ABSTRACT
Objective
To evaluate the cost-effectiveness of clinical education models for undergraduate nursing programs.
Methods
A model-based cost-effectiveness analysis. Settings were universities with undergraduate nursing courses. Participants consisted of the decision tree that guided the structure of the model, filled in with effectiveness results from a hypothetical cohort of undergraduate nursing students. Interventions were Clinical Preceptor or Clinical Facilitator or Clinical Education Unit. Main outcome measure was effectiveness, defined as improvement of clinical education. The projected economic outcomes included incremental costs, incremental effectiveness, and incremental cost-effectiveness ratio. Monte Carlo probabilistic sensitivity analysis was employed to assess uncertainty in the model and robustness of our results.
Results
The model based on Clinical Education Unit could be defined as the best, followed by Clinical Facilitator and Clinical Preceptor. The incremental cost of telephone-support intervention was US$ 59,604.40 higher than the second-best performing intervention (Clinical Facilitator), and US$ 32,661.86 higher than the last best performing intervention (Clinical Preceptor). In addition, Clinical Education Unit model showed 7% and 19% more effectiveness than Clinical Facilitator and Clinical Preceptor, respectively.
Conclusion
Clinical Education Unit represents the best choice to promote better development of skills, knowledge and socialization in undergraduate nursing programs considering its effectiveness and costs.
Costs and cost analysis; Economics; Nursing education research; Education
RESUMO
Objetivo
Avaliar a relação de custo-efetividade dos modelos de educação clínica para cursos de graduação em enfermagem.
Métodos
Análise de custo-efetividade baseada em modelo. Os ambientes foram universidades com cursos de graduação em enfermagem. Os participantes consistiram na árvore de decisão, que norteou a estrutura do modelo, preenchida com resultados de efetividade de uma coorte hipotética de estudantes de graduação em enfermagem. As intervenções foram o Preceptor Clínico ou o Facilitador Clínico ou a Unidade de Educação Clínica. A principal medida de resultado foi a efetividade, definida como a melhoria da educação clínica. Os resultados econômicos projetados incluíram custos incrementais, efetividade incremental e custo incremental por efetividade. A análise probabilística de sensibilidade de Monte Carlo foi utilizada para avaliar a incerteza no modelo e a robustez de nossos resultados.
Resultados
O modelo baseado na Unidade de Educação Clínica foi o melhor, seguido pelo Facilitador Clínico e pelo Preceptor Clínico. O custo incremental da intervenção com suporte por telefone foi US$ 59,604.40 a mais do que o da segunda intervenção de melhor desempenho (Facilitador Clínico) e US$ 32,661.86 a mais do que a última intervenção de melhor desempenho (clínico preceptor). Além disso, o modelo da Unidade de Educação Clínica mostrou 7% e 19% mais efetividade do que Facilitador Clínico e Preceptor Clínico, respectivamente.
Conclusão
A Unidade de Educação Clínica representa a melhor escolha para promover um desenvolvimento de habilidades otimizado, conhecimentos e socialização nos cursos de graduação em enfermagem, considerando efetividade e custos.
Custos e análise de custo; Economia; Pesquisa em educação de enfermagem; Educação
INTRODUCTION
Health care services and education organizations have currently sought alternatives to optimize learning of students.(11. Jayasekara R, Smith C, Hall C, Rankin E, Smith M, Visvanathan V, et al. The effectiveness of clinical education models for undergraduate nursing programs: a systematic review. Nurse Educ Pract. 2018;29:116-26. Review.) In the nursing context, the traditional model of clinical instruction predominates and, in many cases, has remained unchanged for decades.(22. Fischer SA. Transformational leadership in nursing education: making the case. Nurs Sci Q. 2017;30(2):124-8.
