Abstract
OBJECTIVE: To examine the severity of trauma in entrapped victims and to identify risk factors for mortality and morbidity. INTRODUCTION: Triage and rapid assessment of trauma severity is essential to provide the needed resources during prehospital and hospital phases and for outcome prediction. It is expected that entrapped victims will have greater severity of trauma and mortality than non-entrapped subjects. METHODS: A transverse, case-control, retrospective study of 1203 victims of motor vehicle collisions treated during 1 year by the prehospital service in São Paulo, Brazil was carried out. All patients were drivers, comprising 401 entrapped victims (33.3%) and 802 non-entrapped consecutive controls (66.7%). Sex, age, mortality rates, Glasgow Coma Scale (GCS), Revised Trauma Score (RTS), corporal segments, timing of the prehospital care and resource use were compared between the groups. The results were analysed by χ2, Zres, analysis of variance and Bonferroni tests. RESULTS: Entrapped victims were predominantly men (84.8%), aged 32±13.1 years, with immediate mortality of 10.2% and overall mortality of 11.7%. They had a probability of death at the scene 8.2 times greater than that of non-entrapped victims. The main cause of death was hemorrhage for entrapped victims (45.2%) and trauma for non-entrapped victims. Of the entrapped victims who survived, 18.7% had a severe GCS (OR = 10.62), 12% a severe RTS (OR = 9.78) and 23.7% were in shock (OR = 3.38). Entrapped victims were more commonly transported to advanced life support units and to tertiary hospitals. CONCLUSION: Entrapped victims had greater trauma severity, more blood loss and a greater mortality than respective, non-entrapped controls.
Trauma severity; Blood loss; Public health; Traffic accidents
CLINICAL SCIENCE
Entrapped victims in motor vehicle collisions: characteristics and prehospital care in the city of São Paulo, Brazil
Adriano Rogério Navarro Dias; Simone de Campos Vieira Abib; Luiz Francisco Poli-de-Figueiredo; João Aléssio Juliano Perfeito
Federal University of São Paulo - Paulista School of Medicine - Surgery. E-mail: simoneabib@uol.com.br Tel.: 55 11 3836-0730
ABSTRACT
OBJECTIVE: To examine the severity of trauma in entrapped victims and to identify risk factors for mortality and morbidity.
INTRODUCTION: Triage and rapid assessment of trauma severity is essential to provide the needed resources during prehospital and hospital phases and for outcome prediction. It is expected that entrapped victims will have greater severity of trauma and mortality than non-entrapped subjects.
METHODS: A transverse, case-control, retrospective study of 1203 victims of motor vehicle collisions treated during 1 year by the prehospital service in São Paulo, Brazil was carried out. All patients were drivers, comprising 401 entrapped victims (33.3%) and 802 non-entrapped consecutive controls (66.7%). Sex, age, mortality rates, Glasgow Coma Scale (GCS), Revised Trauma Score (RTS), corporal segments, timing of the prehospital care and resource use were compared between the groups. The results were analysed by χ2, Zres, analysis of variance and Bonferroni tests.
RESULTS: Entrapped victims were predominantly men (84.8%), aged 32±13.1 years, with immediate mortality of 10.2% and overall mortality of 11.7%. They had a probability of death at the scene 8.2 times greater than that of non-entrapped victims. The main cause of death was hemorrhage for entrapped victims (45.2%) and trauma for non-entrapped victims. Of the entrapped victims who survived, 18.7% had a severe GCS (OR = 10.62), 12% a severe RTS (OR = 9.78) and 23.7% were in shock (OR = 3.38). Entrapped victims were more commonly transported to advanced life support units and to tertiary hospitals.
CONCLUSION: Entrapped victims had greater trauma severity, more blood loss and a greater mortality than respective, non-entrapped controls.
Keywords: Trauma severity; Blood loss; Public health; Traffic accidents.
INTRODUCTION
Morbidity and mortality of motor vehicle collisions play an important role in public health in industrialized countries, hence, efforts must aim at their prevention and care of the victims.1 A total of 383,371 traffic accidents with victims occurred in Brazil during 2005; 7% of the victims died. Of those dying, death occurred at the scene in 93% and some days after the event in 7%. Collisions were the main trauma mechanism (53.5%), followed by accidents involving pedestrians (17.5%).2 The impact of motor collisions on society may be underestimated, as young and economically productive people die or have permanent sequelae that generate high costs for the National System of Health.3
Although the number of entrapped victims is small, they have severe injuries that demand specific equipment and trained personnel during the prehospital phase of care, and such care is expensive. In São Paulo, Brazil, a single firemen headquarters regulate the dispatch of prehospital units and cared for about 12,000 motor collisions victims in 2003-of whom, 604 were entrapped.
