Abstract
Considering that female sexual hormones may modulate the inflammatory response and also exhibit direct effects on the cells of the immune system, herein, we intend to discuss the sex differences and the role of estradiol in modulating the lung and systemic inflammatory response, focusing on its possible application as a treatment modality for SARS-CoV-2 patients. COVID-19 patients develop severe hypoxemia early in the course of the disease, which is silent most of the time. Small fibrinous thrombi in pulmonary arterioles and a tumefaction of endothelial were observed in the autopsies of fatal COVID-19 cases. Studies showed that the viral infection induces a vascular process in the lung, which included vasodilation and endothelial dysfunction. Further, the proportions of CD4+ T and CD8+ T lymphocytes were strongly reduced in patients with severe SARS-CoV-2 infection. Estradiol is connected with CD4+ T cell numbers and increases T-reg cell populations, affecting immune responses to infection. It is known that estradiol exerts a protective effect on endothelial function, activating the generation of nitric oxide (NO) via endothelial nitric oxide synthase. Estrogen attenuates the vasoconstrictor response to various stimuli and induces vasodilation in the pulmonary vasculature during stress situations like hypoxia. It exerts a variety of rapid actions, which are initiated after its coupling with membrane receptors, which in turn, may positively modulate vascular responses in pulmonary disease and help to maintain microvascular flow. Direct and indirect mechanisms underlying the effects of estradiol were investigated, and the results point to a possible protective effect of estradiol against COVID-19, indicating that it may be considered as an adjuvant therapeutic element for the treatment of patients affected by the novel coronavirus.
17β-Estradiol; COVID-19; Infection; Coagulation; Inflammation
INTRODUCTION
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), a novel coronavirus, is responsible for the pandemic viral disease outbreak that originated in Wuhan, China, in December 2019. The disease is characterized by severe acute respiratory syndrome, and the virus has already infected more than 3 million people worldwide. No therapies have been shown to be effective to date (11. Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review. JAMA. 2020. https://doi.org/10.1001/jama.2020.6019.
https://doi.org/10.1001/jama.2020.6019...
). Data regarding the clinical management of the disease have been published, some of which have demonstrated that there are differences in prevalence and mortality regarding sex (22. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-81. https://doi.org/10.1016/S2213-2600(20)30079-5.
https://doi.org/10.1016/S2213-2600(20)30...
3. Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. https://doi.org/10.1136/bmj.m1091.
https://doi.org/10.1136/bmj.m1091...
-44. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20. https://doi.org/10.1056/NEJMoa2002032.
https://doi.org/10.1056/NEJMoa2002032...
). There is a higher predominance of men affected in several countries (55. Global Health [Internet]. Available from: https://globalhealth5050.org/covid19/
https://globalhealth5050.org/covid19/...
); in Italy, a prevalence of 70% of men among deceased people was reported (66. La Vignera S, Cannarella R, Condorelli RA, Torre F, Aversa A, Calogero AE. Sex-Specific SARS-CoV-2 Mortality: Among Hormone-Modulated ACE2 Expression, Risk of Venous Thromboembolism and Hypovitaminosis D. Int J Mol Sci. 2020;21(8). pii: E2948. https://doi.org/10.3390/ijms21082948.
https://doi.org/10.3390/ijms21082948...
). Recent data reported by the New York City Department of Health and Mental Hygiene (77. New York Health [Internet]. Available from: https://www1.nyc.gov/site/doh/covid/covid-19-data.page
https://www1.nyc.gov/site/doh/covid/covi...
) confirmed the higher prevalence and mortality of the disease in men. Moreover, a study of nine pregnant women infected with SARS-CoV-2 showed that the infection did not evolve to severe coronavirus disease 2019 (COVID-19) during the pregnancy (88. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809-15. https://doi.org/10.1016/S0140-6736(20)30360-3.
https://doi.org/10.1016/S0140-6736(20)30...
).
Although there is evidence that the immune response (innate and adaptive) differs between men and women, sexual dimorphism does not receive deserved attention as a potential factor for understanding the different immune responses observed between men and women (99. Fish EN. The X-files in immunity: sex-based differences predispose immune responses. Nat Rev Immunol. 2008;8(9):737-44. https://doi.org/10.1038/nri2394.
https://doi.org/10.1038/nri2394...
,1010. Roved J, Westerdahl H, Hasselquist D. Sex differences in immune responses: Hormonal effects, antagonistic selection, and evolutionary consequences. Horm Behav. 2017;88:95-105. https://doi.org/10.1016/j.yhbeh.2016.11.017.
https://doi.org/10.1016/j.yhbeh.2016.11....
). In fact, clinical studies show that women have a lower incidence of pneumonia, sepsis, and multiple organ failure than men (1111. Grossman CJ. Interactions between the gonadal steroids and the immune system. Science. 1985;227(4684):257-61. https://doi.org/10.1126/science.3871252.
https://doi.org/10.1126/science.3871252...
12. Olsen NJ, Kovacs WJ. Gonadal steroids and immunity. Endocr Rev. 1996;17(4):369-84. https://doi.org/10.1210/edrv-17-4-369.
https://doi.org/10.1210/edrv-17-4-369...
-1313. Schröder J, Kahlke V, Book M, Stüber F. Gender differences in sepsis: genetically determined? Shock. 2000;14(3):307-10. https://doi.org/10.1097/00024382-200014030-00011.
https://doi.org/10.1097/00024382-2000140...
). There are several reports on the participation of female sex hormones in mediating the repercussions caused by trauma followed by hemorrhagic shock (1414. Al-Tarrah K, Moiemen N, Lord J. The influence of sex steroid hormones on the response to trauma and burn injury. Burn Trauma. 2017;5:29. https://doi.org/10.1186/s41038-017-0093-9.
https://doi.org/10.1186/s41038-017-0093-...
15. Angele MK, Schwacha MG, Ayala A, Chaudry IH. Effect of gender and sex hormones on immune responses following shock. Shock. 2000;14(2):81-90. https://doi.org/10.1097/00024382-200014020-00001.
https://doi.org/10.1097/00024382-2000140...
16. Angele MK, Frantz MC, Chaudry IH. Gender and sex hormones influence the response to trauma and sepsis: potential therapeutic approaches. Clinics. 2006;61(5):479-88. https://doi.org/10.1590/S1807-59322006000500017.
https://doi.org/10.1590/S1807-5932200600...
17. Chaudry IH, Samy TS, Schwacha MG, Wang P, Rue LW, Bland KI. Endocrine targets in experimental shock. J Trauma. 2003;54(5 Suppl):S118-25. https://doi.org/10.1097/01.TA.0000064511.14322.F1.
https://doi.org/10.1097/01.TA.0000064511...
18. Frink M, Pape HC, van Griensven M, Krettek C, Chaudry IH, Hildebrand F. Influence of sex and age on mods and cytokines after multiple injuries. Shock. 2007;27(2):151-6. https://doi.org/10.1097/01.shk.0000239767.64786.de.
https://doi.org/10.1097/01.shk.000023976...
19. Hildebrand F, Thobe BM, Hubbard WJ, Choudhry MA, Pape HC, Chaudry IH. Effects of 17beta-estradiol and flutamide on splenic macrophages and splenocytes after trauma-hemorrhage. Cytokine. 2006;36(3-4):107-14. https://doi.org/10.1016/j.cyto.2006.11.002.
https://doi.org/10.1016/j.cyto.2006.11.0...
20. Hsieh YC, Frink M, Thobe BM, Hsu JT, Choudhry MA, Schwacha MG, et al. 17Beta-estradiol downregulates Kupffer cell TLR4-dependent p38 MAPK pathway and normalizes inflammatory cytokine production following trauma-hemorrhage. Mol Immunol. 2007;44(9):2165-72. https://doi.org/10.1016/j.molimm.2006.11.019.
https://doi.org/10.1016/j.molimm.2006.11...
21. Knöferl MW, Jarrar D, Angele MK, Ayala A, Schwacha MG, Bland KI, et al. 17 beta-Estradiol normalizes immune responses in ovariectomized females after trauma-hemorrhage. Am J Physiol Cell Physiol. 2001;281(4):C1131-8. https://doi.org/10.1152/ajpcell.2001.281.4.C1131.
https://doi.org/10.1152/ajpcell.2001.281...
22. Knöferl MW, Angele MK, Diodato MD, Schwacha MG, Ayala A, Cioffi WG, et al. Female sex hormones regulate macrophage function after trauma-hemorrhage and prevent increased death rate from subsequent sepsis. Ann Surg. 2002;235(1):105-12. https://doi.org/10.1097/00000658-200201000-00014.
https://doi.org/10.1097/00000658-2002010...
-2323. Moeinpour F, Choudhry MA, Kawasaki T, Timares L, Schwacha MG, Bland KI, et al. 17 Beta-estradiol normalizes Toll receptor 4, mitogen activated protein kinases and inflammatory response in epidermal keratinocytes following trauma-hemorrhage. Mol Immunol. 2007;44(13):3317-23. https://doi.org/10.1016/j.molimm.2007.02.023.
https://doi.org/10.1016/j.molimm.2007.02...
). Important differences exist in epidemiology, pathophysiology, and treatment of cardiovascular diseases, such as coronary artery disease, hypertension, cardiomyopathy, and heart failure. Cardiovascular disorders are also more severe in postmenopausal women (2424. Stangl V, Baumann G, Stangl K. Coronary atherogenic risk factors in women. Eur Heart J. 2002;23(22):1738-52. https://doi.org/10.1053/euhj.2002.3329.
https://doi.org/10.1053/euhj.2002.3329...
).
Suba (2525. Suba Z. Prevention and therapy of COVID-19 via exogenous estrogen treatment for both male and female patients. J Pharm Pharm Sci. 2020;23(1):75-85. https://doi.org/10.18433/jpps31069.
https://doi.org/10.18433/jpps31069...
) revealed that epidemiological data from SARS and MERS CoV epidemics indicated that the outcome of human coronavirus infections is strongly sex-dependent, suggesting the role of a strong protective estrogen signal in adult female patients compared to age-matched males. In this context, considering that female sexual hormones may modulate the inflammatory response and also exhibit direct effects on the cells of the immune system, here we intend to discuss the sex differences and the role of estradiol in modulating the lung and the systemic inflammatory response and its possible application as a treatment for SARS-CoV-2 patients.
The effects of SARS-CoV-2
The inflammatory response is a natural defense mechanism of the body to remove harmful stimuli such as pathogens and initiate the recovery process. SARS-CoV-2, the new coronavirus that induces COVID-19, enters the body through the interaction between the S protein on the virus surface and angiotensin-converting enzyme-2 (ACE-2) molecules expressed in epithelial cells in the lungs (2626. Xu X, Chen P, Wang J, Feng J, Zhou H, Li X, et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63(3):457-60. https://doi.org/10.1007/s11427-020-1637-5.
https://doi.org/10.1007/s11427-020-1637-...
). After SARS-CoV-2 replication in the respiratory and intestinal epithelium cells (2727. Wujtewicz M, Dylczyk-Sommer A, Aszkiełowicz A, Zdanowski S, Piwowarczyk S, Owczuk R. COVID-19 - what should anaethesiologists and intensivists know about it? Anaesthesiol Intensive Ther. 2020;52(1):34-41. https://doi.org/10.5114/ait.2020.93756.
https://doi.org/10.5114/ait.2020.93756...
), it can induce an immune response that causes several alterations in the lung including inflammation and respiratory failure. The binding of the COVID-19 protein to ACE-2 has been shown to downregulate its enzymatic activity and decrease angiotensin production (2828. Mo P, Xing Y, Xiao Y, Deng L, Zhao Q, Wang H, et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020. pii: ciaa270. https://doi.org/10.1093/cid/ciaa270.
https://doi.org/10.1093/cid/ciaa270...
). This mechanism may be involved in the pathogenesis of pulmonary hypertension and insufficiency caused by SARS-CoV-2 infection (2929. Gurwitz D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev Res. 2020. https://doi.org/10.1002/ddr.21656.
https://doi.org/10.1002/ddr.21656...
).
The inflammatory process is accompanied by the activation of the coagulation system, which is characterized by the interaction of coagulation factors, and as observed in severe cases of sepsis, could lead to a disseminated intravascular coagulation process. As recent studies described, COVID-19 is commonly complicated with coagulopathy, and disseminated intravascular coagulation (DIC) may exist in the majority of deaths. In addition to pulmonary pneumonia and inflammation, the presence of vascular dysfunction and thrombosis have been noted in severe COVID-19 patients (3030. Zhang H, Zhou P, Wei Y, Yue H, Wang Y, Hu M, et al. Histopathologic Changes and SARS-CoV-2 Immunostaining in the Lung of a Patient With COVID-19. Ann Intern Med. 2020. https://doi.org/10.7326/M20-0533.
https://doi.org/10.7326/M20-0533...