3. Ralph N, Birks M, Chapman Y. The accreditation of nursing education in Australia. Collegian. 2015;22(1):3-7.
4. Miller TW. The dedicated education unit: a practice and education partnership. Nurs Leadersh Forum. 2005;9(4):169-73.-55. Hall KC, Diffenderfer SK, Stidham A, Mullins CM. Student and preceptor advancement in a dedicated education site: innovation in clinical education for advanced practice nurses. Nurs Educ Perspect. 2019;40(1):60-1.) Although this model had been enough for decades, recent trends in education, health systems, and care of patients require that nursing education programs investigate innovative clinical teaching models to ensure optimal student preparation for practice.(66. Springer PJ, Johnson P, Lind B, Walker E, Clavelle J, Jensen N. The Idaho dedicated education unit model: cost-effective, high-quality education. Nurse Educ. 2012;37(6):262-7.
7. Randon G, Bortolami E, Grosso S. [Back to units for nursing students’ education? The Dedicated Education Units (DEU)]. Assist Inferm Ric. 2017; 36(1):24-30. Review. Italian.-88. Kim J, Park JH, Shin S. Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Med Educ. 2016;16:152.)
In this context, there is evidence that the clinical education model promotes a better development of skills, knowledge and socialization.(99. Mulready-Shick J, Flanagan KM, Banister GE, Mylott L, Curtin LJ. Evaluating dedicated education units for clinical education quality. J Nurs Educ. 2013; 52(11):606-14.) Clinical education models were developed to improve clinical learning of future nurses, resulting in better quality of care provided to patients.(11. Jayasekara R, Smith C, Hall C, Rankin E, Smith M, Visvanathan V, et al. The effectiveness of clinical education models for undergraduate nursing programs: a systematic review. Nurse Educ Pract. 2018;29:116-26. Review.) The clinical education model is based on patient’s total care experiences, permeating a project of learning activities and adequate skills at undergraduate level.(33. Ralph N, Birks M, Chapman Y. The accreditation of nursing education in Australia. Collegian. 2015;22(1):3-7.,44. Miller TW. The dedicated education unit: a practice and education partnership. Nurs Leadersh Forum. 2005;9(4):169-73.,1010. Auxier N, Simpson H. Transforming the role of the clinical faculty coordinator in the dedicated education unit. Nurs Educ Perspect. 2018;39(6):383-4.
11. Grealish L, van de Mortel T, Brown C, Frommolt V, Grafton E, Havell M, et al. Redesigning clinical education for nursing students and newly qualified nurses: a quality improvement study. Nurse Educ Pract. 2018;33:84-9.-1212. Pappas S. Improving patient safety and nurse engagement with a dedicated education unit. Nurse Lead. 2007;5(3):40-3.)
Although there is evidence evaluating various clinical education models for nursing undergraduate students, no attention has been given to the cost-effectiveness ratio of these models. Thus, there is a clear need for a complete cost-effectiveness assessment to examine the effectiveness of different models of clinical education, considering their costs and providing the best evidence available, so that managers of education organizations can choose the model that best fits in their financial scope.
OBJECTIVE
To evaluate the cost-effectiveness of clinical education models for undergraduate nursing programs.
METHODS
Study design and patients
This study is a cost-effectiveness analysis comparing models to improve clinical education in undergraduate nursing programs, conducted at University of South Australia, Australia, in December 2018. It was carried out according to the recommendations of the Second Panel on Cost-Effectiveness in Health and Medicine.(1313. Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, Augustovski F, Briggs AH, Mauskopf J, Loder E; ISPOR Health Economic Evaluation Publication F, Guidelines – CHEERS Good Reporting Practices Task Force. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)-explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Heal. 2013;16(2):231-50.) The analysis was also performed from the perspective of the Australian Education System (payer perspective). The result of this analysis was expressed as a ratio of incremental costs and incremental health intervention outcomes. The incremental cost-effectiveness ratios (ICER) were calculated in American dollars, in 2018.
Interventions and model structure
The models of clinical education in undergraduate nursing programs define the model structure. They are Clinical Preceptor, Clinical Facilitator, and Clinical Education Unit (CEU).(11. Jayasekara R, Smith C, Hall C, Rankin E, Smith M, Visvanathan V, et al. The effectiveness of clinical education models for undergraduate nursing programs: a systematic review. Nurse Educ Pract. 2018;29:116-26. Review.)
