Abstract
OBJECTIVES:
Hyperinfection or disseminated strongyloidiasis has been frequently reported after transplants and is related to high mortality. This study aimed to screen for strongyloidiasis using serological diagnoses in transplant candidates.
METHODS:
An ELISA test was performed with filariform larvae of Strongyloides venezuelensis as a source of antigen.
RESULTS:
In the serum from transplant candidates, anti-Strongyloides IgG antibodies were detected in 35/150 (23.3%) samples by soluble fractions in phosphate buffered saline (PBS), 31/150 (20.7%) samples by soluble fractions in Tris-HCl, 27/150 (18.0%) samples by membrane fractions in PBS and 22/150 (14.7%) samples by membrane fractions in Tris-HCl.
CONCLUSIONS:
The present results suggest the ELISA test, ideally using soluble fractions of filariform larvae S. venezuelensis in PBS, as an additional strategy for the diagnosis of strongyloidiasis in transplant candidates.
Heterologous Antigen; Strongyloides Venezuelensis; ELISA Test; Transplant Candidates
INTRODUCTION
The intestinal nematode Strongyloides stercoralis is responsible for human strongyloidiasis, which is endemic in tropical and subtropical regions (11. Olsen A, van Lieshout L, Marti H, Polderman T, Polman K, Steinmann P, et al. Strongyloidiasis - the most neglected of the neglected tropical diseases? Trans R Soc Trop Med Hyg. 2009;103(10):967-72, https://doi.org/10.1016/j.trstmh.2009.02.013.
https://doi.org/10.1016/j.trstmh.2009.02...
). This helminth may cause a benign asymptomatic infection but may also result in more severe complications, such as hyperinfection and disseminated disease, especially in immunocompromised patients (22. Keiser PB, Nutman TB. Strongyloides stercoralis in the Immunocompromised Population. Clin Microbiol Rev. 2004;17(1):208-17, https://doi.org/10.1128/CMR.17.1.208-217.2004.
https://doi.org/10.1128/CMR.17.1.208-217...
). Case reports of hyperinfection or disseminated strongyloidiasis have been frequently reported after solid-organ transplants (33. Vilela EG, Clemente WT, Mira RR, Torres HO, Veloso LF, Fonseca LP, et al. Strongyloides stercoralis hyperinfection syndrome after liver transplantation: case report and literature review. Transpl Infect Dis. 2009;11(2):132-6, https://doi.org/10.1111/j.1399-3062.2008.00350.x.
https://doi.org/10.1111/j.1399-3062.2008...
,44. Khuroo MS. Hyperinfection strongyloidiasis in renal transplant recipients. BMJ Case Rep. 2014;2014. pii: bcr2014205068, https://doi.org/10.1136/bcr-2014-205068.
https://doi.org/10.1136/bcr-2014-205068...
) and after transplantation of hematopoietic cells (55. Izquierdo I, Briones J, Lluch R, Arqueros C, Martino R. Fatal Strongyloides hyperinfection complicating a gram-negative sepsis after allogeneic stem cell transplantation: a case report and review of the literature. Case Rep Hematol. 2013;2013:860976, https://doi.org/10.1155/2013/860976.
https://doi.org/10.1155/2013/860976...
) and are frequently associated with high mortality. In this context, patients who are candidates for transplantation constitute an important group for S. stercoralis screening.
Early diagnosis and treatment of strongyloidiasis prior to transplantation are important factors in minimizing the probability of disease progression to more severe forms (66. Roxby AC, Gottlieb GS, Limaye AP. Strongyloidiasis in transplant patients. Clin Infect Dis. 2009;49(9):1411-23, https://doi.org/10.1086/630201.
https://doi.org/10.1086/630201...
). Therefore, the provision of specific and sensitive techniques for the diagnosis of S. stercoralis infection in both donors and recipients has therapeutic potential, especially in endemic areas. The diagnosis of human strongyloidiasis is based on the observation of S. stercoralis larvae in feces, particularly by concentration or culture techniques (77. Levenhagen MA, Costa-Cruz JM. Update on immunologic and molecular diagnosis of human strongyloidiasis. Acta Trop. 2014;135:33-43, https://doi.org/10.1016/j.actatropica.2014.03.015.
https://doi.org/10.1016/j.actatropica.20...
