Abstract
OBJECTIVES:
Anemia and changes in platelets (PLT) are common in inflammatory bowel disease (IBD). In our study, we aimed to verify whether PLT count can independently reflect the severity of IBD.
METHODS:
In our hospital, 137 Crohn’s Disease (CD), 69 Ulcerative colitis (UC) patients, and 412 healthy controls were included to compare the differences in PLT count. In addition, the effect of anemia, C-reactive protein (CRP), age, CD activity index (CDAI) or Mayo on PLTs was also analyzed. If PLTs independently affected CD or UC, we used the receiver operating characteristic (ROC) curve to verify the diagnostic value and obtain the cut-off value of PLT.
RESULTS:
CD and UC patients had higher PLT than controls (p<0.001, p<0.001; respectively). In CD patients, the results showed that patients with anemia (P<0.01), Iron Deficiency Anemia (IDA) (p<0.001), CRP≥8 mg/L (p=0.046), and CDAI≥150 (p<0.001) had higher PLT, while in UC patients, those with anemia (p=0.018), CRP≥8 mg/L (p=0.045), and Mayo≥3 (p=0.029) had higher PLT. Univariate analysis showed that CDAI was positively correlated with PLT count (p<0.001), while hemoglobin (p=0.001) and age (p<0.001) were negatively correlated with PLT in CD. In UC patients, Mayo (p=0.001) and CRP (p<0.001) were positively correlated with PLT, while hemoglobin (p=0.002) was negatively correlated. Finally, by linear stepwise multivariate analysis, we clarified the positive relationship between PLT and CD (p<0.001) by eliminating the interference of hemoglobin, and determined the cut-off value of PLT as 298×109/L. For UC, we did not obtain similar results.
CONCLUSIONS:
PLT can be an indicator of disease severity in CD, while there is a lack of evidence regarding this finding in UC.
Platelet; Anemia; Crohn's Disease; Ulcerative Colitis
INTRODUCTION
Inflammatory bowel disease (IBD), including Crohn's disease (CD) and ulcerative colitis (UC), refers to a group of chronic gastrointestinal disorders characterized by dysregulated intestinal inflammation (11. Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361(21):2066-78. https://doi.org/10.1056/NEJMra0804647.
https://doi.org/10.1056/NEJMra0804647...
). The immune dysregulation may dominate IBD pathogenesis with its active components (22. Bouma G, Strober W. The immunological and genetic basis of inflammatory bowel disease. Nat Rev Immunol. 2003;3(7):521-33. https://doi.org/10.1038/nri1132.
https://doi.org/10.1038/nri1132...
), while other factors such as genetic (33. Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, Ramos R, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001;411(6837):603-6. https://doi.org/10.1038/35079114.
https://doi.org/10.1038/35079114...
) and environmental factors (44. Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126(6):1504-17. https://doi.org/10.1053/j.gastro.2004.01.063.
https://doi.org/10.1053/j.gastro.2004.01...
) have also been implicated. In addition, an increasing amount of evidence has highlighted the importance of non-immune cells and platelets (PLT) as key players in the development of IBD (55. Danese S, Motte Cd Cde L, Fiocchi C. Platelets in inflammatory bowel disease: clinical, pathogenic, and therapeutic implications. Am J Gastroenterol. 2004;99(5):938-45. https://doi.org/10.1111/j.1572-0241.2004.04129.x.
https://doi.org/10.1111/j.1572-0241.2004...
).
The primary role of PLT is hemostasis, including surveying the endothelial barrier consistency and interfering when vessel integrity is threatened (66. Fiocchi C. Inflammatory bowel disease: etiology and pathogenesis. Gastroenterology. 1998;115(1):182-205. https://doi.org/10.1016/S0016-5085(98)70381-6.
https://doi.org/10.1016/S0016-5085(98)70...
). Moreover, it has been demonstrated that PLT have immunological properties. Through the activity of GP VI and integrin family surface receptors, activated PLT transform into high-affinity platforms that are suitable for participating in inflammatory reactions (77. Huang HS, Chang HH. Platelets in inflammation and immune modulations: functions beyond hemostasis. Arch Immunol Ther Exp. 2012;60(6):443-51. https://doi.org/10.1007/s00005-012-0193-y.
https://doi.org/10.1007/s00005-012-0193-...
). They also express Toll-like receptors that can bind to lipopolysaccharides on the outer membrane of gram(-) bacteria (88. Cognasse F, Lafarge S, Chavarin P, Acquart S, Garraud O. Lipopolysaccharide induces sCD40L release through human platelets TLR4, but not TLR2 and TLR9. Intensive Care Med. 2007;33(2):382-4. https://doi.org/10.1007/s00134-006-0488-8.
https://doi.org/10.1007/s00134-006-0488-...
). When activated at inflammatory sites, PLT excrete large amounts of pro-inflammatory substances located in their intracellular granules (99. Smyth SS, McEver RP, Weyrich AS, Morrell CN, Hoffman MR, Arepally GM, et al. Platelet functions beyond hemostasis. J Thromb Haemost. 2009;7(11):1759-66. https://doi.org/10.1111/j.1538-7836.2009.03586.x.
https://doi.org/10.1111/j.1538-7836.2009...
), as well as immune-like cells even at distant sites such as PLT-derived CD40 ligand (CD40L), to activate dendritic cells in the injured tissue (1010. Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392(6673):245-52. https://doi.org/10.1038/32588.
https://doi.org/10.1038/32588...
).
We know that patients with IBD usually have gastrointestinal symptoms, such as diarrhea, abdominal pain, weight loss, or gastrointestinal bleeding. Remarkably, approximately one-third of IBD patients present at least one extra-intestinal feature (1111. Bernstein CN, Blanchard JF, Rawsthorne P, Yu N. The prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study. Am J Gastroenterol. 2001;96(4):1116-22. https://doi.org/10.1111/j.1572-0241.2001.03756.x.
https://doi.org/10.1111/j.1572-0241.2001...
