Abstract
OBJECTIVE: To evaluate the effectiveness of the Brazilian Cardioprotective Diet Program in reducing blood pressures, fasting glucose levels and body mass indices in patients with established atherothrombotic disease. METHOD: This randomized controlled pilot trial included outpatients who were over 45 years of age with atherothrombotic cardiovascular disease. Group A, who received the Brazilian Cardioprotective Diet Program, had weekly sessions with dietitians. Groups B and C received the usual dietary therapy that is given to patients with cardiovascular diseases as proposed by the Brazilian guidelines. This diet had the same nutrient profile as that given to Group A, but it was customized by the integration of typical Mediterranean foods. The difference between Groups B and C was the number of sessions with the dietitian. Group B received weekly sessions, while group C only had monthly sessions. ClinicalTrials.gov: NCT 01453166. RESULTS: There was a greater reduction in systolic (7.8%) and diastolic (10.8%) blood pressures in Group A compared with Group B (2.3% and 7.3%), and Group C (3.9% and 4.9%, respectively). Fasting glucose decreased by 5.3% and 2% in Groups A and B, respectively. Fasting glucose increased by 3.7% in Group C. The BMIs decreased by 3.5% and 3.3% in Groups A and B, respectively. Group C did not present with any changes in BMI. However, none of these data showed statistical differences between the groups, which is methodologically acceptable in pilot trials. CONCLUSIONS: The Brazilian Cardioprotective Diet Program seems to be more effective in reducing blood pressures, fasting glucose levels, weights and BMIs in patients with previous cardiovascular disease compared with the diet that has been proposed by the Brazilian guidelines.
Diet; Cardiovascular Diseases; Risk factors; Prevention
CLINICAL SCIENCE
Effects of Brazilian Cardioprotective Diet Program on risk factors in patients with coronary heart disease: a Brazilian Cardioprotective Diet randomized pilot trial
Bernardete Weber; Andrea Polo Galante; Angela Cristine Bersch-Ferreira; Camila Ragne Torreglosa; Vitor Oliveira Carvalho; Elivane da Silva Victor; Jose Amalth do Espírito-Santo; Maria Beatriz Ross-Fernandes; Rafael Marques Soares; Rosana Perim Costa; Enilda de Sousa Lara; Anna Maria Buehler; Otávio Berwanger
Hospital do Coração (IEP-HCor), Research Institute, São Paulo/SP, Brazil
ABSTRACT
OBJECTIVE: To evaluate the effectiveness of the Brazilian Cardioprotective Diet Program in reducing blood pressures, fasting glucose levels and body mass indices in patients with established atherothrombotic disease.
METHOD: This randomized controlled pilot trial included outpatients who were over 45 years of age with atherothrombotic cardiovascular disease. Group A, who received the Brazilian Cardioprotective Diet Program, had weekly sessions with dietitians. Groups B and C received the usual dietary therapy that is given to patients with cardiovascular diseases as proposed by the Brazilian guidelines. This diet had the same nutrient profile as that given to Group A, but it was customized by the integration of typical Mediterranean foods. The difference between Groups B and C was the number of sessions with the dietitian. Group B received weekly sessions, while group C only had monthly sessions. ClinicalTrials.gov: NCT 01453166.
RESULTS: There was a greater reduction in systolic (7.8%) and diastolic (10.8%) blood pressures in Group A compared with Group B (2.3% and 7.3%), and Group C (3.9% and 4.9%, respectively). Fasting glucose decreased by 5.3% and 2% in Groups A and B, respectively. Fasting glucose increased by 3.7% in Group C. The BMIs decreased by 3.5% and 3.3% in Groups A and B, respectively. Group C did not present with any changes in BMI. However, none of these data showed statistical differences between the groups, which is methodologically acceptable in pilot trials.
CONCLUSIONS: The Brazilian Cardioprotective Diet Program seems to be more effective in reducing blood pressures, fasting glucose levels, weights and BMIs in patients with previous cardiovascular disease compared with the diet that has been proposed by the Brazilian guidelines.