31. Barrett CD, Moore HB, Yaffe MB, Moore EE. ISTH interim guidance on recognition and management of coagulopathy in COVID-19: A Comment. J Thromb Haemost. 2020. https://doi.org/10.1111/jth.14860.
https://doi.org/10.1111/jth.14860...
-3232. Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020. pii: blood.2020006000. https://doi.org/10.1182/blood.2020006000.
https://doi.org/10.1182/blood.2020006000...
).
Because ACE-2, the receptor necessary for virus uptake, is expressed in the cardiovascular system (3333. Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, et al. Angiotensin Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2. Circ Res. 2020;126(10):1456-74. https://doi.org/10.1161/CIRCRESAHA.120.317015.
https://doi.org/10.1161/CIRCRESAHA.120.3...
), it is expected that this tissue is also susceptible to SARS-CoV-2 infection. Some new studies showed that COVID induces a vascular process in the lung, which includes vasodilation and endothelial dysfunction (3434. Leisman DE, Deutschman CS, Legrand M. Facing COVID-19 in the ICU: vascular dysfunction, thrombosis, and dysregulated inflammation. Intensive Care Med. 2020. https://doi.org/10.1007/s00134-020-06059-6.
https://doi.org/10.1007/s00134-020-06059...
). In this regard, Caruso et al. (3535. Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, et al. Chest CT Features of COVID-19 in Rome, Italy. Radiology. 2020. https://doi.org/10.1148/radiol.2020201237.
https://doi.org/10.1148/radiol.202020123...
) observed subsegmental vascular enlargement via computer tomography of patients with COVID-19. The presence of thrombosis or acute pulmonary embolism in COVID-19 patients associated with increased respiratory dead space was also reported by Chen et al. (3636. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;30(5):2620-9. https://doi.org/10.1172/JCI137244.
https://doi.org/10.1172/JCI137244...
).
Similar to the disease caused by SARS-CoV identified in 2002, pulmonary involvement is the dominant clinical feature observed in COVID-19. Zhang et al. (3030. Zhang H, Zhou P, Wei Y, Yue H, Wang Y, Hu M, et al. Histopathologic Changes and SARS-CoV-2 Immunostaining in the Lung of a Patient With COVID-19. Ann Intern Med. 2020. https://doi.org/10.7326/M20-0533.
https://doi.org/10.7326/M20-0533...
) observed the presence of Rp3 NP SARS-CoV-2 protein in alveolar epithelium cells, including those that were peeled and injured in the alveolar space in lung biopsies. These authors also observed diffuse alveolar damage, epithelial cells peeling with type II reactive hyperplasia of pneumocytes, and fibrinous exudate associated with interstitial fibrosis and chronic inflammatory infiltrate.
Radiological findings in SARS-CoV-2-infected patients have been well-reported in several articles, and the consensus is that COVID-19 induces pneumonia with bilateral lung involvement and ground-glass opacity, the latter being one of the most important radiological characteristic of COVID-19 that can be present even in asymptomatic patients (3030. Zhang H, Zhou P, Wei Y, Yue H, Wang Y, Hu M, et al. Histopathologic Changes and SARS-CoV-2 Immunostaining in the Lung of a Patient With COVID-19. Ann Intern Med. 2020. https://doi.org/10.7326/M20-0533.
https://doi.org/10.7326/M20-0533...
,3737. Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425-34. https://doi.org/10.1016/S1473-3099(20)30086-4.
https://doi.org/10.1016/S1473-3099(20)30...
38. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. https://doi.org/10.1016/j.ijantimicag.2020.105924.
https://doi.org/10.1016/j.ijantimicag.20...
-3939. Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47(5):1275-80. https://doi.org/10.1007/s00259-020-04735-9.
https://doi.org/10.1007/s00259-020-04735...
).
According to Mason (4040. Mason RJ. Pathogenesis of COVID-19 from a cell biologic perspective. Eur Respir J. 2020;55(4) pii: 2000607. https://doi.org/10.1183/13993003.00607-2020.
https://doi.org/10.1183/13993003.00607-2...
), the pathogenesis of COVID-19 can be divided into three stages. The first asymptomatic phase occurs when the inhaled virus SARS-CoV-2 starts to replicate in the epithelial cells in the nasal cavity. The second phase occurs when the virus migrates through the lung and a more vigorous innate immune response is triggered. The last phase is manifested by hypoxia, ground glass infiltrate, and progression to respiratory failure. A range of 20% to 30% of infected patients will progress to stage 3 of the disease and will develop pulmonary infiltrates that can also evolve into acute respiratory distress syndrome (ARDS). ARDS is an acute inflammatory lung injury, characterized by increased pulmonary vascular permeability, enlarged lung weight, and loss of aerated lung tissue (4141. ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526-33. https://doi.org/10.1001/jama.2012.5669.
https://doi.org/10.1001/jama.2012.5669...
). ARDS in its most severe form presents with intense pulmonary inflammation where there is severe hypoxemia (4242. Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149(3 Pt 1):818-24. https://doi.org/10.1164/ajrccm.149.3.7509706.
https://doi.org/10.1164/ajrccm.149.3.750...
). In terms of diagnosis, ARDS is characterized by a Pa02/Fi02 ratio equal to or less than 200 mmHg. In essence, the mechanisms underlying the triggering of ARDS are limited to damage to the alveolar epithelium and capillary endothelium (4343. Randhawa R, Bellingan G. Acute lung injury. Anaesth Intensive Care Med. 2007;8(11):477-80. https://doi.org/10.1016/j.mpaic.2007.09.003.
https://doi.org/10.1016/j.mpaic.2007.09....
,4444. Matthay MA, Zemans RL, Zimmerman GA, Arabi YM, Beitler JR, Mercat A, et al. Acute respiratory distress syndrome. Nat Rev Dis Prim. 2019;5(1):18.). There is activation of neutrophils and high levels of proinflammatory cytokine release as well as activation of M1-like macrophages and reactive oxygen and nitrogen species. The incidence of ARDS is higher in older patients (4545. Hecker L. Mechanisms and consequences of oxidative stress in lung disease: therapeutic implications for an aging populace. Am J Physiol Lung Cell Mol Physiol. 2018;314(4):L642-L653. https://doi.org/10.1152/ajplung.00275.2017.
https://doi.org/10.1152/ajplung.00275.20...
), and aging of the lungs may contribute to the higher mortality rate due to SARS-CoV-2 in elderly and immunosuppressed individuals.
The severe form of COVD-19 is well-characterized by dyspnea, hypoxemia, and pulmonary tissue damage. In addition, 67-85% of critically ill patients admitted to the intensive care unit (ICU) with COVID-19 will develop ARDS, and this will be the cause of death (4646. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. https://doi.org/10.1016/S0140-6736(20)30183-5.
https://doi.org/10.1016/S0140-6736(20)30...
,4747. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020. https://doi.org/10.1007/s00134-020-05991-x.
https://doi.org/10.1007/s00134-020-05991...
). Huang et al. (4646. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. https://doi.org/10.1016/S0140-6736(20)30183-5.
https://doi.org/10.1016/S0140-6736(20)30...
) reported that dyspnea and lymphopenia was present in more than 50% of infected patients, and all of them showed abnormal findings on a chest CT scan. Considering the inflammatory responses, Lagunas-Rangel et al. (4848. Lagunas‐Rangel FA, Chávez‐Valencia V. High IL‐6/IFN‐γ ratio could be associated with severe disease in COVID‐19 patients. J Med Virol. 2020. https://doi.org/10.1002/jmv.25900.
https://doi.org/10.1002/jmv.25900...
) suggested that patients with severe COVID-19 show a cytokine storm with acute increased levels of IL-2, IL-7, G-CSF, CXCL10, MCP-1, MIP-1α, TNF-α, and IL-6, similar to patients diagnosed with SARS and MERS. Thus, this suggests that mortality could be due to viral hyperinflammation that exacerbates lung damage.
Some evidence associated high IL-6 levels with the severity and mortality of COVID-19 (4949. Zhou Y, Han T, Chen J, Hou C, Hua L, He S, et al. Clinical and Autoimmune Characteristics of Severe and Critical Cases with COVID-19. Clin Transl Sci. 2020. https://doi.org/10.1111/cts.12805.
https://doi.org/10.1111/cts.12805...
,5050. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020. https://doi.org/10.1001/jamainternmed.2020.0994.
https://doi.org/10.1001/jamainternmed.20...
), although the levels of interferon (IFN)-γ tend to be somewhat decreased in severe cases compared with moderate cases. These cytokines are also increased in both the serum and bronchoalveolar lavage as well as in lung tissue from ARDS patients (5151. Pires-Neto RC, Morales MM, Lancas T, Inforsato N, Duarte MIS, Amato MB, et al. Expression of acute-phase cytokines, surfactant proteins, and epithelial apoptosis in small airways of human acute respiratory distress syndrome. J Crit Care. 2013;28(1):111.e9-111.e15. https://doi.org/10.1016/j.jcrc.2012.05.013.
https://doi.org/10.1016/j.jcrc.2012.05.0...
52. Parsons EC, Hough CL, Seymour CW, Cooke CR, Rubenfeld GD, Watkins TR, et al. Red blood cell transfusion and outcomes in patients with acute lung injury, sepsis and shock. Crit Care. 2011;15(5):R221. https://doi.org/10.1186/cc10458.
https://doi.org/10.1186/cc10458...
-5353. Schütte H, Lohmeyer J, Rosseau S, Ziegler S, Siebert C, Kielisch H, et al. Bronchoalveolar and systemic cytokine profiles in patients with ARDS, severe pneumonia and cardiogenic pulmonary oedema. Eur Respir J. 1996;9(9):1858-67. https://doi.org/10.1183/09031936.96.09091858.
https://doi.org/10.1183/09031936.96.0909...
). This alteration in inflammatory response observed in COVID-19 patients could be associated with a reduction in CD4+, CD8+, and NK lymphocytes (3636. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;30(5):2620-9. https://doi.org/10.1172/JCI137244.
https://doi.org/10.1172/JCI137244...
). In this regard, CD4+ T and CD8+ T were strongly reduced in patients with severe COVID-19 compared with those in patients with mild disease (5454. Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, et al. Relationships among lymphocyte subsets, cytokines, and the pulmonary inflammation index in coronavirus (COVID‐19) infected patients. Br J Haematol. 2020;189(3):428-37. https://doi.org/10.1111/bjh.16659.
https://doi.org/10.1111/bjh.16659...
).
Sex differences in immune response and inflammation
Steroid sex hormones may affect the strength of immune responses in opposite directions and result in a general difference between males and females, with stronger immune responses in females than in males (for review see Roved et al. (1010. Roved J, Westerdahl H, Hasselquist D. Sex differences in immune responses: Hormonal effects, antagonistic selection, and evolutionary consequences. Horm Behav. 2017;88:95-105. https://doi.org/10.1016/j.yhbeh.2016.11.017.
https://doi.org/10.1016/j.yhbeh.2016.11....
)). The dominant profile of the immune response may be dependent on hormonal variation during the female sexual cycle. Data indicate that female sex hormones enhance Th2 immune responses and reduce Th1, and this influence has been comprehensively covered in many reviews (99. Fish EN. The X-files in immunity: sex-based differences predispose immune responses. Nat Rev Immunol. 2008;8(9):737-44. https://doi.org/10.1038/nri2394.
https://doi.org/10.1038/nri2394...
,5555. Kovats S. Estrogen receptors regulate innate immune cells and signaling pathways. Cell Immunol. 2015;294(2):63-9. https://doi.org/10.1016/j.cellimm.2015.01.018.
https://doi.org/10.1016/j.cellimm.2015.0...
,5656. Khan D, Ansar Ahmed S. The Immune System Is a Natural Target for Estrogen Action: Opposing Effects of Estrogen in Two Prototypical Autoimmune Diseases. Front Immunol. 2016;6:635. https://doi.org/10.3389/fimmu.2015.00635.
https://doi.org/10.3389/fimmu.2015.00635...
). Females seems to develop stronger cell-dependent and humoral responses to infection and vaccination. The result of these differences can be observed when comparing the incidence of autoimmune diseases between sexes (5757. Fairweather D, Frisancho-Kiss S, Rose NR. Sex differences in autoimmune disease from a pathological perspective. Am J Pathol. 2008;173(3):600-9. https://doi.org/10.2353/ajpath.2008.071008.
https://doi.org/10.2353/ajpath.2008.0710...
), which is higher in females, and also by the observation of higher incidence of sepsis in males in parallel with higher plasma levels of Th1 cytokines (5858. Offner PJ, Moore EE, Biffl WL. Male gender is a risk factor for major infections after Vsurgery. Arch Surg. 1999;134(9):935-8. https://doi.org/10.1001/archsurg.134.9.935.
https://doi.org/10.1001/archsurg.134.9.9...
