Abstracts
Objective:
To identify the incidence of alloimmunization in sickle cell disease patients, as well as autoantibodies and the phenotypic profile of these patients for the following erythrocyte antigen groups: Rh, Kell, Kidd, Duffy and MNS.
Methods:
fifty-seven patients were evaluated during follow-up at the Anemia Outpatient Clinic of Irmandade da Santa Casa de São Paulo, where a search for irregular antibodies and phenotyping was carried out.
Results:
Patients’ median alloimmunization age in sickle cell disease was 25 years, and irregular antibodies were found in 22.6% of them. Anti-Kell antibody was the most frequent (7.5%) followed by anti-C (5.7%).
Conclusion:
The prevalence of alloimmunization and of patients with autoantibodies among individuals with sickle cell disease followed at the Anemia Outpatient Clinic of Irmandade da Santa Casa de Misericórdia de São de Paulo was determined. The risk of alloimmunization was higher in patients who received more than 3 red blood cell units in the past 2 years. The most prevalent alloantibodies were anti-Kell and anti-C.
Anemia, sickle cell/immunology; Blood transfusion; Autoantibodies; Blood group antigens
Objetivo:
Identificar a incidência de aloimunização em pacientes com doença falciforme, a incidência de autoanticorpos e o perfil fenotípico dos pacientes para os seguintes grupos de antígenos eritrocitários: Rh, Kell, Kidd, Duffy e MNS.
Métodos:
Foram avaliados 57 pacientes em acompanhamento no Ambulatório de Anemias da Irmandade da Santa Casa de São Paulo, sendo realizada a pesquisa de anticorpos irregulares e a fenotipagem eritrocitária.
Resultados:
A mediana de idade foi de 25 anos, sendo que 22,6% dos pacientes apresentavam anticorpos irregulares. O anticorpo anti-Kell foi o mais frequente (7,5%), seguido de anti-C (5,7%).
Conclusão:
Foi determinada a prevalência de aloimunização e de pacientes com autoanticorpos em indivíduos com anemia falciforme seguidos no Ambulatório de Anemias da Irmandade da Santa Casa de Misericórdia de São de Paulo. O risco de aloimunização foi maior em pacientes que receberam mais do que 3 unidades de hemácias nos últimos 2 anos. Os aloanticorpos mais prevalentes foram anti-Kell e anti-C.
Anemia falciforme/imunização; Transfusão de sangue; Auto-anticorpos; Antígenos de grupos sanguíneos
INTRODUCTION
Sickle cell disease is one of the most prevalent genetic diseases in the world. According to estimates of the World Health Organization (WHO), the global incidence of hemoglobin diseases is approximately 4.5%(11. Cançado RD. Doenças falciformes. Prática Hospitalar. 2007;9(50):61-4.). The distribution of the S gene in Brazil is very heterogeneous and depends basically on the miscegenation of the Brazilian population. In Brazil, the prevalence of heterozygotes for hemoglobin S is higher in the North and Northeast regions(11. Cançado RD. Doenças falciformes. Prática Hospitalar. 2007;9(50):61-4.).
Data of the Brazilian Ministry of Health estimate there are roughly 7 million carriers of the sickle cell trait and that the annual incidence of newborns with the sickle cell trait is 200,000(11. Cançado RD. Doenças falciformes. Prática Hospitalar. 2007;9(50):61-4.). Regarding sickle cell disease, the estimated number of Brazilians with the disease ranges between 25 and 30 thousand individuals, and the incidence of new cases per year is estimated to be around 3,500(11. Cançado RD. Doenças falciformes. Prática Hospitalar. 2007;9(50):61-4.).
Hemoglobin S is formed by the replacement of a thymine by an adenine, in the sixth codon of the beta gene, leading to the insertion of valine instead of glutamine, in position six of the beta chain, originating hemoglobinopathy SS, also called sickle cell disease. This small change in the structure of the chain is responsible for deep changes in the stability of the molecule and in its solubility. Such change is capable of causing polymerization of hemoglobin chains when its deoxygenation occurs (22. Costa FF. Hematologia: fundamentos e prática. São Paulo: Atheneu; 2004.,33. Alexy T, Pais E, Armstrong JK, Meiselman HJ, Johnson CS, Fisher TC. Rheologic behavior of sickle and normal red blood cell mixtures in sickle plasma: implications for transfusion therapy. Transfusion. 2006;46(6):912-8.).
