medical records of individuals with neurological diseases, fibromyalgia, systemic arthritis, secondary headache or paroxysmal hemicrania, menstrual and cluster headache.
Group establishment
After fulfilling the initial criteria, the medical records were analyzed according to the presence or not of TMD through AAOP criteria1111- De Leeuw R, Klasser GD (editors). Orofacial pain: guidelines for assessment, diagnosis, and management. Chicago: Quintessence; 2008.; and PH based on International Headache Society (IHS)2424- Lipton RB, Bigal ME, Steiner TJ, Silberstein SD, Olesen J. Classification of primary headaches. Neurology. 2004;63(3):427-435., fulfilling the criteria for migraine and/or tensiontype headache.
Patients could be allocated into one of the four groups below:
I) Only muscular TMD (with no headache complaint):
This group was composed of 64 medical records of subjects with muscular TMD only. Muscular TMD encompassed localized myalgia and masticatory myofascial pain according to AAOP1111- De Leeuw R, Klasser GD (editors). Orofacial pain: guidelines for assessment, diagnosis, and management. Chicago: Quintessence; 2008..
They had undergone a conservative therapy for three months with a rigid acrylic upper full coverage stabilization appliance, along with counseling for habits and behavioral changes, home care instructions, exercises and Physical therapy modalities99- Conti PC, Alencar EN, Mota Corrêa AS, Lauris JR, Porporatti AL, Costa YM. Behavioural changes and occlusal splints are effective in the management of masticatory myofascial pain: a short-term evaluation. J Oral Rehabil. 2012;39(10):754-60.. Analgesics and anti-inflammatory drugs could also be used.
II) Muscular TMD+primary headache:
This group was composed of 48 medical records of subjects with muscular TMD plus the presence of primary headache. They had undergone the same conservative therapy for group I, with no specific headache management.
III) Only muscular TMD+articular TMD (with no headache complaint):
This group was composed of 173 medical records from subjects with muscular and articular TMD. They had undergone the same conservative therapy for group I.
Articular TMD included arthralgia and disc displacement with or without reduction, with or without mouth opening limitation, fulfilling the AAOP criteria1111- De Leeuw R, Klasser GD (editors). Orofacial pain: guidelines for assessment, diagnosis, and management. Chicago: Quintessence; 2008..
IV) Muscular TMD+articular TMD+primary headache:
This group was composed of 115 medical records of subjects with muscular and articular TMD plus the presence of primary headache. They had undergone the same conservative therapy for group I, with no specific headache management.
Examiners and variables
Two examiners performed all the medical records evaluations. Current pain intensity was analyzed according to self-reported pain on Visual Analogue Scale (VAS) at baseline and after three months of TMD therapy. Moreover, the existence or not of selfreported clenching/bruxism parafunctional habits was analyzed at baseline. The pain experience duration, in months, was also recorded.
Data analysis
The results were analyzed with repeated measurements ANOVA (after Kolmogorov-Smirnov to test normal distribution) to assess within and between groups differences; Chi-Square test followed by Odds Ratio test, with 95% of Confidence Interval (CI), to test association between PH and bruxism; and Spearman Correlation to correlate pain duration and pain intensity variation between baseline and after therapy. The results were established with a significance level of 5%.
RESULTS
The mean age was 36.87 years for group I, 36.79 years for group II, 36.36 for group III, and 36.79 for group IV (p=0.55). Women were 81.25% of group I, 89.58%, 86.12%, and 94.78% of group II, III, and IV, respectively.