59. Wichmann MW, Inthorn D, Andress HJ, Schildberg FW. Incidence and mortality of severe sepsis in surgical intensive care patients: the influence of patient gender on disease process and outcome. Intensive Care Med. 2000;26(2):167-72. https://doi.org/10.1007/s001340050041.
https://doi.org/10.1007/s001340050041...
-6060. George RL, McGwin G Jr, Windham ST, Melton SM, Metzger J, Chaudry IH,et al. Age-related gender differential in outcome after blunt or penetrating trauma. Shock. 2003;19(1):28-32. https://doi.org/10.1097/00024382-200301000-00006.
https://doi.org/10.1097/00024382-2003010...
). Also, the incidence of sepsis in postmenopausal women increases to levels almost equal to those seen in age-matched men (6161. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl. J Med. 2003;348(16):1546-54. https://doi.org/10.1056/NEJMoa022139.
https://doi.org/10.1056/NEJMoa022139...
). In addition to hormonal influences, there is an apparent genetic disparity, since females carry two inherently polymorphic X chromosomes, while males have only one polymorphic X chromosome passed from the mother. The random process of X-chromosome inactivation provides females with a broader panel of proteins and enlarges the potential diversity of cell populations (99. Fish EN. The X-files in immunity: sex-based differences predispose immune responses. Nat Rev Immunol. 2008;8(9):737-44. https://doi.org/10.1038/nri2394.
https://doi.org/10.1038/nri2394...
).
In women, the CD4+ T cell numbers are higher (6262. Amadori A, Zamarchi R, De Silvestro G, Forza G, Cavatton G, Danieli GA, et al. Genetic control of the CD4/CD8 T-cell ratio in humans. Nat Med. 1995;1(12):1279-83. https://doi.org/10.1038/nm1295-1279.
https://doi.org/10.1038/nm1295-1279...
), and the ovarian cycle also influences the T reg cell populations with an increased number when estradiol levels are higher (6363. Arruvito L, Sanz M, Banham AH, Fainboim L. Expansion of CD4+CD25+ and FOXP3+ regulatory T cells during the follicular phase of the menstrual cycle: implications for human reproduction. J Immunol. 2007;178(4):2572-8. https://doi.org/10.4049/jimmunol.178.4.2572.
https://doi.org/10.4049/jimmunol.178.4.2...
). These differences are connected to estradiol influence and affect immune responses to infection. In addition, estradiol exerts anti-inflammatory effects on innate immune responses by reducing monocyte and macrophage inflammatory cytokine release (6464. Kramer PR, Kramer SF, Guan G. 17 beta-estradiol regulates cytokine release through modulation of CD16 expression in monocytes and monocyte-derived macrophages. Arthritis Rheum. 2004;50(6):1967-75. https://doi.org/10.1002/art.20309.
https://doi.org/10.1002/art.20309...
), delaying neutrophil apoptosis and enhancing neutrophil annexin-1 expression without increasing their activation (6565. Molloy EJ, O’Neill AJ, Grantham JJ, Sheridan-Pereira M, Fitzpatrick JM, Webb DW, et al. Sex-specific alterations in neutrophil apoptosis: The role of estradiol and progesterone. Blood. 2003;102(7):2653-9. https://doi.org/10.1182/blood-2003-02-0649.
https://doi.org/10.1182/blood-2003-02-06...
,6666. Nadkarni S, Cooper D, Brancaleone V, Bena S, Perretti M. Activation of the annexin A1 pathway underlies the protective effects exerted by estrogen in polymorphonuclear leukocytes. Arterioscler Thromb Vasc Biol. 2011;31(11):2749-59. https://doi.org/10.1161/ATVBAHA.111.235176.
https://doi.org/10.1161/ATVBAHA.111.2351...
). Experimental data confirm that the leukocyte function in females is more efficient than that in males, detecting and eliminating pathogens more rapidly, and that females have higher numbers of tissue macrophages with a greater density of toll-like receptors; female macrophage phagocytosis is more efficient with NADPH oxidase killing, in parallel with an increased population of resident anti-inflammatory T-lymphocytes (6767. Scotland RS, Stables MJ, Madalli S, Watson P, Gilroy DW. Sex differences in resident immune cell phenotype underlie more efficient acute inflammatory responses in female mice. Blood. 2011;118(22):5918-27. https://doi.org/10.1182/blood-2011-03-340281.
https://doi.org/10.1182/blood-2011-03-34...
). The dendritic cell population is also influenced by female sex hormones, with estradiol signaling via estrogen receptor α ER-α to increase the number of new DCs during inflammation (6868. Kovats S. Estrogen receptors regulate an inflammatory pathway of dendritic cell differentiation: mechanisms and implications for immunity. Horm Behav. 2012;62(3):254-62. https://doi.org/10.1016/j.yhbeh.2012.04.011.
https://doi.org/10.1016/j.yhbeh.2012.04....
). In plasmacytoid dendritic cells, which are mostly involved in antiviral responses, estrogen increases the release of type 1 cytokines that are important for an efficient type 1 immune response (6969. Murphy K, Weaver C. Janeway’s Immunobiology. 9th ed. Taylor & Francis Group L, editor. New York: Garland Science; 2017.). The action of estradiol via ER-α also promotes activation of type 1 INF-inducible innate pathways, and the IFN pathway genes are highly expressed in females, regulating innate immunity (5555. Kovats S. Estrogen receptors regulate innate immune cells and signaling pathways. Cell Immunol. 2015;294(2):63-9. https://doi.org/10.1016/j.cellimm.2015.01.018.
https://doi.org/10.1016/j.cellimm.2015.0...
).
Considering lung inflammation, mortality in ARDS is higher in males compared to females (7070. Agarwal R, Aggarwal AN, Gupta D, Behera D, Jindal SK. Etiology and outcomes of pulmonary and extrapulmonary acute lung injury/ARDS in a respiratory ICU in north India. Chest. 2006;130(3):724-9. https://doi.org/10.1378/chest.130.3.724.
https://doi.org/10.1378/chest.130.3.724...
,7171. Moss M, Mannino DM. Race and gender differences in acute respiratory distress syndrome deaths in the United States: an analysis of multiple-cause mortality data (1979-1996). Crit Care Med. 2002;30(8):1679-85. https://doi.org/10.1097/00003246-200208000-00001.
https://doi.org/10.1097/00003246-2002080...
). In the respiratory system, sex steroids have been demonstrated to play important roles in the development and maturation of lungs and maintenance of normal lung function (7272. Asavasupreechar T, Saito R, Miki Y, Edwards DP, Boonyaratanakornkit V, Sasano H. Systemic distribution of progesterone receptor subtypes in human tissues. J Steroid Biochem Mol Biol. 2020;199:105599. https://doi.org/10.1016/j.jsbmb.2020.105599.
https://doi.org/10.1016/j.jsbmb.2020.105...
), and sexual dimorphism impacts the prevalence and incidence of several lung diseases (7373. Fuentes N, Silveyra P. Endocrine regulation of lung disease and inflammation. Exp Biol Med. 2018;243(17-18):1313-22. https://doi.org/10.1177/1535370218816653.
https://doi.org/10.1177/1535370218816653...
). Sex differences were identified in lung physiology and disease and have been studied in animal models. Sex also influences lung development and disease conditions (7474. Carey MA, Card JW, Voltz JW, Germolec DR, Korach KS, Zeldin DC. The impact of sex and sex hormones on lung physiology and disease: lessons from animal studies. Am J Physiol Lung Cell Mol Physiol. 2007;293(2):L272-8. https://doi.org/10.1152/ajplung.00174.2007.
https://doi.org/10.1152/ajplung.00174.20...
). Sex hormones may contribute to the disease pathophysiology or serve as protective factors, depending on the disease involved. Women may be protected from certain age-related biological processes by producing lower levels of reactive oxidant species, important drivers of pathology in age-related pulmonary disease (7575. Nawrot TS, Staessen JA, Gardner JP, Aviv A. Telomere length and possible link to X chromosome. Lancet. 2004;363(9408):507-10. https://doi.org/10.1016/S0140-6736(04)15535-9.
https://doi.org/10.1016/S0140-6736(04)15...
). Pulmonary diseases in women are influenced by age because of the variation of their level of estrogen. Increasing age is associated with higher levels of circulating inflammatory mediators and acute phase proteins. The reduction of estrogen, the increased fat tissue, and the presence of subclinical infections contribute to the proinflammatory status of postmenopausal women. The development and progression of age-related diseases is dependent on mechanisms associated with cellular senescence that may be triggered by telomere shortening, which in women occurs at a slower rate than in men (7676. Gardner M, Bann D, Wiley L, Cooper R, Hardy R, Nitsch D, et al. Gender and telomere length: systematic review and meta-analysis. Exp Gerontol. 2014;51:15-27. https://doi.org/10.1016/j.exger.2013.12.004.
https://doi.org/10.1016/j.exger.2013.12....
).
Substantial evidence supports the anti-inflammatory role of systemic estrogens. The mechanisms behind the female protection from infection are reported to be mediated mainly by sex hormones, in particular 17β-estradiol, that can directly influence synthesis and signal transduction of multiple cytokines in vitro (6767. Scotland RS, Stables MJ, Madalli S, Watson P, Gilroy DW. Sex differences in resident immune cell phenotype underlie more efficient acute inflammatory responses in female mice. Blood. 2011;118(22):5918-27. https://doi.org/10.1182/blood-2011-03-340281.
https://doi.org/10.1182/blood-2011-03-34...
).
17β-estradiol therapeutic effects in experimental models
Experimental investigations of several disease models confirm that higher levels of systemic estrogens promote anti-inflammatory responses. 17-β-estradiol is the predominant estrogen during the reproductive years, both in its total serum concentration and in overall estrogenic activity. Estradiol down-regulates immune functions in endothelial cells, including the stimulation of leukocyte adhesion and migration to infected tissues (7777. Alvarez A, Hermenegildo C, Issekutz AC, Esplugues JV, Sanz MJ. Estrogens inhibit angiotensin II-induced leukocyte-endothelial cell interactions in vivo via rapid endothelial nitric oxide synthase and cyclooxygenase activation. Circ Res. 2002;91(12):1142-50. https://doi.org/10.1161/01.RES.0000046018.23605.3E.
https://doi.org/10.1161/01.RES.000004601...
78. Gao H, Liang M, Bergdahl A, Hamrén A, Lindholm MW, Dahlman-Wright K, et al. Estrogen attenuates vascular expression of inflammation associated genes and adhesion of monocytes to endothelial cells. Inflamm Res. 2006;55(8):349-53. https://doi.org/10.1007/s00011-006-5194-z.
https://doi.org/10.1007/s00011-006-5194-...
-7979. Geraldes P, Gagnon S, Hadjadj S, Merhi Y, Sirois MG, Cloutier I, et al. Estradiol blocks the induction of CD40 and CD40L expression on endothelial cells and prevents neutrophil adhesion: An ERalpha-mediated pathway. Cardiovasc Res. 2006;71(3):566-73. https://doi.org/10.1016/j.cardiores.2006.05.015.
https://doi.org/10.1016/j.cardiores.2006...
). It is known that estrogen plays a protective role in endothelial function (8080. Ma XL, Gao F, Chen J, Christopher TA, Lopez BL, Ohlstein EH, et al. Endothelial protective and antishock effects of a selective estrogen receptor modulator in rats. Am J Physiol Heart Circ Physiol. 2001;280(2):H876-84. https://doi.org/10.1152/ajpheart.2001.280.2.H876.
https://doi.org/10.1152/ajpheart.2001.28...
), activating the generation of nitric oxide (NO) via endothelial nitric oxide synthase (eNOS), which is mediated by mechanisms that lead to an increase in NO bioavailability through the induction of gene transcription and activation of eNOS via phosphatidylinositol-3-kinase/serine-threonine kinase (PI3K/AKT) (8181. Novella S, Dantas AP, Segarra G, Medina P, Hermenegildo C. Vascular Aging in Women: is Estrogen the Fountain of Youth? Front Physiol. 2012;3:165. https://doi.org/10.3389/fphys.2012.00165.
https://doi.org/10.3389/fphys.2012.00165...
). Still, studies by our group using an aortic occlusion model in male rats indicate that previous treatment with estradiol has a beneficial effect on the course of mesenteric ischemia and intestinal injury, preventing mortality due to systemic inflammation (8282. Rocha de Sousa PT, Breithaupt-Faloppa AC, de Jesus Correia C, Simão RR, Ferreira SG, Fiorelli AI, et al. 17β -Estradiol prevents mesenteric injury induced by occlusion of the proximal descending aorta in male rats. J Vasc Surg. 2018;67(2):597-606. https://doi.org/10.1016/j.jvs.2016.12.125.
https://doi.org/10.1016/j.jvs.2016.12.12...