). Anemia, especially microcytic hypochromic anemia, which is the main hematological symptom, could be perceived as a manifestation or complication of IBD. Anemia is consistently linked with IBD and the prevalence ranges from 4% to 67% (1212. Gasche C, Lomer MC, Cavill I, Weiss G. Iron, anaemia, and inflammatory bowel diseases. Gut. 2004;53(8):1190-7. https://doi.org/10.1136/gut.2003.035758.
https://doi.org/10.1136/gut.2003.035758...
,1313. Kulnigg S, Gasche C. Systematic review: managing anaemia in Crohn's disease. Aliment Pharmacol Ther. 2006;24(11-12):1507-23. https://doi.org/10.1111/j.1365-2036.2006.03146.x.
https://doi.org/10.1111/j.1365-2036.2006...
). In IBD patients, iron deficiency anemia (IDA) is the most frequent manifestation of the microcytic hypochromic anemia (1414. Bager P, Befrits R, Wikman O, Lindgren S, Moum B, Hjortswang H, et al. The prevalence of anemia and iron deficiency in IBD outpatients in Scandinavia. Scand J Gastroenterol. 2011;46(3):304-9. https://doi.org/10.3109/00365521.2010.533382.
https://doi.org/10.3109/00365521.2010.53...
). Either chronic intestinal bleeding caused by mucosal damage or poor nutritional status influencing the absorption of iron in the inflamed mucosa of the duodenum and upper jejunum can result in anemia. Iron supplementation for IBD treatment has gained increasing attention (1515. Murawska N, Fabisiak A, Fichna J. Anemia of Chronic Disease and Iron Deficiency Anemia in Inflammatory Bowel Diseases: Pathophysiology, Diagnosis, and Treatment. Inflamm Bowel Dis. 2016;22(5):1198-208. https://doi.org/10.1097/MIB.0000000000000648.
https://doi.org/10.1097/MIB.000000000000...
).
In IBD, anemia and PLT count changes were observed. However, no study has been conducted to determine whether there is a close relationship between anemia and PLT in IBD. Whether PLT count change is affected by secondary bone marrow metabolic disorder or anemia is yet to be determined. In our study, we aimed to determine the relationship between the three factors of IBD, PLT, and anemia by analyzing clinical data. In addition, we aimed to verify whether PLT can be an independent indicator of IBD severity.
MATERIALS AND METHODS
Patients and diagnostic criteria
Medical records of patients undergoing evaluation and treatment for UC and CD in our hospital between January 1, 2012, and May 1, 2016, were reviewed. This study was approved by our Institutional Review Board. Informed consent was obtained from the participants and their privacy was respected. The experimental protocol was approved by the Ethics Committee of the First Affiliated Hospital, College of Medicine, Zhejiang University. In addition, all procedures were performed in accordance with the relevant guidelines and regulations.
In total, 137 CD patients and 69 UC patients were included. The diagnosis of UC and CD were made based on a combined assessment of abdominal imaging, endoscopy, symptomatology, and histology. The pattern and distribution of UC and CD were obtained from endoscopic, radiological, and histological findings (1616. Bernstein CN, Fried M, Krabshuis JH, Cohen H, Eliakim R, Fedail S, et al. World Gastroenterology Organization Practice Guidelines for the diagnosis and management of IBD in 2010. Inflamm Bowel Dis. 2010;16(1):112-24. https://doi.org/10.1002/ibd.21048.
https://doi.org/10.1002/ibd.21048...
). All the patients enrolled had not received prior treatment with hormones, immunosuppressants, or biological agents. Additionally, we selected 412 healthy controls matched by gender, age, and Body Mass Index (BMI) from an international medical center. Nevertheless, because the values of some BMI data in IBD patients were very low, we selected the lowest BMI in the group of controls for random matching.
The inclusion criteria were as follows: 1) age>18 years old; 2) no history of tuberculosis, cirrhosis, cancer, cardiovascular and cerebrovascular diseases, or other chronic diseases; 3) no history of thrombus or drugs that can influence PLT quantity and activity; 4) no other acute infectious diseases.
We extracted data, including age, gender, general condition, hemoglobin (HB), PLT, C-reactive protein (CRP), hematocrit (HCT), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), and mean corpuscular hemoglobin concentration (MCHC). Moreover, anemia was defined as HB<120 g/L in males or <110 g/L in females. Microcytic hypochromic anemia was defined as MCV<80 fl, MCH<26 pg, and MCHC<310 g/L. CRP was chosen to reflect the disease activity and 8 mg/L was the cut-off level between remission and IBD activity (1717. Iborra M, Beltrán B, Nos P. Noninvasive Testing for Mucosal Inflammation in Inflammatory Bowel Disease. Gastrointest Endosc Clin N Am. 2016;26(4):641-56. https://doi.org/10.1016/j.giec.2016.06.005.
https://doi.org/10.1016/j.giec.2016.06.0...
). In addition, the CD activity index (CDAI) was used to assess the condition of the CD patients, while the Mayo scoring system was used to assess the condition of the UC patients (1818. Gionchetti P, Dignass A, Danese S, Magro Dias FJ, Rogler G, Lakatos PL, et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn's Disease 2016: Part 2: Surgical Management and Special Situations. J Crohns Colitis. 2017;11(2):135-49. https://doi.org/10.1093/ecco-jcc/jjw169.
https://doi.org/10.1093/ecco-jcc/jjw169...
,1919. Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, et al. Third European Evidence-Based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders. J Crohns Colitis. 2017;11(6):649-70. https://doi.org/10.1093/ecco-jcc/jjx008.
https://doi.org/10.1093/ecco-jcc/jjx008...
). The Mayo scoring system (including defecating frequency, bloody stools, endoscopic characteristics, and physician evaluation) indicated that <3 is remission, 3-5 is mild activity, 6-10 is moderate activity, and 11-12 is severe activity. In addition, the CDAI indicated that <150 is remission, 150-220 is mild activity, 221-450 is moderate activity, and >450 is severe activity.
