RAPID COMMUNICATION
Inflammation and circulating endothelial progenitor cells in patients with coronary artery disease and residual platelet reactivity
Antonio Eduardo P. PesaroI,II; Carlos V. Serrano JrII; Marcelo KatzI; Alexandre H. CamposI; Renato D. LopesIII,IV; Luciana C. MartiI; Herlon S. MartinsIV; Rodrigo S. SunaharaII; Raul C. MaranhãoII; José C. NicolauII
IAlbert Einstein Hospital, São Paulo/SP, Brazil
IIHospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, Heart Institute, São Paulo/SP, Brazil
IIIDuke University Medical Center, Duke Clinical Research Institute, Durham, NC, USA
IVFederal University of São Paulo, Paulista School of Medicine, São Paulo/SP, Brazil
VHospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo/SP, Brazil
INTRODUCTION
Atherosclerotic plaque development and progression are associated with vascular inflammation, endothelial dysfunction, and platelet activation (1). Inflammatory mediators, such as C-reactive protein (CRP) and oxidized low-density lipoprotein (oxLDL), can trigger platelet activation and subsequent thrombus formation (2). In turn, activated platelets secrete cytokines, recruit monocytes, and release soluble CD40 ligand (sCD40L), which mediate vascular inflammation (3). An important determinant of endothelial dysfunction in patients with coronary artery disease (CAD) is the reduced number of endothelial progenitor cells (EPCs) (4). Interestingly, EPCs can inhibit platelet activation, while activated platelets modulate EPC proliferation (5).
Aspirin is widely used in the prevention of complications related to CAD. However, the mechanisms that promote high residual platelet reactivity (RPR) in aspirin-treated patients are still under debate (6,7). Because inflammation and endothelial dysfunction may possibly contribute to platelet activation and RPR, we sought to compare inflammatory markers and EPC levels between stable CAD patients treated with aspirin with and without RPR.
METHODS
Study design. This was a substudy of a randomized trial testing lipid-lowering drugs that was performed from July 2006 to January 2009 in a single tertiary specialized cardiology hospital (ClinicalTrials.gov: NCT00474123). Details of the protocol have been published previously (8). In brief, all of the patients (n = 83) met the following inclusion criteria: angiographically documented CAD, simvastatin treatment, and age <80 years. The exclusion criteria were the following: myocardial infarction or revascularization <3 months, ventricular systolic dysfunction, warfarin treatment, malignancy, inflammatory diseases, and renal/liver dysfunction.
Of the original 83 patients, 63 were on aspirin treatment (100 mg/day), presented complete data for hsCRP, sCD40L, oxLDL, and circulating EPCs, and were included in the present study. No patients were treated with clopidogrel within the four weeks before enrollment. Platelet aggregation was measured by the platelet function analyzer (PFA)-100 closure time (CT). Patients with a CT <150 seconds (sec) were considered as having RPR (9).
We compared baseline characteristics, inflammatory levels, and EPC counts between patients with and without RPR. This study was approved by the institutional research committee. All of the subjects gave written informed consent.
Platelet aggregation using the PFA-100 assay. Samples were collected in 3.2% sodium citrate (buffered, pH 5.5, Vacutainer, Becton Dickinson, UK) for platelet function tests. Platelet function was measured with the PFA-100 (epinephrine) point-of-care assay (Dade-Behring, Deer field, IL, USA). We defined the upper normal limit for PFA-100 CT as 150 sec, in agreement with previous studies and the manufacturer's protocol recommendation (9).
hsCRP, sCD40L, and oxLDL. Serum hsCRP was assessed with a latex microparticle-enhanced immunoturbidimetric assay (BN II analyzer, Dade Behring, Deer field, IL, USA). The minimal detectable concentration of hsCRP was 0.2 mg/L. For the other markers, commercial ELISAs detecting sCD40L (R&D Systems, Minneapolis, MN, USA) and oxLDL (Mercodia, Winston Salem, NC, USA) were used. The detection limits of the ELISAs were as follows: sCD40L 15.6 pg/mL (intra-assay variability not available); oxLDL, 0.3 U/ L (intra-assay variability 6.1%).