In the 1930´s, the role of blood transfusions to treat pain crises and manage vessel-occlusive phenomena was acknowledged(33. Alexy T, Pais E, Armstrong JK, Meiselman HJ, Johnson CS, Fisher TC. Rheologic behavior of sickle and normal red blood cell mixtures in sickle plasma: implications for transfusion therapy. Transfusion. 2006;46(6):912-8.,44. Davies SC, Olatunji PO. Blood transfusion in sickle cell disease. Vox Sang. 1995;68(3):145-51.). Blood transfusions have been important to treat stroke patients and for the prophylaxis of new ischemic events(44. Davies SC, Olatunji PO. Blood transfusion in sickle cell disease. Vox Sang. 1995;68(3):145-51.,55. Wang WC. Wintrobes clinical hematology. Philadelphia (PA): Lippincot Williams & Wilkins; 2004.).
Chronic blood transfusion programs are becoming increasingly common in our environment for two main reasons: red blood cell infusion increases oxygen carrying capacity and decreases tissue hypoxia(55. Wang WC. Wintrobes clinical hematology. Philadelphia (PA): Lippincot Williams & Wilkins; 2004.,66. Swerdlow PS. Red cell exchange in sickle cell disease. Hematology Am Soc Hematol Educ Program. 2006:48-53.).
Complications from chronic transfusion treatment include the risk of infections by viruses and bacteria, iron overload and red blood cell alloimunization, that has a frequency ranging between 2.5 and 76% in certain centers(66. Swerdlow PS. Red cell exchange in sickle cell disease. Hematology Am Soc Hematol Educ Program. 2006:48-53.,77. Fabrom Junior A, Bordin J. Estudo da significância clínica de aloanticorpos eritrocitários em pacientes com anemia falciforme [resumo]. Rev Bras Hematol Hemoter. 2001;23(2):121-2.).
Alloimunization limits the availability of compatible red blood cell concentrates for future transfusions, in addition to being a risk for late hemolysis and severe hyper-hemolysis. Alloimmunization is related to the following factors: patient age, number of transfusions received, antigenic differences between patients and donors(88. Sakhalkar VS, Roberts K, Hawthorne LM, McCaskill DM, Veillon DM, Caldito GC, et al. Allosensitization in patients receiving multiple blood transfusions. Ann N Y Acad Sci. 2005;1054:495-9.–1010. American Association of Blood Banks. Technical manual. 13th ed. Bethesda (MD): AABB; 1999.).
The antigens most frequently involved in alloimmunization are antigens of the Rh, Kell, Kidd, Duffy, Lewis and MNS groups (99. Rosse WF, Gallagher D, Kinney TR, Castro O, Dosik H, Moohr J, et al. Transfusion and alloimmunization in sickle cell disease. The Cooperative Study of Sickle Cell Disease. Blood. 1990;76(7):1431-7.,1111. Moreira Júnior G, Bordin JO, Kuroda A, Kerbauy J. Red blood cell alloimmunization in sickle cell disease: the influence of racial and antigenic pattern differences between donors and recipients in Brazil. Am J Hematol. 1996;52(3):197-200.).
OBJECTIVE
To evaluate the incidence of red blood cell alloimmunization in patients on sickle cell disease follow up in a single center in the city of São Paulo, the incidence of autoantibodies and the phenotype profile of patients for the following red blood cell antigen groups: Rh, Kell, Kidd, Duffy and MNS.
METHODS
Between 2007 and 2008, 57 patients diagnosed with sickle cell disease and on follow up at the Anemia Outpatient Clinic of Irmandade da Santa Casa de Misericórdia de São de Paulo were studied.
Inclusion criteria were: diagnosis of sickle cell disease, with phenotypes Hb SS, Hb SC, Hb Sβ+ thal, Hb Sβ0, Hb Sα tal. All diagnoses were confirmed by hemoglobin immunoelectrophoresis; age above 14 years; and a signed consent form. Clinical data were collected through a questionnaire answered by patients themselves or by a legal guardian. The exclusion criterion was having received a blood transfusion up to 90 days before being included in the study.