Keywords: Diet; Cardiovascular Diseases; Risk factors; Prevention.
INTRODUCTION
Cardiovascular diseases (CVD) represent the leading causes of mortality and morbidity in developed countries worldwi de, including Brazil (1). The control of cardiovascular risk factors plays an important role in patients' quality of life and survival rates. The World Health Organization has stated that over three-quarters of all CVD deaths may be avoided with adequate changes in lifestyle, including diet and exercise (2-3).
It is a consensus that the Mediterranean diet is effective and possibly the most appropriate dietary intervention for the prevention and treatment of CVD (2,3,4,5,6). This diet is characterized by a low saturated fat intake in addition to a high consumption of vegetables, fish, and olive oil and a moderate consumption of wine (5). Nevertheless, adherence to this diet seems to be an obstacle in successfully controlling cardiovascular risk factors. Thus, cultural adaptation seems to be the most appropriate means for its management in countries outside of the Mediterranean region (6). In Brazil, the Mediterranean diet differs vastly from local customs, and this factor is seemingly related to low adherence to the diet (7).
Brazil is a developing country with a wide range of cultures and important socio-economic limitations. Additionally, significantly increased mortality and morbidity from CVD have been observed, which compromises the government's finances. Brazil also possesses a rich variety of natural and nutritional resources that are potentially beneficial in the treatment of CVD (8,9). Nevertheless, no studies have explored the putative benefits of food resources that are part of the Brazilian culture in comparison with the standard diet that has been proposed by the Brazilian guidelines in the prevention and treatment of cardiovascular diseases.
The aim of this randomized pilot trial was to evaluate the Brazilian Cardioprotective Diet Program (a Brazilian version of an accessible dietary therapy for cardiovascular diseases) in reducing blood pressures, fasting glucose levels, and body mass indices (BMIs) in patients with established atherothrombotic disease.
METHODS
Trial design
We conducted a randomized (concealed) controlled pilot trial to evaluate the effects of the Brazilian Cardioprotective Diet Program on blood pressures, BMIs, and fasting glucose levels in patients with established atherothrombotic disease. The trial was designed by the Steering Committee and registered at Clinicaltrials.gov (NCT01453166). The study protocol was approved by the ethics committee of our institution. All patients provided informed consent prior to participation.
Study population
We included outpatients who were over 45 years of age with established or previous atherothrombotic CVD occurring in the past 10 years and who were at high CVD risk. Atherothrombotic CVD was defined as follows: coronary heart disease (stable or unstable angina pectoris, a history of myocardial infarction or acute coronary syndrome, a prior coronary revascularization procedure, a history of abdominal segmental wall motion as shown by cardiac echocardiography or a fixed segmental defect in the radionuclide imaging test), ischemic cerebrovascular disease (ischemic stroke or transient ischemic attack), or peripheral vascular disease (prior peripheral revascularization procedure or amputation due to vascular disease).
The patients also had at least one of the following risk factors: diabetes mellitus (serum glucose >100 mg/dl), hypertension (systolic blood pressure >130mm Hg or diastolic blood pressure >85 mm Hg), smoking, dyslipidemia (low density lipoprotein (LDL) >160 mg/dL, triglycerides >150 mg/dL, or total cholesterol (CT) >200 mg/dL), family coronary artery disease history, asymptomatic carotid disease or BMI >25 kg/m2 for adults and >28 kg/ m2 for seniors.
We excluded patients with neurocognitive or psychiatric conditions (as defined by the clinical trial investigators), pregnant or lactating women, patients with hepatic impairment or renal insufficiency, and patients with a life expectancy of less than six months (e.g., those with metastatic malignancies).
Randomization and Allocation Concealment
After providing written informed consent, the patients were randomized in a 1:1:1 ratio to receive one of three dietary interventions (A, B, or C). The allocation concealment was guaranteed by using sealed and opaque envelopes that were numbered sequentially. The patients who were allocated to Group A joined the Brazilian Cardioprotective Diet Program, which involves a Brazilian version of an accessible dietary therapy for cardiovascular diseases and weekly counseling with dieticians. The patients in Group B received the dietary therapy that was proposed by the Brazilian guidelines for cardiovascular diseases and also attended weekly counseling sessions with dietitians. Group C received the same dietary intervention as Group B, but the patients were counseled monthly.