). However, these parasitological techniques have low sensitivity, requiring multiple samples to reach 100% sensitivity (88. Uparanukraw P, Phongsri S, Morakote N. Fluctuations of larval excretion in Strongyloides stercoralis infection. Am J Trop Med Hyg. 1999;60(6):967-73, https://doi.org/10.4269/ajtmh.1999.60.967.
https://doi.org/10.4269/ajtmh.1999.60.96...
). Thus, serological techniques have been used as alternative diagnostic tools, demonstrating higher sensitivity than that of parasitological methods (77. Levenhagen MA, Costa-Cruz JM. Update on immunologic and molecular diagnosis of human strongyloidiasis. Acta Trop. 2014;135:33-43, https://doi.org/10.1016/j.actatropica.2014.03.015.
https://doi.org/10.1016/j.actatropica.20...
). In a previous study by our group (99. Corral MA, Paula FM, Gottardi M, Meisel DM, Castilho VL, Gonçalves EM, et al. Immunodiagnosis of human strongyloidiasis: use of six different antigenic fractions from Strongyloides venezuelensis parasitic females. Rev Inst Med Trop Sao Paulo. 2015;57(5):427-30, https://doi.org/10.1590/S0036-46652015000500010.
https://doi.org/10.1590/S0036-4665201500...
), IgG-ELISA using filariform larvae antigens of Strongyloides venezuelensis showed 90-100% sensitivity and 92.4-98.4% specificity.
In recent years, the number of transplants worldwide has increased considerably (1010. Baptista MV, Pierrotti LC, Abdala E, Clemente WT, Girão ES, Rosa DR, et al. Endemic and opportunistic infections in Brazilian solid organ transplant recipients. Trop Med Int Health. 2011;16(9):1134-42, https://doi.org/10.1111/j.1365-3156.2011.02816.x.
https://doi.org/10.1111/j.1365-3156.2011...
), implying that more transplant candidates are at a risk of infectious diseases such as strongyloidiasis, especially its severe forms. This study aimed to screen for strongyloidiasis by serological diagnosis in transplant candidates using S. venezuelensis as a source of antigen.
MATERIAL AND METHODS
Serum samples
Serum samples (n=150) were obtained at Hospital das Clínicas of Faculdade de Medicina, Universidade de São Paulo, state of São Paulo, Brazil (HC-FMUSP), from patients who signed informed consent. This study was integrated into a larger study on S. stercoralis infection and was approved by the Research Ethics Committee of HC-FMUSP (protocol no. 0123/10). The transplant candidates were 10-60 years of age from both genders and had underlying diseases conferring some degree of immune dysfunction. All of the patients included in the study had previously been administered parasitological tests [spontaneous sedimentation, modified Baermann (1111. Garcia LS (2001). Diagnostic Medical Parasitology, 4th Edn. American Society for Microbiology, Washington, DC.), and agar plate culture (1212. Koga K, Kasuya S, Khamboonruang C, Sukhavat K, Ieda M, Takatsuka N, et al. A modified agar plate method for detection of Strongyloides stercoralis. Am J Trop Med Hyg. 1991;45(4):518-21, https://doi.org/10.4269/ajtmh.1991.45.518.
https://doi.org/10.4269/ajtmh.1991.45.51...
)]. Serum samples were collected at the time of stool sample and stored at -20°C.
Parasites and antigenic fractions
Antigenic fractions were obtained according to well-standardized methods (99. Corral MA, Paula FM, Gottardi M, Meisel DM, Castilho VL, Gonçalves EM, et al. Immunodiagnosis of human strongyloidiasis: use of six different antigenic fractions from Strongyloides venezuelensis parasitic females. Rev Inst Med Trop Sao Paulo. 2015;57(5):427-30, https://doi.org/10.1590/S0036-46652015000500010.
https://doi.org/10.1590/S0036-4665201500...
). Saline extracts of S. venezuelensis filariform larvae (L3) were obtained from charcoal cultures of feces from experimentally infected Rattus norvegicus (Wistar), protocol (CPE-IMT 2011/126). L3 were resuspended in phosphate buffered saline (PBS, 0.01 M, pH 7.2) or Tris-HCl (25 mM, pH 7.5) containing protease inhibitors (Sigma-Aldrich, St. Louis, MO, USA) and then disrupted in an ice bath using a tissue homogenizer. The suspensions were centrifuged at 12,400 g for 30 min at 4°C, and the supernatant was collected. The soluble fractions prepared in PBS and Tris-HCl were labeled “SS” and “TS,” respectively. The pellets were resuspended in 1% SDS, or in buffer (7M urea, 2 M thiourea, 2% CHAPS), and the supernatant was collected. The membrane fractions prepared separately in PBS and Tris-HCl were labeled “SM” and “TM,” respectively.
