Abstract
Whenever humans come in touch with the sea, they become vulnerable to risks, most frequently on account of invading a habitat that belongs to potentially harmful aquatic animals. World literature shows a growing number of incidents in recent years with marine stingrays, despite the fact that these animals only attack when harassed. This report describes an accident in which an amateur fisherman was injured by a marine stingray, probably of the Dasyatis family, on his left forearm. The puncture wound was highly painful and progressed to rhabdomyolysis. It is conjectured that lymphatic drainage, applied in an attempt to reduce edema and its complications, may have contributed to rebound increase in serum creatine kinase levels (CK) and, thus, has exacerbated the intensity of rhabdomyolysis. Therefore, as a measure of caution, lymphatic drainage should not enter current treatment protocols for similar cases, until new studies are performed in order to clarify this issue.
stingray injury; lymphatic drainage; rhabdomyolysis
CASE REPORT
Rhabdomyolysis secondary to an accident with marine stingray (Dasyatis family)
Masson AA; Ormonde do Carmo PHA; Carvalho JLV
Intensive Care Unit, Aeronautics Hospital of Afonsos (HAAF), Rio de Janeiro, Rio de Janeiro State, Brazil
Correspondence to Correspondence to: Antonio Augusto Masson Unidade de Terapia Intensiva, Hospital de Aeronáutica dos Afonsos (HAAF) Av. Mal. Fontenelle, 1628, Campo dos Afonsos 21740-002, Rio de Janeiro, RJ, Brasil Phone/fax: +55 21 3289 6700 Email: antaugmasson@gmail.com
ABSTRACT
Whenever humans come in touch with the sea, they become vulnerable to risks, most frequently on account of invading a habitat that belongs to potentially harmful aquatic animals. World literature shows a growing number of incidents in recent years with marine stingrays, despite the fact that these animals only attack when harassed. This report describes an accident in which an amateur fisherman was injured by a marine stingray, probably of the Dasyatis family, on his left forearm. The puncture wound was highly painful and progressed to rhabdomyolysis. It is conjectured that lymphatic drainage, applied in an attempt to reduce edema and its complications, may have contributed to rebound increase in serum creatine kinase levels (CK) and, thus, has exacerbated the intensity of rhabdomyolysis. Therefore, as a measure of caution, lymphatic drainage should not enter current treatment protocols for similar cases, until new studies are performed in order to clarify this issue.
Key words: stingray injury, lymphatic drainage, rhabdomyolysis.
INTRODUCTION
Whenever humans come into contact with the sea, they become vulnerable to risks. This usually happens due to human invasion of habitat that belongs to potentially harmful aquatic animals.
The most affected group consists of fishermen, surfers and unwary bathers. The last ones are common potential victims, usually affected in their lower limbs, after inadvertently stepping on stingrays hovering over the sandy seafloor. Moreover, the popularization of aquarism around the world exposes to accidents an array of workers, from veterinarians to caregivers, during daily activities that require close contact with these venomous and traumatogenic creatures.
Stingrays are members of the class Chondrichthyes, whose skeletons are all cartilage. It is placed in the subclass Elasmobranchii, as are sharks.
There are around 150 species of stingrays across the globe (1). The number of incidents caused by these traumatogenic and venomous aquatic animals has been increasing over the years. The statistics that reported 750 cases per year in the latter half of the 1960s in the United States of America (USA) jumped to 2,459 cases between 2001 and 2004, representing 0.3% of the bite or sting injuries treated in emergency departments (2, 3).
The costs of these accidents totaled more than $ 3 million, of which over $ 2.7 million was spent on emergency room visits and more than $ 500.000 on hospitalizations during the same period in the USA (3).
The condition of patients injured by marine stingrays is varied, and may include local and systemic changes such as intense local pain disproportionate to the appearance of the lesion, edema, erythema, lymphangitis and lymphadenopathy, vomiting and abdominal pain, bleeding, hypotension and shock (4, 5). There are also reports of cramps, diaphoresis, syncope, headache, and cardiac arrhythmias (6).
These animal venoms are heat-labile and composed of serotonin, 5'-nucleotidase and phosphodiesterases (7). These constituents account for the vasoconstrictor property of the venom, which causes difficulties in wound healing and myonecrosis (8).
Histopathology of the lesions caused by these animals reveals a central hemorrhagic necrosis surrounded by an infiltrate of lymphocytes and eosinophils, suggesting an immune response by the individual, which may contribute to a delay in the healing process (9).
Haddad Junior (10) evaluated a series of 236 accidents caused by marine animals in Brazil of which 25% were caused by venomous fish, a group that includes the stingrays. These animals present docile and non-aggressive behavior, attacking only when harassed (11).
This report describes a case occurred along Brazilian coast of an amateur fisherman injured by a marine stingray sting that stabbed his left forearm and evolved to rhabdomyolysis.