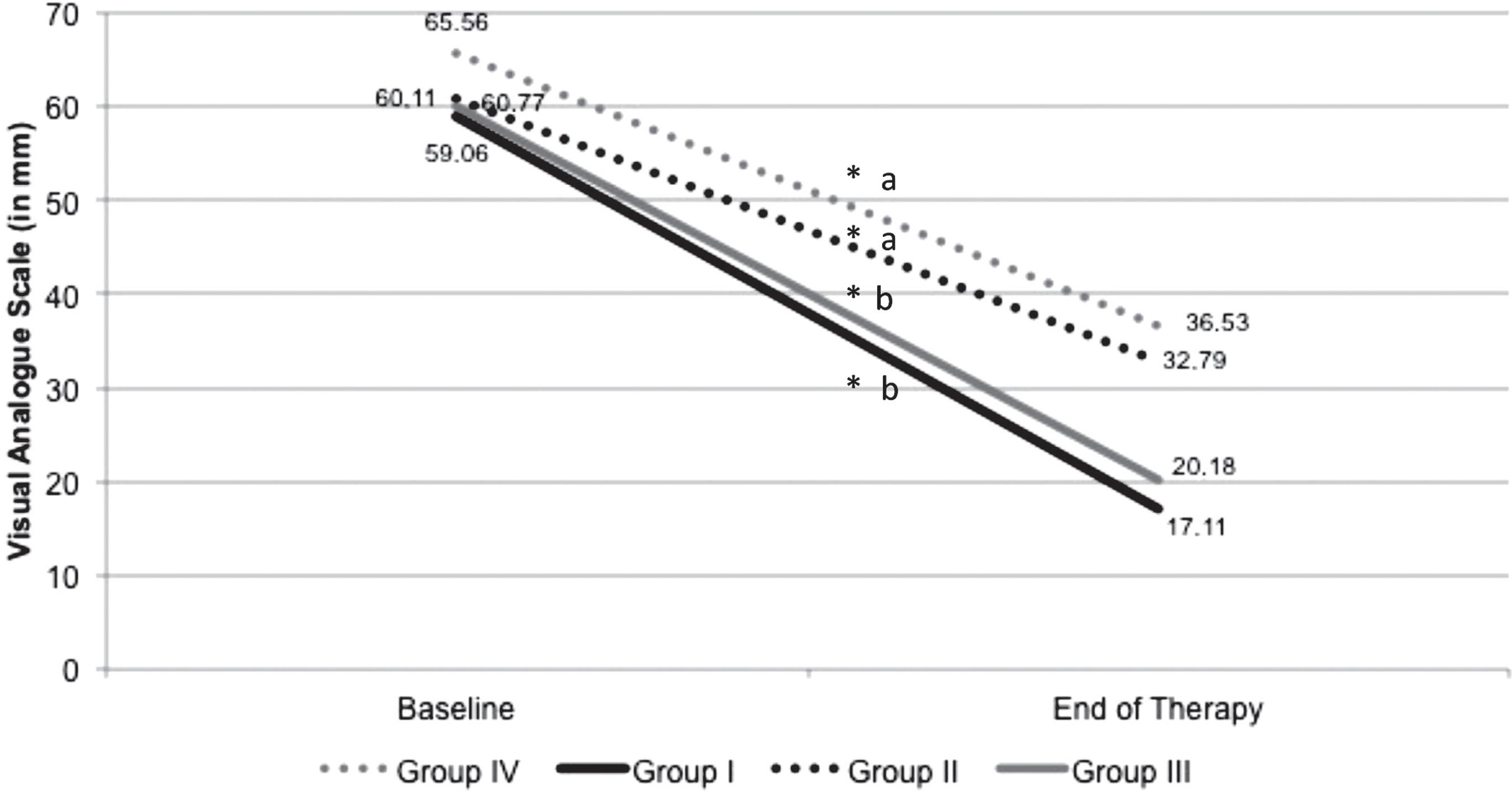
In the within groups analysis, there was a significant reduction in the reported pain for all groups (p<0.05) after three months of TMD therapy (Figure 1).