ELISA test
As described previously (99. Corral MA, Paula FM, Gottardi M, Meisel DM, Castilho VL, Gonçalves EM, et al. Immunodiagnosis of human strongyloidiasis: use of six different antigenic fractions from Strongyloides venezuelensis parasitic females. Rev Inst Med Trop Sao Paulo. 2015;57(5):427-30, https://doi.org/10.1590/S0036-46652015000500010.
https://doi.org/10.1590/S0036-4665201500...
), polystyrene microplates were coated with each of the antigenic fractions (SS, TS, SM, and TM) at concentrations of 10 μg/mL in carbonate-bicarbonate buffer (0.06 M, pH 9.6) prior to incubation overnight at 4°C. After washing with PBS containing 0.05% Tween-20 and 3% nonfat milk (PBS-TM), the microplates were incubated with serum samples diluted 1:200 PBS-TM for 45 min at 37°C. After washing with PBS-T, enzyme-conjugated goat anti-human IgG (Fc specific)-peroxidase antibody (Sigma-Aldrich, St. Louis, MO, USA) was added at a dilution of 1:30,000 in PBS-TM and incubated for 45 min at 37°C. The assay was developed by adding 3,3′, 5,5- tetramethylbenzidine (TMB) chromogen solution (Thermo Fischer Scientific, Waltham, MA, USA) for 6 min. The reaction was interrupted with 2 N H2SO4. Optical densities (ODs) were determined at 450 nm using an ELISA reader (Thermo Fischer Scientific, Waltham, MA, USA). Absorbance levels ≥0.309 for SS, ≥0.492 for TS, ≥0.381 for SM, and ≥0.394 for TM were considered positive. The cut-off values were determined by receiver operating characteristic curve analysis using negative and other parasite samples (n=72). The ELISA index (EI) was determined by the ratio OD/cut-off, and RI values >1 were considered positive.
Statistical analysis
Statistical analysis was performed using GraphPad Prism version 5.0 (GraphPad Software, La Jolla, USA). Detection of IgG antibodies was analyzed by the Kruskal-Wallis test followed by Dunn’s multiple comparison test. The concordance was carried out by analysis of the kappa coefficient (κ). Statistical significance was set at p<0.05.
RESULTS
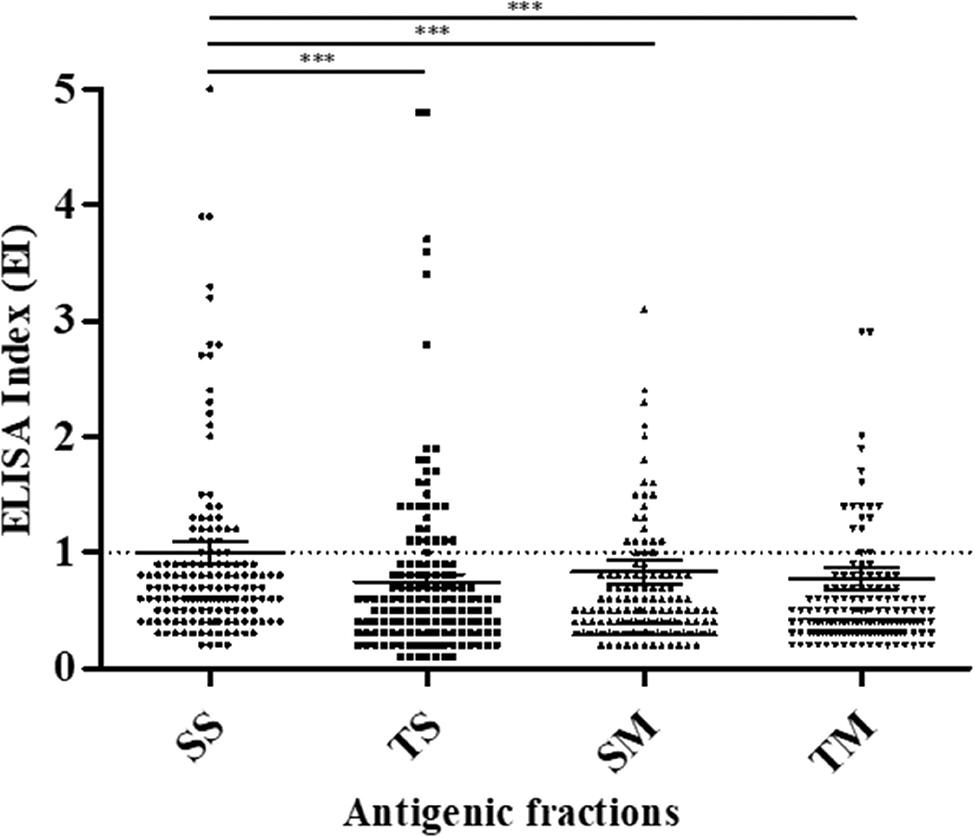
Anti-Strongyloides IgG antibodies in serum from transplant candidates were detected in 35/150 (23.3%) samples by SS, 31/150 (20.7%) samples by TS, 27/150 (18.0%) samples by SM and 22/150 (14.7%) samples by TM (Figure 1). The parasitological diagnosis of the transplant candidates showed that 15/150 (10%) of the patients’ stool samples contained S. stercoralis larvae. Among the fifteen samples that tested positive by the parasitological methods, five showed anti-Strongyloides IgG antibodies detected by using SS and TS antigenic fractions, and four showed anti-Strongyloides IgG antibodies detected by using SM and TM antigenic fractions. Four protozoan-positive samples, including Entamoeba coli (n=3) and Endolimax nana (n=1), were observed, none of which showed reactivity in the different antigenic preparations.