Statistical analysis
Continuous variables were expressed as mean±standard deviation. The variables were tested by SPSS and were found to be normally distributed. Student's t-test was used to compare the difference in PLT between the different subgroups. Univariate analysis of linear regression was performed to compare PLT count with age, anemia, IDA, CRP, CDAI, and Mayo. If a significant difference was found on univariate analysis, it was included into the stepwise multivariate analysis using logistic or linear regression. In addition, Pearson’s correlation coefficient was conducted to correlate PLT and CDAI or Mayo score. Furthermore, coefficients of variables for the multivariate model were estimated. If PLT was related to the severity of CD or UC, we also conducted an ROC curve to verify the diagnostic value of PLT and to obtain the PLT cut-off value. The PLT cut-off value was defined by Youden's index. The statistical significance was defined as p≤0.05. We used SPSS 21.0 (IBM, Chicago, IL, USA) to perform the statistical analysis. Other associated data were calculated and plotted using GraphPad Prism 5 (Graph Pad, San Diego, CA, USA).
RESULTS
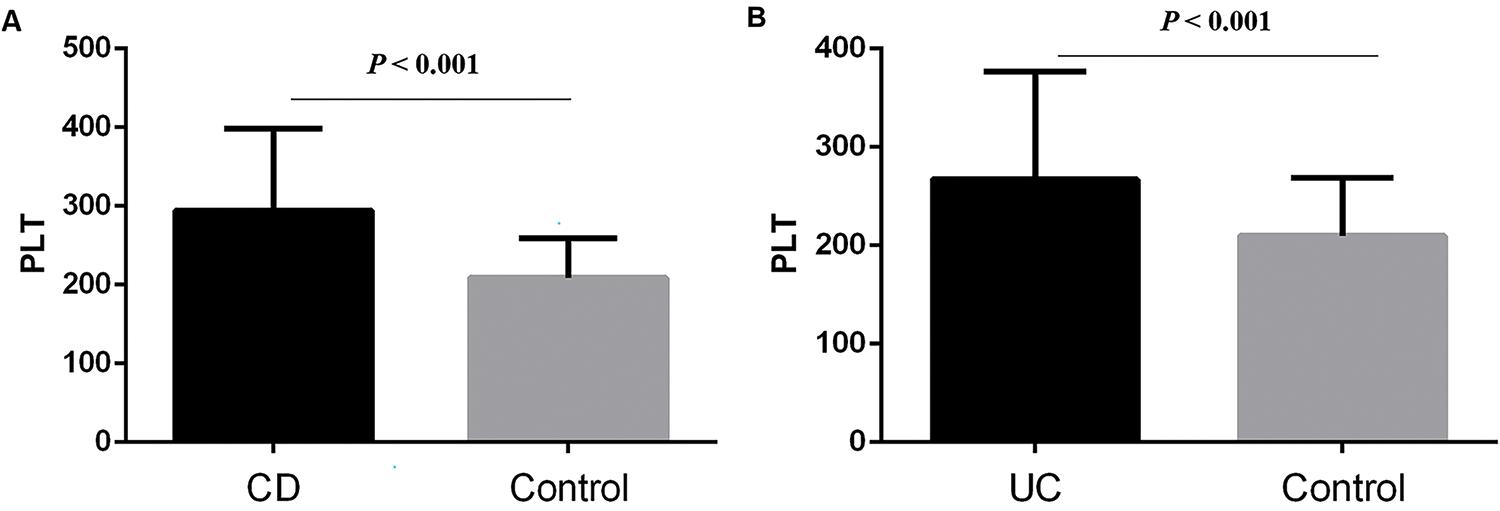
The basic characteristics of the patients, including age, gender, PLT, CRP, hemoglobin, CDAI or Mayo are described in Table 1. We found that CD and UC patients had higher PLT than the controls (294.58±103.86 vs. 208.97±50.39, p<0.001; 267.29±109.34 vs. 209.68±59.2, p<0.001; respectively) (Figure 1 A and B). Then, we sought to determine the factors affecting the PLT of CD and UC. In CD patients, the results showed that patients with anemia (323.4±107.68 vs. 248.89±78.97, p<0.01; Figure 2A), IDA (345.45±101.26 vs. 270.51±96.59, p<0.001; Figure 2B), CRP≥8 mg/L (304.9±104.95 vs. 263.97±100.98, p=0.046; Figure 2C), and CDAI≥150 (345.45±101.26 vs. 273.75±94.22, p<0.001; Figure 2D) had higher PLT. However, there was no significant difference between males and females (p=0.248).
(A) CD patients had higher PLT than controls (294.58±103.86 vs. 208.97±50.39, p<0.001); (B) UC patients had higher PLT than controls (267.29±109.34 vs. 209.68±59.2, p<0.001).
In CD patients, it was demonstrated that patients with (A) anemia (323.4±107.68 vs. 248.89±78.97, p<0.01), (B) IDA (345.45±101.26 vs. 270.51±96.59, p<0.001), (C) CRP≥8 mg/L (304.9±104.95 vs. 263.97±100.98, p=0.046), (D) CDAI≥150 (345.45±101.26 vs. 273.75±94.22, p<0.001) had higher PLT.
Similarly, UC patients with anemia (302.37±127.12 vs. 240.3±85.68, p=0.018; Figure 3A), CRP≥8 mg/L (293.18±117.35 vs. 240.17±96.31, p=0.045; Figure 3B), and Mayo≥3 (277.86±107.21 vs. 192.33±104.01, p=0.029; Figure 3C) had higher PLT, whereas IDA (p=0.241, Figure 3D) and gender (p=0.071) were not statistical significance.
In UC patients, (A) anemia (302.37±127.12 vs. 240.3±85.68, p=0.018), (B) CRP≥8 mg/L (293.18±117.35 vs. 240.17±96.31, p=0.045), (C) Mayo≥3 (277.86±107.21 vs. 192.33±104.01, p=0.029) had higher PLT. IDA (p=0.241) had no significant difference.
