ABSTRACT
Objective:
To evaluate and compare subjective sleep quality in medical students across the various phases of the medical course.
Methods:
This was a cross-sectional study involving medical undergraduates at one medical school in the city of Botucatu, Brazil. All first- to sixth-year students were invited to complete the Pittsburgh Sleep Quality Index, which has been validated for use in Brazil. Participants were divided into three groups according to the phase of the medical course: group A (first- and second-years); group B (third- and fourth-years); and group C (fifth- and sixth-years). The results obtained for the instrument components were analyzed for the total sample and for the groups.
Results:
Of the 540 students invited to participate, 372 completed the instrument fully. Of those, 147 (39.5%) reported their sleep quality to be either very or fairly bad; 110 (29.5%) reported taking more than 30 min to fall asleep; 253 (68.0%) reported sleeping 6-7 h per night; 327 (87.9%) reported adequate sleep efficiency; 315 (84.6%) reported no sleep disturbances; 32 (8.6%) reported using sleeping medication; and 137 (36.9%) reported difficulty staying awake during the day at least once a week. Group comparison revealed that students in group A had worse subjective sleep quality and greater daytime dysfunction than did those in groups B and C.
Conclusions:
Medical students seem to be more exposed to sleep disturbance than other university students, and first- and second-years are more affected than those in other class years because they have worse subjective sleep quality. Active interventions should be implemented to improve sleep hygiene in medical students.
Keywords:
Students, medical; Quality of life; Sleep
RESUMO
Objetivo:
Avaliar a percepção subjetiva de qualidade de sono em estudantes de medicina, comparando as diferentes fases do curso.
Métodos:
Estudo transversal envolvendo todos os estudantes entre o 1º e o 6º ano da graduação em medicina em uma universidade na cidade de Botucatu (SP), que foram convidados a responder o Índice de Qualidade do Sono de Pittsburgh, validado para uso no Brasil. Os resultados dos componentes do índice foram avaliados na amostra global e em três grupos de acordo com o ciclo do curso: básico (1º e 2º anos), de fisiopatologia (3º e 4º anos) e de internato clínico (5º e 6º anos).
Resultados:
Dos 540 estudantes convidados, 372 responderam o instrumento adequadamente. Desses, 147 (39,5%) relataram ter uma qualidade de sono ruim ou muito ruim, 110 (29,5%) demoram mais de 30 min para conseguir dormir, 253 (68,0%) dormem de 6-7 h por noite, 327 (87,9%) relataram ter eficiência do sono adequada, 315 (84,6%) não indicavam ter distúrbios do sono, 32 (8,6%) relataram fazer uso de medicamentos para dormir, e 137 (36,9%) apresentavam dificuldades em se manter acordados durante o dia ao menos uma vez por semana. Na comparação entre os grupos, os alunos do ciclo básico apresentaram uma pior percepção da qualidade subjetiva do sono e de disfunção diurna que os outros alunos.
Conclusões:
Estudantes de medicina parecem estar mais expostos a distúrbios de sono, sendo aqueles nos anos iniciais mais afetados por apresentar uma percepção pior de sono. Intervenções ativas devem ser implantadas para melhorar a higiene do sono desses alunos.
Descritores:
Estudantes de medicina; Qualidade de vida; Sono
INTRODUCTION
Sleep quality has been studied among university students.11 Benavente SB, Silva RM, Higashi AB, Guido Lde A, Costa AL. Influence of stress factors and socio-demographic characteristics on the sleep quality of nursing students [Article in Portuguese]. Rev Esc Enferm USP. 2014;48 (3):514-20. https://doi.org/10.1590/S0080-623420140000300018
https://doi.org/10.1590/S0080-6234201400...
2 Mesquita G, Reimão R. Quality of sleep among university students: effects of nighttime computer and television use. Arq Neuropsiquiatr. 2010;68(5):720-5. https://doi.org/10.1590/S0004-282X2010000500009
https://doi.org/10.1590/S0004-282X201000...
3 Araújo MF, Feritas RW, Lima AC, Pereira DC, Zanetti ML, Damasceno MM. Health indicators associated with poor sleep quality among university students [Article in Portuguese]. Rev Esc Enferm USP. 2014;48(6):1085-92. https://doi.org/10.1590/S0080-623420140000700017
https://doi.org/10.1590/S0080-6234201400...