Pain intensity according to Visual Analogue Scale (VAS) at baseline and in the end of the therapy
* indicates within-groups differences (p<0.05)
aa indicates no between-groups differences (p>0.05)
ab indicates between-groups differences (p<0.05)
Pain improvement in VAS was 70.74% (SD 30.71) and 46.32% (SD 24.70) for group I and II, respectively, and 66.44% (SD 35.37) and 42.56% (SD 31.72) for group III and IV, respectively (Figure 1). Significant results revealed better pain improvement for group I compared to group II, and for group III, when compared to group IV (p<0.05%) (Figure 1).
At baseline, significant differences for the self-report of clenching/bruxism were perceived only between groups I and II with III and IV, which showed that subjects with muscular TMD had at baseline a higher percentage of clenching/bruxism parafunctional habits than subjects with muscular and articular TMD, without considering the presence or not of PH (Table 1). No differences were found on the association between PH and bruxism (Table 2).
Chi-Square test (X2) and Odds Ratio (OR) of association between primary headache and clenching/bruxism parafunctional habits
The mean duration of pain experience was 63.71 months (SD 62.37), 70.95 (SD 76.85), 58.91 (SD 71.00), and 67.92 (SD 84.38) for group I, II, III, and IV, respectively (p=0.10). No significant correlation with the pain improvement was detected (Spearman R=0.036, p=0.39).
DISCUSSION
This study evaluated 400 medical records regarding the efficacy of TMD management in patients with primary headache as a comorbid condition. The null hypothesis was rejected. The main findings were: (1) a conservative therapy with stabilization appliance and counseling for habits and behavioral changes was effective in the TMD pain relief; (2) the presence of concomitant primary headache negatively influenced the efficacy of TMD therapy; (3) no association between the presence of self-reported bruxism and PH was found; and (4) no correlation was found between TMD management efficacy on pain severity and the duration of pain experience.
Our sample was mainly composed of women (88%), aged between 30-45 years (35.47±12.59), which is in agreement with epidemiological publications1717- Fricton J. Myogenous temporomandibular disorders: diagnostic and management considerations. Dent Clin North Am. 2007;51(1):61-83. , 2727- Manfredini D, Piccotti F, Ferronato G, Guarda-Nardini L. Age peaks of different RDC/TMD diagnoses in a patient population. J Dent. 2010;38(5):392-9.. All groups had chronic craniofacial pain, with mean duration of 63.72±74.30 months.
After three months of therapy, management strategies as stabilization splint and counseling for behavioral changes used in the present study provided a significant improvement in the pain levels of articular and/or muscular TMD when judged by the VAS. This management approach is supported by the literature and is recommended as an effective therapy modality77- Bergstrom I, List T, Magnusson T. A follow-up study of subjective symptoms of temporomandibular disorders in patients who received acupuncture and/or interocclusal appliance therapy 18-20 years earlier. Acta Odontol Scand. 2008;66(2):88-92. , 1616- Freitas RF, Ferreira MA, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: a systematic review. J Oral Rehabil. 2013;40(11):864-74. , 1717- Fricton J. Myogenous temporomandibular disorders: diagnostic and management considerations. Dent Clin North Am. 2007;51(1):61-83. , 2121- Helkimo M. Request for expert statement regarding the use of NTI-splint. Stockholm: Socialstyrelesen; 2003. , 2222- Klasser GD, Greene CS. Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(2):212-23. , 3232- Stapelmann H, Türp JC. The NTI-tss device for the therapy of bruxism, temporomandibular disorders, and headache - where do we stand? A qualitative systematic review of the literature. BMC Oral Health. 2008;8:22..
