Abstract
OBJECTIVES: The aim of this prospective study was to compare changes in lipid metabolism and nutritional status after either 6 and 12 months of follow-up in subjects with lipodystrophy syndrome after traditional lifestyle therapy with or without fibric acid analogue intervention (bezafibrate and clofibrate). METHODS: Food intake, alterations in body composition and metabolic abnormalities were assessed in subjects with lipodystrophy syndrome at the beginning of the study. The nutritional status and metabolic alterations of the subjects were monitored, and the subjects received nutritional counseling each time they were seen. The subjects were monitored either two times over a period no longer than six months (Group A; n = 18) or three times over a period of at least 12 months (Group B; n = 35). All of the subjects underwent nutrition counseling that was based on behavior modification. The fibric acid analogue was only given to patients with serum triglyceride levels above 400 mg/dL. RESULTS: After six months of follow-up, Group A showed no alterations in the experimental parameters. After twelve months, there was a decrease in serum triglyceride levels (410.4 ± 235.5 vs. 307.7 ± 150.5 mg/dL, p< 0.05) and an increase in both HDLc levels (37.9±36.6 vs. 44.9 ±27.9 mg/dL, p,0.05) and lean mass (79.9 ± 7.8 vs. 80.3 ± 9.9 %, p< 0.05) in Group B. CONCLUSION: After one year of follow-up (three sessions of nutritional and medical counseling), the metabolic parameters of the subjects with lipodystrophy improved after traditional lifestyle therapy with or without fibric acid analogue intervention.
HIV-Positive Patients; Dyslipidemia; Nutritional Assessment; Lipid Metabolism; Fibrate
CLINICAL SCIENCE
Nutritional and metabolic status of HIV-positive patients with lipodystrophy during one year of follow-up
Eloísa Marchi dos AnjosI; Karina PfrimerII; Alcyone Artioli MachadoII; Selma Freire de Carvalho CunhaII; Roberta Garcia SalomãoI; Jacqueline Pontes MonteiroI
INutrition and Metabolism, School of Medicine of Ribeirão Preto, University of São Paulo, Department of Pediatrics, Ribeirão Preto/SP, Brazil
IIDivision of Clinical Nutrition/Department of Internal Medicine, School of Medicine of Ribeirao Preto, University of São Paulo, Ribeirão Preto/SP, Brazil
ABSTRACT
OBJECTIVES: The aim of this prospective study was to compare changes in lipid metabolism and nutritional status after either 6 and 12 months of follow-up in subjects with lipodystrophy syndrome after traditional lifestyle therapy with or without fibric acid analogue intervention (bezafibrate and clofibrate).
METHODS: Food intake, alterations in body composition and metabolic abnormalities were assessed in subjects with lipodystrophy syndrome at the beginning of the study. The nutritional status and metabolic alterations of the subjects were monitored, and the subjects received nutritional counseling each time they were seen. The subjects were monitored either two times over a period no longer than six months (Group A; n = 18) or three times over a period of at least 12 months (Group B; n = 35). All of the subjects underwent nutrition counseling that was based on behavior modification. The fibric acid analogue was only given to patients with serum triglyceride levels above 400 mg/dL.
RESULTS: After six months of follow-up, Group A showed no alterations in the experimental parameters. After twelve months, there was a decrease in serum triglyceride levels (410.4 ± 235.5 vs. 307.7 ± 150.5 mg/dL, p< 0.05) and an increase in both HDLc levels (37.9±36.6 vs. 44.9 ±27.9 mg/dL, p,0.05) and lean mass (79.9 ± 7.8 vs. 80.3 ± 9.9 %, p< 0.05) in Group B.
CONCLUSION: After one year of follow-up (three sessions of nutritional and medical counseling), the metabolic parameters of the subjects with lipodystrophy improved after traditional lifestyle therapy with or without fibric acid analogue intervention.
Keywords: HIV-Positive Patients; Dyslipidemia; Nutritional Assessment; Lipid Metabolism; Fibrate.