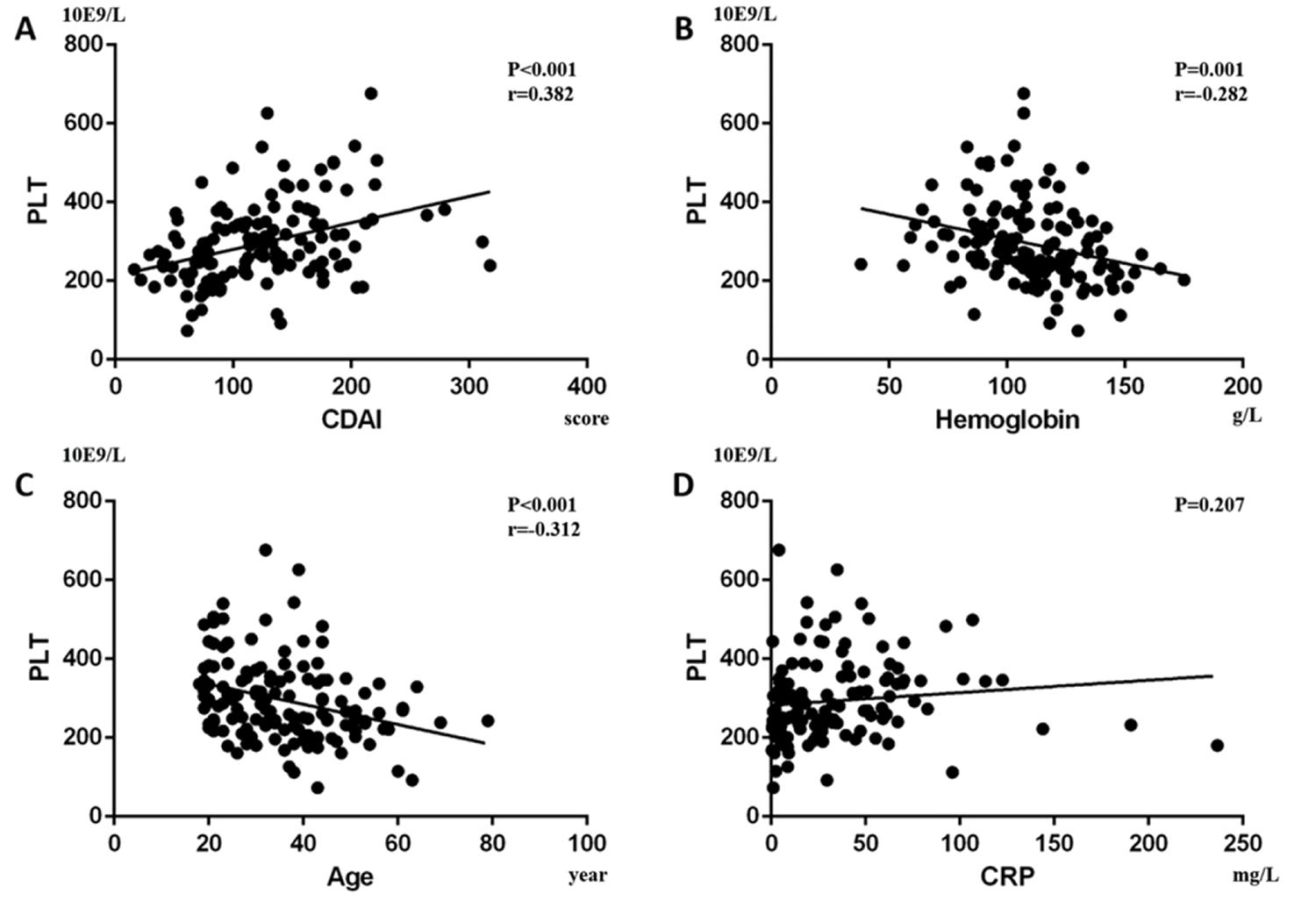
Furthermore, we performed a univariate analysis for the variables above. In CD patients, it showed that CDAI was positively correlated with PLT (p<0.001, Beta=0.382; Figure 4A) and Pearson’s correlation was 0.382 (p<0.001), while hemoglobin (p=0.001, Beta=-0.282; Figure 4B) and age (p<0.001, Beta=-0.312; Figure 4C) were negatively correlated with PLT. In addition, CRP was not statistically correlated with PLT (p=0.207; Figure 4D). In UC patients, we found that Mayo (p=0.001, Beta=0.391; Figure 5A) and CRP (p<0.001, Beta=0.46; Figure 5B) were positively correlated with PLT, while hemoglobin (p=0.002, Beta=-0.374; Figure 5C) was negatively correlated with PLT. Pearson’s correlation between PLT and the Mayo score was 0.391 (p=0.001). Age had no statistical correlation with PLT (-p=0.06; Figure 5D).
. In CD patients, it was shown that (A) CDAI was positively correlated with PLT (p<0.001, Beta=0.382), while (B) hemoglobin (p=0.001, Beta=-0.282) and (C) age (p<0.001, Beta=-0.312) were negatively correlated with PLT. Moreover, (D) CRP had no significant correlation with PLT (p=0.207).
In UC patients, we found that (A) Mayo (p=0.001, Beta=0.391) and (B) CRP (p<0.001, Beta=0.46) were positively correlated with PLT, while (C) hemoglobin (p=0.002, Beta=-0.374) was negatively correlated with PLT. (D) Age had no significant correlation with PLT (p=0.06).
Finally, we performed a linear stepwise multivariate analysis on PLT with age, hemoglobin, CRP, CDAI or Mayo. Firstly, through the analysis of the collinearity of the variables, we found that there was no severe collinearity among the respective variables (VIF<10). For CD patients, we clarified the positive relationship between PLT and CDAI (p<0.001, Beta=0.378, 95%CI: 0.395, 0.935) by eliminating the interference of hemoglobin (P=0.006). In contrast, age was negatively correlated with PLTs (p<0.001, Beta=-0.286, 95%CI: -3.692, -1.110). These results showed that PLT can be used to evaluate the severity of CD. In UC patients, Mayo (p=0.005, Beta=0.302, 95%CI: 3.334, 17.692) and CRP (p=0.002, Beta=0.334, 95%CI: 0.383, 1.627) were still positively correlated with PLT. Moreover, hemoglobin (p=0.006, Beta=-0.286, 95%CI: -2.535, -0.454) was negatively correlated with PLT. For these results, we could not clarify whether PLT change in UC was affected by hemoglobin.
