Abstracts
OBJECTIVE: To compare results of hysteroscopic polypectomy of the endometrium performed in an outpatient clinic, under no anesthesia, to conventional hysteroscopic polypectomy under anesthesia in the operating theatre, assessing success rate, procedure time and complications; and to measure pain referred by patients in both groups. METHODS: An observational cross-sectional study of 60 patients with hysteroscopic diagnosis of endometrial polyps, divided into two groups: the Outpatient Group, comprising patients submitted to outpatient´s hysteroscopic polypectomy by continuous flow vaginoscopy using endoscopic forceps under no anesthesia, and the Conventional Group with patients submitted to hysteroscopic polypectomy in the operating theater, using a monopolar resectoscope under anesthesia. RESULTS: The groups were similar as to age, parity, mode of delivery and menopausal status. Both groups presented 100% efficacy in exeresis of polyps. The mean time of procedure was 7 minutes in the Outpatient Group and 35.16 minutes in the Conventional Group. In the Outpatient Group, menopausal patients (p=0.04) and those with polyps >1cm (p=0.01) had longer procedures. Using the Verbal Analog Scale of Pain, the mean score of pain referred by patients during the procedure was 2.93 in the Outpatient Group and, after anesthetic effect, 1.42 in the Conventional Group. There were no complications in the Outpatient Group. There was one case of uterine perforation and one case of false passage in the Conventional Group. CONCLUSION: Hysteroscopic polypectomy performed in an outpatient setting under no anesthesia is a well-tolerated procedure. As compared to conventional treatment, it displays the same efficacy, but the procedure time is shorter and the complication rate is lower.
Polyps; Hysteroscopy; Pain measurement; Outpatients' surgical procedures; Endometrium; Anesthesia
OBJETIVO: Comparar resultados da polipectomia histeroscópica endometrial efetuada ambulatorialmente, sem anestesia, com polipectomia histeroscópica convencional sob anestesia, em centro cirúrgico, avaliando taxa de sucesso, tempo de procedimento e complicações. Mensurar dor aferida pela paciente nos dois grupos. MÉTODOS: Estudo transversal observacional de 60 pacientes com diagnóstico histeroscópico de pólipo endometrial divididas em dois grupos: Grupo Ambulatorial, composto por pacientes submetidas à polipectomia histeroscópica ambulatorial, utilizando-se pinça endoscópica em histeroscópio operatório ambulatorial de fluxo contínuo, por meio de vaginoscopia sem anestesia, e Grupo Convencional com pacientes submetidas à polipectomia histeroscópica em centro cirúrgico, utilizando-se ressectoscópio monopolar sob anestesia. RESULTADOS: Os grupos foram similares quanto a idade, paridade, tipo de parto e presença ou não de menopausa. Ambos os grupos apresentaram 100% de eficácia na exérese dos pólipos. O tempo médio de procedimento foi de 7 minutos no Grupo Ambulatorial e 35,16 minutos no Grupo Convencional. No Grupo Ambulatorial, as pacientes após a menopausa (p=0,04) e aquelas com pólipos >1cm (p=0,01) apresentaram tempo de procedimento maior. Durante o procedimento,a média de dor referida pelas pacientes, segundo a Escala Analógica Verbal de Dor, no Grupo Ambulatorial, foi de 2,93 e, após efeito anestésico do procedimento no Grupo Convencional, foi de 1,42 pontos. Não houve complicações no Grupo Ambulatorial. No Grupo Convencional, registraram-se um caso de perfuração uterina e um de falso trajeto. CONCLUSÃO: A polipectomia histeroscópica realizada em regime ambulatorial, sem anestesia, é um procedimento bem tolerado. Quando comparada ao tratamento convencional, apresenta a mesma eficácia, porém com menor tempo gasto no procedimento e menor índice de complicações.