-44 Lemma S, Berhane Y, Worku A, Gelaye B, Williams MA. Good quality sleep is associated with better academic performance among university students in Ethiopia. Sleep Breath. 2014;18(2):257-63. https://doi.org/10.1007/s11325-013-0874-8
https://doi.org/10.1007/s11325-013-0874-...
Such studies have shown impairments in sleep quality, which are even greater when it comes to medical undergraduates,55 Preišegolavičiūtė E, Leskauskas D, Adomaitiene V. Associations of quality of sleep with lifestyle factors and profile of studies among Lithuanian students. Medicina (Kaunas). 2010;46(7):482-9. who have a heavy academic schedule and responsibilities in various activities, all of which significantly impact sleep quality.66 Pagnin D, de Queiroz V, Carvalho YT, Dutra AS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Acad Psychiatry. 2014;38(4):438-44. https://doi.org/10.1007/s40596-014-0093-z
https://doi.org/10.1007/s40596-014-0093-...
7 Ribeiro CR, Oliveira SM, Silva YM. The impact of sleep quality in medical education [Article in Portuguese]. Rev Soc Bras Clin Med. 2014;12(1):8-14.
8 Del Pielago Meoño AF, Failoc Rojas VE, Plasencia Dueñas EA, Díaz Vélez C Calidad de sueño y estilo de aprendizaje en estudiantes de Medicina Humana de la Universidad Nacional Pedro Ruiz Gallo. Act Méd Per. 2013;30(4):63-8.-99 Cardoso HC, Bueno FC, Mata JC, Alves AP, Jochims I, Vaz Filho IH, et al. Assessing quality of sleep in medical students [Article in Portuguese]. Rev Bras Educ Med. 2009;33(3):349-55. https://doi.org/10.1590/S0100-55022009000300005
https://doi.org/10.1590/S0100-5502200900...
University students experience disturbances in their circadian cycle because of the stress of the academic environment,11 Benavente SB, Silva RM, Higashi AB, Guido Lde A, Costa AL. Influence of stress factors and socio-demographic characteristics on the sleep quality of nursing students [Article in Portuguese]. Rev Esc Enferm USP. 2014;48 (3):514-20. https://doi.org/10.1590/S0080-623420140000300018
https://doi.org/10.1590/S0080-6234201400...
which is increased by habits such as surfing the Internet, watching television,22 Mesquita G, Reimão R. Quality of sleep among university students: effects of nighttime computer and television use. Arq Neuropsiquiatr. 2010;68(5):720-5. https://doi.org/10.1590/S0004-282X2010000500009
https://doi.org/10.1590/S0004-282X201000...
and using alcohol and tobacco,33 Araújo MF, Feritas RW, Lima AC, Pereira DC, Zanetti ML, Damasceno MM. Health indicators associated with poor sleep quality among university students [Article in Portuguese]. Rev Esc Enferm USP. 2014;48(6):1085-92. https://doi.org/10.1590/S0080-623420140000700017
https://doi.org/10.1590/S0080-6234201400...
habits that are common in this population. Improved sleep quality is associated with engaging in sports and extracurricular activities.88 Del Pielago Meoño AF, Failoc Rojas VE, Plasencia Dueñas EA, Díaz Vélez C Calidad de sueño y estilo de aprendizaje en estudiantes de Medicina Humana de la Universidad Nacional Pedro Ruiz Gallo. Act Méd Per. 2013;30(4):63-8.
Since impairment in sleep quality directly affects academic performance44 Lemma S, Berhane Y, Worku A, Gelaye B, Williams MA. Good quality sleep is associated with better academic performance among university students in Ethiopia. Sleep Breath. 2014;18(2):257-63. https://doi.org/10.1007/s11325-013-0874-8
https://doi.org/10.1007/s11325-013-0874-...
and also emotional aspects,66 Pagnin D, de Queiroz V, Carvalho YT, Dutra AS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Acad Psychiatry. 2014;38(4):438-44. https://doi.org/10.1007/s40596-014-0093-z
https://doi.org/10.1007/s40596-014-0093-...