CASE REPORT
A 48-year-old male patient was admitted to the intensive care unit (ICU) of HAAF, transferred from Hospital of Itaguaí Rio de Janeiro, with reports of stingray accident that had happened for about 24 hours before, while practicing recreational fishing, on the Green Coast of Rio de Janeiro. The victim was fishing alone in his kayak far from the shore when he realized that he had hooked something. In his attempt to reel in the line he was surprised to find that it was a stingray. While towing it to shore, the stingray hid under his kayak. As he tried to bring it back the stingray surprised him, jumping out of water toward his kayak where it transfixed his left forearm with its retro-serrated sting.
During the initial care in the emergency room, the sting was taken out of the left forearm and the patient was treated with opioid analgesics and anti-inflammatory steroids, as coadjutant to relieve the pain, and tetanus vaccine. On the physical examination after admission to the ICU, the patient was lucid, conscious, afebrile (axillary temperature of 36ºC), acyanotic (arterial oxygen saturation of 93% in room air), dehydrated (+++/ 4), eupneic (respiratory rate of 18 bpm) and hypertensive (blood pressure of 196 x 118 mmHg) with normal coloration, good capillary refill and heart rate of 68. The patient reported severe pain in the left upper limb, with severe edema and drainage from the wound (Figure 1). As a result, the forearm showed significant functional limitation.
The authors, although attending on a secondary care basis away from the scene of the incident, attempted to collect clues about the type of stingray involved, aiming to eventually optimize the treatment plan. Images were shown to the victim consisting of those stingrays prevalent along the local coastline. He immediately recognized many characteristics of the Dasyatis family (Figure 2), able to inflict myonecrosis by at least two mechanisms as follows: sting trauma and venom action, which, in turn, leads this family to be viewed as one of the most dangerous (7, 10, 12).
The initial laboratory tests were: hematocrit = 42.8%, hemoglobin = 15.4 g/dL, white blood count 12,800 (↑) with 11% rods (↑), platelets = 260,000/mm3, K = 4.2 mEq/L, Na = 133 mEq/L (↓), glucose = 130 mg/dL (↑), urea = 28 mmol/L, creatinine = 0.8 mg/dL, creatine phosphokinase (CK) = out of range (normal range until 190 U/L), CK-MB = 267 U/L (normal range until 25 U/L). The patient's EKG was normal.
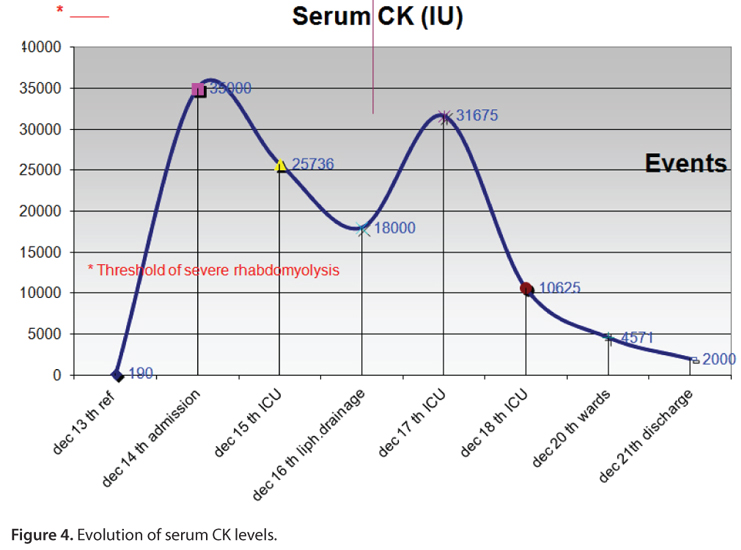
After three hours dosages of CK and CK-MB were repeated, with the following results: CK = 25,737 U/L and CK-MB = 300 U/L. Levels of CK higher than 10,000 U/L indicate rhabdomyolysis with clinical significance when associated with toxins and direct lesions. The C reactive protein (CPR) was elevated 12 mg/dL (normal = 0 to 3 mg/dL), suggesting a systemic inflammatory response.
The ultrasound of the affected limb showed an edema of the subcutaneous tissue and muscle adjacent to the skin holes formed by the entrance and exit of the stinger (Figure 3).
Faced with rhabdomyolysis, the following procedure was adopted: vigorous intravenous hydration, the parenteral administration of 2.75 L of saline 0.9%/day on average, bicarbonate solution, antibiotic therapy with oxacillin (12 g/day for a period of six days), potent analgesia, 20% mannitol, elevation of the affected limb and manual lymphatic drainage.
There was progressive decline of enzyme levels, although a peak occurred after the maneuvers of lymphatic drainage, which occurred on the second day of ICU admission and elevated enzyme levels, reaching a peak CK of 31,675 U/L (Figure 4).