Pólipos; Histeroscopia; Medição da dor; Procedimentos cirúrgicos ambulatoriais; Endométrio; Anestesia
ORIGINAL ARTICLE
IHospital do Servidor Público Estadual "Francisco Morato de Oliveira" - HSPE-FMO, São Paulo (SP), Brazil
IIDivision of Gynecological Endoscopy, Department of Gynecology and Obstetrics, Hospital do Servidor Público Estadual "Francisco Morato de Oliveira" - HSPE-FMO, São Paulo (SP), Brazil
IIIMedical undergraduate student, Universidade Cidade de São Paulo - UNICID, São Paulo (SP), Brazil; Hospital do Servidor Público Estadual "Francisco Morato de Oliveira" - HSPE-FMO, São Paulo (SP), Brazil
Corresponding author
ABSTRACT
OBJECTIVE: To compare results of hysteroscopic polypectomy of the endometrium performed in an outpatient clinic, under no anesthesia, to conventional hysteroscopic polypectomy under anesthesia in the operating theatre, assessing success rate, procedure time and complications; and to measure pain referred by patients in both groups.
METHODS: An observational cross-sectional study of 60 patients with hysteroscopic diagnosis of endometrial polyps, divided into two groups: the Outpatient Group, comprising patients submitted to outpatient´s hysteroscopic polypectomy by continuous flow vaginoscopy using endoscopic forceps under no anesthesia, and the Conventional Group with patients submitted to hysteroscopic polypectomy in the operating theater, using a monopolar resectoscope under anesthesia.
RESULTS: The groups were similar as to age, parity, mode of delivery and menopausal status. Both groups presented 100% efficacy in exeresis of polyps. The mean time of procedure was 7 minutes in the Outpatient Group and 35.16 minutes in the Conventional Group. In the Outpatient Group, menopausal patients (p=0.04) and those with polyps >1cm (p=0.01) had longer procedures. Using the Verbal Analog Scale of Pain, the mean score of pain referred by patients during the procedure was 2.93 in the Outpatient Group and, after anesthetic effect, 1.42 in the Conventional Group. There were no complications in the Outpatient Group. There was one case of uterine perforation and one case of false passage in the Conventional Group.
CONCLUSION: Hysteroscopic polypectomy performed in an outpatient setting under no anesthesia is a well-tolerated procedure. As compared to conventional treatment, it displays the same efficacy, but the procedure time is shorter and the complication rate is lower.
Keywords: Polyps; Hysteroscopy; Pain measurement; Outpatients' surgical procedures; Endometrium; Anesthesia
INTRODUCTION
The endometrial polyp is a focal hyperplasia of the basal layer of the endometrium, which originates a localized tumor and is covered by glandular epithelium. In histology, it is recognized by glands of varied aspect, fibrous stroma and vessels with thickened walls(1). Polyps may be classified histologically as functional, atrophic or hyperplastic, according to the tropism of the epithelium that covers them(1). However, this classification has practically no relation to the patient's clinical picture and does not imply treatment or prognosis(2). The pathogenesis of the endometrial polyp is similar to that of endometrial hyperplasia. The concentration of estrogen and progesterone receptors on the polyp of the endometrium is greater in the glandular epithelium than in the stroma and normal endometrium(3). Polyps may be single or multiple, of various sizes, sessile or pediculate, and their vascularized base may externalize through the uterine cervix(1). They account for approximately one fourth of the cases of abnormal uterine bleeding (AUB) in women before and after menopause.
Metrorrhagia is the most frequent symptom. Less frequent symptoms include menorrhagia and exteriorization of the polyp through the cervical canal. Nevertheless, most polyps are asymptomatic(4). Over the last years, facilitated access to the uterine cavity by means of transvaginal ultrasonography and hysteroscopy has increased the frequency of diagnosis of endometrial polyps.
Its prevalence in women with AUB varies between 10 and 30%. It is rare during the prepubertal phase, and the highest incidence occurs between 51 and 70 years of age(5).
During the reproductive period, in most cases the diagnosis of endometrial polyp is made in symptomatic patients with AUB, or in infertile patients submitted to diagnostic hysteroscopy(2). After menopause, 70 to 75% of patients with endometrial polyps are asymptomatic and present with the single finding of endometrial thickening, generally focal, diagnosed by transvaginal ultrasonography(6).
Endometrial polyps rarely suffer malignant transformation. Endometrial hyperplasia with atypia occurs in approximately 3.1% of patients(5). The frequency of malignity associated with endometrial polyps varies from 0.59 to 3.2%(7). The risk of malignity seems to be greater in women after menopause, with ages over 60 years or with AUB. The association between this risk and a polyp diameter greater than 1 cm, obesity, hypertension or diabetes was reported in a few studies(8,9).