Study interventions
The nutrient profiles of the diets were based on the Brazilian guidelines for cardiovascular disease treatment (10,11,12). The diets contained 50-60% of energy from carbohydrates, 15% from proteins, and 25-35% from fats. In addition, 20-30 g/d of fiber and 2,000 mg/d of sodium were recommended. The concentrations of saturated, monounsaturated, and polyunsaturated fatty acids were <7%, <20%, and <10%, respectively. The total dietary energy intake was adjusted only for patients with a baseline BMI >25 kg/m2.
The main difference between the Brazilian Cardioprotective Diet Program, which involves a Brazilian version of an accessible dietary therapy for cardiovascular diseases, and the usual dietary therapy that is prescribed for cardiovascular diseases was the consideration of energy density. The Brazilian Cardioprotective Diet Program helped the patients to avoid high energy density foods (>1 kcal/g), thus allowing them to eat more and consume fewer calories. As they made the right food choices, they felt less restricted, aiding in the improvement of adherence.
In general, the Brazilian Cardioprotective Diet Program features nutritional recommendations that are feasible for the Brazilian population. Accordingly, the diet composition allows for the easy access and full use of foods, in addition to the prioritization of regional foods that are culturally accepted by the patients (rice, bean, soy oil, and Brazilian fruits and vegetables).
Group A participated in the Brazilian Cardioprotective Diet Program. This group attended weekly session with dietitians. These were conducted in person, by phone or in a gourmet shop. During attendance at the gourmet shop, the patients received tips for eating in restaurants, instructions on label reading and a list of typical Brazilian recipes that were adjusted for nutrients and energy densities. This nutritional prescription protocol was developed by dietitians from our hospital.
Groups B and C received the usual dietary therapy that is prescribed to patients with cardiovascular diseases as proposed by the Brazilian guidelines. This diet had the same nutrient profile as that which was presented in Group A but was customized by the integration of typical Mediterranean foods (e.g., olives, olive oil, chestnuts, walnuts, almonds, hazelnuts, peanuts, and cold water fish). The difference between groups B and C was the number of sessions with the dietitian. Group B received weekly sessions that were conducted in person or by telephone, and Group C had monthly sessions that were conducted in person.
Anthropometric measurements and 24-h dietary recalls were performed by well-trained dietitians. The patients described their average portion sizes for food items in terms of household measurements, the standard weights of food items and validated food portion photographs of known weights. The Nutriquanti diet system (São Paulo, SP, Brazil) (13), which is an online computer program that is based on the Brazilian food database, was used to calculate the Brazilian Cardioprotective Diet Program and dietary assessments. Data quality control was guaranteed by weekly meetings between the investigators and dieticians.
Study procedures
Anthropometric measurements and laboratory tests were performed at baseline and after 6 and 12 weeks. At each contact with the dietitian (weekly or monthly), the dietary intake profile was assessed by a 24-hour dietary recall. The first nutritional session lasted for 60 minutes. The follow-up counseling sessions lasted for 30 minutes once the teaching and nutrition goals were reviewed. The phone interviews lasted approximately 15 minutes and included just the time that was necessary to assess the 24-hour dietary recall.
Outcomes
The primary outcome of this pilot trial was the changes in blood pressures that occurred after 12 weeks of adherence to the Cardioprotective Diet Program. The secondary outcomes of this pilot trial were improved BMIs and fasting glucose levels. Considering that this was a pilot trial, we chose one well-established biochemical, hemodynamic, and anthropometric parameter as the endpoint.
Biochemical analysis
The blood samples were collected and handled according to hospital routines. Fasting glucose was determined by an enzymatic colorimetric dry chemistry method (Ortho-Clinical Diagnostics VITROS 5.1) at the Center for Laboratory Medicine at the Hospital do Coração.