Through the ROC curve, we aimed to determine whether PLTs had a diagnostic value for CD. CD patients were divided into remission and activity by CDAI. The results of the ROC curve showed that PLT had a diagnostic significance for CD (Area=0.695, p<0.001) and the PLT cut-off value was 298×109/L.
DISCUSSION
In our study, we found that PLT count was positively correlated with the CDAI while it was negatively correlated with age. In addition, we identified the diagnostic value of PLT for CD using the ROC curve and defined the PLT cut-off value for CD as 298*10E9/L. In UC patients, we found that Mayo and CRP were positively correlated with PLT, while hemoglobin was negatively correlated with PLT. However, we could not conclude as to whether PLT can reflect the severity of UC because the influence of hemoglobin on PLT could not be ignored.
In CD patients, PLT was negatively correlated with age. As individuals age, the number and function of hematopoietic stem cells may decrease and PLT consumption due to vascular endothelial injury may induce a decrease in PLT. Cowman et al. reported that aging resulted in a significant reduction of the PLT function in the Dynamic Platelet Function Assay (2020. Cowman J, Dunne E, Oglesby I, Byrne B, Ralph A, Voisin B, et al. Age-related changes in platelet function are more profound in women than in men. Sci Rep. 2015;5:12235. https://doi.org/10.1038/srep12235
https://doi.org/10.1038/srep12235...
). Destruction of platelet function may also contribute to affect the lifetime and quantity of PLT.
Murawska et al. found that anemia coexists with IBD (1515. Murawska N, Fabisiak A, Fichna J. Anemia of Chronic Disease and Iron Deficiency Anemia in Inflammatory Bowel Diseases: Pathophysiology, Diagnosis, and Treatment. Inflamm Bowel Dis. 2016;22(5):1198-208. https://doi.org/10.1097/MIB.0000000000000648.
https://doi.org/10.1097/MIB.000000000000...
) and our study was consistent with their results. We know that there is an increased activation of tumor necrosis factor α (TNF-α) in IBD (11. Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361(21):2066-78. https://doi.org/10.1056/NEJMra0804647.
https://doi.org/10.1056/NEJMra0804647...
). Moreover, Roodman et al. first reported that TNF-α can inhibit erythropoiesis (2121. Roodman GD, Bird A, Hutzler D, Montgomery W. Tumor necrosis factor-alpha and hematopoietic progenitors: effects of tumor necrosis factor on the growth of erythroid progenitors CFU-E and BFU-E and the hematopoietic cell lines K562, HL60, and HEL cells. Exp Hematol. 1987;15(9):928-35.). Since then, more studies have reported the relationship between TNF-α and anemia. Some articles had reported that TNF-α indirectly suppresses the expression of erythropoietin synthesis in kidneys, potentially by GATA-2 and nucleus factor kappa B overexpression (2222. La Ferla K, Reimann C, Jelkmann W, Hellwig-Burgel T. Inhibition of erythropoietin gene expression signaling involves the transcription factors GATA-2 and NF-kappaB. FASEB J. 2002;16(13):1811-3. https://doi.org/10.1096/fj.02-0168fje.
https://doi.org/10.1096/fj.02-0168fje...
,2323. Nakano Y, Imagawa S, Matsumoto K, Stockmann C, Obara N, Suzuki N, et al. Oral administration of K-11706 inhibits GATA binding activity, enhances hypoxia-inducible factor 1 binding activity, and restores indicators in an in vivo mouse model of anemia of chronic disease. Blood. 2004;104(13):4300-7. https://doi.org/10.1182/blood-2004-04-1631.
https://doi.org/10.1182/blood-2004-04-16...
). In addition, Rusten et al. found that TNF-α can directly inhibit human erythropoiesis via TNF receptors, including p55 and p75 TNF receptors (2424. Rusten LS, Jacobsen SE. Tumor necrosis factor (TNF)-alpha directly inhibits human erythropoiesis in vitro: role of p55 and p75 TNF receptors. Blood. 1995;85(4):989-96. https://doi.org/10.1182/blood.V85.4.989.bloodjournal854989.
https://doi.org/10.1182/blood.V85.4.989....
). Furthermore, serving as a ligand for cellular iron efflux receptor, hepcidin was strongly correlated with IL-6 levels in CD patients (2525. Basseri RJ, Nemeth E, Vassilaki ME, Basseri B, Enayati P, Shaye O, et al. Hepcidin is a key mediator of anemia of inflammation in Crohn's disease. J Crohns Colitis. 2013;7(8):e286-91. https://doi.org/10.1016/j.crohns.2012.10.013.
https://doi.org/10.1016/j.crohns.2012.10...
).
In IBD patients, in addition to anemia, elevated PLT levels could also be found. In our study, after excluding the effect of anemia on PLT, we found that PLT were directly associated with CD disease activity. Di Sabatino et al. found evidence for enhanced in vivo 11-dehydro-thromboxane-dependent PLT activation and lipid peroxidation in IBD patients while demonstrating that anti-TNF-α therapy with infliximab down-regulates isoprostane generation and TX biosynthesis in vivo in responder IBD patients (2626. Di Sabatino A, Santilli F, Guerci M, Simeone P, Ardizzone S, Massari A, et al. Oxidative stress and thromboxane-dependent platelet activation in inflammatory bowel disease: effects of anti-TNF-alpha treatment. Thromb Haemost. 2016;116(3):486-95. https://doi.org/10.1160/TH16-02-0167.
https://doi.org/10.1160/TH16-02-0167...