). Additionally, in an intestinal ischemia and reperfusion (I/R) model, results indicate that female sex hormones, notably estradiol, exert a protective effect on preventing/reducing lung and intestinal injuries caused by systemic inflammation after ischemic trauma (8383. Breithaupt-Faloppa AC, Fantozzi ET, de Assis Ramos MM, Vitoretti LB, Couto GK, Lino-dos-Santos-Franco A, et al. Protective effect of estradiol on acute lung inflammation induced by an intestinal ischemic insult is dependent on nitric oxide. Shock. 2013;40(3):203-9. https://doi.org/10.1097/SHK.0b013e3182a01e24.
https://doi.org/10.1097/SHK.0b013e3182a0...
84. Breithaupt-Faloppa AC, Thais Fantozzi E, Romero DC, Rodrigues Ada S, de Sousa PT, Lino Dos Santos Franco A, et al. Acute effects of estradiol on lung inflammation due to intestinal ischemic insult in male rats. Shock. 2014;41(3):208-13. https://doi.org/10.1097/SHK.0000000000000092.
https://doi.org/10.1097/SHK.000000000000...
-8585. Ricardo-Da-Silva FY, Fantozzi ET, Rodrigues-Garbin S, Oliveira-Filho RM, Vargaftig BB, Breithaupt-Faloppa AC, et al. Estradiol Modulates Local Gut Injury Induced by Intestinal Ischemia-Reperfusion in Male Rats. Shock. 2017;48(4):477-83. https://doi.org/10.1097/SHK.0000000000000873.
https://doi.org/10.1097/SHK.000000000000...
). Proestrus or estradiol-treated females showed reduced lung damage and inflammation in ischemia and reperfusion models (8686. Deitch EA, Feketeova E, Lu Q, Zaets S, Berezina TL, Machiedo GW, et al. Resistance of the female, as opposed to the male, intestine to I/R-mediated injury is associated with increased resistance to gut-induced distant organ injury. Shock. 2008;29(1):78-83. https://doi.org/10.1097/shk.0b013e318063e98a.
https://doi.org/10.1097/shk.0b013e318063...
,8787. Mrazkova H, Lischke R, Herget J. Influence of gender on ischemia-reperfusion injury in lungs in an animal model. Physiol Res. 2016;65(6):953-8. https://doi.org/10.33549/physiolres.933273.
https://doi.org/10.33549/physiolres.9332...
) and in a hemorrhagic shock model (8888. Raju R, Chaudry IH. Sex steroids receptor antagonist: their use as adjuncts after trauma-hemorrhage for improving immune/cardiovascular responses and for decreasing mortality from subsequent sepsis. Anesth Analg. 2008;107(1):159-66. https://doi.org/10.1213/ane.0b013e318163213d.
https://doi.org/10.1213/ane.0b013e318163...
). In addition, treatment with estradiol showed anti-inflammatory action similar to that of glucocorticoids, with reduced expression of transcription factors involved in the inflammatory response and reduced recruitment of neutrophils by decreasing the production of interleukins, such as IL-8, in addition to chemokines and adhesion molecules (6666. Nadkarni S, Cooper D, Brancaleone V, Bena S, Perretti M. Activation of the annexin A1 pathway underlies the protective effects exerted by estrogen in polymorphonuclear leukocytes. Arterioscler Thromb Vasc Biol. 2011;31(11):2749-59. https://doi.org/10.1161/ATVBAHA.111.235176.
https://doi.org/10.1161/ATVBAHA.111.2351...
,8989. Nadkarni S, McArthur S. Oestrogen and immunomodulation: new mechanisms that impact on peripheral and central immunity. Curr Opin Pharmacol. 2013;13(4):576-81. https://doi.org/10.1016/j.coph.2013.05.007.
https://doi.org/10.1016/j.coph.2013.05.0...
).
Evidence from clinical and experimental studies strongly suggests that estrogens can modulate lung inflammation and allergic reactions, because activation of estrogen receptors modulates immune cells and both innate and adaptive immune responses (5555. Kovats S. Estrogen receptors regulate innate immune cells and signaling pathways. Cell Immunol. 2015;294(2):63-9. https://doi.org/10.1016/j.cellimm.2015.01.018.
https://doi.org/10.1016/j.cellimm.2015.0...
,7373. Fuentes N, Silveyra P. Endocrine regulation of lung disease and inflammation. Exp Biol Med. 2018;243(17-18):1313-22. https://doi.org/10.1177/1535370218816653.
https://doi.org/10.1177/1535370218816653...
). However, the effects of estradiol as a pro or anti-inflammatory factor seem to be dependent on the pathogenesis of the diseases studied. Estradiol plays a critical role in improving outcomes in the settings of trauma, shock, sepsis, myocardial ischemia/reperfusion, and acute lung injury (ALI). Experimental data with an intestinal I/R model show that estradiol treatment in ovariectomized females reduces lung inflammation and exerts these effects by modulating eNOS protein expression in the lungs (8383. Breithaupt-Faloppa AC, Fantozzi ET, de Assis Ramos MM, Vitoretti LB, Couto GK, Lino-dos-Santos-Franco A, et al. Protective effect of estradiol on acute lung inflammation induced by an intestinal ischemic insult is dependent on nitric oxide. Shock. 2013;40(3):203-9. https://doi.org/10.1097/SHK.0b013e3182a01e24.
https://doi.org/10.1097/SHK.0b013e3182a0...
). As permeability edema represents a life-threatening complication of ALI, estradiol effects on the control of lung vascular permeability could be considered among the therapeutic strategies to reduce lung edema (8383. Breithaupt-Faloppa AC, Fantozzi ET, de Assis Ramos MM, Vitoretti LB, Couto GK, Lino-dos-Santos-Franco A, et al. Protective effect of estradiol on acute lung inflammation induced by an intestinal ischemic insult is dependent on nitric oxide. Shock. 2013;40(3):203-9. https://doi.org/10.1097/SHK.0b013e3182a01e24.
https://doi.org/10.1097/SHK.0b013e3182a0...
). In this model, the inflammatory status of the lungs in ovariectomized females remains for a long period after the mesenteric reperfusion has been reestablished and is characterized by the release of proinflammatory mediators and danger signals. The treatment with estradiol is able to downregulate the lung inflammation and its capacity for releasing cytokines (9090. Fantozzi ET, Breithaupt-Faloppa AC, Ricardo-da-Silva FY, Rodrigues-Garbin S, Romero DC, da Silva Rodrigues A, et al. Estradiol mediates the long-lasting lung inflammation induced by intestinal ischemia and reperfusion. J Surg Res. 2018;221:1-7. https://doi.org/10.1016/j.jss.2017.07.038.
https://doi.org/10.1016/j.jss.2017.07.03...
). In males, using the same I/R model, estradiol treatment was effective in reducing lung inflammation even at 1h after the reestablishment of intestinal perfusion (8484. Breithaupt-Faloppa AC, Thais Fantozzi E, Romero DC, Rodrigues Ada S, de Sousa PT, Lino Dos Santos Franco A, et al. Acute effects of estradiol on lung inflammation due to intestinal ischemic insult in male rats. Shock. 2014;41(3):208-13. https://doi.org/10.1097/SHK.0000000000000092.
https://doi.org/10.1097/SHK.000000000000...
). Thus, the effects of estradiol are important in the modulation of an already established lung inflammatory response. It is noteworthy to point out that the proposed treatment was acute and could be considered a clinical alternative.
Estrogen attenuates the vasoconstrictor response to various stimuli and induces vasodilation in the pulmonary vasculature during stress situations like hypoxia (9191. Lahm T, Crisostomo PR, Markel TA, Wang M, Weil BR, Novotny NM, et al. The effects of estrogen on pulmonary artery vasoreactivity and hypoxic pulmonary vasoconstriction: potential new clinical implications for an old hormone. Crit Care Med. 2008;36(7):2174-83. https://doi.org/10.1097/CCM.0b013e31817d1a92.
https://doi.org/10.1097/CCM.0b013e31817d...
). This is mediated by increased levels of prostacyclin and NO as well as decreased levels of endothelin-1 (ET-1). It is well-established that estradiol exerts important vasoactive effects by activation of eNOS, as well as modulation of vasoactive substances released from endothelial cells or the direct vasodilation effect via relaxation of smooth muscle cells (9292. Kuebler JF, Jarrar D, Toth B, Bland KI, Rue L 3rd, Wang P, et al. Estradiol administration improves splanchnic perfusion following trauma-hemorrhage and sepsis. Arch Surg. 2002;137(1):74-9. https://doi.org/10.1001/archsurg.137.1.74.
https://doi.org/10.1001/archsurg.137.1.7...
). The vasoactive effects of ET-1 can be influenced by estradiol and are organ-dependent (9393. Ba ZF, Lu A, Shimizu T, Szalay L, Schwacha MG, Rue W 3rd, et al. 17beta-Estradiol modulates vasoconstriction induced by endothelin-1 following trauma-hemorrhage. Am J Physiol Hear Circ Physiol. 2007;292(1):H245-50. https://doi.org/10.1152/ajpheart.00809.2006.
https://doi.org/10.1152/ajpheart.00809.2...
), and estradiol and its metabolites inhibit ET-1 synthesis (9494. Dubey RK, Jackson EK, Keller PJ, Imthurn B, Rosselli M. Estradiol metabolites inhibit endothelin synthesis by an estrogen receptor-independent mechanism. Hypertension. 2001;37(2 Pt 2):640-4. https://doi.org/10.1161/01.HYP.37.2.640.
https://doi.org/10.1161/01.HYP.37.2.640...
). Ovariectomized female rats present higher ET-1, and estradiol replacement reduces ET-1 peptide expression (9595. Akishita M, Ouchi Y, Miyoshi H, Orimo A, Kozaki K, Eto M, et al. Estrogen inhibits endothelin-1 production and c-fos gene expression in rat aorta. Atherosclerosis. 1996;125(1):27-38. https://doi.org/10.1016/0021-9150(96)05836-4.
https://doi.org/10.1016/0021-9150(96)058...
). Thus, estradiol acts as a protective vasoactive agent against deleterious microcirculatory conditions, such as brain death and ischemia/reperfusion injury (8282. Rocha de Sousa PT, Breithaupt-Faloppa AC, de Jesus Correia C, Simão RR, Ferreira SG, Fiorelli AI, et al. 17β -Estradiol prevents mesenteric injury induced by occlusion of the proximal descending aorta in male rats. J Vasc Surg. 2018;67(2):597-606. https://doi.org/10.1016/j.jvs.2016.12.125.
https://doi.org/10.1016/j.jvs.2016.12.12...
,9696. Vieira RF, Breithaupt-Faloppa AC, Matsubara BC, Rodrigues G, Sanches MP, Armstrong-Jr R, et al. 17β-Estradiol protects against lung injuries after brain death in male rats. J Hear Lung Transplant. 2018;37(11):1381-7. https://doi.org/10.1016/j.healun.2018.06.015.
https://doi.org/10.1016/j.healun.2018.06...
). Brain-dead rats treated with 17β-estradiol exhibit reduced lung injury, mainly because of its actions on endothelial and inducible nitric oxide synthase (iNOS) (9696. Vieira RF, Breithaupt-Faloppa AC, Matsubara BC, Rodrigues G, Sanches MP, Armstrong-Jr R, et al. 17β-Estradiol protects against lung injuries after brain death in male rats. J Hear Lung Transplant. 2018;37(11):1381-7. https://doi.org/10.1016/j.healun.2018.06.015.
https://doi.org/10.1016/j.healun.2018.06...
). Regarding injury, estrogen can inhibit vascular responses and thus prevent proatherosclerotic events (9797. Arnal JF, Fontaine C, Billon-Galés A, Favre J, Laurell H, Lenfant F, et al. Estrogen receptors and endothelium. Arterioscler Thromb Vasc Biol. 2010;30(8):1506-12. https://doi.org/10.1161/ATVBAHA.109.191221.
https://doi.org/10.1161/ATVBAHA.109.1912...
). The maintenance of organ homeostasis depends on a complex network of systems, and reduction of blood flow may have profound consequences on organ status. Microcirculatory function following trauma can be affected by sex hormones (9898. Sharawy N, Ribback S, Al-Banna N, Lehmann C, Kern H, Wendt M, et al. Estradiol receptors agonists induced effects in rat intestinal microcirculation during sepsis. Microvasc Res. 2013;85(1):118-27. https://doi.org/10.1016/j.mvr.2012.10.002.
https://doi.org/10.1016/j.mvr.2012.10.00...
), altering tissue perfusion and influencing inflammatory processes. Estrogen exerts a variety of rapid actions, initiated after coupling with membrane receptors, which may positively modulate vascular responses in pulmonary disease and help to maintain microvascular flow.