Clinical Preceptor involves assignment of students to practice, for a defined period, with experienced clinicians employed in the clinical facility. In the Clinical Facilitator model, healthcare workers (Clinical Facilitator) are employed by the education organizations to oversee aspects of the clinical placement for undergraduate nursing students across different clinical venues, including offering direct supervision and evaluation. Clinical Facilitators are experienced clinicians, mostly seconded from the hospital to the university. The CEU or Dedicated Education Unit (DEU) is a health care unit, developed by lecturers and clinicians, dedicated to the clinical education of nursing students. In Australia, a university collaborated with healthcare units to design a DEU that provides clinical placements of undergraduate nursing students during any year of the program.
Model inputs
We derived model inputs from one systematic review(11. Jayasekara R, Smith C, Hall C, Rankin E, Smith M, Visvanathan V, et al. The effectiveness of clinical education models for undergraduate nursing programs: a systematic review. Nurse Educ Pract. 2018;29:116-26. Review.) that evaluated the effectiveness of clinical education models for undergraduate nursing programs and additional literature searches.
Costs were simulated based on the hour value of the professionals involved during the whole course of the nursing students. The values are measured by the student training cycle (considering the beginning and end of the undergraduate program). The cost was obtained from an estimate of the syllabus of the School of Nursing and Midwifery (University of South Australia).
Cost and effectiveness outcomes were discounted by 5%. Discounting was used in sensitivity analyses assessing differential effectiveness between strategies. All data of model inputs are present in table 1.
Cost-effectiveness analysis
Effectiveness was defined as advance of clinical education by improving clinical decision-making and critical thinking skills.(11. Jayasekara R, Smith C, Hall C, Rankin E, Smith M, Visvanathan V, et al. The effectiveness of clinical education models for undergraduate nursing programs: a systematic review. Nurse Educ Pract. 2018;29:116-26. Review.) The three clinical education models for undergraduate nursing programs included in this analysis conferred statistically significantly improved clinical education, as compared to the Clinical Preceptor. The Clinical Preceptor was used for reference.
The projected economic outcomes included incremental costs, incremental effectiveness, and incremental cost-effectiveness ratio. We did not use a cost-effectiveness threshold. Results of cost-effectives analysis will be classified as possibly cost-effective (intervention more effective and less costly than the next least costly intervention), weakly dominated (intervention less effective, but has a smaller cost than the next highest ranked intervention), and dominated (intervention less effective and with a higher cost than the next least costly scenario).(1414. Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for Economic Evaluation of Health Care Programmes. 4th ed. USA: Oxford University Press; 2015.)
Sensitivity analysis
Monte Carlo probabilistic sensitivity analysis was employed to assess uncertainty of the model and robustness of our results. We ran our model 100,000 times to estimate the mean costs and effectiveness, and used an informal method to produce equal distributions in a formal Bayesian analysis with uninformative priors.(1515. Marill KA, Chang Y, Wong KF, Friedman AB. Estimating negative likelihood ratio confidence when test sensitivity is 100%: a bootstrapping approach. Stat Methods Med Res. 2017;26(4):1936-48.)
RESULTS
Our base-case results are presented in figure 1. They show that across all interventions to improve clinical education in undergraduate nursing students, we have three possibly cost-effective interventions. The model based in CEU could be defined as the best, followed by Clinical Facilitator and Cinical Preceptor. Telephone-support intervention incremental cost was US$ 59,604.40 higher than the second-best performing intervention (Clinical Facilitator), and US$ 32,661.86 than the last best performing intervention (Clinical Preceptor). In addition, CEU model shows 7% and 19% more effectiveness than Clinical Facilitator and Clinical Preceptor, respectively.
The ICER of Clinical Facilitator compared to Clinical Preceptor was US$ 278,271.66, and the ICER of CEU comparing to Clinical Preceptor was US$ 909,825.50 per percent increase in clinical education (Table 2).