). Except for hemostatic function, the innate immunological properties of PLT have become increasingly elucidated. Youssefian et al. demonstrated that PLT can internalize pathogens resistant to clearance, such as Staphylococcus aureus or HIV virus, promoting further PLT activation changes (2727. Youssefian T, Drouin A, Massé JM, Guichard J, Cramer EM. Host defense role of platelets: engulfment of HIV and Staphylococcus aureus occurs in a specific subcellular compartment and is enhanced by platelet activation. Blood. 2002;99(11):4021-9. https://doi.org/10.1182/blood-2001-12-0191.
https://doi.org/10.1182/blood-2001-12-01...
). In addition, PLT can crosstalk, recruit, and activate leukocytes, endothelial, and immune-like cells by excreting large amounts of pro-inflammatory substances located in their intracellular granules (99. Smyth SS, McEver RP, Weyrich AS, Morrell CN, Hoffman MR, Arepally GM, et al. Platelet functions beyond hemostasis. J Thromb Haemost. 2009;7(11):1759-66. https://doi.org/10.1111/j.1538-7836.2009.03586.x.
https://doi.org/10.1111/j.1538-7836.2009...
). Heits et al. have shown that IBD patients have elevated plasma thrombopoietin (TPO) and IL-6 levels, an acute phase reactant, which can promote hepatic TPO production (2828. Heits F, Stahl M, Ludwig D, Stange EF, Jelkmann W. Elevated serum thrombopoietin and interleukin-6 concentrations in thrombocytosis associated with inflammatory bowel disease. J Interferon Cytokine Res. 1999;19(7):757-60. https://doi.org/10.1089/107999099313604.
https://doi.org/10.1089/107999099313604...
,2929. Kaushansky K. Determinants of platelet number and regulation of thrombopoiesis. Hematology Am Soc Hematol Educ Program. 2009;147-52. https://doi.org/10.1182/asheducation-2009.1.147.
https://doi.org/10.1182/asheducation-200...
). Since PLT are involved in immune responses, can platelets act as active inflammatory components?
Collins et al. demonstrated that PLT circulate at a highly activated state in IBD and activation possibly occurs in the mesenteric microcirculation (3030. Collins CE, Cahill MR, Newland AC, Rampton DS. Platelets circulate in an activated state in inflammatory bowel disease. Gastroenterology. 1994;106(4):840-5. https://doi.org/10.1016/0016-5085(94)90741-2.
https://doi.org/10.1016/0016-5085(94)907...
,3131. Collins CE, Rampton DS, Rogers J, Williams NS. Platelet aggregation and neutrophil sequestration in the mesenteric circulation in inflammatory bowel disease. Eur J Gastroenterol Hepatol. 1997;9(12):1213-7.). During activation, PLT can develop receptors for chemokines, cytokines, and complement components, enabling them to participate in various inflammatory cascades in IBD (3232. Voudoukis E, Karmiris K, Koutroubakis IE. Multipotent role of platelets in inflammatory bowel diseases: a clinical approach. World J Gastroenterol. 2014;20(12):3180-90. https://doi.org/10.3748/wjg.v20.i12.3180.
https://doi.org/10.3748/wjg.v20.i12.3180...
). Proteomic studies have identified that more than 300 proteins accumulated in the granules of activated PLT (3333. Senzel L, Gnatenko DV, Bahou WF. The platelet proteome. Curr Opin Hematol. 2009;16(5):329-33. https://doi.org/10.1097/MOH.0b013e32832e9dc6.
https://doi.org/10.1097/MOH.0b013e32832e...
). For example, P-selectin is a member of the CAMs family mainly produced in PLT, which is also detected in patients with IBD. P-selectin can bind to PSGL-1 in leukocytes (3232. Voudoukis E, Karmiris K, Koutroubakis IE. Multipotent role of platelets in inflammatory bowel diseases: a clinical approach. World J Gastroenterol. 2014;20(12):3180-90. https://doi.org/10.3748/wjg.v20.i12.3180.
https://doi.org/10.3748/wjg.v20.i12.3180...
). Moreover, it can also induce tissue factor (TF) generation, stimulating the release of PDMPs bearing TF by leukocytes (3434. Celi A, Pellegrini G, Lorenzet R, De Blasi A, Ready N, Furie BC, et al. P-selectin induces the expression of tissue factor on monocytes. Proc Natl Acad Sci U S A. 1994;91(19):8767-71. https://doi.org/10.1073/pnas.91.19.8767.
https://doi.org/10.1073/pnas.91.19.8767...
). This may support the evidence of P-selectin in IBD pathogenesis. In addition, as a member of the family of CD40, sCD40L is believed to be produced and released only by activated PLT in IBD patients. Increased levels of CD40L(+) PLT and sCD40L are demonstrated in IBD (3535. Danese S, Katz JA, Saibeni S, Papa A, Gasbarrini A, Vecchi M, et al. Activated platelets are the source of elevated levels of soluble CD40 ligand in the circulation of inflammatory bowel disease patients. Gut. 2003;52(10):1435-41. https://doi.org/10.1136/gut.52.10.1435.
https://doi.org/10.1136/gut.52.10.1435...
). In an animal experiment, Vowinkel et al. found that CD40 deficient mice experienced significantly milder dextran sodium sulfate (DSS) colitis compared to wild-type littermates (3636. Vowinkel T, Anthoni C, Wood KC, Stokes KY, Russell J, Gray L, et al. CD40-CD40 ligand mediates the recruitment of leukocytes and platelets in the inflamed murine colon. Gastroenterology. 2007;132(3):955-65. https://doi.org/10.1053/j.gastro.2006.12.027.
https://doi.org/10.1053/j.gastro.2006.12...
). These immune functions of PLT lay the foundation for their role in IBD.
Our study demonstrated the significance of PLT as an important indicator of inflammation in CD; however, some limitations still exist. Firstly, the main limitation of the study was related to the lack of endoscopic examination. The absence of endoscopic examination data led to the inability to understand the severity and healing of the colonic mucosa, thereby making it impossible to combine PLT, disease activity score, and endoscopic examination for disease assessment. This factor also made our results less reliable. Secondly, the PLT cut-off value for CD was 298*10E9/L in our study, which is almost the normal upper limit of PLT. We require more cases to improve the cut-off value. In addition, we need more data of moderate and severe CD patients to improve the PLT evaluation system. Second, although PLT cannot independently reflect the severity of UC, more data is needed to support our result. In the case of excluding anemia in UC patients, PLT can still be used as a reference index to reflect the disease activity to some extent.