COVID-19, coagulation, and estradiol influence
Although one of the consequences of severe COVID-19 is the development of ARDS, some studies indicated that respiratory phenotypes induced by COVID-19 are slightly different from those classical phenotypes observed in ARDS patients (9999. Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020. https://doi.org/10.1007/s00134-020-06033-2.
https://doi.org/10.1007/s00134-020-06033...
). COVID-19 patients developed a severe hypoxemia early in the course of the disease, which is silent most of the time (100100. Xie J, Tong Z, Guan X, Du B, Qiu H, Slutsky AS. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020. https://doi.org/10.1007/s00134-020-05979-7.
https://doi.org/10.1007/s00134-020-05979...
). Most recently, small fibrinous thrombi in small pulmonary arterioles and a tumefaction of endothelial were observed in autopsies in cases of fatal COVID-19 (101101. Dolhnikoff M, Duarte-Neto AN, de Almeida Monteiro RA, Ferraz da Silva LF, Pierre de Oliveira E, Nascimento Saldiva PH, et al. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thromb Haemost. 2020. https://doi.org/10.1111/jth.14844.
https://doi.org/10.1111/jth.14844...
). This could indicate the activation of the coagulation cascade in these patients. In addition, they also reported diffuse alveolar damage with intense epithelial viral cytopathic effects both in the alveolar and small airways. More interestingly, the presence of thrombus occurred in both damaged and preserved lung parenchyma areas. All together, these features suggested that anticoagulant drugs could have beneficial effects in COVID-19 patients.
Estrogen reduces platelet aggregation, the opposite effect of testosterone (102102. Maccarrone M, Bari M, Battista N, Finazzi-Agrò A. Estrogen stimulates arachidonoylethanolamide release from human endothelial cells and platelet activation. Blood. 2002;100(12):4040-8. https://doi.org/10.1182/blood-2002-05-1444.
https://doi.org/10.1182/blood-2002-05-14...
,103103. Selles J, Polini N, Alvarez C, Massheimer V. Progesterone and 17 beta-estradiol acutely stimulate nitric oxide synthase activity in rat aorta and inhibit platelet aggregation. Life Sci. 2001;69(7):815-27. https://doi.org/10.1016/S0024-3205(01)01174-2.
https://doi.org/10.1016/S0024-3205(01)01...
). Notelovitz et al. (104104. Notelovitz M, Kitchens CS, Ware MD. Coagulation and fibrinolysis in estrogen-treated surgically menopausal women. Obstet Gynecol. 1984;63(5):621-5.) studied the short-term effects of estrogens on the coagulation-fibrinolysis process in surgically treated women, and the results did not show abnormal or thrombogenic changes in coagulation parameters. In vitro, 17β-estradiol is able to inhibit platelet aggregation by promoting Ca2+ extrusion or reuptake activity, and its action is dependent on the increase of NO synthesis (105105. Nakano Y, Oshima T, Matsuura H, Kajiyama G, Kambe M. Effect of 17beta-estradiol on inhibition of platelet aggregation in vitro is mediated by an increase in NO synthesis. Arterioscler Thromb Vasc Biol. 1998;18(6):961-7. https://doi.org/10.1161/01.ATV.18.6.961.
https://doi.org/10.1161/01.ATV.18.6.961...
). Platelet reactivity plays a pivotal role in thrombus formation, and in vitro data suggest that although women have a higher magnitude of platelet reactivity, their response to aspirin is similar or even larger compared to that of men (106106. Becker DM, Segal J, Vaidya D, Yanek LR, Herrera-Galeano JE, Bray PF, et al. Sex differences in platelet reactivity and response to low-dose aspirin therapy. JAMA. 2006;295(12):1420-7. https://doi.org/10.1001/jama.295.12.1420.
https://doi.org/10.1001/jama.295.12.1420...
). Experimental data show that a chronic high physiologic level of estrogen equivalent to that observed in pregnant mice had a significant inhibitory effect on platelet aggregation (107107. Valéra MC, Gratacap MP, Gourdy P, Lenfant F, Cabou C, Toutain CE, et al. Chronic estradiol treatment reduces platelet responses and protects mice from thromboembolism through the hematopoietic estrogen receptor α. Blood. 2012;120(8):1703-12. https://doi.org/10.1182/blood-2012-01-405498.
https://doi.org/10.1182/blood-2012-01-40...
). Estrogen mediates beneficial effects on the cerebral microcirculation and moderated cerebral thrombotic mechanisms by enhancing the plasma levels of NO (108108. Ono H, Sasaki Y, Bamba E, Seki J, Giddings JC, Yamamoto J. Cerebral thrombosis and microcirculation of the rat during the oestrous cycle and after ovariectomy. Clin Exp Pharmacol Physiol. 2002;29(1-2):73-8. https://doi.org/10.1046/j.1440-1681.2002.03600.x.
https://doi.org/10.1046/j.1440-1681.2002...
). Moreover, estrogens exert positive effects on the pulmonary vasculature by increasing prostacyclin release and NO production by eNOS (109109. Morrell ED, Tsai BM, Crisostomo PR, Hammoud ZT, Meldrum DR. Experimental therapies for hypoxia-induced pulmonary hypertension during acute lung injury. Shock. 2006;25(3):214-26. https://doi.org/10.1097/01.shk.0000191380.44972.46.
https://doi.org/10.1097/01.shk.000019138...
). Cowman et al. (110110. Cowman J, Dunne E, Oglesby I, Byrne B, Ralph A, Voisin B, et al. Age-related changes in platelet function are more profound in women than in men. Sci Rep. 2015;5:12235. https://doi.org/10.1038/srep12235.
https://doi.org/10.1038/srep12235...
) evidenced a connection between age and decreases in platelet tracks, platelet translocation, and unstable platelet interactions. The altered platelet function associated with aging was more profound in females compared with that of males and could be a result of a reduction in estrogen levels in women.
The role of estrogen and estrogen-related compounds in antiviral mechanism activity
Considering virus-induced lung inflammation, the excessive inflammation leads to tissue damage. In this regard, T cells seems to be reduced in COVID-19 patients, and the present T cells seemed to be functionally exhausted (111111. Chiappelli F, Khakshooy A, Greenberg G. CoViD-19 Immunopathology and Immunotherapy. Bioinformation. 2020;16(3):219-22. https://doi.org/10.6026/97320630016219.
https://doi.org/10.6026/97320630016219...
). Severe COVID-19 can induce ARDS in more than 50% of patients, and neutrophils are considered to be the central cells involved in the pathogenesis of ARDS. Infected female mice that were administered estradiol showed pulmonary recruitment of neutrophils and virus-specific CD8 T cells, releasing more INF-γ and TNF-α (112112. Robinson DP, Hall OJ, Nilles TL, Bream JH, Klein SL. 17β-estradiol protects females against influenza by recruiting neutrophils and increasing virus-specific CD8 T cell responses in the lungs. J Virol. 2014;88(9):4711-20. https://doi.org/10.1128/JVI.02081-13.
https://doi.org/10.1128/JVI.02081-13...
). Moreover, exogenous estrogen treatment in female mice infected with H1N1 reduced total pulmonary inflammation and the levels of pro-inflammatory genes in the lung (113113. Vermillion MS, Ursin RL, Attreed SE, Klein SL. Estriol Reduces Pulmonary Immune Cell Recruitment and Inflammation to Protect Female Mice From Severe Influenza. Endocrinology. 2018;159(9):3306-20. https://doi.org/10.1210/en.2018-00486.
https://doi.org/10.1210/en.2018-00486...
).
Many viruses are affected by estrogen at the molecular level, specifically in the replication machinery and maturation of the virion, but to date, no evidence has been presented for SARS-CoV-2. Despite the well-known role of estrogen in inflammation to combat pathogens and infections, it has been shown that estrogen receptors participate in repressing transcription virus genes. One example is the hepatitis B virus (HBV) infection, where ER-α interferes with virus gene expression through (HNF)-4α (hepatocyte nuclear factor 4α) binding to HBV enhancer I in hepatocytes (114114. Wang SH, Yeh SH, Lin WH, Yeh KH, Yuan Q, Xia NS, et al. Estrogen receptor α represses transcription of HBV genes via interaction with hepatocyte nuclear factor 4α. Gastroenterology. 2012;142(4):989-998.e4. https://doi.org/10.1053/j.gastro.2011.12.045.
https://doi.org/10.1053/j.gastro.2011.12...
). In the hepatitis C virus (HCV) infection model in vitro (Huh7 cells), 17β-estradiol reduced virus infection by interfering with assembly and/or virus release, disrupting the virus life cycle, and this effect was inhibited by anti-estrogen Fulvestrant (115115. Magri A, Barbaglia MN, Foglia CZ, Boccato E, Burlone ME, Cole S, et al. 17,β-estradiol inhibits hepatitis C virus mainly by interference with the release phase of its life cycle. Liver Int. 2017;37(5):669-77. https://doi.org/10.1111/liv.13303.
https://doi.org/10.1111/liv.13303...
). Moreover, HCV-infected women, after postmenopause, exhibit a reduced response to antiviral therapy and greater incidence of hepatic fibrosis and hepatic carcinoma (116116. Villa E, Karampatou A, Cammè C, Di Leo A, Luongo M, Ferrari A, et al. Early menopause is associated with lack of response to antiviral therapy in women with chronic hepatitis C. Gastroenterology. 2011;140(3):818-29. https://doi.org/10.1053/j.gastro.2010.12.027.
https://doi.org/10.1053/j.gastro.2010.12...
,117117. Yu JW, Sun LJ, Zhao YH, Kang P, Yan BZ. Impact of sex on virologic response rates in genotype 1 chronic hepatitis C patients with peginterferon alpha-2a and ribavirin treatment. Int J Infect Dis. 2011;15(11):e740-6. https://doi.org/10.1016/j.ijid.2011.05.018.
https://doi.org/10.1016/j.ijid.2011.05.0...
).
Nevertheless, the most likely antiviral effects of estrogen are mediated by inflammation modulation. Regarding the cells that participate in the immune response, dendritic cells play a crucial role. Escribese et al. (118118. Escribese MM, Kraus T, Rhee E, Fernandez-Sesma A, López CB, Moran TM. Estrogen inhibits dendritic cell maturation to RNA viruses. Blood. 2008;112(12):4574-84. https://doi.org/10.1182/blood-2008-04-148692.
https://doi.org/10.1182/blood-2008-04-14...
) infected dendritic cells with Newcastle disease virus (NDV) and treated the cells with 17β-estradiol. The authors observed a diminished type I IFN synthesis, also reducing the CD4 T cell response, suggesting that estrogen has an antiviral activity on RNA viruses.
According to the evidence that female sex hormones exert antiviral activity in many organs, the use of selective estrogen receptor modulators (SERMs) has been extensively explored in experimental systems to reduce virus infections (reviewed by Montoya & Krysan, (119119. Montoya MC, Krysan DJ. Repurposing Estrogen Receptor Antagonists for the Treatment of Infectious Disease. mBio. 2018;9(6). pii: e02272-18. https://doi.org/10.1128/mBio.02272-18.
https://doi.org/10.1128/mBio.02272-18...
)). In general, SERMs have been used for several therapeutic purposes, such as in the treatment for infertility and osteoporosis, but are mainly related to cancer as adjuvants in chemotherapy, such as tamoxifen. In viral infection, this compound was suggested to be considered as an antiviral therapy, because of its properties of disrupting viral replication during HIV (human immunodeficiency virus) infection in monocytes and CD4+ T-lymphocyte cell lines (120120. Laurence J, Cooke H, Sikder SK. Effect of tamoxifen on regulation of viral replication and human immunodeficiency virus (HIV) long terminal repeat-directed transcription in cells chronically infected with HIV-1. Blood. 1990;75(3):696-703. https://doi.org/10.1182/blood.V75.3.696.696.
https://doi.org/10.1182/blood.V75.3.696....
). Tamoxifen has also displayed a capacity to inhibit HCV replication via estrogen receptor assembly to RNA-dependent RNA polymerase NS5B (121121. Watashi K, Inoue D, Hijikata M, Goto K, Aly HH, Shimotohno K. Anti-hepatitis C virus activity of tamoxifen reveals the functional association of estrogen receptor with viral RNA polymerase NS5B. J Biol Chem. 2007;282(45):32765-72. https://doi.org/10.1074/jbc.M704418200.
https://doi.org/10.1074/jbc.M704418200...
,122122. Murakami Y, Fukasawa M, Kaneko Y, Suzuki T, Wakita T, Fukazawa H. Selective estrogen receptor modulators inhibit hepatitis C virus infection at multiple steps of the virus life cycle. Microbes Infect. 2013;15(1):45-55. https://doi.org/10.1016/j.micinf.2012.10.003.
https://doi.org/10.1016/j.micinf.2012.10...