The patient progressed well, with improvement in pain symptoms and edema, and was discharged from ICU after three days.
Due to the restricted movement of the arm and hand, resulting from neuropathy and loss of muscle mass, physical therapy sessions were continued for 90 days with full reversal of complaints.
DISCUSSION
The treatment of the case followed the international recommendations to prevent the myoglobinuric acute renal failure.
Several studies recommend as part of the initial protocol treatment, since the venom is heat-labile, the immersion of the affected limb in hot water (43-46ºC), for 30 to 90 minutes or the maximum period that the patient can tolerate without bringing him any harmful consequence. This measure aims to inactivate the venom, and thus obtain significant symptomatic relief (1-2, 4-6, 8).
The initial emergency care and rapid transfer to the ICU contributed to the prevention of systemic complications, especially the renal protection against myoglobinuric renal failure. These factors probably contributed to the good clinical course of the case.
Excessively high levels of serum CK reinforce the idea that one should assign more importance to stingray accidents, regardless of the magnitude of external wounds, since they possess an elevated degree of power to injure tissue, as demonstrated in this report.
The immune response of this patient may have contributed adversely to the high degree of rhabdomyolysis. The trauma caused by the sting is the additional factor that synergizes with the action of the venom.
There were no references in the literature to validate the lymphatic drainage in these cases. On the contrary, the only one found was against this practice in inflamed or infected limbs, because it could spread the infection or exacerbate the symptoms (13). This is precisely what was observed in this case, and documented in Figure 4 by the delayed rebound elevation of CK levels that had been in decline and showed a high rebound on the day after the manipulation, with no other apparent cause for this fact, except the lymphatic drainage measures performed in the ICU. This factor was considered deleterious by the authors, raising a possible contraindication in relation to this treatment modality for similar future cases, until new studies are performed to clarify this issue.
ACKNOWLEDGMENTS
We are grateful to HAAF intensive care team for their contribution during data collection.
Received: February 24, 2012
Accepted: April 2, 2012
Abstract published online: April 5, 2012
Full paper published online: August 31, 2012
CONFLICTS OF INTEREST: The authors declared no conflicts of interest.
CONSENT: Written informed consent was obtained from Division of Medical Ethics and from the patient for publication of this case report and any accompanying images.
- 1. Endom EE. Marine envenomations from coral, sea urchins, or stingrays [Internet]. Waltham (MA); 2011 Jun 8 [updated 2011 Set 10; cited 2012 Jan 19]. Available from: http://www.uptodate.com/contents/marine-envenomations-from-coral-sea-urchins-or-stingrays
- 2. Russell FE. Stingray injuries. Public Health Rep. 1959; 74(10):855-60.
- 3. O'Neil ME, Mack KA, Gilchrist J. Epidemiology of non-canine bite and sting injuries treated in U.S. emergency departments, 2001-2004. Public Health Rep. 2007;122(6):764-75.
- 4. Zoltan TB, Taylor KS, Achar SA. Health issues for surfers. Am Fam Physician. 2005;71(12):2313-7.
- 5. Weinstein S, Dart R, Staples A, White J. Envenomations: an overview of clinical toxinology for the primary care physician. Am Fam Physician. 2009;80(8):793-802.
- 6. Evans RJ, Davies RS. Stingray injury. J Accid Emerg Med. 1996;13(3):224-5.
- 7. Rodríguez, HGR, Sánchez EC, Méndez JD. Stingray poisoning, a careless aspect in México. Adv Environ Biol. 2008;2(2):54-62.
- 8. Perkins RA, Morgan SS. Poisoning, envenomation, and trauma from marine creatures. Am Fam Physician. 2004;69(4):885-90.
- 9. Germain M, Smith KJ, Skelton H. The cutaneous cellular infiltrate to stingray envenomization contains increased TIA+ cells. Br J Dermatol. 2000;143(5):1074-7.
- 10. Haddad Junior V. Aquatic animals of medical importance in Brazil. Rev Soc Bras Med Trop. 2003;36(5):591-7.
- 11. Diaz JH. The epidemiology, evaluation, and management of stingray injuries. J La State Med Soc. 2007;159(4):198-204.
- 12. Vianna M. FishBase [Internet]; 2012 Mar 31 [updated 2012 Feb; cited 2003 Out 27]. Available from: http://www.fishbase.org
- 13. Mohler ER, Mondry TE. Lymphedema: prevention and treatment [Internet]. Waltham (MA); 2011 Set 15 [updated 2011 Dez 08; cited 2012 Jan 19]. Available from: http://www.uptodate.com/contents/lymphedema-prevention-and-treatment
Publication Dates
-
Publication in this collection
14 Sept 2012 -
Date of issue
2012
History
-
Received
24 Feb 2012 -
Accepted
02 Apr 2012