Endometrial polyps can be diagnosed by ultrasound, hysterosonography, hysterosalpingography, endometrial biopsy, and uterine curettage, but diagnostic hysteroscopy is considered the method with the greatest sensitivity and specificity, with values of 95.3 and 95.4%, respectively(10). This test easily identifies polypoid lesions and allows guided biopsy of the lesion. Although it evaluates with details the entire uterine cavity, it might not differentiate benign from malignant polyps(2). Despite being considered benign lesions, there is still no consensus as to the best management regarding the disease. There are authors who suggest their systematic removal(7). Others propose more conservative treatments, recommending their removal only in symptomatic cases, such as, for example, in AUB and infertility(11).
The treatment of asymptomatic endometrial polyps has been discussed by various authors. Ben-Aire et al.(12) concluded that asymptomatic polyps, after menopause, should be removed and that small polyps, in menacme, may be observed. However, Lieng et al. suggested hysteroscopic resection of endometrial polyps in symptomatic and asymptomatic women due to the similar rate of malignity between these two groups(13). Conventional hysteroscopic polypectomy performed in an operating room, requires cervical dilation and anesthesia, which increases the risk of complications(14). After the 1990´s, the development of hysteroscopes with a smaller diameter, continuous flow and accessory working channels enabled the use of surgical instruments to treat uterine conditions during diagnosis, such as outpatient polypectomy, without the need for cervical dilation and anesthesia(14-16).
Several studies demonstrated that outpatient hysteroscopic polypectomy is an effective procedure, with high levels of satisfaction for the patient when compared to the procedure carried out at a day hospital(14,17,18).
OBJECTIVE
The objective of this present study was to compare the results of conventional outpatient hysteroscopic endometrial polypectomy with no anesthesia to those of conventional endometrial polypectomy performed under anesthesia in an operating room, assessing the efficacy of the procedure, time spent on it and pain reported by the patient during or after the procedure and complications.
METHODS
An observational cross-sectional study was conducted with 60 patients treated at the Gynecologic Endoscopy Division of the Hospital do Servidor Público Estadual "Francisco Morato de Oliveira" (HSPE-FMO), with hysteroscopic diagnosis of endometrial polyp. This project was approved by Research Ethics Committee of the Instituto de Assistência ao Servidor Público Estadual de São Paulo (IAMSPE).
A total of 30 patients submitted to hysteroscopic polypectomy of the endometrium performed at the hysteroscopy outpatient clinic comprised the Outpatient Group (OG), and 30 patients submitted to conventional hysteroscopic polypectomy, performed in the operating room, formed the Conventional Group (CG). All procedures were carried out by a gynecologist licensed in gynecological endoscopy.
The study included women of different age groups, with hysteroscopic diagnosis of endometrial polyp <2 cm in size and with a maximum of three in number. The procedure was explained in detail to each patient before it was performed, and the patient signed an Informed Consent Form authorizing her inclusion into the study.
All patients answered a questionnaire applied by the medical team at the time of admission, with the objective of evaluating epidemiological data, such as age, number of pregnancies, type of delivery and menopause. Additionally, information regarding the surgery was recorded, such as site, size and number of polyps, complete or incomplete resection, and duration of the procedure. Complications were also reported.
Quantification of pain was made by means of the discrete quantitative Pain Verbal Rating Scale (VRS)(19,20), that varies from 0 to 10 (equivalent to no pain and the worst pain experienced, respectively). Patients from the OG group quantified pain immediately after the procedure, whereas in the CG group, pain was assessed before hospital discharge, after the effects of the spinal anesthesia had worn off.
For the most part, the groups were made up of women after menopause (76.6%), with a mean age of 58.2 years. The mean age of menopause was similar in both groups: 48.52 years in the OG group and 47.61 years in the CG group, and there was no difference in frequency of patients after menopause in both groups. Of the total, 73% of the patients had two or more prior deliveries, and 5.9% were nulliparous. Most patients (60%) had had at least one prior vaginal delivery. The mean number of gestations and the frequency of patients with vaginal delivery and caesarian delivery were similar between the two groups studied (Table 1).