Endothelial progenitor cells. The detection of EPCs was performed as previously described (10). In brief, 100 µL of mononuclear cells derived from peripheral blood was immunostained with monoclonal antibodies against human CD31/FITC, CD3/PE-Cy5, CD19/PE-Cy5, CD34/PE-Cy7, CD14/APC Cy-7 (BD Pharmingen, UK), VEGFR2/PE (R&D System, Minneapolis, MN, USA), and the appropriate isotype control antibodies (BD Pharmingen, UK). EPCs were negative for CD3, CD19, and CD14 and positive for CD31, CD34, and VEGFR2.
At least 70,000 events were acquired per tube by flow cytometry (FACSARIA, BD Biosciences, UK). The analysis was performed using FACSDIVA software (BD Biosciences, UK).
Statistical analysis. Continuous variables were expressed as the mean (+ standard deviation [SD]) or median (25th, 75 t h percentile). Differences were analyzed with a 2-sample t test when the distribution was normal; otherwise, we used the Mann-Whitney U test. The X2 test was used for categorical variables. A value of P<0.05 was considered significant. Analyses were performed using STATA/SE 9.2 (Stata Corp LP, USA). Spearman's rank test was performed to assess correlations.
RESULTS
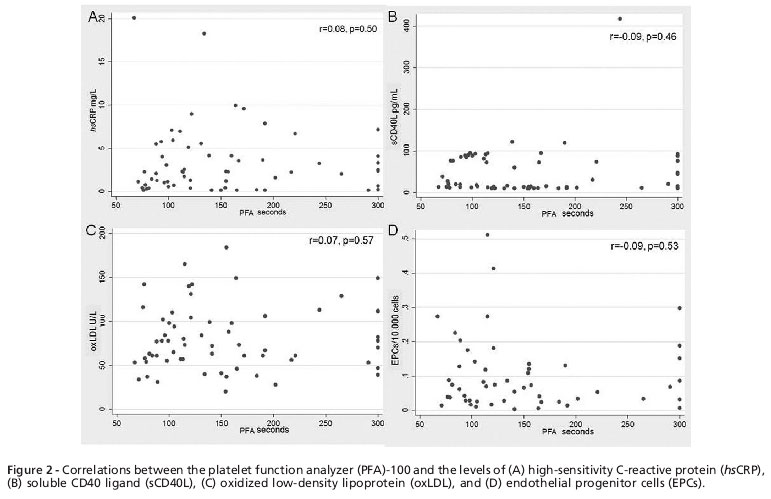
The baseline characteristics, including lipids and metabolic profiles, of the 63 patients are shown in Table 1. The mean (+ SD) age was 63 + 9 years. Forty patients (64%) were male, and 36 (57%) were classified as having RPR. The median (25th, 75th) PFA-100 CT was 202 (165, 300) sec in patients without RPR vs. 101 (86, 120) sec in patients with RPR (p<0.001). The median (25th, 75th) LDL cholesterol levels were similar and in the normal range in patients both without and with RPR (103 [89,117] vs. 99 [85,126] mg/dL, p= 0.99), as were triglycerides (118 [85,151] vs. 136 [92,163] mg/dL, p = 0.86) and hemoglobin Ale (5.9% [5.7%, 6.5%] vs. 6% [5.7%, 6.3%], p = 0.73).