Blood pressures and weights
Blood pressures were assessed by an auscultatory method following the recommendations of the American Heart Association (14). The patients were seated comfortably with their backs supported, and their upper arms were free of constrictive clothing. Arms were supported at heart level, and the mercury columns were deflated at 2-3 mm/sec. The first and last audible sounds were recorded as the systolic and diastolic pressures, respectively. Two readings were performed at intervals of at least 1 minute, and the average was taken as the patient's blood pressure. If there was a difference of greater than 5 mm Hg between the first and second readings, additional (one or two) readings were obtained, and the average of these multiple readings was used (17).
To assess the weights, we used a digital scale with a maximum capacity of 150 kg. The patients dressed in as little clothing as possible and removed objects that could interfere with measurements. Heights were measured using a stadiometer with a bilateral scale from 35 to 213 cm and a resolution of 0.1 cm. BMIs were calculated by dividing the patients' current weights by the square of their heights in meters and classified according to WHO recommendations (15).
Sample size
Considering this pilot trial, the sample size was set to compare the groups in relation to changes in the systolic and diastolic blood pressures following dietary intervention. We anticipated a standard deviation of 14 mm Hg in the systolic or diastolic blood pressures. To detect a difference of 7 mm Hg in the systolic and diastolic blood pressures with 80% statistical power and a two-tailed p-value of 5%, we sought to include 50 patients in each of the three groups.
Statistical analyses
All analyses followed the ''intention to treat'' principle. To evaluate the effects of the diet interventions, we used an analysis of variance (ANOVA). In cases of significant group effects, we used multiple comparisons with Bonferroni corrections to locate the differences. All tests were performed with the SPSS statistical software or STATA SE 11 for Windows (College Station, USA). Statistical significance was defined as p<0.05.
Quality Control
Due to the type of intervention in this pilot trial, it was not possible to blind the investigators and participants. To improve quality control, the laboratory technicians who performed the biochemical tests were not aware of which group the patients had been allocated to. Data quality control was guaranteed by weekly contacts with investigators, and general feedback was provided at investigators' meetings.
Moreover, two independent investigators evaluated the database, and anthropometric measurements were performed twice to ensure the reliability of the data.
RESULTS
Baseline Characteristics
This trial enrolled 117 patients from September to December 2011 in a cardiology hospital (Figure 1). The baseline characteristics, such as the medication intakes, were similar between the groups (Table 1). More than 70% of the patients presented with histories of hypertension and/or dyslipidemia in addition to reporting the frequent use of antihypertensive and hypolipidemic drugs. The baseline characteristics were well balanced between the groups, except in the case of asymptomatic carotid disease.
Participation in all visits, phone calls and contact with the dietitians was evaluated in Groups A and B due to the similarities in the number of contacts (weekly sessions, which in Group C were monthly sessions). The attendance of patients in Group A at the meetings with the dieticians was higher than that in Group B (88.1% versus 78%, respectively).
The analyses of the dietary recalls that were collected during the intervention period show that the caloric intakes decreased between the initial and final assessments in a similar manner in all three groups. The consumption of total cholesterol, saturated fatty acids, and sodium also decreased (Table 2). The ingestion of all nutrients showed lower variabilities following the intervention period, indicating greater homogeneity in consumption.