A possible explanation on the use of this management approach is based on a decrease of the overload masticatory system22- Alencar F Jr, Becker A. Evaluation of different occlusal splints and counselling in the management of myofascial pain dysfunction. J Oral Rehabil. 2009;36(2):79-85. , 2323- Kopp S. Short term evaluation of counselling and occlusal adjustment in patients with mandibular dysfunction involving the temporomandibular joint. J Oral Rehabil. 1979;6(2):101-9.. Stabilization splints provide proper occlusal relationship, reduction in muscular activity, stable physiologic mandibular posture; and with the potential cognitive and placebo effect2020- Greene CS, Goddard G, Macaluso GM, Mauro G. Topical review: placebo responses and therapeutic responses. How are they related? J Orofac Pain. 2009;23(2):93-107. , 3131- Pollo A, Carlino E, Benedetti F. Placebo mechanisms across different conditions: from the clinical setting to physical performance. Philos Trans R Soc Lond B Biol Sci. 2011;366(1572):1790-8.. The actual results may have an essential correlation with all these mechanisms of action. Furthermore, the patient education about behavioral changes, the probable high impact of the patient's initial reaction to a professional orientation, and also placebo effect, natural evolution of the disease and regression towards the mean99- Conti PC, Alencar EN, Mota Corrêa AS, Lauris JR, Porporatti AL, Costa YM. Behavioural changes and occlusal splints are effective in the management of masticatory myofascial pain: a short-term evaluation. J Oral Rehabil. 2012;39(10):754-60. may play a role in the pain reduction for all groups observed in this study.
After the TMD management, groups with additional diagnosis of primary headache did not have the same level of amelioration than groups with only TMD and without PH. It has been very well established that nociceptive impulses arising from masticatory muscles and temporomandibular joint, as well as cranial tissues and head area, may induce central sensitization mechanisms in the subnucleus caudalis of the trigeminal nerve system1919- Gonçalves DA, Speciali JG, Jales LC, Camparis CM, Bigal ME. Temporomandibular symptoms, migraine, and chronic daily headaches in the population. Neurology. 2009;73(8):645-6.. Since both areas, TMD and head region, share similar ascendant pain pathways in the trigeminal system, the increase in pain transmission from peripheral tissues to the trigeminal system could explain the fact that the presence of comorbid PH, not treated, could influence negatively a TMD therapy, and the approach of both conditions should be stated.
The effectiveness of stabilization devices in the management of TMD pain is well documented and it is related to the re-establishment of proper occlusal relationship; the reduction in muscular activity; the cognitive effect, since the patients became aware of their oral parafunctional habits; and the placebo effect77- Bergstrom I, List T, Magnusson T. A follow-up study of subjective symptoms of temporomandibular disorders in patients who received acupuncture and/or interocclusal appliance therapy 18-20 years earlier. Acta Odontol Scand. 2008;66(2):88-92. , 99- Conti PC, Alencar EN, Mota Corrêa AS, Lauris JR, Porporatti AL, Costa YM. Behavioural changes and occlusal splints are effective in the management of masticatory myofascial pain: a short-term evaluation. J Oral Rehabil. 2012;39(10):754-60. , 1717- Fricton J. Myogenous temporomandibular disorders: diagnostic and management considerations. Dent Clin North Am. 2007;51(1):61-83. , 2222- Klasser GD, Greene CS. Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(2):212-23. , 3232- Stapelmann H, Türp JC. The NTI-tss device for the therapy of bruxism, temporomandibular disorders, and headache - where do we stand? A qualitative systematic review of the literature. BMC Oral Health. 2008;8:22.. However, the literature is vague about this fact in headache improvement. Some studies report headache pain decrease, in both intensity and frequency, about 30 to 50% when TMD was treated with splint therapy, in short and long-term evaluations1212- Doepel M, Nilner M, Ekberg E, Vahlberg T, Bell YI. Headache: short- and long-term effectiveness of a prefabricated appliance compared to a stabilization appliance. Acta Odontol Scand. 2011;69(3):129-36. , 1313- Ekberg EC, Nilner M. Treatment outcome of short- and longterm appliance therapy in patients with TMD of myogenous origin and tension-type headache. J Oral Rehabil. 2006;33(10):713-21. , 3030- Nilsson H, Vallon D, Ekberg EC. Long-term efficacy of resilient appliance therapy in TMD pain patients: a randomised, controlled trial. J Oral Rehabil. 2011;38(10):713-21..