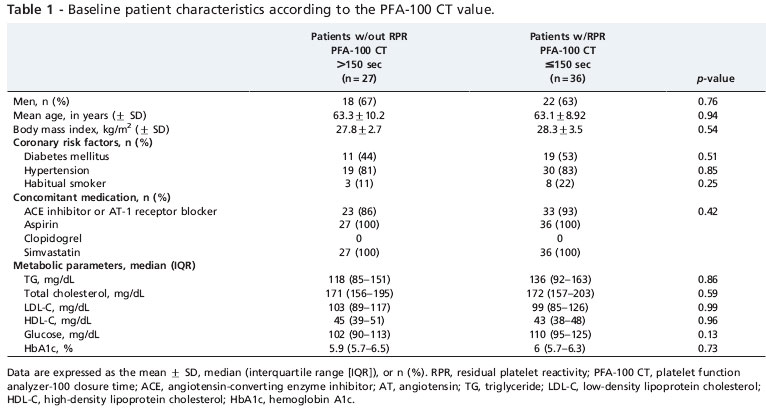
As demonstrated in Figure 1, mflammatory markers and the circulating levels of EPCs were similar in patients with and without RPR. mflammatory marker and EPC levels were not associated with RPR (sCD40L, hazard ratio [HR] 0.99, 95% confidence interval [CI] 0.99-1.0, p = 0.75; oxLDL, HR 1.0, 95% CI 0.99-1.02, p = 0.94; hsCRP, HR 1.02, 95% CI 0.89-1.17, p = 0.71; and EPCs, HR 1.03, 95% CI 0.97-1.1, p = 0.30). Additionally, no correlation was noted between PFA-100 and inflammatory markers or EPC values (Figure 2).
DISCUSSION
Our study did not identify an association between inflammatory markers or circulating EPCs and RPR in patients with stable CAD treated with low-dose aspirin. Additionally, no correlation was noted between PFA-100 and inflammatory markers or EPC values.
We evaluated inflammation by measuring the plasma levels of feCRP, oxLDL, and sCD40L which are biomarkers that have traditionally been correlated with atherosclerotic activity (11-13). Despite the previous use of aspirin, 57% of our patients presented with RPR. Previous studies have also reported a high RPR prevalence in patients treated with aspirin, but RPR may differ depending on the test applied (14,15). We performed a PFA-100, an assay with high sensitivity that is extensively used to identify RPR (15,16). Moreover, RPR detected by PFA-100 may identify patients with a higher cardiovascular risk (17).
We hypothesized that RPR could be related to inflammation and endothelial dysfunction. Our hypothesis was supported by several in vitro studies demonstrating inflammatory mechanisms activating platelets, which in turn increase atherothrombotic activity (18). OxLDL can activate platelets by acting on the scavenger receptor CD36 (19). Similarly, sCD40L can trigger platelet aggregation and is correlated with plasma P-selectin and urinary thromboxane levels (20,21). Activated platelets can induce the secretion of chemokines in various cells of the vascular wall (3). Platelet factor-4 attracts monocytes, promoting their differentiation into macrophages (22). In addition, CD40L expressed by activated platelets acts on endothelial cells, increasing the release of interleukin-8 and monocyte chemoattractant protein-1 (23).
In contrast, few clinical studies have investigated the association between inflammation or endothelial dysfunction and platelet hyper-aggregation. Dotsenko et al. have demonstrated a correlation between increased platelet aggregation and hsCKP (24). In patients with acute coronary syndromes, Gori et al. tested the association between several inflammatory markers and platelet aggregation and found an association only with IFN-gamma and IL-4 (25). Two small studies have demonstrated a correlation between sCD40L, CRP, and IL-8 and heightened thrombogenicity in patients undergoing coronary angioplasty (26,27). Conversely, in patients with stable CAD, a larger study did not find an association between circulating sCD40L levels and RPR (28).
In our study, the EPC levels did not differ between patients with and without RPR. We found EPC levels comparable to previous findings in patients with stable CAD (29). EPCs are reduced in CAD patients and are inhibited by atherosclerotic inflammatory agents, such as oxLDL and CRP (31,32). The relationship between EPCs and RPR has been poorly investigated. Daub et al. demonstrated that oxLDL-activated platelets may reduce EPC numbers (2). Alternatively, chemokine stromal cell factor-1, which is derived from activated platelets, may increase EPC levels (33). Finally, Abou-Saleh et al. showed that EPCs bind to and inhibit platelet activation via prostacyclin modulation (5).
Thus, despite previous in vitro evidence linking platelet activation to atherosclerotic inflammation, when we translated this assumption to human subjects, we did not find an association between inflammatory markers or circulating EPCs and RPR in patients with stable CAD treated with aspirin.