In patients from the OG group, the hysteroscopic polypectomy was performed immediately after the diagnosis of endometrial polyps with <2cm in size and a maximum of three in number. This procedure was performed in the outpatient clinic, with no anesthesia or analgesia. The technique used was vaginoscopy, as described by Bettocchi and Selvaggi(21), which consists of performing the test without prior digital vaginal examination and without the use of speculum or Pozzi forceps to traction the cervix. A 2.9-mm-scope was used, with a 30º angle, an internal inflow sheath, final diameter of 4mm and oval distal extremity (Bettocchi hysteroscope, Karl Storz®, Germany). For vaginal distension, 0.9% saline solution was used, at room temperature, with pressure determined by gravity and pressure cuff filling around the flexible flask, with pressure sufficient to adequately visualize the cervical canal and uterine cavity(21). The image was transmitted to a TV monitor, with a 300-W xenon light source. Polypectomy was performed with grasping forceps and/or scissors, without the use of electrical current. With the grasping forceps, the polyp was grasped at its base and pushed towards the uterine fundus with repetitive movements, until its complete detachment. When using scissors, the base was sectioned and pulled with the grasping forceps until its detachment(16). Time count in the OG group began with the vaginoscopy and went until the removal of the scope, including the time of diagnostic hysteroscopy.
In the CG group, polypectomy was performed in an operating room, with the same criteria regarding number and size of polyps as the previous group. These patients had already been diagnosed with endometrial polyp in a prior diagnostic hysteroscopy. Patients of the CG group were submitted to spinal anesthesia. After asepsis, antisepsis and placement of sterile drapes, temporary urinary catheterization was performed in addition to combined vaginal digital examination, introduction of vaginal speculum, identification of the uterine cervix and traction with the Pozzi forceps. Next, cervical dilation was performed with progressive Hegar dilators, up to number 9.5. For the hysteroscopic procedure, per se, a 4.0-mm scope was used, with a 30º angle, coupled with the electrocautery resection loop and inserted into a monopolar resectoscope, comprised of an internal sheath with inflow valve and external sheath with outflow valve, with a total diameter of 9.3mm. The distension medium used was 1.5% glycine, at room temperature, with pressure and flow determined by a uterine distention device(16). Images were transferred to a TV monitor, and the light source used was 300-W xenon. Procedure time included cervical dilation with Hegar dilators until the end of the polypectomy.
Statistical analysis was made with the Epi-Info 3.3.2 statistics program. All variables were descriptively analyzed, and for quantitative variables, the minimal and maximal values were calculated, in addition to means and standard deviation. For qualitative variables, absolute and relative frequencies were calculated. For comparison of the means of both groups, Student's t test and Fisher's exact test were used, since the expected frequencies were less than 5. The significance level used for the tests was 5%.
RESULTS
Eighty-seven polypectomies were performed. Single polyps were diagnosed in 63.3% of the patients, and the mean number of polyps per patient was 1.43 in the OG group and 1.46 in the CG group. This mean was similar in both groups.
The mean size of polyps resected was 1.39cm. The polyps resected in the outpatient clinic had a mean size of 1.15cm and those resected in the operating room, 1.65cm.
As to location, most polyps were found on the posterior wall (29%), followed by the lateral right wall (20.3%). Frequency of polyp site was also similar in both groups.
Polyp exeresis was complete in all patients. Two patients (6.7%) in the CG group had complications: one case of uterine perforation and one false passage. Both occurred during mechanical cervical dilation with Hegar dilators. The procedure was interrupted, the instruments were removed from the uterus, and the vital parameters were monitored. There was no injury to viscera or hemodynamic instability. Both patients were discharged from the hospital that same day.
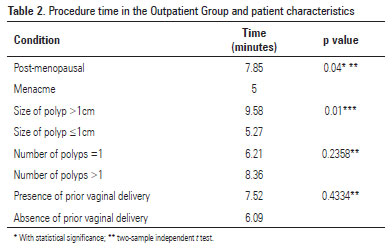
In the OG group, there were no complications. The mean time of surgery was 7 minutes (variation of 2 to 20 minutes) and in the CG group, it was 35.16 minutes (variation of 15 to 70 minutes) (p<0.0000001). However, when including the anesthesia time, the mean duration for the procedure in the CG group was 48 minutes. In the OG group, procedure time was higher in patients after menopause (p=0.04) and with polyps >1cm (p=0.01). There was no statistical difference when procedure time was compared with the number of polyps and the presence of prior vaginal delivery (Table 2). In the CG group, the reproductive phase, number and size of polyps, and the presence or absence of prior vaginal delivery had no influence in operating time (Table 3).