). Murakami et al. (122122. Murakami Y, Fukasawa M, Kaneko Y, Suzuki T, Wakita T, Fukazawa H. Selective estrogen receptor modulators inhibit hepatitis C virus infection at multiple steps of the virus life cycle. Microbes Infect. 2013;15(1):45-55. https://doi.org/10.1016/j.micinf.2012.10.003.
https://doi.org/10.1016/j.micinf.2012.10...
) showed that various SERMs reduce the production of HCV RNA, preferentially related to the extracellular but also intracellular virus proteins, suggesting that SERMs may be a multi-targeted drug that interferes with several processes, comprising virus entry and replication.
Of note, the most approximate model of SARS-CoV-2 viral infection is found in MERS-CoV and SARS-CoV. Both have been demonstrated to be affected by toremifene citrate (a classical SERM), which delayed virus infection due to the inhibition of the late endosome virus trafficking (123123. Dyall J, Coleman CM, Hart BJ, Venkataraman T, Holbrook MR, Kindrachuk J, et al. Repurposing of clinically developed drugs for treatment of Middle East respiratory syndrome coronavirus infection. Antimicrob Agents Chemother. 2014;58(8):4885-93. https://doi.org/10.1128/AAC.03036-14.
https://doi.org/10.1128/AAC.03036-14...
), and a similar effect was observed previously with Ebola virus infection (124124. Johansen LM, Brannan JM, Delos SE, Shoemaker CJ, Stossel A, Lear C, et al. FDA-approved selective estrogen receptor modulators inhibit Ebola virus infection. Sci Transl Med. 2013;5(190):190ra79. https://doi.org/10.1126/scitranslmed.3005471.
https://doi.org/10.1126/scitranslmed.300...
). In addition, both in vitro and in vivo experiments showed that toremifene and clomifene present antiviral activity against a large variety of Ebola virus strains (125125. Nelson EA, Barnes AB, Wiehle RD, Fontenot GK, Hoenen T, White JM. Clomiphene and Its Isomers Block Ebola Virus Particle Entry and Infection with Similar potency: Potential Therapeutic Implications. Viruses. 2016;8(8). pii: E206. https://doi.org/10.3390/v8080206.
https://doi.org/10.3390/v8080206...
,126126. Madrid PB, Panchal RG, Warren TK, Shurtleff AC, Endsley AN, Green CE, et al. Evaluation of Ebola Virus Inhibitors for Drug Repurposing. ACS Infect Dis. 2015;1(7):317-26. https://doi.org/10.1021/acsinfecdis.5b00030.
https://doi.org/10.1021/acsinfecdis.5b00...
). Importantly, it was also demonstrated that SERMs can elevate the survival rate of infected animals by 90% and 50% when using clomifene and toremifene, respectively. Mechanistically, it has been proposed that toremifen could target envelope proteins GP1 and GP2, which permit the viral attachment and access to host cells, decreasing its stability and resulting in reduced endolysosomal membrane fusion (127127. Zhao Y, Ren J, Harlos K, Jones DM, Zeltina A, Bowden TA, et al. Toremifene interacts with and destabilizes the Ebola virus glycoprotein. Nature. 2016;535(7610):169-72. https://doi.org/10.1038/nature18615.
https://doi.org/10.1038/nature18615...
). This may be considered good evidence to support that estrogen and estrogen-related compounds play a major role in antiviral therapies for SARS-CoV-2.
CONCLUSION
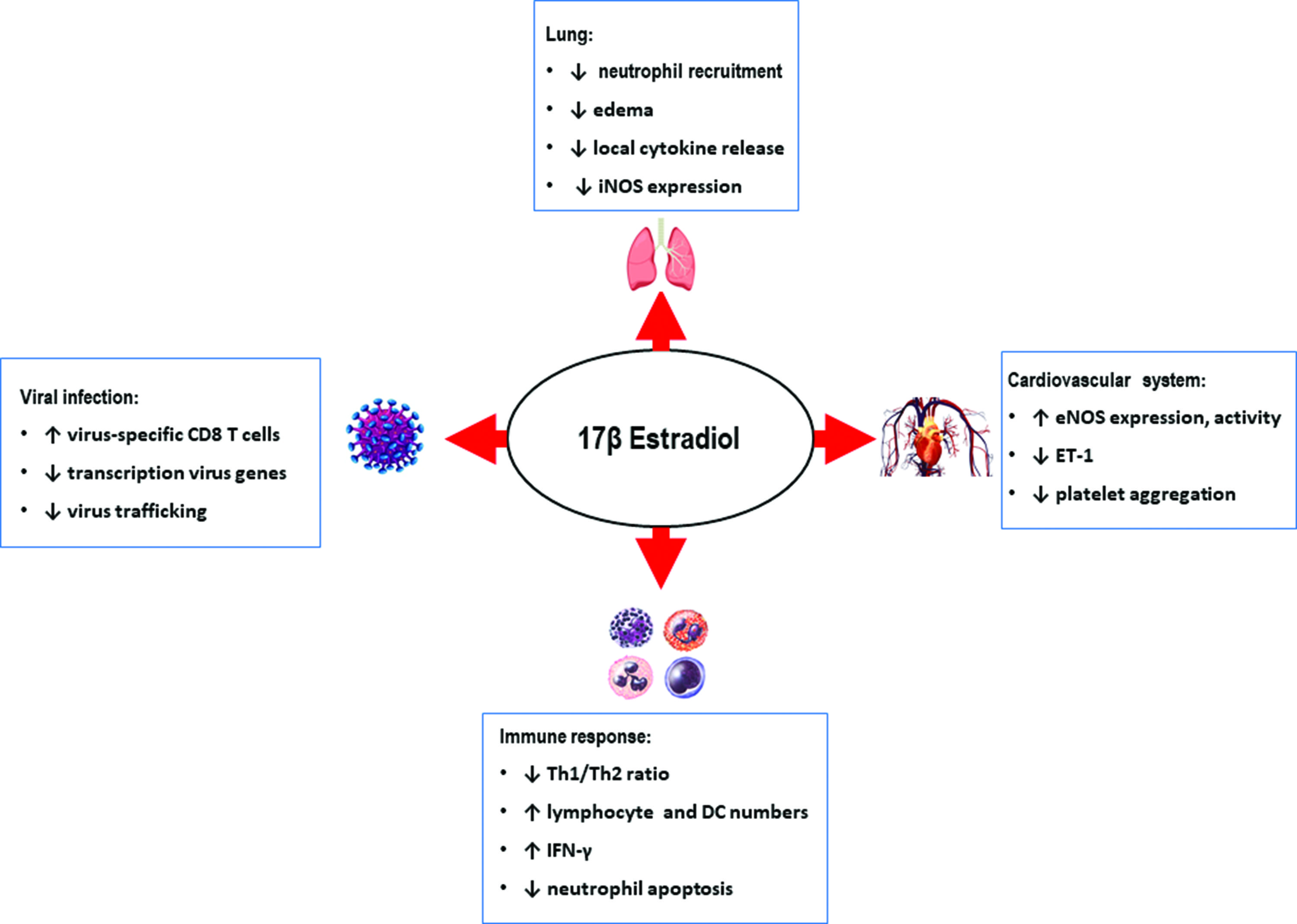
Abundant literature highlights sex differences in immune response and its influence on the incidence and severity of diseases. Considering trauma, shock, and infection, the female sex is associated with advantageous outcomes. Since the hormonal context exerts an important influence on the homeostasis control and the defense mechanisms, it is important to consider the beneficial effects of estrogens with regard to providing better control of defense and the different immune cells involved, in addition to cardiovascular system protection and flow maintenance. Direct and indirect mechanisms underlying the effects of estradiol were investigated, and the results point to a possible positive effect of estradiol as an adjuvant therapeutic element for the treatment of patients affected by the novel coronavirus, SARS-CoV-2 (Figure 1). Studies are being carried out in order to analyze the effects estradiol on SARS-CoV-2 in vitro, and in parallel, there is already a clinical trial in course.
REFERENCES
-
1Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review. JAMA. 2020. https://doi.org/10.1001/jama.2020.6019
» https://doi.org/10.1001/jama.2020.6019 -
2Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-81. https://doi.org/10.1016/S2213-2600(20)30079-5
» https://doi.org/10.1016/S2213-2600(20)30079-5 -
3Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. https://doi.org/10.1136/bmj.m1091
» https://doi.org/10.1136/bmj.m1091 -
4Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20. https://doi.org/10.1056/NEJMoa2002032
» https://doi.org/10.1056/NEJMoa2002032 -
5Global Health [Internet]. Available from: https://globalhealth5050.org/covid19/
» https://globalhealth5050.org/covid19/ -
6La Vignera S, Cannarella R, Condorelli RA, Torre F, Aversa A, Calogero AE. Sex-Specific SARS-CoV-2 Mortality: Among Hormone-Modulated ACE2 Expression, Risk of Venous Thromboembolism and Hypovitaminosis D. Int J Mol Sci. 2020;21(8). pii: E2948. https://doi.org/10.3390/ijms21082948
» https://doi.org/10.3390/ijms21082948 -
7New York Health [Internet]. Available from: https://www1.nyc.gov/site/doh/covid/covid-19-data.page
» https://www1.nyc.gov/site/doh/covid/covid-19-data.page -
8Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809-15. https://doi.org/10.1016/S0140-6736(20)30360-3
» https://doi.org/10.1016/S0140-6736(20)30360-3 -
9Fish EN. The X-files in immunity: sex-based differences predispose immune responses. Nat Rev Immunol. 2008;8(9):737-44. https://doi.org/10.1038/nri2394
» https://doi.org/10.1038/nri2394 -
10Roved J, Westerdahl H, Hasselquist D. Sex differences in immune responses: Hormonal effects, antagonistic selection, and evolutionary consequences. Horm Behav. 2017;88:95-105. https://doi.org/10.1016/j.yhbeh.2016.11.017
» https://doi.org/10.1016/j.yhbeh.2016.11.017 -
11Grossman CJ. Interactions between the gonadal steroids and the immune system. Science. 1985;227(4684):257-61. https://doi.org/10.1126/science.3871252
» https://doi.org/10.1126/science.3871252 -
12Olsen NJ, Kovacs WJ. Gonadal steroids and immunity. Endocr Rev. 1996;17(4):369-84. https://doi.org/10.1210/edrv-17-4-369
» https://doi.org/10.1210/edrv-17-4-369 -
13Schröder J, Kahlke V, Book M, Stüber F. Gender differences in sepsis: genetically determined? Shock. 2000;14(3):307-10. https://doi.org/10.1097/00024382-200014030-00011
» https://doi.org/10.1097/00024382-200014030-00011 -
14Al-Tarrah K, Moiemen N, Lord J. The influence of sex steroid hormones on the response to trauma and burn injury. Burn Trauma. 2017;5:29. https://doi.org/10.1186/s41038-017-0093-9
» https://doi.org/10.1186/s41038-017-0093-9 -
15Angele MK, Schwacha MG, Ayala A, Chaudry IH. Effect of gender and sex hormones on immune responses following shock. Shock. 2000;14(2):81-90. https://doi.org/10.1097/00024382-200014020-00001
» https://doi.org/10.1097/00024382-200014020-00001 -
16Angele MK, Frantz MC, Chaudry IH. Gender and sex hormones influence the response to trauma and sepsis: potential therapeutic approaches. Clinics. 2006;61(5):479-88. https://doi.org/10.1590/S1807-59322006000500017
» https://doi.org/10.1590/S1807-59322006000500017 -
17Chaudry IH, Samy TS, Schwacha MG, Wang P, Rue LW, Bland KI. Endocrine targets in experimental shock. J Trauma. 2003;54(5 Suppl):S118-25. https://doi.org/10.1097/01.TA.0000064511.14322.F1
» https://doi.org/10.1097/01.TA.0000064511.14322.F1 -
18Frink M, Pape HC, van Griensven M, Krettek C, Chaudry IH, Hildebrand F. Influence of sex and age on mods and cytokines after multiple injuries. Shock. 2007;27(2):151-6. https://doi.org/10.1097/01.shk.0000239767.64786.de
» https://doi.org/10.1097/01.shk.0000239767.64786.de -
19Hildebrand F, Thobe BM, Hubbard WJ, Choudhry MA, Pape HC, Chaudry IH. Effects of 17beta-estradiol and flutamide on splenic macrophages and splenocytes after trauma-hemorrhage. Cytokine. 2006;36(3-4):107-14. https://doi.org/10.1016/j.cyto.2006.11.002
» https://doi.org/10.1016/j.cyto.2006.11.002 -
20Hsieh YC, Frink M, Thobe BM, Hsu JT, Choudhry MA, Schwacha MG, et al. 17Beta-estradiol downregulates Kupffer cell TLR4-dependent p38 MAPK pathway and normalizes inflammatory cytokine production following trauma-hemorrhage. Mol Immunol. 2007;44(9):2165-72. https://doi.org/10.1016/j.molimm.2006.11.019
» https://doi.org/10.1016/j.molimm.2006.11.019 -
21Knöferl MW, Jarrar D, Angele MK, Ayala A, Schwacha MG, Bland KI, et al. 17 beta-Estradiol normalizes immune responses in ovariectomized females after trauma-hemorrhage. Am J Physiol Cell Physiol. 2001;281(4):C1131-8. https://doi.org/10.1152/ajpcell.2001.281.4.C1131
» https://doi.org/10.1152/ajpcell.2001.281.4.C1131 -
22Knöferl MW, Angele MK, Diodato MD, Schwacha MG, Ayala A, Cioffi WG, et al. Female sex hormones regulate macrophage function after trauma-hemorrhage and prevent increased death rate from subsequent sepsis. Ann Surg. 2002;235(1):105-12. https://doi.org/10.1097/00000658-200201000-00014
» https://doi.org/10.1097/00000658-200201000-00014 -
23Moeinpour F, Choudhry MA, Kawasaki T, Timares L, Schwacha MG, Bland KI, et al. 17 Beta-estradiol normalizes Toll receptor 4, mitogen activated protein kinases and inflammatory response in epidermal keratinocytes following trauma-hemorrhage. Mol Immunol. 2007;44(13):3317-23. https://doi.org/10.1016/j.molimm.2007.02.023
» https://doi.org/10.1016/j.molimm.2007.02.023 -
24Stangl V, Baumann G, Stangl K. Coronary atherogenic risk factors in women. Eur Heart J. 2002;23(22):1738-52. https://doi.org/10.1053/euhj.2002.3329
» https://doi.org/10.1053/euhj.2002.3329 -
25Suba Z. Prevention and therapy of COVID-19 via exogenous estrogen treatment for both male and female patients. J Pharm Pharm Sci. 2020;23(1):75-85. https://doi.org/10.18433/jpps31069
» https://doi.org/10.18433/jpps31069 -