we emphasize the importance of measuring sleep quality in medical students and monitoring it across the various phases of the medical course. To that end, there are instruments for self-assessment of sleep quality in the literature, such as the Pittsburgh Sleep Quality Index (PSQI),1010 Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. https://doi.org/10.1016/0165-1781(89)90047-4
https://doi.org/10.1016/0165-1781(89)900...
which has been validated for use in Brazil1111 Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, Miozzo IC, de Barba ME, et al. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med. 2011;12(1):70-5. https://doi.org/10.1016/j.sleep.2010.04.020
https://doi.org/10.1016/j.sleep.2010.04....
and which, because of its high efficacy (high specificity and high sensitivity), is recommended for use in clinical practice and research. The PSQI contains 19 items, which address sleep latency, usual bedtime and wake time, and sleep and nap quality.1010 Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. https://doi.org/10.1016/0165-1781(89)90047-4
https://doi.org/10.1016/0165-1781(89)900...
Therefore, the objective of the present study was to evaluate and compare subjective sleep quality in medical students across the various phases of the medical course, by using the PSQI.
METHODS
This was a cross-sectional study involving medical undergraduates at the Botucatu School of Medicine, located in the city of Botucatu, Brazil. All first- to sixth-year students (N = 540) were invited to participate. Data were collected over two months. The study was approved by the local human research ethics committee (Protocol no. 400/08). All participants gave written informed consent.
All students who completed the PSQI fully within the specified period were included in the study. The students who declined the invitation to participate in the study or who did not complete the entire questionnaire were excluded.
The research instrument selected was the PSQI1111 Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, Miozzo IC, de Barba ME, et al. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med. 2011;12(1):70-5. https://doi.org/10.1016/j.sleep.2010.04.020
https://doi.org/10.1016/j.sleep.2010.04....
because this is an analysis instrument that is used worldwide and is validated for assessing sleep disturbances, as well as allowing assessment of questions in isolation or the overall result. Its seven components-subjective sleep quality; sleep latency; sleep duration; habitual sleep efficiency; sleep disturbances; use of sleeping medication; and daytime dysfunction-were analyzed separately. The range of this instrument is from 0 to 21 points, and scores ≥ 5 signify poor sleep quality, indicating possible sleep disturbance. The sum of the seven component scores produces a global score.
Statistical analysis
The data from the completed questionnaires were entered into tables using Microsoft Excel, one of which showing the results for the total sample and the others showing the results for each undergraduate class year. The class years were then grouped according to the traditional phases of the medical course (initial phase, pathophysiology phase, and clinical clerkship phase) and participants were divided into three groups: group A, with first- and second-year students; group B, with third- and fourth-year students; and group C, with fifth- and sixth-year students. The results were described for the total sample and for the groups, and among- and between-group comparisons were conducted.
Analysis was performed using the proportions of different responses as a function of each component. In the inductive analysis, the chi-square test was used for among-group comparisons of the seven components of the PSQI, whereas the Wilcoxon test was used for between-group comparisons of the components and the Student’s t-test was used for between-group comparisons of the global score. Values of p < 0.05 were considered significant.
RESULTS
Of the total of 540 students who were invited to participate in the study, 372 (68.9%) completed the PSQI, being distributed by class year as follows: 72, first-years; 53, second-years; 86, third-years; 67, fourth-years; 30, fifth-years; and 64, sixth-years. As for gender distribution, there was a larger proportion of females (Table 1).
The results for the seven components of the PSQI were analyzed for the total sample and for the three study groups (Table 2). Of the total sample, 39.5% of the participants classified their sleep quality as either very or fairly bad, and 29.5% reported taking more than 30 min to fall asleep two or more times a week. The average number of hours slept per night ranged from 6 h and 14 min among fifth-years to 6h and 34 min among second-years. Inductive statistical results showed no significant differences among the three groups regarding subjective sleep quality, sleep latency, or sleep duration.
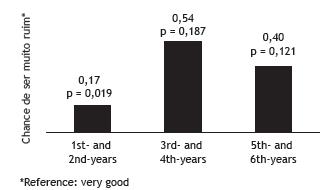
A more thorough analysis of subjective sleep quality, by using the classification of this quality as “very good” as a reference, revealed that only students in group A were statistically significantly likely to have “very bad” subjective sleep quality (Figure 1). Habitual sleep efficiency was considered adequate in 87.9% of the total sample, and the frequency of sleep disturbances was considered low in 84.6% of the total sample. In the group analysis, neither component showed significant differences.