INTRODUCTION
The treatment of human immunodeficiency virus (HIV) infection with HAART (highly active antiretroviral therapy), particularly the inclusion of protease inhibitors, was a major advance in improving the survival of HIV-positive individuals. However, this therapy is associated with a lipodystrophy syndrome, which involves the wasting of adipose tissue from peripheral sites with the preservation of central adipose depots, hyperlipidemia, impaired glucose tolerance and overt type 2 diabetes.1
The consumption of a low-glycemic-index diet that is also low in saturated fats and high in vitamins, fiber, mono unsaturated fatty acids and polyunsaturated fatty acids may decrease triglyceride and low-density lipoprotein choles terol levels in HIV-negative and HIV-positive subjects with cardiovascular risk factors.2-5 Twenty percent of persons with HIV who are on the HAART have a 10-year risk of developing coronary heart disease of 10% or higher, and this risk may also be associated with inadequate dietary habits.6 The nutritional strategies used to manage AIDS related lipodystrophy syndrome are not well described, and fibrates have been shown to have a significant effect on the treatment of diet-resistant hyperlipidemia. Fibrates are carboxylic acids that are used in the treatment of dyslipidemia because they moderately lower LDLc levels, significantly lower triglyceride levels and raise HDLc levels. Micronized fenofibrate is a fibrate derivative that was approved in February 1998 by the Food and Drug Administration (FDA).7 Examples of fibrates include ciprofibrate, bezafibrate, etofibrate, beclofibrate and pirifibrate.
The present study aimed to confirm the hypothesis that, with the same medical and nutritional counseling, twelve months of follow-up is more effective than six months of follow-up in both the treatment of hyperlipidemia and the improvement of nutritional status in HIV-1-positive patients with lipodystrophy.
MATERIALS AND METHODS
Using a computer program, 53 HIV-1-positive8,9 adult patients with lipodystrophy syndrome were randomly recruited from the outpatient clinic of infectious diseases at the School Hospital of the University of São Paulo, Ribeirão Preto, Brazil, which provides treatment for 240 subjects annually.
Criteria for inclusion in the study included confirmed HIV infection and the use of continuous HAART with at least one protease inhibitor (PI) and two nucleoside reverse transcriptase inhibitors (NRTI) for > 2 months. All of the patients provided written informed consent as approved by the local Institutional Review Board.
The nutritional assessments and laboratory analyses were performed at baseline (during the first visit), after 6 months and after 12 months. The weight and height of each participant were measured using standard methods that have been previously validated.10,11 Body mass index [BMI - weight (kg)/ height2 (meters)] was calculated by the standard formula using height and weight. The mid-arm circumference, subscapular skinfold and triceps skinfold were also measured as a reflection of lean body and fat mass.10 Lipid profiles were measured using standard clinical laboratory methods.12
The impedance bioelectric technique was performed with a BIA RJL System 101Q® (BIA-101A; RJL Systems, Clinton Township, MI) to measure body composition.
The nutritional and medical counseling was based on recall of food intake, representative examples of each patient's usual diet and encouragement to consume a lowglycemic-index diet that was also low in saturated fat (, 10% total energy) and high in vitamins, fiber (25 g/day), monoun saturated fatty acids (< 10% total energy), and polyunsaturated fatty acids (>10% total energy). The counseling was based on behavior modification13 and took approximately 2 hours. Fibrate analogues were adminis tered to the subjects with hyperlipidemia whose triglyceride levels were > 400 mg/dl. The subjects were divided into two groups according to the length of follow-up, and each subject attended nutritional and medical counseling sessions either two times over a period no longer than six months (Group A; n = 18) or three times over a period of at least 12 months (Group B; n = 35).
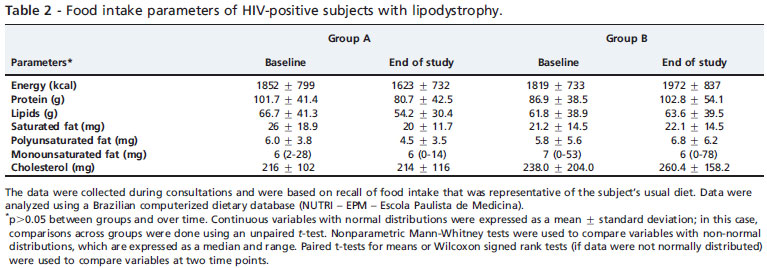
Energy and nutrient intake was analyzed using a Brazilian computerized dietary database (NUTRI-EPM-Escola Paulista de Medicina).
Demographic data and physical activity level were also recorded in the database.
Statistical analyses were performed using SPSS 10.0 software. Continuous variables with normal distributions were expressed as mean ± standard deviation, and comparisons across groups were done by unpaired t-test for these variables. The nonparametric Mann-Whitney test was used to compare variables with non-normal distributions, which are represented by the median and range. Paired ttests for means or Wilcoxon signed rank tests (if data were not normally distributed) were used to compare the variables at two different time points. Nominal data were analyzed by either the x 2 or Fisher exact test. P values of < 0.05 were considered statistically significant.