Victims are considered to be entrapped when they cannot leave the vehicle because parts of the body or the whole body is confined in the distorted vehicle after the impact. Such a situation requires special extrication procedures. Deformity of the vehicle may be complete, when the vehicle structure is damaged, or relative, when the victim is entrapped by safety devices (security bars, seat belt, etc), or when they are confined in the vehicle because a door or window is blocked.4-6
Triage and rapid assessment of trauma severity is essential to assure that the resources required will be available during the prehospital and hospital phases of care, and for prediction of outcome.
The importance of evaluating the trauma severity and mortality of entrapped victims is essential to appreciate the violence involved in such accidents, and hence properly design the appropriate treatment.
OBJECTIVE
To examine the severity of trauma in entrapped victims and to identify risk factors for mortality and morbidity of this group of patients treated by the prehospital team in São Paulo, Brazil.
METHODS
São Paulo has 17 million inhabitants and the firemen headquarters receives about 5,000 calls a day, which leads to 450 dispatches a day. Whenever an accident is categorized as a collision with an entrapped victim, a group of units is dispatched; these include one unit with special devices for extrication, a basic unit (three firemen) and an advanced life support unit (a doctor, a nurse and a firemen). A transverse case-control retrospective study was designed, comparing 1203 victims of motor vehicle collisions, divided into two groups of patients: entrapped and non-entrapped victims, treated by the prehospital service of São Paulo, Brazil, from 2002 to 2003. A control group for each entrapped victim was formed from the non-entrapped victim immediately before, and immediately after, the entrapped victim. Data were collected from the Firemen Operation Control Center and from the Legal Medicine Institute from São Paulo, Brazil. Only drivers (aged >18 years) who were involved in motor vehicle collisions with small and medium-sized vehicles were included in the study. The following collisions were excluded: motor vehicle collisions outside the metropolitan area of the city of São Paulo, collisions involving larger vehicles (buses or trucks), pedestrians who were impaled on the vehicle, collisions involving motorcycles and bicycles, collisions with more than one entrapped victim, collisions in which the entrapped victim was not the driver, drivers aged <18 years.
Sex, age, mortality rates, Glasgow Coma Scale (GCS), Revised Trauma Score (RTS), presence of signs of shock, corporal segments, timing of the prehospital care, type of ambulance and hospital as final destination were compared between the groups.
For the severity score, RTS >7 was classified as mild, 5-6 as moderate or 0-4 as severe. GCS was mild, moderate or severe according to the Advance Trauma Life Support standards. Victims were classified in two groups: those with shock signs (pulse >100 bpm and systolic blood pressure <90 mmHg) and those with no such signs (pulse <100 bpm and systolic blood pressure >90 mmHg).
The following anatomic regions were considered for analysis: head, face, neck, shoulders and arms, thorax, abdomen, pelvis and/or legs.
Mortality was analyzed until 30 days after the traumatic event, and was divided into immediate (at the scene) and subsequent mortality up until the 30th day.
The final destination was classified as primary, secondary and tertiary hospitals (in Brazil, tertiary hospitals correspond to trauma centers).
The results were analysed by χ2, Zres, analysis of variance and Bonferroni tests.