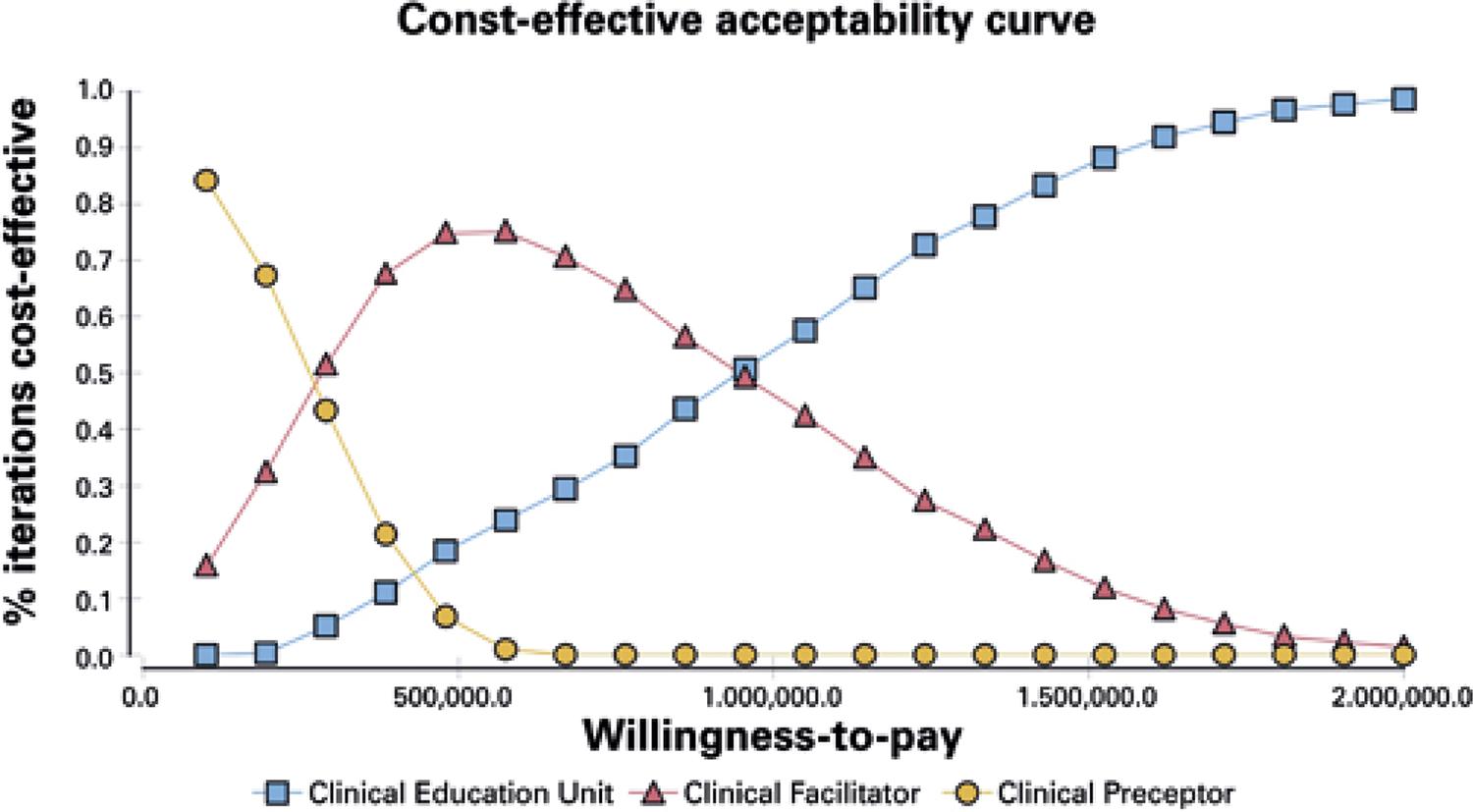
The probabilistic sensitivity analysis verified that our base-case cost-effectiveness analysis was robust. The probabilistic sensitivity analysis showed, in the most hypothetical scenarios, the intervention based in CEU is the best choice, considering a willingness-to-pay of 1,000,000 (Figure 2).
DISCUSSION
This model suggested that CEU represents an additional effectiveness and cost to education models for undergraduate nursing programs, when compared to Clinical Facilitator or Clinical Preceptor.(66. Springer PJ, Johnson P, Lind B, Walker E, Clavelle J, Jensen N. The Idaho dedicated education unit model: cost-effective, high-quality education. Nurse Educ. 2012;37(6):262-7.)