In conclusion, PLT can reflect the disease severity of CD, while there is a lack of evidence regarding this finding in UC. The higher the PLT count, the more serious the CD. Furthermore, we need more multi-center research and data to support our results because it is possible that PLT can reflect the severity of UC independently.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (81700485, 81600414) and the Natural Science Foundation of Zhejiang Province (LQ16H030001).
REFERENCES
-
1Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361(21):2066-78. https://doi.org/10.1056/NEJMra0804647
» https://doi.org/10.1056/NEJMra0804647 -
2Bouma G, Strober W. The immunological and genetic basis of inflammatory bowel disease. Nat Rev Immunol. 2003;3(7):521-33. https://doi.org/10.1038/nri1132
» https://doi.org/10.1038/nri1132 -
3Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, Ramos R, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001;411(6837):603-6. https://doi.org/10.1038/35079114
» https://doi.org/10.1038/35079114 -
4Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126(6):1504-17. https://doi.org/10.1053/j.gastro.2004.01.063
» https://doi.org/10.1053/j.gastro.2004.01.063 -
5Danese S, Motte Cd Cde L, Fiocchi C. Platelets in inflammatory bowel disease: clinical, pathogenic, and therapeutic implications. Am J Gastroenterol. 2004;99(5):938-45. https://doi.org/10.1111/j.1572-0241.2004.04129.x
» https://doi.org/10.1111/j.1572-0241.2004.04129.x -
6Fiocchi C. Inflammatory bowel disease: etiology and pathogenesis. Gastroenterology. 1998;115(1):182-205. https://doi.org/10.1016/S0016-5085(98)70381-6
» https://doi.org/10.1016/S0016-5085(98)70381-6 -
7Huang HS, Chang HH. Platelets in inflammation and immune modulations: functions beyond hemostasis. Arch Immunol Ther Exp. 2012;60(6):443-51. https://doi.org/10.1007/s00005-012-0193-y
» https://doi.org/10.1007/s00005-012-0193-y -
8Cognasse F, Lafarge S, Chavarin P, Acquart S, Garraud O. Lipopolysaccharide induces sCD40L release through human platelets TLR4, but not TLR2 and TLR9. Intensive Care Med. 2007;33(2):382-4. https://doi.org/10.1007/s00134-006-0488-8
» https://doi.org/10.1007/s00134-006-0488-8 -
9Smyth SS, McEver RP, Weyrich AS, Morrell CN, Hoffman MR, Arepally GM, et al. Platelet functions beyond hemostasis. J Thromb Haemost. 2009;7(11):1759-66. https://doi.org/10.1111/j.1538-7836.2009.03586.x
» https://doi.org/10.1111/j.1538-7836.2009.03586.x -
10Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392(6673):245-52. https://doi.org/10.1038/32588
» https://doi.org/10.1038/32588 -
11Bernstein CN, Blanchard JF, Rawsthorne P, Yu N. The prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study. Am J Gastroenterol. 2001;96(4):1116-22. https://doi.org/10.1111/j.1572-0241.2001.03756.x
» https://doi.org/10.1111/j.1572-0241.2001.03756.x -
12Gasche C, Lomer MC, Cavill I, Weiss G. Iron, anaemia, and inflammatory bowel diseases. Gut. 2004;53(8):1190-7. https://doi.org/10.1136/gut.2003.035758
» https://doi.org/10.1136/gut.2003.035758 -
13Kulnigg S, Gasche C. Systematic review: managing anaemia in Crohn's disease. Aliment Pharmacol Ther. 2006;24(11-12):1507-23. https://doi.org/10.1111/j.1365-2036.2006.03146.x
» https://doi.org/10.1111/j.1365-2036.2006.03146.x -
14Bager P, Befrits R, Wikman O, Lindgren S, Moum B, Hjortswang H, et al. The prevalence of anemia and iron deficiency in IBD outpatients in Scandinavia. Scand J Gastroenterol. 2011;46(3):304-9. https://doi.org/10.3109/00365521.2010.533382
» https://doi.org/10.3109/00365521.2010.533382 -
15Murawska N, Fabisiak A, Fichna J. Anemia of Chronic Disease and Iron Deficiency Anemia in Inflammatory Bowel Diseases: Pathophysiology, Diagnosis, and Treatment. Inflamm Bowel Dis. 2016;22(5):1198-208. https://doi.org/10.1097/MIB.0000000000000648
» https://doi.org/10.1097/MIB.0000000000000648 -
16Bernstein CN, Fried M, Krabshuis JH, Cohen H, Eliakim R, Fedail S, et al. World Gastroenterology Organization Practice Guidelines for the diagnosis and management of IBD in 2010. Inflamm Bowel Dis. 2010;16(1):112-24. https://doi.org/10.1002/ibd.21048
» https://doi.org/10.1002/ibd.21048 -
17Iborra M, Beltrán B, Nos P. Noninvasive Testing for Mucosal Inflammation in Inflammatory Bowel Disease. Gastrointest Endosc Clin N Am. 2016;26(4):641-56. https://doi.org/10.1016/j.giec.2016.06.005
» https://doi.org/10.1016/j.giec.2016.06.005 -
18Gionchetti P, Dignass A, Danese S, Magro Dias FJ, Rogler G, Lakatos PL, et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn's Disease 2016: Part 2: Surgical Management and Special Situations. J Crohns Colitis. 2017;11(2):135-49. https://doi.org/10.1093/ecco-jcc/jjw169
» https://doi.org/10.1093/ecco-jcc/jjw169 -
19Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, et al. Third European Evidence-Based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders. J Crohns Colitis. 2017;11(6):649-70. https://doi.org/10.1093/ecco-jcc/jjx008
» https://doi.org/10.1093/ecco-jcc/jjx008 -
20Cowman J, Dunne E, Oglesby I, Byrne B, Ralph A, Voisin B, et al. Age-related changes in platelet function are more profound in women than in men. Sci Rep. 2015;5:12235. https://doi.org/10.1038/srep12235
» https://doi.org/10.1038/srep12235 -
21Roodman GD, Bird A, Hutzler D, Montgomery W. Tumor necrosis factor-alpha and hematopoietic progenitors: effects of tumor necrosis factor on the growth of erythroid progenitors CFU-E and BFU-E and the hematopoietic cell lines K562, HL60, and HEL cells. Exp Hematol. 1987;15(9):928-35.