26Xu X, Chen P, Wang J, Feng J, Zhou H, Li X, et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63(3):457-60. https://doi.org/10.1007/s11427-020-1637-5
» https://doi.org/10.1007/s11427-020-1637-5 -
27Wujtewicz M, Dylczyk-Sommer A, Aszkiełowicz A, Zdanowski S, Piwowarczyk S, Owczuk R. COVID-19 - what should anaethesiologists and intensivists know about it? Anaesthesiol Intensive Ther. 2020;52(1):34-41. https://doi.org/10.5114/ait.2020.93756
» https://doi.org/10.5114/ait.2020.93756 -
28Mo P, Xing Y, Xiao Y, Deng L, Zhao Q, Wang H, et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020. pii: ciaa270. https://doi.org/10.1093/cid/ciaa270
» https://doi.org/10.1093/cid/ciaa270 -
29Gurwitz D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev Res. 2020. https://doi.org/10.1002/ddr.21656
» https://doi.org/10.1002/ddr.21656 -
30Zhang H, Zhou P, Wei Y, Yue H, Wang Y, Hu M, et al. Histopathologic Changes and SARS-CoV-2 Immunostaining in the Lung of a Patient With COVID-19. Ann Intern Med. 2020. https://doi.org/10.7326/M20-0533
» https://doi.org/10.7326/M20-0533 -
31Barrett CD, Moore HB, Yaffe MB, Moore EE. ISTH interim guidance on recognition and management of coagulopathy in COVID-19: A Comment. J Thromb Haemost. 2020. https://doi.org/10.1111/jth.14860
» https://doi.org/10.1111/jth.14860 -
32Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020. pii: blood.2020006000. https://doi.org/10.1182/blood.2020006000
» https://doi.org/10.1182/blood.2020006000 -
33Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, et al. Angiotensin Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2. Circ Res. 2020;126(10):1456-74. https://doi.org/10.1161/CIRCRESAHA.120.317015
» https://doi.org/10.1161/CIRCRESAHA.120.317015 -
34Leisman DE, Deutschman CS, Legrand M. Facing COVID-19 in the ICU: vascular dysfunction, thrombosis, and dysregulated inflammation. Intensive Care Med. 2020. https://doi.org/10.1007/s00134-020-06059-6
» https://doi.org/10.1007/s00134-020-06059-6 -
35Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, et al. Chest CT Features of COVID-19 in Rome, Italy. Radiology. 2020. https://doi.org/10.1148/radiol.2020201237
» https://doi.org/10.1148/radiol.2020201237 -
36Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;30(5):2620-9. https://doi.org/10.1172/JCI137244
» https://doi.org/10.1172/JCI137244 -
37Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425-34. https://doi.org/10.1016/S1473-3099(20)30086-4
» https://doi.org/10.1016/S1473-3099(20)30086-4 -
38Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. https://doi.org/10.1016/j.ijantimicag.2020.105924
» https://doi.org/10.1016/j.ijantimicag.2020.105924 -
39Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47(5):1275-80. https://doi.org/10.1007/s00259-020-04735-9
» https://doi.org/10.1007/s00259-020-04735-9 -
40Mason RJ. Pathogenesis of COVID-19 from a cell biologic perspective. Eur Respir J. 2020;55(4) pii: 2000607. https://doi.org/10.1183/13993003.00607-2020
» https://doi.org/10.1183/13993003.00607-2020 -
41ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526-33. https://doi.org/10.1001/jama.2012.5669
» https://doi.org/10.1001/jama.2012.5669 -
42Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149(3 Pt 1):818-24. https://doi.org/10.1164/ajrccm.149.3.7509706
» https://doi.org/10.1164/ajrccm.149.3.7509706 -
43Randhawa R, Bellingan G. Acute lung injury. Anaesth Intensive Care Med. 2007;8(11):477-80. https://doi.org/10.1016/j.mpaic.2007.09.003
» https://doi.org/10.1016/j.mpaic.2007.09.003 -
44Matthay MA, Zemans RL, Zimmerman GA, Arabi YM, Beitler JR, Mercat A, et al. Acute respiratory distress syndrome. Nat Rev Dis Prim. 2019;5(1):18.
-
45Hecker L. Mechanisms and consequences of oxidative stress in lung disease: therapeutic implications for an aging populace. Am J Physiol Lung Cell Mol Physiol. 2018;314(4):L642-L653. https://doi.org/10.1152/ajplung.00275.2017
» https://doi.org/10.1152/ajplung.00275.2017 -
46Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. https://doi.org/10.1016/S0140-6736(20)30183-5
» https://doi.org/10.1016/S0140-6736(20)30183-5 -
47Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020. https://doi.org/10.1007/s00134-020-05991-x
» https://doi.org/10.1007/s00134-020-05991-x -
48Lagunas‐Rangel FA, Chávez‐Valencia V. High IL‐6/IFN‐γ ratio could be associated with severe disease in COVID‐19 patients. J Med Virol. 2020. https://doi.org/10.1002/jmv.25900
» https://doi.org/10.1002/jmv.25900 -
49Zhou Y, Han T, Chen J, Hou C, Hua L, He S, et al. Clinical and Autoimmune Characteristics of Severe and Critical Cases with COVID-19. Clin Transl Sci. 2020. https://doi.org/10.1111/cts.12805
» https://doi.org/10.1111/cts.12805 -
50Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020. https://doi.org/10.1001/jamainternmed.2020.0994
» https://doi.org/10.1001/jamainternmed.2020.0994 -
51Pires-Neto RC, Morales MM, Lancas T, Inforsato N, Duarte MIS, Amato MB, et al. Expression of acute-phase cytokines, surfactant proteins, and epithelial apoptosis in small airways of human acute respiratory distress syndrome. J Crit Care. 2013;28(1):111.e9-111.e15. https://doi.org/10.1016/j.jcrc.2012.05.013
» https://doi.org/10.1016/j.jcrc.2012.05.013 -
52Parsons EC, Hough CL, Seymour CW, Cooke CR, Rubenfeld GD, Watkins TR, et al. Red blood cell transfusion and outcomes in patients with acute lung injury, sepsis and shock. Crit Care. 2011;15(5):R221. https://doi.org/10.1186/cc10458
» https://doi.org/10.1186/cc10458 -
53Schütte H, Lohmeyer J, Rosseau S, Ziegler S, Siebert C, Kielisch H, et al. Bronchoalveolar and systemic cytokine profiles in patients with ARDS, severe pneumonia and cardiogenic pulmonary oedema. Eur Respir J. 1996;9(9):1858-67. https://doi.org/10.1183/09031936.96.09091858
» https://doi.org/10.1183/09031936.96.09091858 -
54Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, et al. Relationships among lymphocyte subsets, cytokines, and the pulmonary inflammation index in coronavirus (COVID‐19) infected patients. Br J Haematol. 2020;189(3):428-37. https://doi.org/10.1111/bjh.16659
» https://doi.org/10.1111/bjh.16659 -
55Kovats S. Estrogen receptors regulate innate immune cells and signaling pathways. Cell Immunol. 2015;294(2):63-9. https://doi.org/10.1016/j.cellimm.2015.01.018
» https://doi.org/10.1016/j.cellimm.2015.01.018 -
56Khan D, Ansar Ahmed S. The Immune System Is a Natural Target for Estrogen Action: Opposing Effects of Estrogen in Two Prototypical Autoimmune Diseases. Front Immunol. 2016;6:635. https://doi.org/10.3389/fimmu.2015.00635
» https://doi.org/10.3389/fimmu.2015.00635 -
57Fairweather D, Frisancho-Kiss S, Rose NR. Sex differences in autoimmune disease from a pathological perspective. Am J Pathol. 2008;173(3):600-9. https://doi.org/10.2353/ajpath.2008.071008
» https://doi.org/10.2353/ajpath.2008.071008 -
58Offner PJ, Moore EE, Biffl WL. Male gender is a risk factor for major infections after Vsurgery. Arch Surg. 1999;134(9):935-8. https://doi.org/10.1001/archsurg.134.9.935
» https://doi.org/10.1001/archsurg.134.9.935 -
59Wichmann MW, Inthorn D, Andress HJ, Schildberg FW. Incidence and mortality of severe sepsis in surgical intensive care patients: the influence of patient gender on disease process and outcome. Intensive Care Med. 2000;26(2):167-72. https://doi.org/10.1007/s001340050041
» https://doi.org/10.1007/s001340050041 -
60George RL, McGwin G Jr, Windham ST, Melton SM, Metzger J, Chaudry IH,et al. Age-related gender differential in outcome after blunt or penetrating trauma. Shock. 2003;19(1):28-32. https://doi.org/10.1097/00024382-200301000-00006
» https://doi.org/10.1097/00024382-200301000-00006 -
61Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl. J Med. 2003;348(16):1546-54. https://doi.org/10.1056/NEJMoa022139
» https://doi.org/10.1056/NEJMoa022139 -
62Amadori A, Zamarchi R, De Silvestro G, Forza G, Cavatton G, Danieli GA, et al. Genetic control of the CD4/CD8 T-cell ratio in humans. Nat Med. 1995;1(12):1279-83. https://doi.org/10.1038/nm1295-1279
» https://doi.org/10.1038/nm1295-1279 -
63Arruvito L, Sanz M, Banham AH, Fainboim L. Expansion of CD4+CD25+ and FOXP3+ regulatory T cells during the follicular phase of the menstrual cycle: implications for human reproduction. J Immunol. 2007;178(4):2572-8. https://doi.org/10.4049/jimmunol.178.4.2572
» https://doi.org/10.4049/jimmunol.178.4.2572 -
64Kramer PR, Kramer SF, Guan G. 17 beta-estradiol regulates cytokine release through modulation of CD16 expression in monocytes and monocyte-derived macrophages. Arthritis Rheum. 2004;50(6):1967-75. https://doi.org/10.1002/art.20309
» https://doi.org/10.1002/art.20309 -
65Molloy EJ, O’Neill AJ, Grantham JJ, Sheridan-Pereira M, Fitzpatrick JM, Webb DW, et al. Sex-specific alterations in neutrophil apoptosis: The role of estradiol and progesterone. Blood. 2003;102(7):2653-9. https://doi.org/10.1182/blood-2003-02-0649
» https://doi.org/10.1182/blood-2003-02-0649 -
66Nadkarni S, Cooper D, Brancaleone V, Bena S, Perretti M. Activation of the annexin A1 pathway underlies the protective effects exerted by estrogen in polymorphonuclear leukocytes. Arterioscler Thromb Vasc Biol. 2011;31(11):2749-59. https://doi.org/10.1161/ATVBAHA.111.235176
» https://doi.org/10.1161/ATVBAHA.111.235176 -
67Scotland RS, Stables MJ, Madalli S, Watson P, Gilroy DW. Sex differences in resident immune cell phenotype underlie more efficient acute inflammatory responses in female mice. Blood. 2011;118(22):5918-27. https://doi.org/10.1182/blood-2011-03-340281
» https://doi.org/10.1182/blood-2011-03-340281 -
68Kovats S. Estrogen receptors regulate an inflammatory pathway of dendritic cell differentiation: mechanisms and implications for immunity. Horm Behav. 2012;62(3):254-62. https://doi.org/10.1016/j.yhbeh.2012.04.011
» https://doi.org/10.1016/j.yhbeh.2012.04.011 -
69Murphy K, Weaver C. Janeway’s Immunobiology. 9th ed. Taylor & Francis Group L, editor. New York: Garland Science; 2017.