The mean level of pain in the OG group, referred immediately after the end of the test by means of the VRS, was 2.93 points. When the pain was stratified into mild (VRS between 0 and 4), moderate (VRS between 5 and 7) and intense (VRS between 8 and 10), it was noted that 66.6%(20)of patients reported the pain as mild, 26.6%(8)as moderate, and 6.7%(2) as intense pain (Figure 1). There was no statistical difference when the mean level of pain was compared between the patients in menacme (2.66) and after menopause (3.04; p=0.4002). Other factors that could modify the pain index, such as number and size of the polyp, and prior gestations and deliveries, showed no influence on the results. The mean level of pain referred by the patients from CG was 1.42 points, with a minimum of 0 and a maximum of 8. Of the total, 28 patients (93.3%) referred mild pain, 1 (3.3%) referred moderate pain and 1 (3.3%) referred intense pain.
DISCUSSION
Hysteroscopy is currently the gold standard test for diagnosis and treatment of intrauterine abnormalities(15,22). Over the last 10 years, technological advances have allowed simultaneous diagnosis and treatment ("see and treat") in the outpatient clinic, without the need for cervical dilation and anesthesia(22).
Evidence suggests that outpatient polypectomy has economic advantages and is preferred by women, in comparison with that performed in the operating theatre(18). Office hysteroscopies have become less painful and better tolerated by patients, which increases the acceptability of this procedure and allows the performance of therapeutic hysteroscopic procedures at an outpatient setting, reserving the conventional hysteroscopies, in an operating room, for the treatment of more complex uterine conditions(23,24).
Hysteroscopic polypectomy is a minimally invasive procedure that enables removing the lesion under direct visualization. The instruments used depend basically on the experience of the surgeon, the size and the location of the disease(25). However, this procedure displays excellent efficacy, regardless of the technique used, improving symptoms in 75 to 100% of the patients(26).
The mean time of procedure in the OG group was 7 minutes - similar to what has been found by other authors(27). This time is significantly lower than the time in the CG group, which showed a mean operating time of 35.16 minutes. Preutthipan and Herabutya described a mean operating time, with the use of the resectoscope, of 31.9 minutes(25). The greater diameter of the resectoscope imposes the need for mechanical dilation of the uterine cervix, which prolongs the operating time and increases the chances of complications. Litta et al. evaluated the limits and advantages of outpatient hysteroscopic polypectomy, using a 5.2-mm hysteroscope, without analgesia or anesthesia. The diameter of the polyps varied from 0.5 to 5cm, and the mean procedure time was 10 minutes, varying from 3 to 30 minutes. They concluded that outpatient polypectomy is viable and safe and should be performed in patients with endometrial polyps of up to 2cm in diameter, with a procedure time of less than 15 minutes, regardless of the patient's being post-menopausal or not, or of the presence of a prior vaginal delivery. Polyps >2cm had to be sliced, which increased surgical time and caused a significant increase in discomfort for the patient(27).
The majority of patients in this study (66.6%) treated in the outpatient setting referred absence of pain or mild pain. These data were similar to those found by Marsh et al., in which 65% of the women submitted to outpatient polypectomy referred the absence of pain or mild pain(18). Hysteroscopic polypectomy at outpatient clinic proved to be a safe method without complications. However, in the CG group, a complication rate of 6.7% was noted. Uterine perforation is the most common complication of hysteroscopy and it occurs most frequently during the mechanical dilation of the cervix or during insertion of the hysteroscope(28). Most of the studies describe a uterine perforation rate during hysteroscopic polypectomy of 0.8 to 1.6%(28,29). Preutthipan et al. evaluated hysteroscopic polypectomy in 240 pre- and post-menopausal women and found an 8.8% frequency of complications, with 5.8% cervical stenosis, 2.1% false passage, and 0.4% uterine perforation(25). In this same study, comparing the different instruments used during the polypectomy, the use of the resectoscope required more time to complete the procedure and greater absorption of glycine when compared to the other instruments, such as the electric probe, scissors and endoscopic forceps (p<0.05)(25).