RESULTS
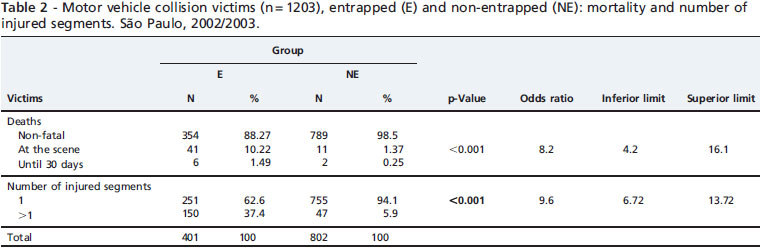
Of the initial total of 1233 victims, 10 were excluded together with their controls owing to a lack of information - a total of 30 victims, 2.4% of the sample. Thus 1203 victims were included in the study comprising 401 entrapped (32.5%) and 802 non-entrapped victims (65.1%). #Table 1 summarizes the gender and age of both groups. Mal victims were more common (76.9%), with a ratio of men:women of 3.33:1. Age varied from 18 to 93 years, median 32 (± 13.1) years, and the predominant age group was 18-23 years (29.3%). The overall mortality was 4.9%, being 4.3% at the scene and 0.7% subsequently up to 30 days. Entrapped victims died more frequently at the scene than non - entrapped ones (10.2% vs 1.37%) and also after 30 days (1.5% vs 0.25%). The profile of the entrapped victims was: male (84.8%), aged 23-30 years, immediate mortality of 10.2% and overall mortality of 11.7%. They had an 8.2 times greater probability of death at the scene than non-entrapped victims. The mortality of non-entrapped victims was 1.6% (p<0.001) (Table 2). Pelvis, legs and head were the corporal segments mainly injured in entrapped victims who survived. The number of injured segments was greater in the entrapped group than in non-entrapped victims (37.4% vs 5.9%) (Tables 2 and 3). Motor vehicle collisions with entrapped victims were more common in the peripheral north and east zones of São Paulo. Entrapped victims were more commonly transported in advanced support units and to tertiary hospitals. Hemorrhag was the major cause of death for entrapped victims (45.2%), whereas head trauma was the major cause for non-entrapped victims (Table 3). Entrapped victims who survived had a severe GCS in 18.7% (OR = 10.62), severe RTS in 12% (OR = 9.78) and 23.7% were in shock (OR = 3.38), compared with shock in 9.5% of non-entrapped victims. Thus, entrapped victims had a 3.4 times greater probability of having shock than non-entrapped ones (Table 4).
Length of time at the scene was greater in the entrapped group (median 27.3±16.3 min) than in the non-entrapped group (median 16.6±14 min) (p<0.001). Entrapped victims were more commonly transported by advanced support units (24.7%) and helicopter (3%) than non-entrapped ones (2%).
DISCUSSION
The reasons for the appalling numbers of collisions in the city are lack of city planning and lack of preventive actions-such as, education and severe traffic laws, maintenance of safe roads and streets and of the vehicles themselves. Unfortunately, the numbers continue to increase, but the prehospital capacity to care for these victims reached a plateau during the past 4 years. Attempts have been made to increase the prehospital capacity using motorcycles to cut through the heavy traffic in order to reach the victims rapidly, but trauma victims need to be properly immobilized and transported in ambulances; however, the use of motorcycles can be useful to reach the victims of a heart attack more quickly.
The numbers of accidents in the city of São Paulo demonstrate the need for good databases for trauma in the city, including the prehospital and hospital phases, and also to record the sequelae and impact of preventive actions. Continuous monitoring of the data is needed so that the actions and protocols can be adapted as necessary.
Entrapped victims have more severe trauma and multiple injuries, which may be worsened by the extrication procedures. Thus, the personnel involved must have proper training in order to minimize complications.4,7 This study shows a significant difference in the mortality rates of entrapped victims (11.7%) compared with non-entrapped ones (1.6%). They have an 8.2 times greater probability of death at the scene than those who are not entrapped. Such findings indicate that a proper strategy for diagnosis and treatment is needed, in order to enhance survival and minimize morbidity, which is the target of the prehospital phase. The mortality of non-entrapped victims in this series was lower than mortality rates reported in the literature (4-45%),8,9 probably because our studies do not refer to the kinetics of trauma, or to other variables involved in the event.
Olson et al.10 and Sauai et al.11 studied the impact of prehospital care in trauma victims and concluded that the kinetics and causes of death were similar, but that the late mortality due to head trauma increased. Another interesting finding was that there has been a shift in the three peaks of mortality previously described. Our findings show that entrapped victims follow the previous pattern described by Trunkey et al. in 1977, with greater mortality in the prehospital phas.