The CEU promotes learning and allows time and space for reflection, besides developing a professional group identity, and learning to recognize and implement the responsibilities related to the nurse professional role.(77. Randon G, Bortolami E, Grosso S. [Back to units for nursing students’ education? The Dedicated Education Units (DEU)]. Assist Inferm Ric. 2017; 36(1):24-30. Review. Italian.) An educational model focused on education organizations, as herein considered, is likely to reduce duplication of costs and results in savings, when considering the different undergraduate courses using CEU. However, the model assumed that the costs were unique to the undergraduate nursing course, regardless of the number of students. In the future, models involving the maintenance of different undergraduate courses can be developed.
The cost to implement and maintain CEU was significantly higher than the tradition model (Clinical Preceptor).(44. Miller TW. The dedicated education unit: a practice and education partnership. Nurs Leadersh Forum. 2005;9(4):169-73.,1212. Pappas S. Improving patient safety and nurse engagement with a dedicated education unit. Nurse Lead. 2007;5(3):40-3.,1616. Moscato SR, Miller J, Logsdon K, Weinberg S, Chorpenning L. Dedicated education unit: an innovative clinical partner education model. Nurs Outlook. 2007;55(1):31-7.) However, no study was able to determine the effectiveness and long-term cost when these undergraduate students would be working as nurses. We know that as an educational administrator, it is very attractive to have a model that allows training more students with similar results and at a lower financial cost. However, the current focus should be on the quality that these professionals can provide while they are working. The costs of complications arising from inadequate health care can be much higher than the investment in setting up and maintaining a CEU.
Educational factors have limited the number of undergraduate nursing students in advanced practice and consequent delay in training human resources.(55. Hall KC, Diffenderfer SK, Stidham A, Mullins CM. Student and preceptor advancement in a dedicated education site: innovation in clinical education for advanced practice nurses. Nurs Educ Perspect. 2019;40(1):60-1.,1010. Auxier N, Simpson H. Transforming the role of the clinical faculty coordinator in the dedicated education unit. Nurs Educ Perspect. 2018;39(6):383-4.,1111. Grealish L, van de Mortel T, Brown C, Frommolt V, Grafton E, Havell M, et al. Redesigning clinical education for nursing students and newly qualified nurses: a quality improvement study. Nurse Educ Pract. 2018;33:84-9.) Aiming to assist in the shortage of nurses, health services are challenged to release part of the nursing team to become supervisors in clinical supervision models, and require a significant investment in nurses’ education to achieve adequate teaching effectiveness.(55. Hall KC, Diffenderfer SK, Stidham A, Mullins CM. Student and preceptor advancement in a dedicated education site: innovation in clinical education for advanced practice nurses. Nurs Educ Perspect. 2019;40(1):60-1.,1010. Auxier N, Simpson H. Transforming the role of the clinical faculty coordinator in the dedicated education unit. Nurs Educ Perspect. 2018;39(6):383-4.,1111. Grealish L, van de Mortel T, Brown C, Frommolt V, Grafton E, Havell M, et al. Redesigning clinical education for nursing students and newly qualified nurses: a quality improvement study. Nurse Educ Pract. 2018;33:84-9.) In this way, CEU provides a simulation, and the academic-practice partnership model can offer innovative approaches to clinical training, aiming to produce graduates who can provide safe and quality care services within the complex environment based on system practice of health.(11. Jayasekara R, Smith C, Hall C, Rankin E, Smith M, Visvanathan V, et al. The effectiveness of clinical education models for undergraduate nursing programs: a systematic review. Nurse Educ Pract. 2018;29:116-26. Review.,55. Hall KC, Diffenderfer SK, Stidham A, Mullins CM. Student and preceptor advancement in a dedicated education site: innovation in clinical education for advanced practice nurses. Nurs Educ Perspect. 2019;40(1):60-1.,1010. Auxier N, Simpson H. Transforming the role of the clinical faculty coordinator in the dedicated education unit. Nurs Educ Perspect. 2018;39(6):383-4.,1111. Grealish L, van de Mortel T, Brown C, Frommolt V, Grafton E, Havell M, et al. Redesigning clinical education for nursing students and newly qualified nurses: a quality improvement study. Nurse Educ Pract. 2018;33:84-9.)