One additional advantage of office hysteroscopic polypectomy, not evaluated in this study, would be cost reduction. A recent investigation compared the cost of three models of hysteroscopy: outpatient "see and treat" hysteroscopy, outpatient hysteroscopy followed by surgical hysteroscopy with general anesthesia, and "see and treat" hysteroscopy under general anesthesia. It was concluded that the group of outpatient "see and treat" hysteroscopy had the lowest treatment cost, regardless of the patient's age, characteristics of the childbearing phase, and indication for the procedure(30). Marsh et al.(18), in a controlled randomized study with 40 patients, compared outpatient hysteroscopic polypectomy with that performed at a day hospital, under general anesthesia, and demonstrated that the outpatient procedure can be successful, with minimal discomfort, least time away from home, and quicker return to work, and is the method preferred by women when compared to the polypectomy carried out in the day hospital.
CONCLUSION
The hysteroscopic polypectomy performed in the outpatient setting, without anesthesia, is a procedure well-tolerated by patients and displays a high level of efficacy, similar to that found in the procedure performed under anesthesia in the operating room. The procedure time was shorter and complications were fewer when carried out in the outpatient clinic.
REFERENCES
- 1. Dreisler E, Stampe Sorensen S, Ibsen PH, Lose G. Prevalence of endometrial polyps and abnormal uterine bleeding in a Danish population aged 20-74 years. Ultrasound Obstet Gynecol. 2009;33(1):102-8.
- 2. Nogueira AA. Pólipos endometriais. Rev Bras Ginecol Obstet. 2005;27(5):289-92.
- 3. Lopes RG, Baracat EC, Albuquerque Neto LC, Ramos JF, Yatabe S, Depesr DB, et al. Analysis of estrogen- and progesterone-receptor expression in endometrial polyps. J Minim Invasive Gynecol. 2007;14(3)300-3.
- 4. Hassa H, Tekin B, Senses T, Kaya M, Karatas A. Are the site, diameter, and number of endometrial polyps related with symptomatology? Am J Obstet Gynecol. 2006;194(3):718-21.
- 5. Savelli L, De Iaco P, Santini D, Rosati F, Ghi, T, Pignotti E, et al. Histopathologic features and risk factors for benignity, hyperplasia, and cancer in endometrial polyps. Am J Obstet Gynecol. 2003;188(4):927-31.
- 6. Almeida EC, Nogueira AA, Reis FJ, Ramalho LN, Zucoloto S. Immunohistochemical expression of estrogen and progesterone receptors in endometrial polyps and adjacent endometrium in postmenopausal women. Maturitas. 2004;49(3):229-33.
- 7. Bakour SH, Khan KS, Gupta JK. The risk of premalignant and malignant pathology in endometrial polyps. Acta Obstet Gynecol Scand. 2000;79(4):317-20.
- 8. Wang JH, Zhao J, Lin J. Opportunities and risk factors for premalignant and malignant transformation of endometrial polyps: management strategies. J Minim Invasive Gynecol. 2010;17(1):53-8.
- 9. Baiocchi G, Manci N, Pazzaglia M, Giannone L, Burnelli L, Giannone E, et al. Malignancy in endometrial polyps: a 12-year experience. Am J Obstet Gynecol. 2009;201(5):462.e1-4.
- 10. Garuti G, Sambruni I, Colonnelli M, Luerti M. Accuracy of hysteroscopy in predicting histopathology of endometrium in 1500 women. J Am Assoc Gynecol Laparosc. 2001;8(2):207-13.
- 11. Torrejon R, Fernandez-Alba JJ, Carnicer I, Martin A, Castro C, Garcia-Cabanillas J, et al. The value of hysteroscopic exploration for abnormal uterine bleeding. J Am Assoc Gynecol Laparosc. 1997;4(4):453-6.
- 12. Ben-Arie A, Goldchmit C, Laviv Y, Levy R, Caspi B, Huszar M, et al. The malignant potential of endometrial polyps. Eur J Obstet Gynecol Reprod Biol. 2004;115(2):206-10.