Inductive statistics for the subjective sleep quality component and corresponding p values. Chi-square test.
Of the total sample, 8.6% of the participants reported using sleeping medication at least once a week, and 87.4% reported having difficulty staying awake during the day at least once a week. In addition, 50.4% reported having trouble engaging in daily activities at least once a week, and 70.6% reported dozing; of the latter, 47.7% did not intend to doze and 44.0% regarded dozing as necessary. In the group analysis, p values = 0.72 were obtained for use of sleeping medication, whereas, for daily dysfunction, group A showed a significant difference (p = 0.006; Figure 2).
Inductive statistics for the daytime dysfunction component and corresponding p values. Chi-square test.
The mean global PSQI scores for groups A, B, and C were, respectively, 6.62 ± 2.55, 6.20 ± 2.65, and 6.66 ± 2.64, and 12.9% of the total sample had scores < 5 (Table 3). Analysis by undergraduate class year revealed scores < 5 in 5.5% of first-years, 7.6% of second-years, 15.9% of third-years, 10.1% of fourth-years, 10.0% of fifth-years, and 9.4% of sixth-years. Logistic regression, considering results > 5 (1) and ≤ 5 (0) for assessing group influence, revealed no significant intergroup influence (p = 0.24).
In addition, the mean scores on the seven components of the PSQI were compared between groups, and no significant differences were found between any of the groups (Table 4).
DISCUSSION
Sleep quality among medical students is a subject that has been studied worldwide because of its repercussions on the academic routine and personal life of this population. Therefore, investigating sleep quality by means of an instrument that has been validated for use in Brazil and allows quantification, such as the PSQI,1111 Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, Miozzo IC, de Barba ME, et al. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med. 2011;12(1):70-5. https://doi.org/10.1016/j.sleep.2010.04.020
https://doi.org/10.1016/j.sleep.2010.04....
is extremely important for the monitoring of sleep health in such students, aiding in the planning of interventions aimed at raising awareness of this problem. By this means, we found that aspects of sleep quality were altered in our sample, with 12.9% of the participants having scores < 5, which indicate significant impairment in sleep quality.
Adherence in this study was nearly 70%, which is consistent with literature findings on the rate of return of this type of questionnaire (73.3%).77 Ribeiro CR, Oliveira SM, Silva YM. The impact of sleep quality in medical education [Article in Portuguese]. Rev Soc Bras Clin Med. 2014;12(1):8-14. In terms of participation by gender, we found a female predominance in effective participation in the study, which is not true for other studies that used this instrument with medical students, in which there was a predominance of males-73%88 Del Pielago Meoño AF, Failoc Rojas VE, Plasencia Dueñas EA, Díaz Vélez C Calidad de sueño y estilo de aprendizaje en estudiantes de Medicina Humana de la Universidad Nacional Pedro Ruiz Gallo. Act Méd Per. 2013;30(4):63-8. and 54.7%.99 Cardoso HC, Bueno FC, Mata JC, Alves AP, Jochims I, Vaz Filho IH, et al. Assessing quality of sleep in medical students [Article in Portuguese]. Rev Bras Educ Med. 2009;33(3):349-55. https://doi.org/10.1590/S0100-55022009000300005
https://doi.org/10.1590/S0100-5502200900...
Nearly 40% of the students in our sample classified their sleep quality as either very or fairly bad, a proportion that is lower than that reported in the literature, with findings of poor sleep quality in 61.5%1212 Rique GL, Fernandes Filho GM, Ferreira AD, de Sousa-Muñoz RL. Relationship between chronotype and quality of sleep in medical students at the Federal University of Paraiba, Brazil. Sleep Sci. 2014;7(2):96-102. https://doi.org/10.1016/j.slsci.2014.09.004
https://doi.org/10.1016/j.slsci.2014.09....