All material collected was sent to the immunohematology lab of the Irmandade da Santa Casa de Misericóridia de São Paulo Blood Bank, where ABO and Rh typing was performed, in addition to searching for alloantibodies against red blood cell antigens, according to the standard technical protocols of the blood bank.
When antibodies were observed, they were identified through a labeled red blood cell panel reaction, using column agglutination methods and gel centrifugation (ID-Diapanel and ID-Diapanel-P, DiaMed AG)(1212. Murao M, Viana MB. Risk factors for alloimmunization by patients with sickle cell disease. Braz J Med Biol Res. 2005;38(5):675-82.,1313. Mollison PL, Engelfriet CP, Contreras M. Blood transfusion in clinical medicine. Oxford: Blackwell Scientific Publications; 1997.).
After the identification, antibody elution was performed, followed by phenotyping for the following blood systems: Rh, Kell, Kidd, Duffy and MNS, according to the standard blood bank protocol.
Statistical analysis of association variables was performed using χ2 and Mann-Whitney tests. All tests were performed with the Statistical Package for the Social Sciences (SPSS) 15 software.
RESULTS
Of the 57 patients evaluated initially, 4 patients could not be phenotyped, because they had a double antigen population, and were excluded from the study.
The final sample was comprised of 53 patients, 30 were women (56.6%). The median age was 30 years. Regarding ethnicity, 44 patients were black (83%) and 9 white (17%). As to schooling, 17 patients (32.1%) had only fundamental schooling, 27 (50.9%) patients had completed high school and only 7 patients (13.2%) had gone to college (Table 1).