Study limitations
This was a subgroup analysis of a trial investigating lipid-lowering agents (8). The sample size and power were primarily estimated based on the main outcome of the original trial. However, our main results were corroborated by the absence of a correlation between PFA-100 CT and inflammatory markers or EPC values. Additionally, we used a single platelet function assay; it is possible that our results may have been different if a different platelet test had been used.
This investigation demonstrated no association between inflammatory markers or circulating EPCs and RPR in patients treated with aspirin. Thus, low-grade inflammation and endothelial dysfunction do not affect the responsiveness to aspirin in patients with stable CAD. Our findings highlight the importance of better understanding the underlying mechanism of RPR and the uncertainties inherent to this field of study.
AUTHOR CONTRIBUTIONS
Pesaro AE and Campos AH were responsible for study design, acquisition, analysis and interpretation of data, manuscript draft and approval of the manuscript final version.Serrano Jr CV and Nicolau JC were responsible for study design, analysis and interpretation of data, manuscript draft and approval of the manuscript final version. Katz M and Lopes RD were responsible for analysis and interpretation of data, manuscript draft and approval of the manuscript final version. Marti LC, Martins HS, Sunahara RS and Maranhão RC were responsible for acquisition, analysis and interpretation of data, review of the manuscript draft and approval of the manuscript final version.
REFERENCES
1. Libby P, Okamoto Y, Rocha VZ, Polco E. Inflammation in atherosclerosis: transition from theory to practice. Care J. 2010;74(2)213-20, http://dx.doi.org/10.1253/circj.QJ-09-0706.
2. Daub K, Seizer P, Stellos K, Krämer BP, Bigalke B, Schauer M, et al. Oxidized LDL-activated platelets induce vascular inflammation. Semin Thromb Hemost. 2010;36(2):146-56, http://dx.doi.org/10.1055/s-0030-1251498.
3. von Hundelshausen P, Petersen P, Brandt E. Platelet-derived chemokines in vascular biology. Thromb Haemost. 2007;97(5):704-13.
4. Hill JM, Zalos G, Halcox JP, Schenke WH, Wadawiw MA, Quyyumi AA, et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003;348(7):593-600, http://dx.doi.org/10.1056/NEJMoa022287.
5. Abou-Saleh H, Yacoub D, Théorét JP, Gillis MA, Neagoe PE, Labarthe B, et al. Endothelial progenitor cells bind and inhibit platelet function and thrombus formation. Circulation. 2009,120(22):2230-9, http://dx.doí.org/10.1161/CIRCULATIONAHA.109.894642.
6. Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR. Aspirin "resistance" and risk of cardiovascular morbidity: systematic review and meta-analysis. BMJ. 2008;336(7637):195-8.
7. Sanderson S, Emery J, Baglin T, Kinmonth AL. Narrative review: aspirin resistance and its clinical implications. Ann Intern Med. 2005;142(5):370-80.
8. Cavalcanti AB, Campos AH, Martins HS, Maranhão RC, et al. Pleiotropic effects of ezetimibe/simvastatin vs. high dose simvastatin. Int J Cardiol. 2011. [Epub ahead of print]
9. Böck M, De Haan J, Beck KH, Hertfelder HJ, Karger R, Heim MU, et al. Standardization of the PPA-IOO(R) platelet function test in 105 mmol/l buffered citrate: effect of gender, smoking and oral contraceptives. Br J Haematol. 1999;106(4):898-904, http://dx.doi.org/10.1046/j-1365-2141.1999.01660.x.
10. Yoder MC, Mead LE, Prater D, Krier TR, Mroueh KN, Li P, et al. Redefining endothelial progenitor cells via clonal analysis and hematopoietic stem/progenitor cell principals. Blood. 2007;109(5):1801-9, http://dx.doi.org/10.1182/blood-2006-08-043471.
11. Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002;347(20):1557-65, http://dx.doi.org/10.1056/NEJMoa021993.
12. Heeschen C, Dimmeler S, Hamm CW, van den Brand MJ, Boersma E, Zeiher AM, Simoons ML, et al. Soluble CD40 ligand in acute coronary syndromes. N Engl J Med. 2003,348(12) :1104-11, http://dx.doi.org/10.1056/NEJMoa022600.