) and 61.9%,77 Ribeiro CR, Oliveira SM, Silva YM. The impact of sleep quality in medical education [Article in Portuguese]. Rev Soc Bras Clin Med. 2014;12(1):8-14. specifically among medical students. The poor sleep quality observed in group A is consistent with reports from other studies, which also observed these findings in incoming students, emphasizing the correlation between poor sleep quality and first-year undergraduates, in whom poor sleep hygiene habits, such as Internet surfing at night, poor social life, and bad eating habits, are found to be aggravating factors.1313 Cheng SH, Shih CC, Lee IH, Hou YW, Chen KC, Chen KT, et al. A study on the sleep quality of incoming university students. Psychiatry Res. 2012;197(3):270-4. https://doi.org/10.1016/j.psychres.2011.08.011
https://doi.org/10.1016/j.psychres.2011....
Poor sleep quality is associated with excessive daytime sleepiness.77 Ribeiro CR, Oliveira SM, Silva YM. The impact of sleep quality in medical education [Article in Portuguese]. Rev Soc Bras Clin Med. 2014;12(1):8-14.,99 Cardoso HC, Bueno FC, Mata JC, Alves AP, Jochims I, Vaz Filho IH, et al. Assessing quality of sleep in medical students [Article in Portuguese]. Rev Bras Educ Med. 2009;33(3):349-55. https://doi.org/10.1590/S0100-55022009000300005
https://doi.org/10.1590/S0100-5502200900...
In the present study, daytime dysfunction was reported by 36.9% of the participants, who had difficulty staying awake during the day at least once a week. This is consistent with the literature, although there are variations across studies in the proportion of medical students reporting daytime sleepiness: 31%77 Ribeiro CR, Oliveira SM, Silva YM. The impact of sleep quality in medical education [Article in Portuguese]. Rev Soc Bras Clin Med. 2014;12(1):8-14.; 42.1%1212 Rique GL, Fernandes Filho GM, Ferreira AD, de Sousa-Muñoz RL. Relationship between chronotype and quality of sleep in medical students at the Federal University of Paraiba, Brazil. Sleep Sci. 2014;7(2):96-102. https://doi.org/10.1016/j.slsci.2014.09.004
https://doi.org/10.1016/j.slsci.2014.09....
; and 63%.66 Pagnin D, de Queiroz V, Carvalho YT, Dutra AS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Acad Psychiatry. 2014;38(4):438-44. https://doi.org/10.1007/s40596-014-0093-z
https://doi.org/10.1007/s40596-014-0093-...
Therefore, students in group A experienced greater deleterious effects on subjective sleep quality and daytime dysfunction than did those in the other groups, with daytime dysfunction showing a trend toward a significant difference when comparing groups A and C (p = 0.05). This can be explained by the fact that incoming students go through a transitional period of change from attending preparatory courses for college entrance examinations and/or attending high school to attending an undergraduate course, which is characterized by too many academic activities and irregular daily routines, which vary too much because of the class load, shifts, breaks, and free study periods. It should also be emphasized that attending a medical course requires a high level of dedication and selflessness, signifying harmful lifestyle changes,1414 Mirghani HO, Mohammed OS, Almurtadha YM, Ahmed MS. Good sleep quality is associated with better academic performance among Sudanese medical students. BMC Res Notes. 2015;8:706. https://doi.org/10.1186/s13104-015-1712-9
https://doi.org/10.1186/s13104-015-1712-...
15 Mota MC, De-Souza DA, Mello MT, Tufik S, Crispim CA. Lifestyle and medical education: impact on the nutritional profile [Article in Portuguese]. Rev Bras Educ Med. 2012;36(3):358-68. https://doi.org/10.1590/S0100-55022012000500010
https://doi.org/10.1590/S0100-5502201200...
-1616 Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, et al. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med 2015;11(1):69-74. https://doi.org/10.5664/jcsm.4370
https://doi.org/10.5664/jcsm.4370...
such as sleep deprivation and poor sleep hygiene habits.1616 Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, et al. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med 2015;11(1):69-74. https://doi.org/10.5664/jcsm.4370
https://doi.org/10.5664/jcsm.4370...
,1717 Pérez-Olmos I, Ibáñez-Pinilla M. Night shifts, sleep deprivation, and attention performance in medical students. Int J Med Educ. 2014;5:56-62. https://doi.org/10.5116/ijme.531a.f2c9
https://doi.org/10.5116/ijme.531a.f2c9...
After the second year of the undergraduate course, there may be accommodation and better adaptation to the routine of studies and visits.