The literature suggests that subjects with sleep bruxism have increased risk for myofascial and joint pain conditions1515- Fernandes G, Franco AL, Siqueira JT, Goncalves DA, Camparis CM. Sleep bruxism increases the risk for painful temporomandibular disorder, depression and non-specific physical symptoms. J Oral Rehabil. 2012;39(7):538-44.. In this study, the prevalence of clenching/bruxism parafunctional habits was very high for all groups.
Some studies had showed that the postexercise muscle soreness is associated with this overload mechanism of muscle pain in individuals with bruxism, which can be a risk factor to the installation of myofascial TMD33- Arima T, Svensson P, Arendt-Nielsen L. Experimental grinding in healthy subjects: a model for postexercise jaw muscle soreness? J Orofac Pain. 1999;13(2):104-14. , 1010- Dao TT, Lund JP, Lavigne GJ. Comparison of pain and quality of life in bruxers and patients with myofascial pain of the masticatory muscles. J Orofac Pain. 1994;8(4):350-6. , 1515- Fernandes G, Franco AL, Siqueira JT, Goncalves DA, Camparis CM. Sleep bruxism increases the risk for painful temporomandibular disorder, depression and non-specific physical symptoms. J Oral Rehabil. 2012;39(7):538-44.. Our results show higher prevalence of bruxism in the muscular TMD groups only, and lower values in the articular TMD groups. It is possible that this outcome could be a result of a difference in the pathophysiology between the articular and the muscular TMD. In the group presenting with articular and muscular TMD, the muscle pain might be a consequence of the articular pain conditions, which, in turn, could lead to a muscle co-contraction. In this case, the occurrence of parafunctional habits could not be as important as in the case of only muscle pain. Furthermore, the prevalence of bruxism in articular TMD patients is lower2525- Manfredini D, Cantini E, Romagnoli M, Bosco M. Prevalence of bruxism in patients with different research diagnostic criteria for temporomandibular disorders (RDC/TMD) diagnoses. Cranio. 2003;21(4):279-85.. Finally, considering that muscle pain could be a symptom of bruxism44- Bader G, Lavigne G. Sleep bruxism; an overview of an oromandibular sleep movement disorder. REVIEW ARTICLE. Sleep Med Rev. 2000;4(1):27-43., in the group of only muscular TMD, bruxism could be the primary source of pain, which explains the higher prevalence in the groups I and II.
The causal relationship between bruxism and TMD is controversial. A recent systematic review found that studies based on self-report or clinical diagnosis of bruxism have a positive association with TMD, while studies based on more specific quantitative diagnostic methods revealed a weak association with symptoms of TMD2626- Manfredini D, Lobbezoo F. Relationship between bruxism and temporomandibular disorders: a systematic review of literature from 1998 to 2008. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(6):e26-50.. Although parafunctional habits increase the activation of masticatory muscles1818- Glaros AG, Burton E. Parafunctional clenching, pain, and effort in temporomandibular disorders. J Behav Med. 2004;27(1):91-100., which sometimes may cause pain11- Ahlberg K, Ahlberg J, Könönen M, Alakuijala A, Partinen M, Savolainen A. Perceived orofacial pain and its associations with reported bruxism and insomnia symptoms in media personnel with or without irregular shift work. Acta Odontol Scand. 2005;63(4):213-7., bruxism is not always correlated with the pain caused by TMD. In this sense, to establish a direct causal relationship between bruxism and TMD is difficult.
Our study showed that self-reported bruxism was not associated with the presence of PH. A recent study evaluated the association between TMD, sleep bruxism (SB) and PH. It could be found that in patients with painful TMD and SB, only the presence of sleep bruxism did not increase the risk for any kind of PH1414- Fernandes G, Franco AL, Goncalves DA, Speciali JG, Bigal ME, Camparis CM. Temporomandibular disorders, sleep bruxism, and primary headaches are mutually associated. J Orofac Pain. 2013;27(1):14-20..