13. Tsimikas S, Brilakis ES, Miller ER, McConnell JP, Lennon RJ, Komman KS, et al. Oxidized phospholipids, Lp(a) lipoprotein, and coronary artery disease. N Engl J Med. 2005;353(l):46-57, http://dx.doi.org/10.1056/NEJMoa043175.
14. Lordkipanidzé M, Pharand C, Schampaert E, Turgeon J, Palisaitis DA, Diodati JG. A comparison of six major platelet function tests to determine the prevalence of aspirin resistance in patients with stable coronary artery disease. Eur Heart J. 2007;28(14):1702-8, http://dx.doi.org/10.1093/eurheartj/ehm226.
15. Crescente M, Di Castelnuovo A, lacoviello L, Vermylen J, Cerletti C, de Gaetano G. Response variability to aspirin as assessed by the platelet function analyzer (PPA)-IOO. A systematic review. Thromb Haemost. 2008;99(l):14-26.
16. Mammen EP, Comp PC, Gosselin R, Greenberg C, Hoots WK, Kessler CM, et al. PFA-100 system: a new method for assessment of platelet dysfunction. Semin Thromb Hemost. 1998;24(2):195-202, http://dx.doi.org/10.1055/s-2007-995840.
17. Reny JL, De Moerloose P, Dauzat M, Fontana P. Use of the PFA-100 closure time to predict cardiovascular events in aspirin-treated cardiovascular patients: a systematic review and meta-analysis. J Thromb Haemost. 2008;6(3):444-50, http://dx.doi.org/10.1111/J.1538-7836.2008.02897.X.
18. Langer HF, Gawaz M. Platelet-vessel wall interactions in atherosclerotic disease. Thromb Haemost. 2008;99(3):480-6.
19. Relou IA, Hackeng CM, Akkerman JW, Malle E. Low-density lipoprotein and its effect on human blood platelets. Cell Mol Life Sei. 2003;60(5):961-971.
20. Prasad KS, Andre P, He M, Bao M, Manganello J, Phillips DR. Soluble CD40 ligand induces beta3 integrin tyrosine phosphorylation and triggers platelet activation by outside-in signaling. Proc Natl Acad Sei USA. 2003,100(21):12367-71, http://dx.doi.org/10.1073/pnas.2032886100.
21. Cipollone F, Mezzetti A, Porreca E, Di Febbo C, Nutini M, Fazia M, et al. Association between enhanced soluble CD40L and prothrombotic state in hypercholesterolemia: effects of statin therapy. Qrculation. 2002,106(4)399-402, http://dx.doi.org/10.1161/01.CIR.0000025419.95769F0.
22. Scheuerer B, Ernst M, Dürrbaum-Landmann I, Fleischer J, Grage-Griebenow E, Brandt E, et al. The CXC-chemokine platelet factor 4 promotes monocyte survival and induces monocyte differentiation into macrophages. Blood. 2000;95(4):1158-66.
23. Lutgens E, Lievens D, Beckers L, Donners M, Daemen M. CD-40 and its ligand in atherosclerosis. Trends Cardiovasc Med. 2007;17(4):118-23, http://dx.doi.org/10.1016/j.tcm.2007.02.004.
24. Dotsenko O, Chaturvedi N, Thorn SA, Wright AR, Mayet J, Shore A, et al. Platelet and leukocyte activation, atherosclerosis and inflammation in European and South Asian men. J Thromb Haemost. 2007;5(10):2036-42, http://dx.doi.org/10.1111/j.1538-7836.2007.02711.x.
25. Gori AM, Cesari P, Marcucci R, Giusti B, Paniccia R, Antonucci E, et al. The balance between pro- and anti-inflammatory cytokines is associated with platelet aggregability in acute coronary syndrome patients. Atherosclerosis. 2009,202(1):255-62, http://dx.doi.org/10.1016/j.atherosclerosis.2008.04.001.