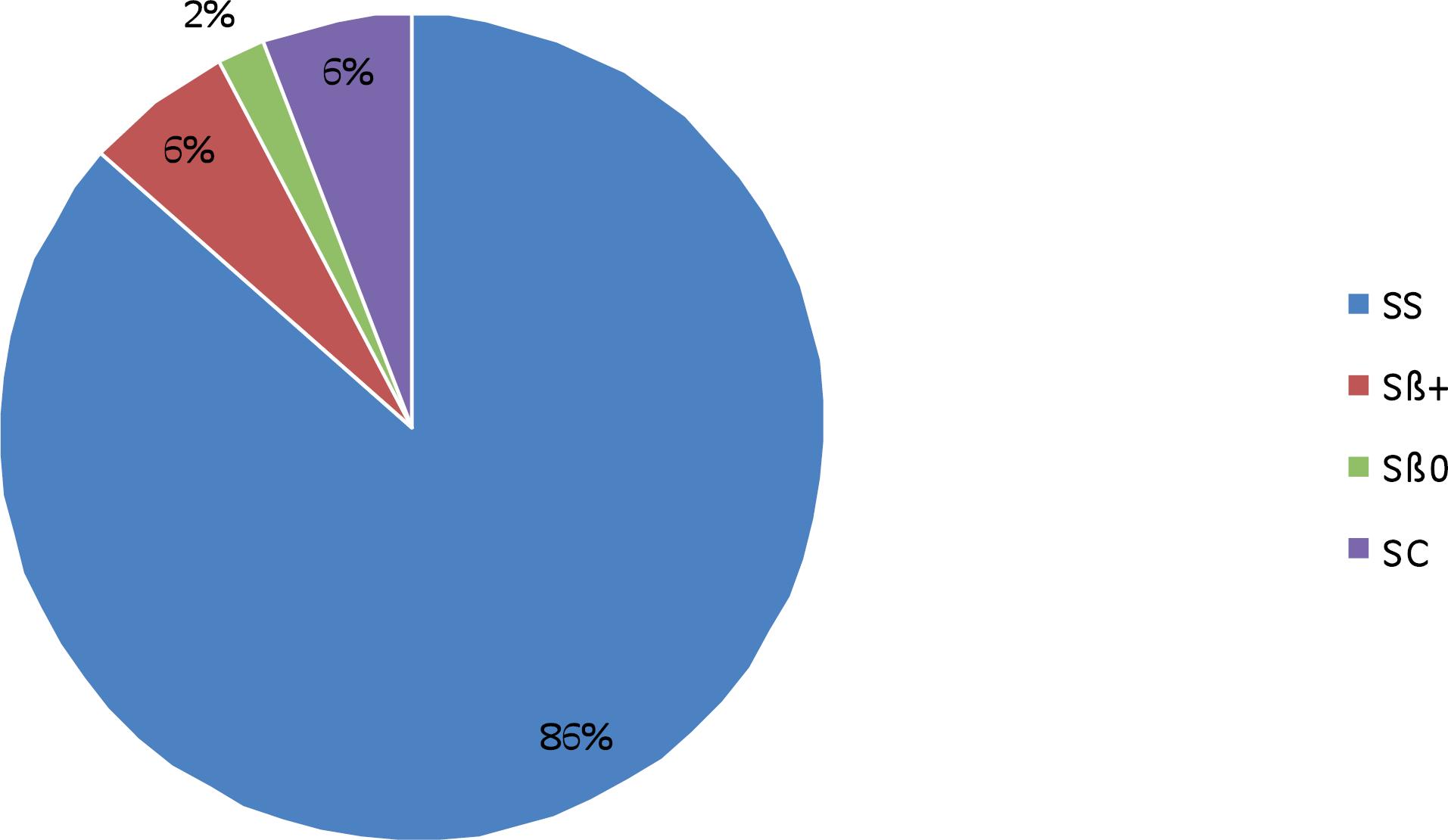
As to underlying diagnosis, 45 patients were SS (84.9%), three patients were SC (5.7%), three patients were Sβ+ (5.7%); only 1 patient with a diagnosis of Sβ-thal (1.9%) and Sα/thal (1.9%) were found (Figure 1).
Regarding the number of transfusions received throughout life, results can be seen on Table 2. Of patients who received blood transfusions, 9 (17%) were on an ongoing transfusion regimen.
The presence of irregular antibodies was positive in 12 patients (22.6%) and negative in 41 (77.4%). The presence of autoantibodies was positive in six (11.3%) patients.
As to blood ABO and Rh group type, results can be seen on tables 3 and 4, respectively.
The frequency of red blood cell antigens can be seen on Table 5 and the frequency of the Rh phenotype is on Table 6.
The presence of alloantibodies was found in 12 (22.6%) patients, with 4 patients (7%) presenting 2 different alloantibodies and 1 patient (1.8%) with 4 different alloantibodies. There was a total of 15 different alloantibodies, in that, of the 15 alloantibodies identified, 33.3% were against Rhesus group antigens and 26.6% against Kell group antigens. The specificity of the alloantibodies found is registered in Table 7.
The risk of alloimmunization in relation to age, sex, genotype, and number of transfusions in the past 2 years was not statistically significant, but there was a trend toward a higher risk of alloimmunization for patients over 30 years of age (p < 0.658). Regarding sex, there was no difference as to the risk of alloimmunization, although women with over three pregnancies showed a strong trend toward alloimmunization (p < 0.12).