It is essential to assess the severity of the victim's injuries, so that the necessary procedures and treatment can be implemented rapidly, thus reducing morbidity and mortality. Traffic education, the use of security devices other than the seat belt and salvage procedures must be reviewed to achieve this aim.2,12
Many studies in many countries have used different severity scores and obtained divergent results owing to the variations in populations and methods used during the prehospital phase of care.3,4,13-18 Our study separated the entrapped victims from other collision victims, aiming to examine the severity, in order to offer specific tools in the prehospital phase. The severity scores analyzed showed that entrapped victims have more frequent severe (10 times more) and moderate scores than non-entrapped subjects, although there are limitations and disagreements about the anatomic and physiologic trauma scores for triage and survival evaluation, owing to population differences, type of trauma and type of prehospital system of care.19-22 Because entrapped victims have a different degree of trauma severity, requiring greater times at the scene, further studies are necessary to verify the sensitiv ity, specificity and reliability of trauma scores in such situations. We suggest that time should be incorporated in the scores of entrapped victims, so that severity and mortality can be better analyzed. This score could be useful in determining the best timing for invasive procedures during extrication, without making the situa tion worse.
Blood pressure is a well-known parameter in emergency care, both in prehospital and hospital scenarios. Dove et al. studied 3000 trauma victims and observed that 50% of them presented shock signs at admission, and of the 108 fatalities, 80% had shock signs before entering the emergency room.21-23 For this reason we studied this parameter in the entrapped group, during the prehospital care. Our results show that entrapped victims have a 3 times greater chance of having shock signs, which is directly related to severity and timing. So, entrapped victims presenting shock must be dealt with effectively, using advanced support procedures and rapid extrication maneuvers, to reduce the scene time and guarantee rapid transportation to the appropriate hospital facility.
The anatomic distribution of injuries tends to relate to the vulnerability of each segment of the body, as well as to the type of event.11,24,25 The vulnerability of various segments of entrapped victims enhances the need for careful primary and secondary examinations, and, in particular, constant and multisystemic reassessment, so that early management of injuries can be accomplished.
Necropsy findings showed that non-entrapped victims died owing to head trauma, and entrapped victims owing to hemorrhage, confirming the hypothesis of greater impairment of segments other than the head. Further studies are needed to provide details about the sources of hemorrhage, so that new guidelines can be designed for its treatment (conservative or surgical treatment to control bleeding) during the prehospital care period.
Although the protection afforded by seat belts is limited, their use in reducing mortality is obvious. It prevents the victim from being ejected from the vehicle and reduces the impact of the body against the internal parts of the vehicle. Our study did not examine the use of this safety device, but the limited protection offered by the seat belt may explain why entrapped victims had the anatomic injury distribution reported and also greater trauma severity. This fact emphasizes the need for better traffic policies, including the requirement by law of other security devices (airbags, protection bars) and not as optional devices in vehicles, as they are at present.
CONCLUSIONS
In conclusion, the majority of entrapped victims cared for by the prehospital system in São Paulo are young, male, and had a greater chance of either dying at the scene or having severe injuries than non-entrapped ones. Prospective studies are needed to guide the implementation of emergency systems and protocols of treatment for the prehospital care of such victims.
REFERENCES
1. ABRAMET. Associação Brasileira de Medicina de Tráfego [database online]. São Paulo, Brasil. Available at: http://www.abramet.org/atlas.zi.
2. DENATRAN - Departamento Nacional de Trânsito [database online]. São Paulo, Brazil. Available at: http://www.denatran.gov.br/.
3. DATASUS - Banco de Dados do Sistema Único de Saúde [database online]. Brazil. Available at: http://tabnet.datasus.gov.br/cgi/idb2006/matriz.htm<morb.
4. SEADE - Fundação Sistema Estadual de Análise de Dados [database online]. São Paulo. Brasil. Available at: http://www.seade.gov.br/produtos/anuario/2003/index.php
5. Siegel JH, Loo G, Dischinger PC, Burgess AR, Wang SC, Schneider LW, et al. Factors influencing the patterns of injuries and outcomes in car versus car crashes compared to sport utility, van, or pick-up truck versus car crashes: Crash Injury Research Engineering Network Study. J Trauma. 2001;51:975-90.
6. Wilmink AB, Samra GS, Watson LM, Wilson AW. Vehicle entrapment rescue and prehospital trauma care. Injury. 1996;27:21-5, doi: 10.1016/0020-1383(95)00162-X.
7. Alves D, Mussi FC, Jeukens MM, Furbringer E, Silva SC, Da Silva EB, et al. What do patients with head injuries remember about their time of hospitalization? Rev Lat Am Enfermagem. 2000;8:91-8.
8. Lerner EB, Maio RF, Garrison HG, Spaite DW, Nichol G. Economic value of out-of-hospital emergency care: a structured literature review. Ann Emerg Med. 2006;47:515-24, doi: 10.1016/j.annemergmed.2006.01.012.