RESULTS
The rate of subject compliance was 100%. Nutritional status and metabolic alterations were monitored, and the subjects received nutritional counseling at every appointment. The 53 subjects were divided into two groups: Group (A) consisted of subjects who were monitored two times over a period no longer than six months (n = 18), and Group (B) consisted of subjects who were monitored three times over a period of at least 12 months (n = 35). The majority of the subjects were men (Group A = 76%; Group B = 80%), and the groups were age-matched (Group A = 47.1 ± 11.1; Group B = 43.3 ± 7.9 years of age; p > 0.05). None of the subjects claimed to exercise regularly. All of the subjects had serum triglyceride levels that were greater than or equal to 150 mg/dl, but subjects were only given a fibrate if their serum levels were above 400 mg/dl. Six patients (33.33%) in Group A received fibrates (bezafibrate or clofibrate), and twelve (34.3%) patients in Group B received fibrates (bezafibrate or clofibrate) (p = 0.94).
There were no changes in the anthropometric and metabolic parameters of Group A. In Group B, the triglycer ide levels were significantly lower and the HDL levels and lean mass were significantly higher at the end of the study (Table 1). No statistically significant differences in food intake were observed between the two groups (Table 2).
DISCUSSION
The findings of our study suggest that HIV-positive patients with lipodystrophy who were followed for twelve months (three nutritional and medical counseling sessions) in an outpatient clinic for infectious diseases showed an improvement in serum triglyceride and HDLc levels and an increase in lean mass compared to HIV-positive patients with lipodystrophy who received the same multidisciplinary approach but were followed for only six months (two nutritional and medical counseling sessions). These results cannot be attributed to differences in either food intake or the percentage of subjects taking a fibrate because there were no differences in these variables between the two groups.
The levels of total cholesterol and LDL-cholesterol did not significantly improve during the study. Some possible reasons for this lack of effect include the pathophysiology of lipid abnormalities in HIV-infected patients14 and the effects of antiretrovirals, which may have limited the effects of lifestyle modification on lipid metabolism.
The lipid profiles of HIV-positive patients are characterized by low levels of HDL (high density lipoprotein) and high levels of both LDL (low density lipoprotein) cholesterol and total cholesterol; this type of lipid profile predisposes patients to atherogenesis. Some studies have shown that the incidence of cardiovascular events in patients with HIV infection who are on HAART is higher than that in the general population.15 Diet therapy is recommended for primary prevention and control of dyslipidemia in HIVpositive patients on HAART.16
Our study failed to reveal any statistically significant changes in food intake after either 6 or 12 months of follow up. These results could be partially explained by either an under or overestimation of food intake resulting from memory bias and an inability to diet.17 Similar results were reported in another study in which no differences in dietary intake parameters were observed between a group receiving weekly one-on-one counseling sessions and a control group.18
As has been reported previously,19,20 no anthropometric changes were detected during the present study. More sophisticated techniques, such as DEXA or CT, would have provided a clearer view of the relative changes in body tissue composition over time.
Our results revealed a significant alteration in free-fat mass. Other variables, such as physical activity level, may also have contributed to this finding, but none of the subjects claimed to exercise regularly. The significant alterations in body composition in patients with HIV were characterized by bioelectrical impedance analysis (BIA), but this form of analysis may not accurately assess body composition in patients with lipodystrophy. A recent longitudinal study reported no significant differences in estimates of changes in fat mass.22
A change in diet alone can markedly improve elevated triglyceride levels, but these levels are unlikely to return to normal without interventional counseling. In Brazil, lipidlowering agents, such as gemfibrozil and fenofibrate, have been used to treat isolated or severe hypertriglyceridemia and/or elevated LDL and total cholesterol levels in patients who do not respond to modification of antiretroviral therapy or therapeutic lifestyle changes, as well as in patients in whom such modifications are not appropriate. 23 Fibrates, such as gemfibrozil, increase the activity of lipoprotein lipase, resulting in a reduction in triglyceride levels.24 Gemfibrozil and other fibrates activate peroxisome proliferator-activated receptors (PPARs), which allows these drugs to modulate lipoprotein metabolism.25
Several studies have found that, when used for primary prevention, fibrate therapy leads to a 71% decrease in residual risk, leaving only a 3.8% major CVD event rate. Others studies have shown that fibrate therapy, when used in primary prevention, reduces the residual risk by 19% to 8.9%.26,27
The difference in sample size between the two groups was not a confounding variable because, when we did statistical analyses that randomly excluded subjects in Group B, the results were the same (data not shown).