No correlation between TMD improvement after three months and duration of pain experience was found. It was expected that the longer the pain experience, the higher the peripheral and central sensitization, associated to some sort of impairment of the descending inhibitory analgesic system, which could influence the efficacy of pain management. However, this fact was not tested here. The non-administration of central acting medication and strategies devoted to revert such central alterations could explain this similarity between those with more time of pain experience and those with less time.
Another limitation of the present study is the relatively weak reliability of the data obtained from the medical records, usually handled by different professionals. Although extracted from records from the same treatment center, variations in diagnosis and management strategies are expected, jeopardizing the present results.
Based on the aforementioned, this study showed the potential and significant effect that headache has in the efficacy of TMD management. A combined approach to both pain conditions is suggested.
REFERENCES
-
1- Ahlberg K, Ahlberg J, Könönen M, Alakuijala A, Partinen M, Savolainen A. Perceived orofacial pain and its associations with reported bruxism and insomnia symptoms in media personnel with or without irregular shift work. Acta Odontol Scand. 2005;63(4):213-7.
-
2- Alencar F Jr, Becker A. Evaluation of different occlusal splints and counselling in the management of myofascial pain dysfunction. J Oral Rehabil. 2009;36(2):79-85.
-
3- Arima T, Svensson P, Arendt-Nielsen L. Experimental grinding in healthy subjects: a model for postexercise jaw muscle soreness? J Orofac Pain. 1999;13(2):104-14.
-
4- Bader G, Lavigne G. Sleep bruxism; an overview of an oromandibular sleep movement disorder. REVIEW ARTICLE. Sleep Med Rev. 2000;4(1):27-43.
-
5- Ballegaard V, Thede-Schmidt-Hansen P, Svensson P, Jensen R. Are headache and temporomandibular disorders related? A blinded study. Cephalalgia. 2008;28(8):832-41.
-
6- Bendtsen L, Jensen R. Tension-type headache. Neurol Clin. 2009;27(2):525-35.
-
7- Bergstrom I, List T, Magnusson T. A follow-up study of subjective symptoms of temporomandibular disorders in patients who received acupuncture and/or interocclusal appliance therapy 18-20 years earlier. Acta Odontol Scand. 2008;66(2):88-92.
-
8- Ciancaglini R, Radaelli G. The relationship between headache and symptoms of temporomandibular disorder in the general population. J Dent. 2001;29(2):93-8.
-
9- Conti PC, Alencar EN, Mota Corrêa AS, Lauris JR, Porporatti AL, Costa YM. Behavioural changes and occlusal splints are effective in the management of masticatory myofascial pain: a short-term evaluation. J Oral Rehabil. 2012;39(10):754-60.
-
10- Dao TT, Lund JP, Lavigne GJ. Comparison of pain and quality of life in bruxers and patients with myofascial pain of the masticatory muscles. J Orofac Pain. 1994;8(4):350-6.
-
11- De Leeuw R, Klasser GD (editors). Orofacial pain: guidelines for assessment, diagnosis, and management. Chicago: Quintessence; 2008.
-
12- Doepel M, Nilner M, Ekberg E, Vahlberg T, Bell YI. Headache: short- and long-term effectiveness of a prefabricated appliance compared to a stabilization appliance. Acta Odontol Scand. 2011;69(3):129-36.
-
13- Ekberg EC, Nilner M. Treatment outcome of short- and longterm appliance therapy in patients with TMD of myogenous origin and tension-type headache. J Oral Rehabil. 2006;33(10):713-21.
-
14- Fernandes G, Franco AL, Goncalves DA, Speciali JG, Bigal ME, Camparis CM. Temporomandibular disorders, sleep bruxism, and primary headaches are mutually associated. J Orofac Pain. 2013;27(1):14-20.