9. Liberman M, Roudsari BS. Prehospital trauma care: what do we really know? Curr Opin Crit Care. 2007;13:691-6, doi: 10.1097/MCC.0b013e3282f1e77e.
10. Olson CJ, Brand D, Mullins RJ, Harrahill M, Trunkey DD. Time to death of hospitalized injured patients as a measure of quality of care. J Trauma. 2003;55:45-52.
11. Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, et al. Epidemiology of trauma deaths: a reassessment. J Trauma 1995;38:185-93.
12. Shapiro MJ, Morey JC, Small SD, Langford V, Kaylor CJ, Jagminas L, et al. Simulation based teamwork training for emergency department staff: does it improve clinical team performance when added to an existing didactic teamwork curriculum? Qual Saf Health Care. 2004;13:417-21, doi: 10.1136/qshc.2003.005447.
13. Clark DE. Motor vehicle crash fatalities in the elderly: rural versus urban. J Trauma. 2001;51:896-900.
14. Bachulis BL, Sangster W, Gorrell GW, Long WB. Patterns of injury in helmeted and nonhelmeted motorcyclists. Am J Surg. 1988;155:708-11.
15. Chen B, Maio RF, Green PE, Burney RE. Geographic variation in preventable deaths from motor vehicle crashes. J Trauma. 1995;38:228-32.
16. Muelleman RL, Wadman MC, Tran TP, Ullrich F, Anderson JR. Rural motor vehicle crash risk of death is higher after controlling for injury severity. J Trauma. 2007;62:221-6.
17. Ersson A, Lundberg M, Wramby CO, Svensson H. Extrication of entrapped victims from motor vehicle accidents: the crew concept. Eur J Emerg Med. 1999;6:341-7.
18. Drongowski RA, Coran AG, Maio RF, Polley TZ Jr. Trauma scores, accident deformity codes, and car restraints in children. J Pediatr Surg. 1993;28:1072-5, doi: 10.1016/0022-3468(93)90522-M.
19. Taheri PA., Butz DA., Lottenberg L, Clawson A, Flint LM. The cost of trauma center readiness. Am J Surg. 2004;187(1):7-13.
20. Treviranus GR. Safety belt restraints and compartment intrusions in frontal and lateral motor vehicle crashes. J Trauma. 1995;38:459-62.
21. Abib SCV, Schettini ST, Poli de Figueiredo LF. Prehospital pediatric trauma classification (PHPTC) as a tool for optimizing trauma care resources in the city of São Paulo, Brazil. Acta Cir Bras. 2006;21:7-11, doi: 10.1590/S0102-86502006000100003.
22. Whitaker IY, De Gutiérrez MG, Koizumi MS. Trauma severity assessment in prehospital setting. Rev Assoc Med Bras. 1998;44:111-9, doi: 10.1590/S0104-42301998000200008.
23. Dove DB, Stahl WM, Delguercio LR. A five-year review of deaths following urban trauma. J Trauma. 1980;20:760-6.
24. Muelleman RL, Wadman MC, Tran TP, Ullrich F, Anderson JR. Rural motor vehicle crash risk of death is higher after controlling for injury severity. J Trauma. 2007;62:221-6.
25. Trunkey DD. Trauma centers and trauma systems. JAMA. 2003;289:1566-7, doi: 10.1001/jama.289.12.1566.
Received for publication on September 24, 2010; First review completed on September 27, 2010; Accepted for publication on October 1, 2010
-
1ABRAMET. Associação Brasileira de Medicina de Tráfego [database online]. São Paulo, Brasil. Available at: http://www.abramet.org/atlas.zi
» link -
2DENATRAN - Departamento Nacional de Trânsito [database online]. São Paulo, Brazil. Available at: http://www.denatran.gov.br/
» link -
4SEADE - Fundação Sistema Estadual de Análise de Dados [database online]. São Paulo. Brasil. Available at: http://www.seade.gov.br/produtos/anuario/2003/index.php
» link - 5. Siegel JH, Loo G, Dischinger PC, Burgess AR, Wang SC, Schneider LW, et al. Factors influencing the patterns of injuries and outcomes in car versus car crashes compared to sport utility, van, or pick-up truck versus car crashes: Crash Injury Research Engineering Network Study. J Trauma. 2001;51:975-90.