-
22La Ferla K, Reimann C, Jelkmann W, Hellwig-Burgel T. Inhibition of erythropoietin gene expression signaling involves the transcription factors GATA-2 and NF-kappaB. FASEB J. 2002;16(13):1811-3. https://doi.org/10.1096/fj.02-0168fje
» https://doi.org/10.1096/fj.02-0168fje -
23Nakano Y, Imagawa S, Matsumoto K, Stockmann C, Obara N, Suzuki N, et al. Oral administration of K-11706 inhibits GATA binding activity, enhances hypoxia-inducible factor 1 binding activity, and restores indicators in an in vivo mouse model of anemia of chronic disease. Blood. 2004;104(13):4300-7. https://doi.org/10.1182/blood-2004-04-1631
» https://doi.org/10.1182/blood-2004-04-1631 -
24Rusten LS, Jacobsen SE. Tumor necrosis factor (TNF)-alpha directly inhibits human erythropoiesis in vitro: role of p55 and p75 TNF receptors. Blood. 1995;85(4):989-96. https://doi.org/10.1182/blood.V85.4.989.bloodjournal854989
» https://doi.org/10.1182/blood.V85.4.989.bloodjournal854989 -
25Basseri RJ, Nemeth E, Vassilaki ME, Basseri B, Enayati P, Shaye O, et al. Hepcidin is a key mediator of anemia of inflammation in Crohn's disease. J Crohns Colitis. 2013;7(8):e286-91. https://doi.org/10.1016/j.crohns.2012.10.013
» https://doi.org/10.1016/j.crohns.2012.10.013 -
26Di Sabatino A, Santilli F, Guerci M, Simeone P, Ardizzone S, Massari A, et al. Oxidative stress and thromboxane-dependent platelet activation in inflammatory bowel disease: effects of anti-TNF-alpha treatment. Thromb Haemost. 2016;116(3):486-95. https://doi.org/10.1160/TH16-02-0167
» https://doi.org/10.1160/TH16-02-0167 -
27Youssefian T, Drouin A, Massé JM, Guichard J, Cramer EM. Host defense role of platelets: engulfment of HIV and Staphylococcus aureus occurs in a specific subcellular compartment and is enhanced by platelet activation. Blood. 2002;99(11):4021-9. https://doi.org/10.1182/blood-2001-12-0191
» https://doi.org/10.1182/blood-2001-12-0191 -
28Heits F, Stahl M, Ludwig D, Stange EF, Jelkmann W. Elevated serum thrombopoietin and interleukin-6 concentrations in thrombocytosis associated with inflammatory bowel disease. J Interferon Cytokine Res. 1999;19(7):757-60. https://doi.org/10.1089/107999099313604
» https://doi.org/10.1089/107999099313604 -
29Kaushansky K. Determinants of platelet number and regulation of thrombopoiesis. Hematology Am Soc Hematol Educ Program. 2009;147-52. https://doi.org/10.1182/asheducation-2009.1.147
» https://doi.org/10.1182/asheducation-2009.1.147 -
30Collins CE, Cahill MR, Newland AC, Rampton DS. Platelets circulate in an activated state in inflammatory bowel disease. Gastroenterology. 1994;106(4):840-5. https://doi.org/10.1016/0016-5085(94)90741-2
» https://doi.org/10.1016/0016-5085(94)90741-2 -
31Collins CE, Rampton DS, Rogers J, Williams NS. Platelet aggregation and neutrophil sequestration in the mesenteric circulation in inflammatory bowel disease. Eur J Gastroenterol Hepatol. 1997;9(12):1213-7.
-
32Voudoukis E, Karmiris K, Koutroubakis IE. Multipotent role of platelets in inflammatory bowel diseases: a clinical approach. World J Gastroenterol. 2014;20(12):3180-90. https://doi.org/10.3748/wjg.v20.i12.3180
» https://doi.org/10.3748/wjg.v20.i12.3180 -
33Senzel L, Gnatenko DV, Bahou WF. The platelet proteome. Curr Opin Hematol. 2009;16(5):329-33. https://doi.org/10.1097/MOH.0b013e32832e9dc6
» https://doi.org/10.1097/MOH.0b013e32832e9dc6 -
34Celi A, Pellegrini G, Lorenzet R, De Blasi A, Ready N, Furie BC, et al. P-selectin induces the expression of tissue factor on monocytes. Proc Natl Acad Sci U S A. 1994;91(19):8767-71. https://doi.org/10.1073/pnas.91.19.8767
» https://doi.org/10.1073/pnas.91.19.8767 -
35Danese S, Katz JA, Saibeni S, Papa A, Gasbarrini A, Vecchi M, et al. Activated platelets are the source of elevated levels of soluble CD40 ligand in the circulation of inflammatory bowel disease patients. Gut. 2003;52(10):1435-41. https://doi.org/10.1136/gut.52.10.1435
» https://doi.org/10.1136/gut.52.10.1435 -
36Vowinkel T, Anthoni C, Wood KC, Stokes KY, Russell J, Gray L, et al. CD40-CD40 ligand mediates the recruitment of leukocytes and platelets in the inflamed murine colon. Gastroenterology. 2007;132(3):955-65. https://doi.org/10.1053/j.gastro.2006.12.027
» https://doi.org/10.1053/j.gastro.2006.12.027
Publication Dates
-
Publication in this collection
10 July 2020 -
Date of issue
2020
History
-
Received
24 Oct 2019 -
Accepted
26 Mar 2020