-
15- Fernandes G, Franco AL, Siqueira JT, Goncalves DA, Camparis CM. Sleep bruxism increases the risk for painful temporomandibular disorder, depression and non-specific physical symptoms. J Oral Rehabil. 2012;39(7):538-44.
-
16- Freitas RF, Ferreira MA, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: a systematic review. J Oral Rehabil. 2013;40(11):864-74.
-
17- Fricton J. Myogenous temporomandibular disorders: diagnostic and management considerations. Dent Clin North Am. 2007;51(1):61-83.
-
18- Glaros AG, Burton E. Parafunctional clenching, pain, and effort in temporomandibular disorders. J Behav Med. 2004;27(1):91-100.
-
19- Gonçalves DA, Speciali JG, Jales LC, Camparis CM, Bigal ME. Temporomandibular symptoms, migraine, and chronic daily headaches in the population. Neurology. 2009;73(8):645-6.
-
20- Greene CS, Goddard G, Macaluso GM, Mauro G. Topical review: placebo responses and therapeutic responses. How are they related? J Orofac Pain. 2009;23(2):93-107.
-
21- Helkimo M. Request for expert statement regarding the use of NTI-splint. Stockholm: Socialstyrelesen; 2003.
-
22- Klasser GD, Greene CS. Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(2):212-23.
-
23- Kopp S. Short term evaluation of counselling and occlusal adjustment in patients with mandibular dysfunction involving the temporomandibular joint. J Oral Rehabil. 1979;6(2):101-9.
-
24- Lipton RB, Bigal ME, Steiner TJ, Silberstein SD, Olesen J. Classification of primary headaches. Neurology. 2004;63(3):427-435.
-
25- Manfredini D, Cantini E, Romagnoli M, Bosco M. Prevalence of bruxism in patients with different research diagnostic criteria for temporomandibular disorders (RDC/TMD) diagnoses. Cranio. 2003;21(4):279-85.
-
26- Manfredini D, Lobbezoo F. Relationship between bruxism and temporomandibular disorders: a systematic review of literature from 1998 to 2008. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(6):e26-50.
-
27- Manfredini D, Piccotti F, Ferronato G, Guarda-Nardini L. Age peaks of different RDC/TMD diagnoses in a patient population. J Dent. 2010;38(5):392-9.
-
28- Mitrirattanakul S, Merrill RL. Headache impact in patients with orofacial pain. J Am Dent Assoc. 2006;137(9):1267-74.
-
29- Nagamatsu-Sakaguchi C, Minakuchi H, Clark GT, Kuboki T. Relationship between the frequency of sleep bruxism and the prevalence of signs and symptoms of temporomandibular disorders in an adolescent population. Int J Prosthodont. 2008;21(4):292-8.
-
30- Nilsson H, Vallon D, Ekberg EC. Long-term efficacy of resilient appliance therapy in TMD pain patients: a randomised, controlled trial. J Oral Rehabil. 2011;38(10):713-21.
-
31- Pollo A, Carlino E, Benedetti F. Placebo mechanisms across different conditions: from the clinical setting to physical performance. Philos Trans R Soc Lond B Biol Sci. 2011;366(1572):1790-8.
-
32- Stapelmann H, Türp JC. The NTI-tss device for the therapy of bruxism, temporomandibular disorders, and headache - where do we stand? A qualitative systematic review of the literature. BMC Oral Health. 2008;8:22.
-
33- Wiendels NJ, Knuistingh Neven A, Rosendaal FR, Spinhoven P, Zitman FG, Assendelft WJ, et al. Chronic frequent headache in the general population: prevalence and associated factors. Cephalalgia. 2006;26(12):1434-42.
Publication Dates
-
Publication in this collection
04 July 2014 -
Date of issue
Mar-Apr 2015
History
-
Received
29 Oct 2013 -
Reviewed
10 Feb 2014 -
Accepted
31 Mar 2014