The results for the sleep latency component showed that sleep latency was slightly altered in 29.9% of the participants, whereas the results for the sleep duration component revealed that 68.0% of the participants reported sleeping 6-7 h per night, which is similar to the variation from 6 h and 55 min to 7 h and 25 min found in one study1818 Lima PF, Medeiros AL, Araujo JF. Sleep-wake pattern of medical students: early versus late class starting time. Braz J Med Biol Res. 2002;35(11):1373-7. https://doi.org/10.1590/S0100-879X2002001100016
https://doi.org/10.1590/S0100-879X200200...
and the average of 6.48 h reported by students at the Universidad Adventista del Plata,1919 Fontana SA, Raimondi W, Rizzo ML. Quality of sleep and selective attention in university students: descriptive cross-sectional study [Article in Spanish]. Medwave. 2014;14(8):e6015. https://doi.org/10.5867/medwave.2014.08.6015
https://doi.org/10.5867/medwave.2014.08....
but different from the average of 5.8 h of sleep per night reported by students at the Saudi Medical School.2020 Alsaggaf MA, Wali SO, Merdad RA, Merdad LA. Sleep quantity, quality, and insomnia symptoms of medical students during clinical years. Relationship with stress and academic performance. Saudi Med J. 2016;37(2):173-82. https://doi.org/10.15537/smj.2016.2.14288
https://doi.org/10.15537/smj.2016.2.1428...
Frequent use of sleeping medication was identified in 8.6% of the participants in the present study, but this proportion is lower than that found in a study involving medical students in Saudi Arabia, which identified that 17% of those students used drugs for sleep induction; this fact indicates the need for early intervention programs targeting poor lifestyle habits.2121 Al-Sayed AA, Al-Rashoudi AH, Al-Eisa AA, Addar AM, Al-Hargan AH, Al-Jerian AA, et al. Sedative Drug Use among King Saud University Medical Students: A Cross-Sectional Sampling Study. Depress Res Treat. 2014;2014:378738. https://doi.org/10.1155/2014/378738
https://doi.org/10.1155/2014/378738...
Global PSQI scores > 5 were observed in 87.1% of the our total sample, surpassing the literature findings of 59.4%55 Preišegolavičiūtė E, Leskauskas D, Adomaitiene V. Associations of quality of sleep with lifestyle factors and profile of studies among Lithuanian students. Medicina (Kaunas). 2010;46(7):482-9. and 20.7%.2222 Machado-Duque ME, Echeverri Chabur JE, Machado-Alba JE. Excessive Daytime Sleepiness, Poor Quality Sleep, and Low Academic Performance in Medical Students [Article in Spanish]. Rev Colomb Psiquiatr. 2015;44(3):137-42. https://doi.org/10.1016/j.rcp.2015.04.002
https://doi.org/10.1016/j.rcp.2015.04.00...
When we analyzed mean global PSQI scores, we found results between 6 and 7 in the different groups, values that are lower than those reported in another study (8.1).2323 Waqas A, Khan S, Sharif W, Khalid U, Ali A. Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. Peer J. 2015;3:e840. https://doi.org/10.7717/peerj.840
https://doi.org/10.7717/peerj.840...
In summary, we investigated sleep quality in medical students at one medical school in the city of Botucatu, Brazil, and found impairments in certain PSQI components, which suggests that investigations should continue in different regions of the country and the world, in order to monitor the profile of such students and encourage the translation of findings into health promotion practices. Our results are in agreement with literature findings of a high frequency of altered aspects in sleep quality, a high frequency that is not regarded as a problem or disorder, which may have harmful effects on health.
Since the most substantial results were obtained for the sleep quality and daily dysfunction components, a limitation of the present study was that we did not use other instruments, such as the Epworth Sleepiness Scale, which could provide details on daytime sleep dysfunction. In addition, specific protocols for assessing sleep habits could have been used to better compare student behaviors across the various phases of the medical course, given that students in group A had greater problems regarding subjective sleep quality and daytime dysfunction than did those in groups B and C.
There is a need for health promotion measures, such as proposals of changes in adopted health behaviors specifically related to good sleep hygiene, among the population of higher education students. Such proposals are found in the literature and are targeted at the general population,2424 Corrêa Cde C, Blasca WQ, Berretin-Felix G. Health promotion in obstructive sleep apnea syndrome. Int Arch Otorhinolaryngol. 2015;19(2):166-70. https://doi.org/10.1055/s-0034-1390327
https://doi.org/10.1055/s-0034-1390327...