26. Obradovic SD, Antovic JP, Antonijevic NM, Ratkovic NG, Vojvodic DV, Subota VS, et al. Elevations in soluble CD40 ligand in patients with high platelet aggregability undergoing percutaneous coronary intervention. Blood coagulation & fibrinolysis: an international journal in haemostasis and thrombosis. 2009;20(4):283-9, http://dx.doi.org/10.1097/MBC.0b013e328329f28c.
27. Gurbel PA, Bliden KP, Kreutz RP, Dichiara J, Antonino Ml, Tantry US. The link between heightened fhrombogenicity and inflammation: pre-procedure characterization of the patient at high risk for recurrent events after stenting. Platelets. 2009;(2):97-104, http://dx.doi.org/10.1080/09537100802687666.
28. Pamukcu B, Oflaz H, Onur I, Midilli K, Yilmaz G, Yilmaz E, et al. Relationship between the serum sCD40L level and aspirin-resistant platelet aggregation in patients with stable coronary artery disease. Circ J. 2008;72(l):61-6, http://dx.doi.org/10.1253/circj.72.61.
29. Schmidt-Lucke C, Rossig L, Fichtischerer S, Vasa M, Britten M, Kamper U, et al. Reduced number of circulating endothelial progenitor cells predicts future cardiovascular events: proof of concept for the clinical importance of endogenous vascular repair. Circulation. 2005;111(22)2981-7, http://dx.doi.org/10.1161/CIRCULATIONAHA.104.504340.
30. Hristov M, Erl W, Weber PC. Endothelial progenitor cells: mobilization, differentiation, and homing. Arteriosclerosis, thrombosis, and vascular biology. 2003;23(7):1185-9, http://dx.doi.org/10.1161/01.ATV.0000073832.49290.B5.
31. Imanishi T, Hano T, Sawamura T, Nishio I. Oxidized low-density lipoprotein induces endothelial progenitor cell senescence, leading to cellular dysfunction. Clinical and experimental pharmacology & physiology. 2004;31(7):407-13, http://dx.doi.org/10.1111/J.1440-1681.2004.04022.X.
32. Werner N, Kosiol S, Schiegl T, Ahlers P, Walenta K, Link A, et al. Circulating endothelial progenitor cells and cardiovascular outcomes. The New England journal of medicine. 2005;353(10):999-1007, http://dx.doi.org/10.1056/NEJMoa043814.
33. Stellos K, Seizer P, Bigalke B, Daub K, Geisler T, Gawaz M. Platelet aggregates-induced human CD34+ progenitor cell proliferation and differentiation to macrophages and foam cells is mediated by stromal cell derived factor 1 in vitro. Semin Thromb Hemost. 2010;36(2):139-45, http://dx.doi.org/10.1055/s-0030-1251497.
No potential conflict of interest was reported.
Funding: This work was supported by public grants from the São Paulo Research Foundation (FAPESP/05/57710-3). No industry support was provided for this study.
Email: antonioepp@einstein.br
Tel.: 55 11 2151-5408
- 1. Libby P, Okamoto Y, Rocha VZ, Polco E. Inflammation in atherosclerosis: transition from theory to practice. Care J. 2010;74(2)213-20, http://dx.doi.org/10.1253/circj.QJ-09-0706
- 2. Daub K, Seizer P, Stellos K, Krämer BP, Bigalke B, Schauer M, et al. Oxidized LDL-activated platelets induce vascular inflammation. Semin Thromb Hemost. 2010;36(2):146-56, http://dx.doi.org/10.1055/s-0030-1251498
- 3. von Hundelshausen P, Petersen P, Brandt E. Platelet-derived chemokines in vascular biology. Thromb Haemost. 2007;97(5):704-13.
- 4. Hill JM, Zalos G, Halcox JP, Schenke WH, Wadawiw MA, Quyyumi AA, et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003;348(7):593-600, http://dx.doi.org/10.1056/NEJMoa022287
- 5. Abou-Saleh H, Yacoub D, Théorét JP, Gillis MA, Neagoe PE, Labarthe B, et al. Endothelial progenitor cells bind and inhibit platelet function and thrombus formation. Circulation. 2009,120(22):2230-9, http://dx.doí.org/10.1161/CIRCULATIONAHA.109.894642
- 6. Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR. Aspirin "resistance" and risk of cardiovascular morbidity: systematic review and meta-analysis. BMJ. 2008;336(7637):195-8.