Specific anti-Strongyloides IgG expressed as the ELISA index (EI) for serum samples from transplant candidates using S. venezuelensis antigenic fractions (SS, TS, SM and TM). The dashed lines represent the positivity threshold (EI >1.0).
When comparing the number of positive results identified using different buffers, but the same type of fraction (soluble or membrane), a moderate concordance was observed for both TS and SS (κ=0.567 (0.396−0.739)), and TM and SM (κ=0.433 (0.259−0.608)). When comparing soluble and membrane fractions within the same buffer, a moderate concordance was observed for both TS and TM (κ=0.567 (0.396−0.739)) and SS and SM (κ=0.433 (0.259−0.608)). Similarly, when the number of positive serum samples from patients was analyzed by using soluble (TS and SS) or membrane (TM and SM) fractions, kappa indices of 0.573 (0.414−0.732) and 0.781 (0.644−0.918), respectively, were observed, indicating moderate and good concordance, respectively. Comparing the results of the parasitological tests with those obtained by the ELISA, none of the antigenic fractions demonstrated superior performance.
DISCUSSION
Currently, there is an increased concern about transplantation and S. stercoralis infection, especially due to the increase in the number of transplant cases (1313. Fitzpatrick MA, Caicedo JC, Stosor V, Ison MG. Expanded infectious diseases screening program for Hispanic transplant candidates. Transpl Infect Dis. 2010;12(4):336-41, https://doi.org/10.1111/j.1399-3062.2010.00517.x.
https://doi.org/10.1111/j.1399-3062.2010...
). Camargo et al. (1414. Camargo LFA, Kamar N, Gotuzzo E, Wright AJ. Schistosomiasis and Strongyloidiasis recommendations for solid-organ transplant recipients and donors. Transplantation. 2018;102(2S Suppl 2):S27-S34, https://doi.org/10.1097/TP.0000000000002016.
https://doi.org/10.1097/TP.0000000000002...
) have stressed the need for new research for the rapid diagnosis and early treatment of solid-organ donors and recipients before transplantation. Several studies evaluated extracts from Strongyloides spp. suggesting that rodent species, such as S. ratti and S. venezuelensis, can be used as good source of antigens for the immunodiagnosis of human strongyloidiasis (1515. Feliciano ND, Gonzaga HT, Goncalves-Pires Mdo R, Goncalves AL, Rodrigues RM, Ueta MT, et al. Hydrophobic fractions from Strongyloides venezuelensis for use in the human immunodiagnosis of strongyloidiasis. Diagn Microbiol Infect Dis. 2010;67(2):153-61, https://doi.org/10.1016/j.diagmicrobio.2010.01.012.
https://doi.org/10.1016/j.diagmicrobio.2...