,2525 Corrêa CC, Berretin-Felix G, Blasca WQ. Educational program applied to obstructive sleep apnea. Commun Disord Deaf Stud Hearing Aids. 2016;4(2):1-6. but they are also applicable to and indispensable for populations such as that of the present study.
We therefore conclude that poor subjective sleep quality was high for students in all class years of the undergraduate medical course. The comparison across the various phases of the course showed that first- and second-years (group A) reported worse sleep quality and greater daytime dysfunction than did those in other class years (groups B and C).
REFERENCES
-
1Benavente SB, Silva RM, Higashi AB, Guido Lde A, Costa AL. Influence of stress factors and socio-demographic characteristics on the sleep quality of nursing students [Article in Portuguese]. Rev Esc Enferm USP. 2014;48 (3):514-20. https://doi.org/10.1590/S0080-623420140000300018
» https://doi.org/10.1590/S0080-623420140000300018 -
2Mesquita G, Reimão R. Quality of sleep among university students: effects of nighttime computer and television use. Arq Neuropsiquiatr. 2010;68(5):720-5. https://doi.org/10.1590/S0004-282X2010000500009
» https://doi.org/10.1590/S0004-282X2010000500009 -
3Araújo MF, Feritas RW, Lima AC, Pereira DC, Zanetti ML, Damasceno MM. Health indicators associated with poor sleep quality among university students [Article in Portuguese]. Rev Esc Enferm USP. 2014;48(6):1085-92. https://doi.org/10.1590/S0080-623420140000700017
» https://doi.org/10.1590/S0080-623420140000700017 -
4Lemma S, Berhane Y, Worku A, Gelaye B, Williams MA. Good quality sleep is associated with better academic performance among university students in Ethiopia. Sleep Breath. 2014;18(2):257-63. https://doi.org/10.1007/s11325-013-0874-8
» https://doi.org/10.1007/s11325-013-0874-8 -
5Preišegolavičiūtė E, Leskauskas D, Adomaitiene V. Associations of quality of sleep with lifestyle factors and profile of studies among Lithuanian students. Medicina (Kaunas). 2010;46(7):482-9.
-
6Pagnin D, de Queiroz V, Carvalho YT, Dutra AS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Acad Psychiatry. 2014;38(4):438-44. https://doi.org/10.1007/s40596-014-0093-z
» https://doi.org/10.1007/s40596-014-0093-z -
7Ribeiro CR, Oliveira SM, Silva YM. The impact of sleep quality in medical education [Article in Portuguese]. Rev Soc Bras Clin Med. 2014;12(1):8-14.
-
8Del Pielago Meoño AF, Failoc Rojas VE, Plasencia Dueñas EA, Díaz Vélez C Calidad de sueño y estilo de aprendizaje en estudiantes de Medicina Humana de la Universidad Nacional Pedro Ruiz Gallo. Act Méd Per. 2013;30(4):63-8.