Effects on risk factors
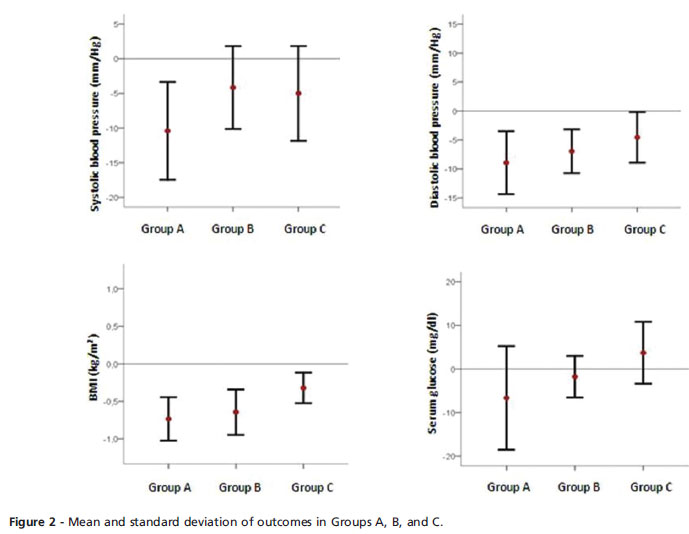
Considering our primary outcome, there was a greater reduction in the systolic (7.8%) and diastolic (10.8%) blood pressures in Group A compared with Groups B (2.3% and 7.3%) and C (3.9% and 4.9%, respectively). Considering our secondary outcome, the fasting glucose levels decreased by 5.3% and 2% in Groups A and B, respectively. In Group C, they increased by 3.7%. The BMIs decreased by 3.5% and 3.3% in Groups A and B, respectively. The BMIs in Group C did not change (Figure 2). Nevertheless, none of these data showed statistical differences between the groups, which is methodologically acceptable in pilot trials (Table 3).
DISCUSSION
This is the first study to investigate the clinical effects of a diet that is based on widely available foods in the Brazilian culture on cardiovascular risk factors. The main finding of this randomized pilot trial was that Group A, who received the Brazilian Cardioprotective Diet Program, showed greater decreases in blood pressures, serum glucose levels, and BMIs compared with Groups B and C, who received the dietary therapy that has been proposed by the Brazilian guidelines for CVD.
Among the various dietary interventions, there is a consensus that the Mediterranean diet is effective and possibly more appropriate for the prevention and treatment of CVD (2,7). This diet is characterized by the low intake of saturated fat, high consumption of vegetables, fish, olive oil, and moderate consumption of wine (8). Despite the remarkable effects of the Mediterranean diet, there is some controversy regarding its administration in countries outside of the Mediterranean region.
The Lyon Diet Heart Study showed no differences between patients that followed the Mediterranean diet and those that followed common eating habits in the secondary prevention of CAD. This study investigated the total cholesterol levels (650 vs. 617 mmol/l; p>0.05), LDLs (452 vs. 418 mmol/l; p>0.05), HDLs (116 vs. 128 mmol/l; p>0.05), triglycerides (215 vs. 185 mmol/l; p>0.05), weights (74.2 vs. 75.6 kg; p>0.05), and systolic (119 vs. 126 mm Hg; p>0.05) and diastolic (74 vs. 78 mm Hg; p>0.05) blood pressures of patients during a period of three years of follow-up (16). Our pilot study, which was conducted during a brief 12-week period, showed a trend of decreasing blood pressures, BMIs, and fasting plasma glucose levels; these factors were not evaluated in the Lyon study. Moreover, the only Brazilian study that evaluated the influence of the Mediterranean diet in secondary prevention showed no differences in BMIs, systolic or diastolic blood pressures, or fasting glucose levels (10).
However, studies that have adapted the Mediterranean diet to the tastes and cultural habits of the local population observed greater effectiveness in reducing cardiovascular risk factors. An Indian study showed that after one year of dietary intervention, blood glucose levels decreased by 1.36 mmol/l, systolic blood pressures decreased by 13.4 mm Hg, and diastolic blood pressures decreased by 9.3 mm Hg (17). A Swedish study (NORDIET) that also adapted the Mediterranean dietary habits for patients in the primary prevention program observed reductions in systolic blood pressures by 9.5 mm Hg and weights by 14.4 kg (18).
In our pilot study, the Brazilian Cardioprotective Diet Program seemed to be more efficient than the diet intervention that was proposed by the Brazilian guidelines. We believe that a cardioprotective diet including foods that are widely available in Brazil played a key role in our results. Our findings are of potentially great importance to public health in our country, considering the promising cost/benefit relationship (19,20,21). The financial costs of the foods were not assessed in this pilot study; however, the diet that was proposed by the Brazilian guidelines to control cardiovascular risk factors, which involves components of the Mediterranean diet, is costly for a major proportion of the Brazilian population. Thus, we propose a new intervention with potentially low costs and high feasibility in Brazil. The efficacy of the Brazilian Cardioprotective Diet Program is substantiated by the fact that the diet that has been proposed by the Brazilian guidelines is not widely available nor is it in accordance with the Brazilian culture.