,1616. Eamudomkarn C, Sithithaworn P, Sithithaworn J, Kaewkes S, Sripa S, Itoh M. Comparative evaluation of Strongyloides ratti and S. stercoralis larval antigen for diagnosis of strongyloidiasis in an endemic area of opisthorchiasis. Parasitol Res. 2015;114(7):2543-51, https://doi.org/10.1007/s00436-015-4458-3.
https://doi.org/10.1007/s00436-015-4458-...
). This study is the first to demonstrate the detection of anti-Strongyloides IgG antibodies in candidates for transplantation by an ELISA test using S. venezuelensis as an antigen.
Although the use of serology is a challenging proposal for immunocompromised patients, many studies suggest that it may be beneficial to this profile of patients (1717. Schaffel R, Nucci M, Carvalho E, Braga M, Almeida L, Portugal R, et al. The value of an immunoenzymatic test (enzyme-linked immunosorbent assay) for the diagnosis of strongyloidiasis in patients immunosuppressed by hematologic malignancies. Am J Trop Med Hyg. 2001;65(4):346-50, https://doi.org/10.4269/ajtmh.2001.65.346.
https://doi.org/10.4269/ajtmh.2001.65.34...
,1818. da Silva H, de Carvalho CJ, Levenhagen MA, Costa-Cruz JM. The detergent fraction is effective in the detection of IgG anti-Strongyloides stercoralis in serum samples from immunocompromised individuals. Parasitol Int. 2014;63(6):790-3, https://doi.org/10.1016/j.parint.2014.07.005.
https://doi.org/10.1016/j.parint.2014.07...
). In an ELISA using heterologous S. ratti antigen, 12.05% of the samples showed positive results compared with 2.4% positive results observed using parasitological techniques in immunocompromised children (1919. de Paula FM, de Castro E, Gonçalves-Pires Md, Marçal Md, Campos DM, Costa-Cruz JM. Parasitological and immunological diagnoses of strongyloidiasis in immunocompromised and non-immunocompromised children at Uberlândia, State of Minas Gerais, Brazil. Rev Inst Med Trop Sao Paulo. 2000;42(1):51-5, https://doi.org/10.1590/S0036-46652000000100009.
https://doi.org/10.1590/S0036-4665200000...
). In a study by Schaffel et al. (1717. Schaffel R, Nucci M, Carvalho E, Braga M, Almeida L, Portugal R, et al. The value of an immunoenzymatic test (enzyme-linked immunosorbent assay) for the diagnosis of strongyloidiasis in patients immunosuppressed by hematologic malignancies. Am J Trop Med Hyg. 2001;65(4):346-50, https://doi.org/10.4269/ajtmh.2001.65.346.
https://doi.org/10.4269/ajtmh.2001.65.34...
) involving patients immunocompromised by malignant hematological disease, the performance of ELISA using homologous antigen (18.8% tested positive) was superior to that of parasitological methods (9.1% tested positive). In the present study, ELISA showed a higher number of positive results (14.7−20.7%) than did parasitological methods (10%), independent of the antigenic preparation. Thus, the use of the ELISA technique could be included for diagnostic screening in immunocompromised patients.
However, it is important to emphasize that antigen preparation may interfere with serological test results (11. Olsen A, van Lieshout L, Marti H, Polderman T, Polman K, Steinmann P, et al. Strongyloidiasis - the most neglected of the neglected tropical diseases? Trans R Soc Trop Med Hyg. 2009;103(10):967-72, https://doi.org/10.1016/j.trstmh.2009.02.013.
https://doi.org/10.1016/j.trstmh.2009.02...
). In the present study, soluble fractions showed a higher number of positive results than did membrane fractions. Although soluble protein fractions are more frequently used in the immunodiagnosis of human strongyloidiasis (1515. Feliciano ND, Gonzaga HT, Goncalves-Pires Mdo R, Goncalves AL, Rodrigues RM, Ueta MT, et al. Hydrophobic fractions from Strongyloides venezuelensis for use in the human immunodiagnosis of strongyloidiasis. Diagn Microbiol Infect Dis. 2010;67(2):153-61, https://doi.org/10.1016/j.diagmicrobio.2010.01.012.
https://doi.org/10.1016/j.diagmicrobio.2...