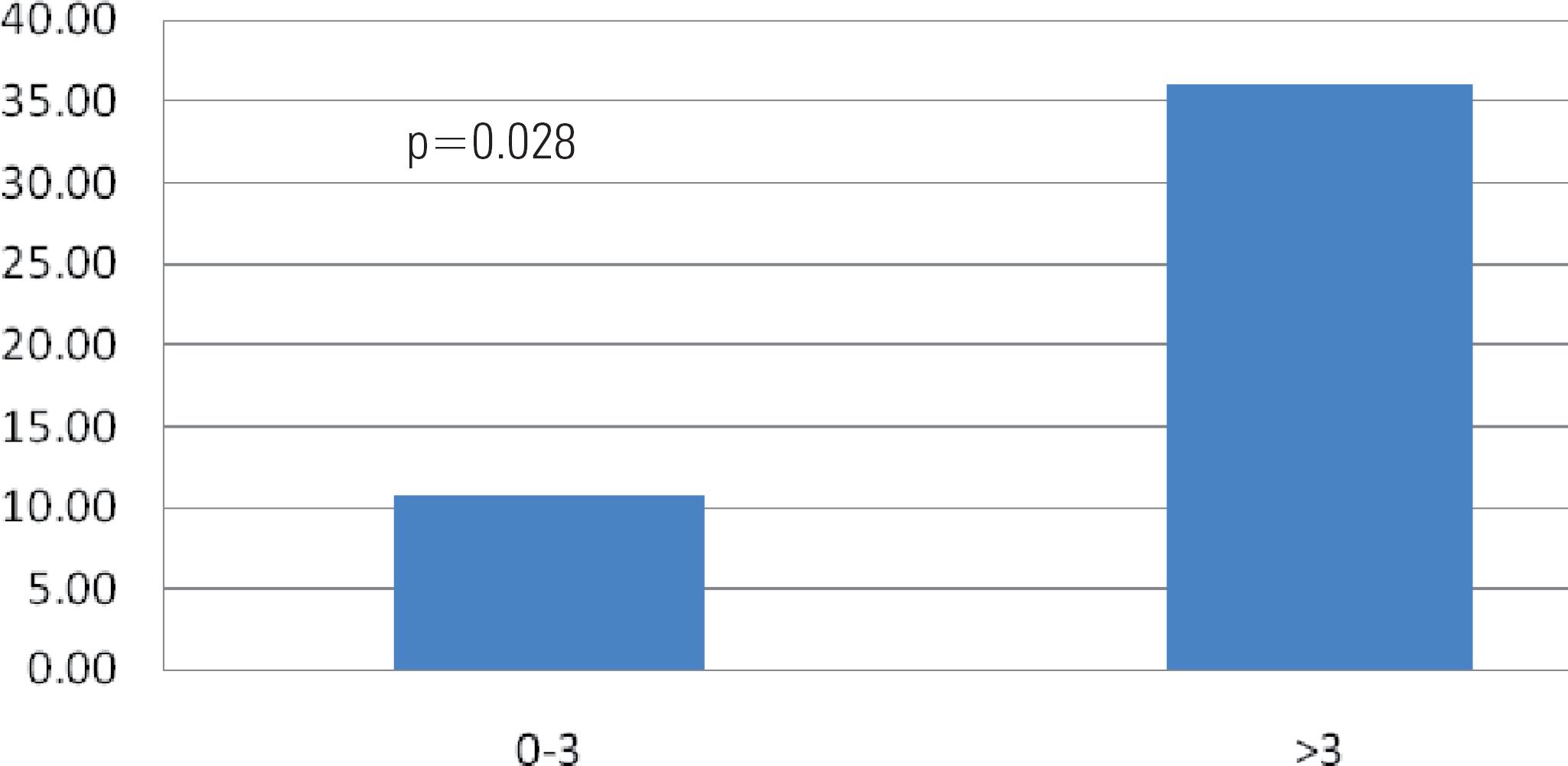
As to the number of transfusions, the risk for patients with over five transfusions throughout life, was observed to be higher than for patients that received up to five transfusions (p < 0.106); when patients who received more than 3 transfusions in the past two years were compared to patients who received up to 3 transfusions, the risk of alloimmunization was statistically significant (p < 0.028) (Figures 2 and 3).
DISCUSSION
The frequency of alloimmunization found in the study was compatible with data in the literature. Several studies have shown rates that range between 2.6 and 47%(99. Rosse WF, Gallagher D, Kinney TR, Castro O, Dosik H, Moohr J, et al. Transfusion and alloimmunization in sickle cell disease. The Cooperative Study of Sickle Cell Disease. Blood. 1990;76(7):1431-7.–1111. Moreira Júnior G, Bordin JO, Kuroda A, Kerbauy J. Red blood cell alloimmunization in sickle cell disease: the influence of racial and antigenic pattern differences between donors and recipients in Brazil. Am J Hematol. 1996;52(3):197-200.). The studies that have lower alloimmunization rates include predominantly pediatric patients. In Brazil, alloimmunization rates are referred as ranging between 3.2 and 20.8%(1111. Moreira Júnior G, Bordin JO, Kuroda A, Kerbauy J. Red blood cell alloimmunization in sickle cell disease: the influence of racial and antigenic pattern differences between donors and recipients in Brazil. Am J Hematol. 1996;52(3):197-200.,1212. Murao M, Viana MB. Risk factors for alloimmunization by patients with sickle cell disease. Braz J Med Biol Res. 2005;38(5):675-82.). Again, the lower alloimmunization rates were carried out predominantly with children under 15 years of age; in the present study, none of the patients were less than 16, which may show a difference in the risk of alloimmunization for older patients(99. Rosse WF, Gallagher D, Kinney TR, Castro O, Dosik H, Moohr J, et al. Transfusion and alloimmunization in sickle cell disease. The Cooperative Study of Sickle Cell Disease. Blood. 1990;76(7):1431-7.–1111. Moreira Júnior G, Bordin JO, Kuroda A, Kerbauy J. Red blood cell alloimmunization in sickle cell disease: the influence of racial and antigenic pattern differences between donors and recipients in Brazil. Am J Hematol. 1996;52(3):197-200.).