The present study suggests that, with the same nutritional and medical treatment, patients who were followed for at least twelve months showed a stronger improvement in their lipid profiles than those who were followed for only six months. Confounding clinical and social issues, such as medication interactions, comorbidities, lipodystrophy, food insecurity, aging, and other related conditions, further complicate disease management. Despite a greater understanding of the mechanisms of HIV/AIDS and its impact on the body, as well as the development of new treatments, the wide range of populations affected make the management of chronic HIV infection a complex and demanding issue.28
CONCLUSIONS
Our results suggest that subjects with lipodystrophy syndrome show an improvement in metabolic parameters after nutritional counseling with or without concurrent treatment with a fibrate analogue after one year of followup. Our experimental design did not allow us to distinguish between the effects of these two variables on the metabolic profile. Considering that there was no change in food intake during the follow-up period in either group and that the proportion of patients using fibrate was the same in both groups, it is possible that the effects were due to the combination of the two treatments for a longer period of time. However, studies investigating this issue are scarce. Further double-blind, randomized clinical trials are contributing to clarify the recommendations for nutritional and medical treatment of lipodystrophy syndrome.
ACKNOWLEDGMENTS
We would like to thank the HIV/AIDS Counseling Unit for assisting in this study. We received no financial support for this study, and the authors do not have any associations that might pose a conflict of interest.
Received for publication on November 5, 2010; First review completed on November 5, 2010; Accepted for publication on November 17, 2010
E-mail: jacque@fmrp.usp.br. Tel.: 55 16 3602 2478
- 1. Carr A, Samaras K, Thorisdottir A, Kaufmann GR, Chisholm DJ, Cooper DA. Diagnosis, prediction, and natural history of HIV-1 proteaseinhibitor-associated lipodystrophy, hyperlipidaemia, and diabetes mellitus: a cohort study. Lancet. 1999;353:2093-9, doi: 10.1016/S0140 6736(98)08468-2.
- 2. Welty FK, Nasca MM, Lew NS, Gregoire S, Ruan Y. Effect of onsite Dietitian counseling on weight loss and lipid levels in an outpatient physician office. Am J Cardiol. 2007;100:73-5, doi: 10.1016/j.amjcard. 2007.02.056.
- 3. Holmes A L, Sanderson B, Maisiak R, Brown A, Bittner V. Dietitian Services are Associated with improved patient outcomes and the MEDIFICTS dietary assessment questionnaire is a suitable outcome measure in cardiac rehabilitation. J Am Diet Assoc. 2005;105:1533-40, doi: 10.1016/j.jada.2005.08.001.
- 4. Hendricks KM, Dong KR, Tang AM, Ding B, Spiegelman D, Woods MN, et al. High-fiber diet in HIV-positive men is associated with lower risk of developing fat deposition. Am J Clin Nutr. 2003;78:790-5.
- 5. Roubenoff R, Schmitz H, Baioros L, Layne J, Potts E, Cloutier GJ, et al. Reduction of abdominal obesity in lipodystrophy associated with human immunodeficiency virus infection by means of diet and exercise: case report and proof of principle. Clin Infect Dis. 2002;34:390-3, doi: 10.1086/338402.
- 6. Salyer J, Lyon DE, Settle J, Elswick RK, Rackley D. Coronary heart disease risks and lifestyle behaviors in persons with HIV infection. JANAC. 2006;17:3-17, doi: 10.1016/j.jana.2006.03.001.
- 7. Gray DRP. Micronized fenofibrate: a new fibric acid hypolipidemic agent The Annals of Pharmacotherapy. 1999;33:1083-103.
- 8. Centers for Diseases Control and Prevention. 1993 Revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Morb Mortal Wkly Rep. 1992;41(RR-17):1.
- 9. Ministério da Saúde. Programa Nacional de Doenças Sexualmente Transmissíveis/AIDS. Revisão da definição nacional do caso de AIDS em adultos. Brasília: Ministério da Saúde, 1992;2.
- 10. World Health Organization. Physical status: the use and interpretation of anthropometry. WHO. 1995; Technical Report Series 854.
- 11. Ulijaszek SJ, Kerr DA. Anthropometric measurement error and the assessment of nutrition status. Br J Nutr. 1999;82:165-77, doi: 10.1017/S0007114599001348.
- 12. Yanovski JA, Miller KD, Kino T, Friedman TC, Chrousos GP, Tsigos C, et al. Endocrine and metabolic evaluation of human immunodeficiency virus-infected patients with evidence of protease inhibitor-associated lipodystrophy. J Clin Endocrinol Metab. 1999; 84:1925-31, doi: 10.1210/jc. 84.6.1925.