,1818. da Silva H, de Carvalho CJ, Levenhagen MA, Costa-Cruz JM. The detergent fraction is effective in the detection of IgG anti-Strongyloides stercoralis in serum samples from immunocompromised individuals. Parasitol Int. 2014;63(6):790-3, https://doi.org/10.1016/j.parint.2014.07.005.
https://doi.org/10.1016/j.parint.2014.07...
), research also indicates good performance using membrane fractions (99. Corral MA, Paula FM, Gottardi M, Meisel DM, Castilho VL, Gonçalves EM, et al. Immunodiagnosis of human strongyloidiasis: use of six different antigenic fractions from Strongyloides venezuelensis parasitic females. Rev Inst Med Trop Sao Paulo. 2015;57(5):427-30, https://doi.org/10.1590/S0036-46652015000500010.
https://doi.org/10.1590/S0036-4665201500...
).
The limitations of the present study may be related to the degree of immunosuppression, which may have compromised the sensitivity of the ELISA test, leading to negative ELISA results with positive parasitology. Although the ELISA test used was a noncommercial method, our results suggested its high positivity independent of the antigenic preparation.
It is therefore important to emphasize that screening should be performed with ELISA together with parasitological analysis. Considering that transplant candidates are a risk group for the occurrence of severe forms of strongyloidiasis, a positive ELISA result, independent of the antigenic preparation, is a strong indication for specific treatment. In conclusion, this study suggests the ELISA test, especially one using SS fractions, as an additional technique for the diagnosis of strongyloidiasis in transplant candidates.
ACKNOWLEDGMENTS
This study was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP 2010/51110-2 and 2013/04236-9).
REFERENCES
-
1Olsen A, van Lieshout L, Marti H, Polderman T, Polman K, Steinmann P, et al. Strongyloidiasis - the most neglected of the neglected tropical diseases? Trans R Soc Trop Med Hyg. 2009;103(10):967-72, https://doi.org/10.1016/j.trstmh.2009.02.013
» https://doi.org/10.1016/j.trstmh.2009.02.013 -
2Keiser PB, Nutman TB. Strongyloides stercoralis in the Immunocompromised Population. Clin Microbiol Rev. 2004;17(1):208-17, https://doi.org/10.1128/CMR.17.1.208-217.2004
» https://doi.org/10.1128/CMR.17.1.208-217.2004 -
3Vilela EG, Clemente WT, Mira RR, Torres HO, Veloso LF, Fonseca LP, et al. Strongyloides stercoralis hyperinfection syndrome after liver transplantation: case report and literature review. Transpl Infect Dis. 2009;11(2):132-6, https://doi.org/10.1111/j.1399-3062.2008.00350.x
» https://doi.org/10.1111/j.1399-3062.2008.00350.x -
4Khuroo MS. Hyperinfection strongyloidiasis in renal transplant recipients. BMJ Case Rep. 2014;2014. pii: bcr2014205068, https://doi.org/10.1136/bcr-2014-205068
» https://doi.org/10.1136/bcr-2014-205068 -
5Izquierdo I, Briones J, Lluch R, Arqueros C, Martino R. Fatal Strongyloides hyperinfection complicating a gram-negative sepsis after allogeneic stem cell transplantation: a case report and review of the literature. Case Rep Hematol. 2013;2013:860976, https://doi.org/10.1155/2013/860976
» https://doi.org/10.1155/2013/860976 -
6Roxby AC, Gottlieb GS, Limaye AP. Strongyloidiasis in transplant patients. Clin Infect Dis. 2009;49(9):1411-23, https://doi.org/10.1086/630201
» https://doi.org/10.1086/630201 -
7Levenhagen MA, Costa-Cruz JM. Update on immunologic and molecular diagnosis of human strongyloidiasis. Acta Trop. 2014;135:33-43, https://doi.org/10.1016/j.actatropica.2014.03.015
» https://doi.org/10.1016/j.actatropica.2014.03.015 -
8Uparanukraw P, Phongsri S, Morakote N. Fluctuations of larval excretion in Strongyloides stercoralis infection. Am J Trop Med Hyg. 1999;60(6):967-73, https://doi.org/10.4269/ajtmh.1999.60.967
» https://doi.org/10.4269/ajtmh.1999.60.967 -
9Corral MA, Paula FM, Gottardi M, Meisel DM, Castilho VL, Gonçalves EM, et al. Immunodiagnosis of human strongyloidiasis: use of six different antigenic fractions from Strongyloides venezuelensis parasitic females. Rev Inst Med Trop Sao Paulo. 2015;57(5):427-30, https://doi.org/10.1590/S0036-46652015000500010
» https://doi.org/10.1590/S0036-46652015000500010 -
10Baptista MV, Pierrotti LC, Abdala E, Clemente WT, Girão ES, Rosa DR, et al. Endemic and opportunistic infections in Brazilian solid organ transplant recipients. Trop Med Int Health. 2011;16(9):1134-42, https://doi.org/10.1111/j.1365-3156.2011.02816.x
» https://doi.org/10.1111/j.1365-3156.2011.02816.x -
11Garcia LS (2001). Diagnostic Medical Parasitology, 4th Edn. American Society for Microbiology, Washington, DC.