- 7. Sanderson S, Emery J, Baglin T, Kinmonth AL. Narrative review: aspirin resistance and its clinical implications. Ann Intern Med. 2005;142(5):370-80.
- 8. Cavalcanti AB, Campos AH, Martins HS, Maranhão RC, et al. Pleiotropic effects of ezetimibe/simvastatin vs. high dose simvastatin. Int J Cardiol. 2011. [Epub ahead of print]
- 9. Böck M, De Haan J, Beck KH, Hertfelder HJ, Karger R, Heim MU, et al. Standardization of the PPA-IOO(R) platelet function test in 105 mmol/l buffered citrate: effect of gender, smoking and oral contraceptives. Br J Haematol. 1999;106(4):898-904, http://dx.doi.org/10.1046/j-1365-2141.1999.01660.x
- 10. Yoder MC, Mead LE, Prater D, Krier TR, Mroueh KN, Li P, et al. Redefining endothelial progenitor cells via clonal analysis and hematopoietic stem/progenitor cell principals. Blood. 2007;109(5):1801-9, http://dx.doi.org/10.1182/blood-2006-08-043471
- 11. Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002;347(20):1557-65, http://dx.doi.org/10.1056/NEJMoa021993
- 12. Heeschen C, Dimmeler S, Hamm CW, van den Brand MJ, Boersma E, Zeiher AM, Simoons ML, et al. Soluble CD40 ligand in acute coronary syndromes. N Engl J Med. 2003,348(12) :1104-11, http://dx.doi.org/10.1056/NEJMoa022600
- 13. Tsimikas S, Brilakis ES, Miller ER, McConnell JP, Lennon RJ, Komman KS, et al. Oxidized phospholipids, Lp(a) lipoprotein, and coronary artery disease. N Engl J Med. 2005;353(l):46-57, http://dx.doi.org/10.1056/NEJMoa043175
- 15. Crescente M, Di Castelnuovo A, lacoviello L, Vermylen J, Cerletti C, de Gaetano G. Response variability to aspirin as assessed by the platelet function analyzer (PPA)-IOO. A systematic review. Thromb Haemost. 2008;99(l):14-26.
- 16. Mammen EP, Comp PC, Gosselin R, Greenberg C, Hoots WK, Kessler CM, et al. PFA-100 system: a new method for assessment of platelet dysfunction. Semin Thromb Hemost. 1998;24(2):195-202, http://dx.doi.org/10.1055/s-2007-995840
- 17. Reny JL, De Moerloose P, Dauzat M, Fontana P. Use of the PFA-100 closure time to predict cardiovascular events in aspirin-treated cardiovascular patients: a systematic review and meta-analysis. J Thromb Haemost. 2008;6(3):444-50, http://dx.doi.org/10.1111/J.1538-7836.2008.02897.X
- 18. Langer HF, Gawaz M. Platelet-vessel wall interactions in atherosclerotic disease. Thromb Haemost. 2008;99(3):480-6.
- 19. Relou IA, Hackeng CM, Akkerman JW, Malle E. Low-density lipoprotein and its effect on human blood platelets. Cell Mol Life Sei. 2003;60(5):961-971.
- 20. Prasad KS, Andre P, He M, Bao M, Manganello J, Phillips DR. Soluble CD40 ligand induces beta3 integrin tyrosine phosphorylation and triggers platelet activation by outside-in signaling. Proc Natl Acad Sei USA. 2003,100(21):12367-71, http://dx.doi.org/10.1073/pnas.2032886100
- 21. Cipollone F, Mezzetti A, Porreca E, Di Febbo C, Nutini M, Fazia M, et al. Association between enhanced soluble CD40L and prothrombotic state in hypercholesterolemia: effects of statin therapy. Qrculation. 2002,106(4)399-402, http://dx.doi.org/10.1161/01.CIR.0000025419.95769F0
- 22. Scheuerer B, Ernst M, Dürrbaum-Landmann I, Fleischer J, Grage-Griebenow E, Brandt E, et al. The CXC-chemokine platelet factor 4 promotes monocyte survival and induces monocyte differentiation into macrophages. Blood. 2000;95(4):1158-66.