- 6. Wilmink AB, Samra GS, Watson LM, Wilson AW. Vehicle entrapment rescue and prehospital trauma care. Injury. 1996;27:21-5, doi: 10.1016/0020-1383(95)00162-X.
- 7. Alves D, Mussi FC, Jeukens MM, Furbringer E, Silva SC, Da Silva EB, et al. What do patients with head injuries remember about their time of hospitalization? Rev Lat Am Enfermagem. 2000;8:91-8.
- 8. Lerner EB, Maio RF, Garrison HG, Spaite DW, Nichol G. Economic value of out-of-hospital emergency care: a structured literature review. Ann Emerg Med. 2006;47:515-24, doi: 10.1016/j.annemergmed.2006.01.012.
- 9. Liberman M, Roudsari BS. Prehospital trauma care: what do we really know? Curr Opin Crit Care. 2007;13:691-6, doi: 10.1097/MCC.0b013e3282f1e77e.
- 10. Olson CJ, Brand D, Mullins RJ, Harrahill M, Trunkey DD. Time to death of hospitalized injured patients as a measure of quality of care. J Trauma. 2003;55:45-52.
- 11. Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, et al. Epidemiology of trauma deaths: a reassessment. J Trauma 1995;38:185-93.
- 12. Shapiro MJ, Morey JC, Small SD, Langford V, Kaylor CJ, Jagminas L, et al. Simulation based teamwork training for emergency department staff: does it improve clinical team performance when added to an existing didactic teamwork curriculum? Qual Saf Health Care. 2004;13:417-21, doi: 10.1136/qshc.2003.005447.
- 13. Clark DE. Motor vehicle crash fatalities in the elderly: rural versus urban. J Trauma. 2001;51:896-900.
- 14. Bachulis BL, Sangster W, Gorrell GW, Long WB. Patterns of injury in helmeted and nonhelmeted motorcyclists. Am J Surg. 1988;155:708-11.
- 15. Chen B, Maio RF, Green PE, Burney RE. Geographic variation in preventable deaths from motor vehicle crashes. J Trauma. 1995;38:228-32.
- 16. Muelleman RL, Wadman MC, Tran TP, Ullrich F, Anderson JR. Rural motor vehicle crash risk of death is higher after controlling for injury severity. J Trauma. 2007;62:221-6.
- 17. Ersson A, Lundberg M, Wramby CO, Svensson H. Extrication of entrapped victims from motor vehicle accidents: the crew concept. Eur J Emerg Med. 1999;6:341-7.
- 18. Drongowski RA, Coran AG, Maio RF, Polley TZ Jr. Trauma scores, accident deformity codes, and car restraints in children. J Pediatr Surg. 1993;28:1072-5, doi: 10.1016/0022-3468(93)90522-M.
- 19. Taheri PA., Butz DA., Lottenberg L, Clawson A, Flint LM. The cost of trauma center readiness. Am J Surg. 2004;187(1):7-13.
- 20. Treviranus GR. Safety belt restraints and compartment intrusions in frontal and lateral motor vehicle crashes. J Trauma. 1995;38:459-62.
- 21. Abib SCV, Schettini ST, Poli de Figueiredo LF. Prehospital pediatric trauma classification (PHPTC) as a tool for optimizing trauma care resources in the city of São Paulo, Brazil. Acta Cir Bras. 2006;21:7-11, doi: 10.1590/S0102-86502006000100003.
- 22. Whitaker IY, De Gutiérrez MG, Koizumi MS. Trauma severity assessment in prehospital setting. Rev Assoc Med Bras. 1998;44:111-9, doi: 10.1590/S0104-42301998000200008.
- 23. Dove DB, Stahl WM, Delguercio LR. A five-year review of deaths following urban trauma. J Trauma. 1980;20:760-6.
- 24. Muelleman RL, Wadman MC, Tran TP, Ullrich F, Anderson JR. Rural motor vehicle crash risk of death is higher after controlling for injury severity. J Trauma. 2007;62:221-6.
- 25. Trunkey DD. Trauma centers and trauma systems. JAMA. 2003;289:1566-7, doi: 10.1001/jama.289.12.1566.
Publication Dates
-
Publication in this collection
15 Mar 2011 -
Date of issue
2011
History
-
Accepted
01 Oct 2010 -
Reviewed
27 Sept 2010 -
Received
24 Sept 2010