-
12Koga K, Kasuya S, Khamboonruang C, Sukhavat K, Ieda M, Takatsuka N, et al. A modified agar plate method for detection of Strongyloides stercoralis Am J Trop Med Hyg. 1991;45(4):518-21, https://doi.org/10.4269/ajtmh.1991.45.518
» https://doi.org/10.4269/ajtmh.1991.45.518 -
13Fitzpatrick MA, Caicedo JC, Stosor V, Ison MG. Expanded infectious diseases screening program for Hispanic transplant candidates. Transpl Infect Dis. 2010;12(4):336-41, https://doi.org/10.1111/j.1399-3062.2010.00517.x
» https://doi.org/10.1111/j.1399-3062.2010.00517.x -
14Camargo LFA, Kamar N, Gotuzzo E, Wright AJ. Schistosomiasis and Strongyloidiasis recommendations for solid-organ transplant recipients and donors. Transplantation. 2018;102(2S Suppl 2):S27-S34, https://doi.org/10.1097/TP.0000000000002016
» https://doi.org/10.1097/TP.0000000000002016 -
15Feliciano ND, Gonzaga HT, Goncalves-Pires Mdo R, Goncalves AL, Rodrigues RM, Ueta MT, et al. Hydrophobic fractions from Strongyloides venezuelensis for use in the human immunodiagnosis of strongyloidiasis. Diagn Microbiol Infect Dis. 2010;67(2):153-61, https://doi.org/10.1016/j.diagmicrobio.2010.01.012
» https://doi.org/10.1016/j.diagmicrobio.2010.01.012 -
16Eamudomkarn C, Sithithaworn P, Sithithaworn J, Kaewkes S, Sripa S, Itoh M. Comparative evaluation of Strongyloides ratti and S. stercoralis larval antigen for diagnosis of strongyloidiasis in an endemic area of opisthorchiasis. Parasitol Res. 2015;114(7):2543-51, https://doi.org/10.1007/s00436-015-4458-3
» https://doi.org/10.1007/s00436-015-4458-3 -
17Schaffel R, Nucci M, Carvalho E, Braga M, Almeida L, Portugal R, et al. The value of an immunoenzymatic test (enzyme-linked immunosorbent assay) for the diagnosis of strongyloidiasis in patients immunosuppressed by hematologic malignancies. Am J Trop Med Hyg. 2001;65(4):346-50, https://doi.org/10.4269/ajtmh.2001.65.346
» https://doi.org/10.4269/ajtmh.2001.65.346 -
18da Silva H, de Carvalho CJ, Levenhagen MA, Costa-Cruz JM. The detergent fraction is effective in the detection of IgG anti-Strongyloides stercoralis in serum samples from immunocompromised individuals. Parasitol Int. 2014;63(6):790-3, https://doi.org/10.1016/j.parint.2014.07.005
» https://doi.org/10.1016/j.parint.2014.07.005 -
19de Paula FM, de Castro E, Gonçalves-Pires Md, Marçal Md, Campos DM, Costa-Cruz JM. Parasitological and immunological diagnoses of strongyloidiasis in immunocompromised and non-immunocompromised children at Uberlândia, State of Minas Gerais, Brazil. Rev Inst Med Trop Sao Paulo. 2000;42(1):51-5, https://doi.org/10.1590/S0036-46652000000100009
» https://doi.org/10.1590/S0036-46652000000100009
Publication Dates
-
Publication in this collection
06 June 2019 -
Date of issue
2019
History
-
Received
25 May 2018 -
Accepted
19 Dec 2018