The higher frequency of alloimmunization found in this study, in comparison to other Brazilian studies, may be due to the fact that here the antibody identification method used was tube and gel centrifugation, increasing diagnostic sensitivity in relation to the studies that used the tube centrifugation method only(1212. Murao M, Viana MB. Risk factors for alloimmunization by patients with sickle cell disease. Braz J Med Biol Res. 2005;38(5):675-82.,1313. Mollison PL, Engelfriet CP, Contreras M. Blood transfusion in clinical medicine. Oxford: Blackwell Scientific Publications; 1997.).
However, in the present study, alloimmunization rates found were lower than in international studies, which may reflect higher phenotype compatibility between blood donors and the patients in this population. Other studies are necessary in order to confirm this assumption, because there is only one study that compares phenotype of blood transfusion sickle cell disease donors and receptors in Brazil(1010. American Association of Blood Banks. Technical manual. 13th ed. Bethesda (MD): AABB; 1999.).
The specificity of the antibodies found in this study was similar to that of other studies, due to the high immunogenicity of Rh and Kell antigens (9,13,14).
Although alloimmunization is described as more prevalent in women, in the present study sex was not considered a risk factor, following the trend of other domestic studies(1414. King KE, Shirey RS. Transfusion management of patients with sickle cell disease: the continuing dilemma. Transfusion. 2010;50(1):2-4.,1515. Zimring JC, Hair GA, Deshpande SS, Horan JT. Immunization to minor histocompatibility antigens on transfused RBCs through crosspriming into recipient MHC class I pathways. Blood. 2006;107(1):187-9.).
Like in other studies, older patients tended to present a higher risk of alloimmunization, although without statistical significance. The greater immunological response to antigens, more transfusions and the presence of previous pregnancies are some of the factors that may explain the higher alloimmunization rates in adults.
In the present study, the risk of alloimmunization was associated with the number of blood transfusions, which agreed with the literature(12,14-16). The risk of alloimmunization for patients who received over 30 transfusions was statistically higher than patients who received up to 5 transfusions. Patients who received more than 3 transfusions in the past 2 years had a statistically significant higher risk for alloimmunization than patients who received up to 3 blood cell units in the past 2 years. These data are in agreement with the literature and are basically due to the higher exposure of transfused patients to red blood cell antigens.
Unlike other countries where race was an important risk factor for alloimmunization, in the present study such factor did not prevail and in our environment there also was no phenotype discrepancy between patients and blood donors, probably due to more miscegenation in our population.
There are major differences in the expression of the Rh complex in black and caucasian individuals, and black individuals are more prone to be D positive when compared to caucasians(1717. Novaretti MCZ, Dorhlhiac-Llacer PE, chamone DAF. Estudo de grupos sanguíneos em doadores de sangue caucasoides e negroides na cidade de São Paulo. Rev Bras Hematol Hemoter. 2000;22(1):23-32.). In our study, most patients were D positive, and R1r and R2r were the most prevalent Rh phenotypes.
CONCLUSIONS
The prevalence of alloimmunization and of patients with autoantibodies in individuals with sickle cell disease followed at the Anemia Outpatient Clinic of Irmandade da Santa Casa de Misericórdia de São de Paulo was determined. The risk of alloimmunization was higher for patients who received more than 3 units of red blood cells in the past 2 years. The most prevalent alloantibodies were anti-Kell and anti-C.