- 13. Lieng M, Qvigstad E, Sandvik L, Jorgensen H, Langebrekke A, Istre O. Hysteroscopic resection of symptomatic and asymptomatic endometrial polyps. J Minim Invasive Gynecol. 2007;14(2):189-94.
- 14. Kremer C, Duffy S, Moroney M. Patient satisfaction with outpatient hysteroscopy versus day case hysteroscopy: randomized controlled trial. BMJ. 2000;320(7230):279-82.
- 15. Di Spiezio Sardo A, Taylor A, Tsirkas P, Mastrogamvrakis G, Sharma M, Magos A. Hysteroscopy: a technique for all? Analysis of 5,000 outpatient hysteroscopies. Fertil Steril. 2008;89(2):438-43.
- 16. Bettocchi S, Nappi L, Cecci O, Selvaggi L. What does 'diagnostic hysteroscopy' mean today? The role of the new techniques. Curr Opin Obstet Gynecol. 2003;15(4):303-8.
- 17. Bettocchi S, Ceci O, Napp L, Di Venere R, Masciopinto V, Pansini V, et al. Operative office hysteroscopy without anesthesia: analysis of 4863 cases performed with mechanical instruments. J Am Assoc Gynecol Laparosc. 2004;11(1):59-61.
- 18. Marsh FA, Rogerson LJ, Duffy SR. A randomized controlled trial comparing outpatient versus daycase endometrial polypectomy. BJOG. 2006; 113(8):896-901.
- 19. Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10(4):390-2.
- 20. Salo D, Eget D, Lavery RF, Garner L, Bernstein S, Tandon K. Can patients accurately read a visual analog pain scale? Am J Emerg Med. 2003;21(7):515-9.
- 21. Bettocchi S, Selvaggi L. A vaginoscopy approach to reduce the pain of office hysteroscopy. J Am Assoc Gynecol Laparosc. 1997;4(2):255-8.
- 22. Serden SP. Diagnostic hysteroscopy to evaluate the cause of abnormal uterine bleeding. Obstet Gynecol Clin North Am. 2000;27(2):277-86.
- 23. Cicinelli E, Parisi C, Galantino P, Pinto V, Barba B, Schonauer S. Reliability, feasibility, and safety of minihysteroscopy with a vaginoscopic approach: experience with 6,000 cases. Fertil Steril. 2003;80(1):199-202.
- 24. De Angelis C, Santoro G, Re ME, Nofroni I. Office hysteroscopy and compliance: mini-hysteroscopy versus traditional hysteroscopy in a randomized trial. Hum Reprod. 2003;18(11):2441-5.
- 25. Preutthipan S, Herabutya Y. Hysterocopic polypectomy in 240 premenopausal and postmenopausal women. Fertil Steril. 2005;83(3):705-9.
- 26. Nathani F, Clark TJ. Uterine polypectomy in the management of abnormal uterine bleeding: A systematic review. J Minim Invasive Gynecol. 2006;13(4):260-8.
- 27. Litta P, Cosmi E, Saccardi C, Esposito C, Rui R, Ambrosini G. Outpatient operative polypectomy using a 5 mm-hysteroscope without anaesthesia and/or analgesia: advantages and limits. Eur J Obstet Gynecol Reprod Biol. 2008;139(2):210-4.
- 28. Shveiky D, Rojansky N, Revel A, Benshushan A, Laufer N, Shushan A. Complications of hysteroscopic surgery: "Beyond the learning curve". J Minim Invasive Gynecol. 2007;14(2):218-22.
- 29. Umranikar S, Umranikar A, Cheong Y. Hysteroscopy and hysteroscopic surgery. Obstet Gynaecol Reprod Med. 2010;20(6):167-73.
- 30. Saridogan E, Tilden D, Sykes D, Davis N, Subramanian D. Cost-analysis comparision of outpatient see-and-treat hysteroscopy service with other hysteroscopy service models. J Minim Invasive Gynecol. 2010;17(4):518-25.
Hysteroscopic endometrial polypectomy: outpatient versus conventional treatment
Publication Dates
-
Publication in this collection
29 Oct 2012 -
Date of issue
Sept 2012
History
-
Received
14 July 2011 -
Accepted
24 Jan 2012