- 23. Lutgens E, Lievens D, Beckers L, Donners M, Daemen M. CD-40 and its ligand in atherosclerosis. Trends Cardiovasc Med. 2007;17(4):118-23, http://dx.doi.org/10.1016/j.tcm.2007.02.004
- 24. Dotsenko O, Chaturvedi N, Thorn SA, Wright AR, Mayet J, Shore A, et al. Platelet and leukocyte activation, atherosclerosis and inflammation in European and South Asian men. J Thromb Haemost. 2007;5(10):2036-42, http://dx.doi.org/10.1111/j.1538-7836.2007.02711.x
- 25. Gori AM, Cesari P, Marcucci R, Giusti B, Paniccia R, Antonucci E, et al. The balance between pro- and anti-inflammatory cytokines is associated with platelet aggregability in acute coronary syndrome patients. Atherosclerosis. 2009,202(1):255-62, http://dx.doi.org/10.1016/j.atherosclerosis.2008.04.001
- 26. Obradovic SD, Antovic JP, Antonijevic NM, Ratkovic NG, Vojvodic DV, Subota VS, et al. Elevations in soluble CD40 ligand in patients with high platelet aggregability undergoing percutaneous coronary intervention. Blood coagulation & fibrinolysis: an international journal in haemostasis and thrombosis. 2009;20(4):283-9, http://dx.doi.org/10.1097/MBC.0b013e328329f28c
- 27. Gurbel PA, Bliden KP, Kreutz RP, Dichiara J, Antonino Ml, Tantry US. The link between heightened fhrombogenicity and inflammation: pre-procedure characterization of the patient at high risk for recurrent events after stenting. Platelets. 2009;(2):97-104, http://dx.doi.org/10.1080/09537100802687666
- 28. Pamukcu B, Oflaz H, Onur I, Midilli K, Yilmaz G, Yilmaz E, et al. Relationship between the serum sCD40L level and aspirin-resistant platelet aggregation in patients with stable coronary artery disease. Circ J. 2008;72(l):61-6, http://dx.doi.org/10.1253/circj.72.61
- 29. Schmidt-Lucke C, Rossig L, Fichtischerer S, Vasa M, Britten M, Kamper U, et al. Reduced number of circulating endothelial progenitor cells predicts future cardiovascular events: proof of concept for the clinical importance of endogenous vascular repair. Circulation. 2005;111(22)2981-7, http://dx.doi.org/10.1161/CIRCULATIONAHA.104.504340
- 30. Hristov M, Erl W, Weber PC. Endothelial progenitor cells: mobilization, differentiation, and homing. Arteriosclerosis, thrombosis, and vascular biology. 2003;23(7):1185-9, http://dx.doi.org/10.1161/01.ATV.0000073832.49290.B5
- 31. Imanishi T, Hano T, Sawamura T, Nishio I. Oxidized low-density lipoprotein induces endothelial progenitor cell senescence, leading to cellular dysfunction. Clinical and experimental pharmacology & physiology. 2004;31(7):407-13, http://dx.doi.org/10.1111/J.1440-1681.2004.04022.X
- 32. Werner N, Kosiol S, Schiegl T, Ahlers P, Walenta K, Link A, et al. Circulating endothelial progenitor cells and cardiovascular outcomes. The New England journal of medicine. 2005;353(10):999-1007, http://dx.doi.org/10.1056/NEJMoa043814
- 33. Stellos K, Seizer P, Bigalke B, Daub K, Geisler T, Gawaz M. Platelet aggregates-induced human CD34+ progenitor cell proliferation and differentiation to macrophages and foam cells is mediated by stromal cell derived factor 1 in vitro. Semin Thromb Hemost. 2010;36(2):139-45, http://dx.doi.org/10.1055/s-0030-1251497
Publication Dates
-
Publication in this collection
24 Sept 2012 -
Date of issue
Sept 2012