This study has some limitations. However, we should emphasize that the long-term advantages of CEU can be even greater, since professionals that are more qualified improve patients’ clinical outcomes, reduce costs and have better productivity.
CONCLUSION
This analysis demonstrated that Clinical Preceptor, Clinical Facilitator and Clinical Education Unit are cost-effective models for clinical education of undergraduate nursing students. However, the probabilistic sensitivity analysis showed that, in the most hypothetical scenarios, the intervention based on Clinical Education Unit is the best choice. This suggests that Clinical Education Unit represents the best choice to promote better development of skills, knowledge and socialization for undergraduate nursing programs, considering effectiveness and costs. Nursing programs should encourage the implementation of Clinical Education Unit, so that the training of professionals will be more appropriate to the real needs of patients.
REFERENCES
-
1Jayasekara R, Smith C, Hall C, Rankin E, Smith M, Visvanathan V, et al. The effectiveness of clinical education models for undergraduate nursing programs: a systematic review. Nurse Educ Pract. 2018;29:116-26. Review.
-
2Fischer SA. Transformational leadership in nursing education: making the case. Nurs Sci Q. 2017;30(2):124-8.
-
3Ralph N, Birks M, Chapman Y. The accreditation of nursing education in Australia. Collegian. 2015;22(1):3-7.
-
4Miller TW. The dedicated education unit: a practice and education partnership. Nurs Leadersh Forum. 2005;9(4):169-73.
-
5Hall KC, Diffenderfer SK, Stidham A, Mullins CM. Student and preceptor advancement in a dedicated education site: innovation in clinical education for advanced practice nurses. Nurs Educ Perspect. 2019;40(1):60-1.
-
6Springer PJ, Johnson P, Lind B, Walker E, Clavelle J, Jensen N. The Idaho dedicated education unit model: cost-effective, high-quality education. Nurse Educ. 2012;37(6):262-7.
-
7Randon G, Bortolami E, Grosso S. [Back to units for nursing students’ education? The Dedicated Education Units (DEU)]. Assist Inferm Ric. 2017; 36(1):24-30. Review. Italian.
-
8Kim J, Park JH, Shin S. Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Med Educ. 2016;16:152.
-
9Mulready-Shick J, Flanagan KM, Banister GE, Mylott L, Curtin LJ. Evaluating dedicated education units for clinical education quality. J Nurs Educ. 2013; 52(11):606-14.
-
10Auxier N, Simpson H. Transforming the role of the clinical faculty coordinator in the dedicated education unit. Nurs Educ Perspect. 2018;39(6):383-4.
-
11Grealish L, van de Mortel T, Brown C, Frommolt V, Grafton E, Havell M, et al. Redesigning clinical education for nursing students and newly qualified nurses: a quality improvement study. Nurse Educ Pract. 2018;33:84-9.
-
12Pappas S. Improving patient safety and nurse engagement with a dedicated education unit. Nurse Lead. 2007;5(3):40-3.
-
13Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, Augustovski F, Briggs AH, Mauskopf J, Loder E; ISPOR Health Economic Evaluation Publication F, Guidelines – CHEERS Good Reporting Practices Task Force. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)-explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Heal. 2013;16(2):231-50.
-
14Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for Economic Evaluation of Health Care Programmes. 4th ed. USA: Oxford University Press; 2015.
-
15Marill KA, Chang Y, Wong KF, Friedman AB. Estimating negative likelihood ratio confidence when test sensitivity is 100%: a bootstrapping approach. Stat Methods Med Res. 2017;26(4):1936-48.
-
16Moscato SR, Miller J, Logsdon K, Weinberg S, Chorpenning L. Dedicated education unit: an innovative clinical partner education model. Nurs Outlook. 2007;55(1):31-7.
Publication Dates
-
Publication in this collection
22 June 2020 -
Date of issue
2020
History
-
Received
13 Aug 2019 -
Accepted
29 Nov 2019