Despite our encouraging results, we cannot generalize and recommend the implementation of a cardioprotective diet following the same format as in this pilot study in all Brazilian regions. Our country has continental dimensions and presents with multicultural characteristics that should be considered when interpreting our data and prescribing diets. For the improvement of cardioprotective diets and to contemplate the cultural diversities of the various regions of our country, a multicenter trial is needed. However, the foundation for the Brazilian Cardioprotective Diet has been established.
Study limitations
This study had some limitations; we did not assess the patients' dietary adherences, we only assessed their adherences to the intervention programs. Nevertheless, we observed that the numbers of absences were higher in Group B than in Group A, which was the group following the Brazilian Cardioprotective Diet Program. Our randomization process did not include a web-based automated randomization system, which could represent a methodological disadvantage. Moreover, this study did not find statistically significant differences between groups, which is acceptable in pilot trials. We believe that the statistical significance will be evident when the Brazilian Cardioprotective Diet Program is assessed in a larger population over all regions of Brazil.
The Brazilian Cardioprotective Diet Program seems to be more effective in reducing blood pressures, fasting glucose levels, weights, and BMIs in patients with previous cardiovascular diseases compared with the diet that was proposed by the Brazilian guidelines. The Brazilian Cardioprotective Diet Program can be considered as an alternative for Brazilian patients with cardiovascular risk factors; however, it will be necessary to test this intervention on a larger scale.
ACKNOWLEDGMENTS
The Brazilian Cardioprotective Diet Trial is funded by the Brazilian Ministry of Health (Programa Hospitais de Excelencia a Serviço do SUS). The sponsor had no role in the analyses, study design or decision to publish these results.
AUTHOR CONTRIBUTIONS
Weber B, Galante AP and Berwanger O conceived, designed and coordinated the study, and helped to draft the manuscript. Carvalho VO, Bersch-Ferreira AC, Buehler AM, Torreglosa CR, Espírito-Santo JA, Ross-Fernandes M, Soares RM, Lara ES and Costa RP participated in the study design and helped to draft the manuscript. Victor ES performed the statistical analysis. All the authors read and approved the final version of the manuscript.
Received for publication on July 6, 2012
First review completed on August 10, 2012
Accepted for publication on August 20, 2012
No potential conflict of interest was reported.
E-mail: bweber@hcor.com.br
Tel.: 55 11 3053-6611
- 1. World Health Organization. Mortality estimates by cause, age, and sex for the year 2008. 2011. Geneva: WHO.
- 2. Hooper L, Griffiths E, Abrahams B, Alexander W, Atkins S, Atkinson G, et al. Dietetic guidelines: diet in secondary prevention of cardiovascular disease (first update, June 2003). J Hum Nutr Diet. 2004;17(4):337-49, http://dx.doi.org/10.1111/j.1365-277X.2004.00533.x
- 3. Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER, III, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the Omni Heart randomized trial. JAMA. 2005;294(19):2455-64, http://dx.doi.org/10.1001/jama.294.19.2455
- 4. Parikh P, McDaniel MC, Ashen MD, Miller JI, Sorrentino M, Chan V, et al. Diets and cardiovascular disease: an evidence-based assessment. J Am Coll Cardiol. 2005;45:1379-87, http://dx.doi.org/10.1016/j.jacc.2004.11.068
- 5. Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6 Suppl):1402S-6S.