-
9Cardoso HC, Bueno FC, Mata JC, Alves AP, Jochims I, Vaz Filho IH, et al. Assessing quality of sleep in medical students [Article in Portuguese]. Rev Bras Educ Med. 2009;33(3):349-55. https://doi.org/10.1590/S0100-55022009000300005
» https://doi.org/10.1590/S0100-55022009000300005 -
10Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. https://doi.org/10.1016/0165-1781(89)90047-4
» https://doi.org/10.1016/0165-1781(89)90047-4 -
11Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, Miozzo IC, de Barba ME, et al. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med. 2011;12(1):70-5. https://doi.org/10.1016/j.sleep.2010.04.020
» https://doi.org/10.1016/j.sleep.2010.04.020 -
12Rique GL, Fernandes Filho GM, Ferreira AD, de Sousa-Muñoz RL. Relationship between chronotype and quality of sleep in medical students at the Federal University of Paraiba, Brazil. Sleep Sci. 2014;7(2):96-102. https://doi.org/10.1016/j.slsci.2014.09.004
» https://doi.org/10.1016/j.slsci.2014.09.004 -
13Cheng SH, Shih CC, Lee IH, Hou YW, Chen KC, Chen KT, et al. A study on the sleep quality of incoming university students. Psychiatry Res. 2012;197(3):270-4. https://doi.org/10.1016/j.psychres.2011.08.011
» https://doi.org/10.1016/j.psychres.2011.08.011 -
14Mirghani HO, Mohammed OS, Almurtadha YM, Ahmed MS. Good sleep quality is associated with better academic performance among Sudanese medical students. BMC Res Notes. 2015;8:706. https://doi.org/10.1186/s13104-015-1712-9
» https://doi.org/10.1186/s13104-015-1712-9 -
15Mota MC, De-Souza DA, Mello MT, Tufik S, Crispim CA. Lifestyle and medical education: impact on the nutritional profile [Article in Portuguese]. Rev Bras Educ Med. 2012;36(3):358-68. https://doi.org/10.1590/S0100-55022012000500010
» https://doi.org/10.1590/S0100-55022012000500010 -
16Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, et al. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med 2015;11(1):69-74. https://doi.org/10.5664/jcsm.4370
» https://doi.org/10.5664/jcsm.4370 -
17Pérez-Olmos I, Ibáñez-Pinilla M. Night shifts, sleep deprivation, and attention performance in medical students. Int J Med Educ. 2014;5:56-62. https://doi.org/10.5116/ijme.531a.f2c9
» https://doi.org/10.5116/ijme.531a.f2c9 -
18Lima PF, Medeiros AL, Araujo JF. Sleep-wake pattern of medical students: early versus late class starting time. Braz J Med Biol Res. 2002;35(11):1373-7. https://doi.org/10.1590/S0100-879X2002001100016
» https://doi.org/10.1590/S0100-879X2002001100016 -
19Fontana SA, Raimondi W, Rizzo ML. Quality of sleep and selective attention in university students: descriptive cross-sectional study [Article in Spanish]. Medwave. 2014;14(8):e6015. https://doi.org/10.5867/medwave.2014.08.6015
» https://doi.org/10.5867/medwave.2014.08.6015 -
20Alsaggaf MA, Wali SO, Merdad RA, Merdad LA. Sleep quantity, quality, and insomnia symptoms of medical students during clinical years. Relationship with stress and academic performance. Saudi Med J. 2016;37(2):173-82. https://doi.org/10.15537/smj.2016.2.14288
» https://doi.org/10.15537/smj.2016.2.14288 -
21Al-Sayed AA, Al-Rashoudi AH, Al-Eisa AA, Addar AM, Al-Hargan AH, Al-Jerian AA, et al. Sedative Drug Use among King Saud University Medical Students: A Cross-Sectional Sampling Study. Depress Res Treat. 2014;2014:378738. https://doi.org/10.1155/2014/378738
» https://doi.org/10.1155/2014/378738 -
22Machado-Duque ME, Echeverri Chabur JE, Machado-Alba JE. Excessive Daytime Sleepiness, Poor Quality Sleep, and Low Academic Performance in Medical Students [Article in Spanish]. Rev Colomb Psiquiatr. 2015;44(3):137-42. https://doi.org/10.1016/j.rcp.2015.04.002
» https://doi.org/10.1016/j.rcp.2015.04.002 -
23Waqas A, Khan S, Sharif W, Khalid U, Ali A. Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. Peer J. 2015;3:e840. https://doi.org/10.7717/peerj.840
» https://doi.org/10.7717/peerj.840 -
24Corrêa Cde C, Blasca WQ, Berretin-Felix G. Health promotion in obstructive sleep apnea syndrome. Int Arch Otorhinolaryngol. 2015;19(2):166-70. https://doi.org/10.1055/s-0034-1390327
» https://doi.org/10.1055/s-0034-1390327 -
25Corrêa CC, Berretin-Felix G, Blasca WQ. Educational program applied to obstructive sleep apnea. Commun Disord Deaf Stud Hearing Aids. 2016;4(2):1-6.
-
1
Study carried out at the Faculdade de Medicina de Botucatu, Universidade Estadual Paulista Júlio de Mesquita Filho - FM-UNESP - Botucatu (SP) Brasil.
-
Financial support:
None.
Publication Dates
-
Publication in this collection
Jul-Aug 2017
History
-
Received
22 June 2016 -
Accepted
14 Apr 2017