- 13. Fields-Gardner C, Fergusson P. Nutrition Intervention in the care of persons with human immunodeficiency virus infection: Position of the American Dietetic Association (ADA) and Dietitians of Canada. Can J Diet Pract Res. 2004;65:132-5, doi: 10.3148/65.3.2004.132.
- 14. Grunfeld C, Pang M, Doerrler W, Shigenaga JK, Jensen P, Feingold KR. Lipids, lipoproteins, triglyceride clearance, and cytokines in human immunodeficiency virus infection and the acquired immunodeficiency syndrome. J Clin Endocrinol Metab. 1992; 74:1045-52, doi: 10.1210/jc.74. 5.1045.
- 15. Almeida LB, Giudici KV, Jaime PC. Consumo alimentar e dislipidemia decorrente da terapia antiretroviral combinada para infecção pelo HIV: uma revisão sistemática. Arq Bras Endocrinol Metab. 2009;53:519-27.
- 16. Carosi G, Quiros-Roldan E, Torti C, Antinori A, Bevilacqua M, Bonadonna RC, et al. First Italian consensus statement on diagnosis, prevention and treatment of cardiovascular complications in HIVinfected patients in the HAART. Infectio. 2006;35:134-42, doi: 10.1007/s15010-007-6295-5.
- 17. Nerad J, Romeyn M, Silverman E, Allen-Reid J, Dieterich D, Merchant J, et al. General nutrition management in patients infected with human immunodeficiency virus. Clin Infec Dis. 2003;36:S52-62, doi: 10.1086/367559.
- 18. Fitch KV, Anderson EJ, Hubbard JL, Carpenter SJ, Waddell WR, Caliendo AM, et al. Effects of a lifestyle modification program in HIVinfected patients with the metabolic syndrome. AIDS. 2006;20:1843-50, doi: 10.1097/01.aids.0000244203.95758.db.
- 19. Tien PC, Cole SR, Williams CM, Li R, Justman JE, Cohen MH, et al. Incidence of lipoatrophy and lipohypertrophy in the women's interagency HIV study. J Acquir Immune Defic Syndr. 2003;34:461-6, doi: 10. 1097/00126334-200312150-00003.
- 20. Brown T, Wang Z, Chu H, Palella FJ, Kingsley L, Witt MD, et al. Longitudinal anthropometric changes in HIV-infected and HIV-uninfected men. J Acquir Immune Defic Syndr. 2006;43:356-62, doi: 10.1097/ 01.qai.0000243052.73321.8e.
- 21. Corcoran C, Anderson EJ, Burrows B, Stanley T, Walsh M, Poulos AM, et al. Comparison of total body potassium with other techniques for measuring lean body mass in men and women with AIDS wasting. Am J Clin Nutr. 2000;72:1053-8.
- 22. Schwenk A, Beisenherz A, Kremer G, Diehl V, Salzberger B, Fätkenheuer G. Bioelectrical impedance analysis in HIV-infected patients treated with triple antiretroviral treatment. Am J Clin Nutr. 1999; 70:867-73.
- 23. Henry K, Melroe H, Huebsch J. Atorvastatin and gemfibrozil for protease-inhibitor-related lipid abnormalities. Lancet. 1998; 352:1031-2, doi: 10.1016/S0140-6736(98)00022-1.
- 24. Loomba RS, Arora R. Fibrates:where are we now? Ther ADV Cardiovasc Dis. 2009;3:91, doi: 10.1177/1753944708096281.
- 25. Staels B, Dallongeville J, Auwerx J, Schoonjas K, Leitersdorf E, Fruchart JC. Mechanism of action of fibrates on lipid and lipoprotein metabolism. Circulation. 1998;98:2088-93.
- 26. Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, et al. Effects of long-term fenofibrate therapy on cardiovascular events. Lancet. 2005;366:1849-61, doi: 10.1016/S0140-6736(05)67667-2.
- 27. Samineni D, Fichtenbaum CJ. Fenofibrate in the treatment of dyslipidemia associated with HIV infection. Expert Opin Drug Metab Toxicol. 2010;6:995- 1004, doi: 10.1517/17425255.2010.504715.
- 28. Fields-Gardner C; Campa A. Position of the American Dietetics Association: Nutrition intervention and Human Immunodeficiency Virus Infection. J Am Diet Assoc. 2010;110:1105-19, doi: 10.1016/j.jada. 2010.05.020.
Publication Dates
-
Publication in this collection
29 Apr 2011 -
Date of issue
2011
History
-
Received
05 Nov 2010 -
Reviewed
05 Nov 2010 -
Accepted
17 Nov 2010