- 6. Bellisle F. Infrequently asked questions about the Mediterranean diet. Public Health Nutr. 2009;12(9A):1644-7, http://dx.doi.org/10.1017/S1368980009990498
- 7. Thomazella MC, Góes MF, Andrade CR, Debbas V, Barbeiro DF, Correia RL, et al. Effects of high adherence to mediterranean or low-fat diets in medicated secondary prevention patients. Am J Cardiol. 2011;108 (11):1523-9, http://dx.doi.org/10.1016/j.amjcard.2011.07.008
- 8. Maranhão PA, Kraemer-Aguiar LG, de Oliveira CL, Kuschnir MC, Vieira YR, Souza MG, et al. Brazil nuts intake improves lipid profile, oxidative stress and microvascular function in obese adolescents: a randomized controlled trial. Nutr Metab (Lond). 2011;8(1):32, http://dx.doi.org/10.1186/1743-7075-8-32
- 9. Guerra JF, Magalhães CL, Costa DC, Silva ME, Pedrosa ML. Dietary açai modulates ROS production by neutrophils and gene expression of liver antioxidant enzymes in rats. J Clin Biochem Nutr. 2011;49(3):188-94, http://dx.doi.org/10.3164/jcbn.11-02
- 10. Sposito AC, Caramelli B, Fonseca FAH, Bertolami MC. IV Diretriz Brasileira sobre Dislipidemias e Prevenção da Aterosclerose: Departamento de Aterosclerose da Sociedade Brasileira de Cardiologia. Arq. Bras. Cardiol. 2007;88:suppl1, http://dx.doi.org/10.1590/S0066-782X2007000700002
- 11. Sociedade Brasileira de Cardiologia; Sociedade Brasileira de Hipertensã o; Sociedade Brasileira de Nefrologia. VI Diretrizes Brasileiras de Hipertensã o. Arq Bras Cardiol. 2010;95(supl.1): 1-51.
- 12. Sociedade Brasileira de Cardiologia. I Diretriz Brasileira de Diagnóstico e Tratamento da Síndrome Metabólica. Arq Bras Cardiol. 2005;84(supl. 1):1-28.
- 13. Galante AP. Desenvolvimento e validação de um método computadorizado para avaliação do consumo alimentar, preenchido por indivíduos adultos utilizando a Web. Tese de doutorado. Universidade de São Paulo;2007.
- 14. Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves JW, Hill MN, et al. Recommendations for blood pressure measurement in humans: an AHA scientific statement from the Council on High Blood Pressure Research Professional and Public Education Subcommittee. J Clin Hypertens (Greenwich). 2005;7(2):102-9, http://dx.doi.org/10.1111/j.1524-6175.2005.04377.x
- 15. BMI classification - WHO http://apps.who.int/bmi/index.jsp?introPage=intro_3.html
- 16. de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99:779-85, http://dx.doi.org/10.1161/01.CIR.99.6.779
- 17. Singh RB, Rastogi SS, Verma R, Laxmi B, Singh R, Ghosh S, et al. Randomised controlled trial of cardioprotective diet in patients with recent acute myocardial infarction: results of one year follow up. BMJ. 1992;304(6833):1015-9, http://dx.doi.org/10.1136/bmj.304.6833.1015
- 18. Adamsson V, Reumark A, Fredriksson IB, Hammarström E, Vessby B, Johansson G, et al. Effects of a healthy Nordic diet on cardiovascular risk factors in hypercholesterolaemic subjects: a randomized controlled trial (NORDIET). J Intern Med. 2011;269:150-9, http://dx.doi.org/10.1111/j.1365-2796.2010.02290.x
- 19. Solimene MC. Coronary heart disease in women: a challenge for the 21st century. Clinics. 2010;65:99-106, http://dx.doi.org/10.1590/S1807-59322010000100015
- 20. Torres MR, Ferreira Tda S, Nogueira Lde P, do Nascimento DC, Sanjuliani AF. Dietary counseling on long-term weight loss in overweight hypertensive patients. Clinics. 2011;66(10):1779-85.
- 21. Azevedo CH, Wajngarten M, Prete AC, Diament J, Maranhão RC. Simultaneous transfer of cholesterol, triglycerides, and phospholipids to high-density lipoprotein in aging subjects with or without coronary artery disease. Clinics. 2011;66(9):1543-8.
Publication Dates
-
Publication in this collection
02 Jan 2013 -
Date of issue
Dec 2012
History
-
Received
06 July 2012 -
Accepted
20 Aug 2012 -
Reviewed
10 Aug 2012