Alloimmunization in patients with sickle cell disease who receive blood transfusion is a factor that may be an important obstacle to treatment, making the treatment of severe complications difficult, such as acute chest syndrome or stroke. Measures to prevent alloimmunization should be taken by blood banks.
-
Study carried out at Anemia Outpatient Clinic of Irmandade da Santa Casa de Misericórdia de São de Paulo – Sao Paulo (SP), Brazil.
REFERENCES
-
1Cançado RD. Doenças falciformes. Prática Hospitalar. 2007;9(50):61-4.
-
2Costa FF. Hematologia: fundamentos e prática. São Paulo: Atheneu; 2004.
-
3Alexy T, Pais E, Armstrong JK, Meiselman HJ, Johnson CS, Fisher TC. Rheologic behavior of sickle and normal red blood cell mixtures in sickle plasma: implications for transfusion therapy. Transfusion. 2006;46(6):912-8.
-
4Davies SC, Olatunji PO. Blood transfusion in sickle cell disease. Vox Sang. 1995;68(3):145-51.
-
5Wang WC. Wintrobes clinical hematology. Philadelphia (PA): Lippincot Williams & Wilkins; 2004.
-
6Swerdlow PS. Red cell exchange in sickle cell disease. Hematology Am Soc Hematol Educ Program. 2006:48-53.
-
7Fabrom Junior A, Bordin J. Estudo da significância clínica de aloanticorpos eritrocitários em pacientes com anemia falciforme [resumo]. Rev Bras Hematol Hemoter. 2001;23(2):121-2.
-
8Sakhalkar VS, Roberts K, Hawthorne LM, McCaskill DM, Veillon DM, Caldito GC, et al. Allosensitization in patients receiving multiple blood transfusions. Ann N Y Acad Sci. 2005;1054:495-9.
-
9Rosse WF, Gallagher D, Kinney TR, Castro O, Dosik H, Moohr J, et al. Transfusion and alloimmunization in sickle cell disease. The Cooperative Study of Sickle Cell Disease. Blood. 1990;76(7):1431-7.
-
10American Association of Blood Banks. Technical manual. 13th ed. Bethesda (MD): AABB; 1999.
-
11Moreira Júnior G, Bordin JO, Kuroda A, Kerbauy J. Red blood cell alloimmunization in sickle cell disease: the influence of racial and antigenic pattern differences between donors and recipients in Brazil. Am J Hematol. 1996;52(3):197-200.
-
12Murao M, Viana MB. Risk factors for alloimmunization by patients with sickle cell disease. Braz J Med Biol Res. 2005;38(5):675-82.
-
13Mollison PL, Engelfriet CP, Contreras M. Blood transfusion in clinical medicine. Oxford: Blackwell Scientific Publications; 1997.
-
14King KE, Shirey RS. Transfusion management of patients with sickle cell disease: the continuing dilemma. Transfusion. 2010;50(1):2-4.
-
15Zimring JC, Hair GA, Deshpande SS, Horan JT. Immunization to minor histocompatibility antigens on transfused RBCs through crosspriming into recipient MHC class I pathways. Blood. 2006;107(1):187-9.
-
16Kozarski TB, Howanitz PJ, Howanitz JH, Lilic N, Chauhan YS. Blood transfusions leading to apparent hemoglobin C, S, and O-Arab hemoglobinopathies. Arch Pathol Lab Med. 2006;130(12):1830-3.
-
17Novaretti MCZ, Dorhlhiac-Llacer PE, chamone DAF. Estudo de grupos sanguíneos em doadores de sangue caucasoides e negroides na cidade de São Paulo. Rev Bras Hematol Hemoter. 2000;22(1):23-32.
Publication Dates
-
Publication in this collection
Apr-Jun 2011
History
-
Received
01 Jan 2011 -
Accepted
19 Apr 2011


 Source: Anemia Outpatient´s Clinic - Irmandade da Santa Casa de Misericórdia de São Paulo.
Source: Anemia Outpatient´s Clinic - Irmandade da Santa Casa de Misericórdia de São Paulo.