-
70Agarwal R, Aggarwal AN, Gupta D, Behera D, Jindal SK. Etiology and outcomes of pulmonary and extrapulmonary acute lung injury/ARDS in a respiratory ICU in north India. Chest. 2006;130(3):724-9. https://doi.org/10.1378/chest.130.3.724
» https://doi.org/10.1378/chest.130.3.724 -
71Moss M, Mannino DM. Race and gender differences in acute respiratory distress syndrome deaths in the United States: an analysis of multiple-cause mortality data (1979-1996). Crit Care Med. 2002;30(8):1679-85. https://doi.org/10.1097/00003246-200208000-00001
» https://doi.org/10.1097/00003246-200208000-00001 -
72Asavasupreechar T, Saito R, Miki Y, Edwards DP, Boonyaratanakornkit V, Sasano H. Systemic distribution of progesterone receptor subtypes in human tissues. J Steroid Biochem Mol Biol. 2020;199:105599. https://doi.org/10.1016/j.jsbmb.2020.105599
» https://doi.org/10.1016/j.jsbmb.2020.105599 -
73Fuentes N, Silveyra P. Endocrine regulation of lung disease and inflammation. Exp Biol Med. 2018;243(17-18):1313-22. https://doi.org/10.1177/1535370218816653
» https://doi.org/10.1177/1535370218816653 -
74Carey MA, Card JW, Voltz JW, Germolec DR, Korach KS, Zeldin DC. The impact of sex and sex hormones on lung physiology and disease: lessons from animal studies. Am J Physiol Lung Cell Mol Physiol. 2007;293(2):L272-8. https://doi.org/10.1152/ajplung.00174.2007
» https://doi.org/10.1152/ajplung.00174.2007 -
75Nawrot TS, Staessen JA, Gardner JP, Aviv A. Telomere length and possible link to X chromosome. Lancet. 2004;363(9408):507-10. https://doi.org/10.1016/S0140-6736(04)15535-9
» https://doi.org/10.1016/S0140-6736(04)15535-9 -
76Gardner M, Bann D, Wiley L, Cooper R, Hardy R, Nitsch D, et al. Gender and telomere length: systematic review and meta-analysis. Exp Gerontol. 2014;51:15-27. https://doi.org/10.1016/j.exger.2013.12.004
» https://doi.org/10.1016/j.exger.2013.12.004 -
77Alvarez A, Hermenegildo C, Issekutz AC, Esplugues JV, Sanz MJ. Estrogens inhibit angiotensin II-induced leukocyte-endothelial cell interactions in vivo via rapid endothelial nitric oxide synthase and cyclooxygenase activation. Circ Res. 2002;91(12):1142-50. https://doi.org/10.1161/01.RES.0000046018.23605.3E
» https://doi.org/10.1161/01.RES.0000046018.23605.3E -
78Gao H, Liang M, Bergdahl A, Hamrén A, Lindholm MW, Dahlman-Wright K, et al. Estrogen attenuates vascular expression of inflammation associated genes and adhesion of monocytes to endothelial cells. Inflamm Res. 2006;55(8):349-53. https://doi.org/10.1007/s00011-006-5194-z
» https://doi.org/10.1007/s00011-006-5194-z -
79Geraldes P, Gagnon S, Hadjadj S, Merhi Y, Sirois MG, Cloutier I, et al. Estradiol blocks the induction of CD40 and CD40L expression on endothelial cells and prevents neutrophil adhesion: An ERalpha-mediated pathway. Cardiovasc Res. 2006;71(3):566-73. https://doi.org/10.1016/j.cardiores.2006.05.015
» https://doi.org/10.1016/j.cardiores.2006.05.015 -
80Ma XL, Gao F, Chen J, Christopher TA, Lopez BL, Ohlstein EH, et al. Endothelial protective and antishock effects of a selective estrogen receptor modulator in rats. Am J Physiol Heart Circ Physiol. 2001;280(2):H876-84. https://doi.org/10.1152/ajpheart.2001.280.2.H876
» https://doi.org/10.1152/ajpheart.2001.280.2.H876 -
81Novella S, Dantas AP, Segarra G, Medina P, Hermenegildo C. Vascular Aging in Women: is Estrogen the Fountain of Youth? Front Physiol. 2012;3:165. https://doi.org/10.3389/fphys.2012.00165
» https://doi.org/10.3389/fphys.2012.00165 -
82Rocha de Sousa PT, Breithaupt-Faloppa AC, de Jesus Correia C, Simão RR, Ferreira SG, Fiorelli AI, et al. 17β -Estradiol prevents mesenteric injury induced by occlusion of the proximal descending aorta in male rats. J Vasc Surg. 2018;67(2):597-606. https://doi.org/10.1016/j.jvs.2016.12.125
» https://doi.org/10.1016/j.jvs.2016.12.125 -
83Breithaupt-Faloppa AC, Fantozzi ET, de Assis Ramos MM, Vitoretti LB, Couto GK, Lino-dos-Santos-Franco A, et al. Protective effect of estradiol on acute lung inflammation induced by an intestinal ischemic insult is dependent on nitric oxide. Shock. 2013;40(3):203-9. https://doi.org/10.1097/SHK.0b013e3182a01e24
» https://doi.org/10.1097/SHK.0b013e3182a01e24 -
84Breithaupt-Faloppa AC, Thais Fantozzi E, Romero DC, Rodrigues Ada S, de Sousa PT, Lino Dos Santos Franco A, et al. Acute effects of estradiol on lung inflammation due to intestinal ischemic insult in male rats. Shock. 2014;41(3):208-13. https://doi.org/10.1097/SHK.0000000000000092
» https://doi.org/10.1097/SHK.0000000000000092 -
85Ricardo-Da-Silva FY, Fantozzi ET, Rodrigues-Garbin S, Oliveira-Filho RM, Vargaftig BB, Breithaupt-Faloppa AC, et al. Estradiol Modulates Local Gut Injury Induced by Intestinal Ischemia-Reperfusion in Male Rats. Shock. 2017;48(4):477-83. https://doi.org/10.1097/SHK.0000000000000873
» https://doi.org/10.1097/SHK.0000000000000873 -
86Deitch EA, Feketeova E, Lu Q, Zaets S, Berezina TL, Machiedo GW, et al. Resistance of the female, as opposed to the male, intestine to I/R-mediated injury is associated with increased resistance to gut-induced distant organ injury. Shock. 2008;29(1):78-83. https://doi.org/10.1097/shk.0b013e318063e98a
» https://doi.org/10.1097/shk.0b013e318063e98a -
87Mrazkova H, Lischke R, Herget J. Influence of gender on ischemia-reperfusion injury in lungs in an animal model. Physiol Res. 2016;65(6):953-8. https://doi.org/10.33549/physiolres.933273
» https://doi.org/10.33549/physiolres.933273 -
88Raju R, Chaudry IH. Sex steroids receptor antagonist: their use as adjuncts after trauma-hemorrhage for improving immune/cardiovascular responses and for decreasing mortality from subsequent sepsis. Anesth Analg. 2008;107(1):159-66. https://doi.org/10.1213/ane.0b013e318163213d
» https://doi.org/10.1213/ane.0b013e318163213d -
89Nadkarni S, McArthur S. Oestrogen and immunomodulation: new mechanisms that impact on peripheral and central immunity. Curr Opin Pharmacol. 2013;13(4):576-81. https://doi.org/10.1016/j.coph.2013.05.007
» https://doi.org/10.1016/j.coph.2013.05.007 -
90Fantozzi ET, Breithaupt-Faloppa AC, Ricardo-da-Silva FY, Rodrigues-Garbin S, Romero DC, da Silva Rodrigues A, et al. Estradiol mediates the long-lasting lung inflammation induced by intestinal ischemia and reperfusion. J Surg Res. 2018;221:1-7. https://doi.org/10.1016/j.jss.2017.07.038
» https://doi.org/10.1016/j.jss.2017.07.038 -
91Lahm T, Crisostomo PR, Markel TA, Wang M, Weil BR, Novotny NM, et al. The effects of estrogen on pulmonary artery vasoreactivity and hypoxic pulmonary vasoconstriction: potential new clinical implications for an old hormone. Crit Care Med. 2008;36(7):2174-83. https://doi.org/10.1097/CCM.0b013e31817d1a92
» https://doi.org/10.1097/CCM.0b013e31817d1a92 -
92Kuebler JF, Jarrar D, Toth B, Bland KI, Rue L 3rd, Wang P, et al. Estradiol administration improves splanchnic perfusion following trauma-hemorrhage and sepsis. Arch Surg. 2002;137(1):74-9. https://doi.org/10.1001/archsurg.137.1.74
» https://doi.org/10.1001/archsurg.137.1.74 -
93Ba ZF, Lu A, Shimizu T, Szalay L, Schwacha MG, Rue W 3rd, et al. 17beta-Estradiol modulates vasoconstriction induced by endothelin-1 following trauma-hemorrhage. Am J Physiol Hear Circ Physiol. 2007;292(1):H245-50. https://doi.org/10.1152/ajpheart.00809.2006
» https://doi.org/10.1152/ajpheart.00809.2006 -
94Dubey RK, Jackson EK, Keller PJ, Imthurn B, Rosselli M. Estradiol metabolites inhibit endothelin synthesis by an estrogen receptor-independent mechanism. Hypertension. 2001;37(2 Pt 2):640-4. https://doi.org/10.1161/01.HYP.37.2.640
» https://doi.org/10.1161/01.HYP.37.2.640 -
95Akishita M, Ouchi Y, Miyoshi H, Orimo A, Kozaki K, Eto M, et al. Estrogen inhibits endothelin-1 production and c-fos gene expression in rat aorta. Atherosclerosis. 1996;125(1):27-38. https://doi.org/10.1016/0021-9150(96)05836-4
» https://doi.org/10.1016/0021-9150(96)05836-4 -
96Vieira RF, Breithaupt-Faloppa AC, Matsubara BC, Rodrigues G, Sanches MP, Armstrong-Jr R, et al. 17β-Estradiol protects against lung injuries after brain death in male rats. J Hear Lung Transplant. 2018;37(11):1381-7. https://doi.org/10.1016/j.healun.2018.06.015
» https://doi.org/10.1016/j.healun.2018.06.015 -
97Arnal JF, Fontaine C, Billon-Galés A, Favre J, Laurell H, Lenfant F, et al. Estrogen receptors and endothelium. Arterioscler Thromb Vasc Biol. 2010;30(8):1506-12. https://doi.org/10.1161/ATVBAHA.109.191221
» https://doi.org/10.1161/ATVBAHA.109.191221 -
98Sharawy N, Ribback S, Al-Banna N, Lehmann C, Kern H, Wendt M, et al. Estradiol receptors agonists induced effects in rat intestinal microcirculation during sepsis. Microvasc Res. 2013;85(1):118-27. https://doi.org/10.1016/j.mvr.2012.10.002
» https://doi.org/10.1016/j.mvr.2012.10.002 -
99Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020. https://doi.org/10.1007/s00134-020-06033-2
» https://doi.org/10.1007/s00134-020-06033-2 -
100Xie J, Tong Z, Guan X, Du B, Qiu H, Slutsky AS. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020. https://doi.org/10.1007/s00134-020-05979-7
» https://doi.org/10.1007/s00134-020-05979-7 -
101Dolhnikoff M, Duarte-Neto AN, de Almeida Monteiro RA, Ferraz da Silva LF, Pierre de Oliveira E, Nascimento Saldiva PH, et al. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thromb Haemost. 2020. https://doi.org/10.1111/jth.14844
» https://doi.org/10.1111/jth.14844 -
102Maccarrone M, Bari M, Battista N, Finazzi-Agrò A. Estrogen stimulates arachidonoylethanolamide release from human endothelial cells and platelet activation. Blood. 2002;100(12):4040-8. https://doi.org/10.1182/blood-2002-05-1444
» https://doi.org/10.1182/blood-2002-05-1444 -
103Selles J, Polini N, Alvarez C, Massheimer V. Progesterone and 17 beta-estradiol acutely stimulate nitric oxide synthase activity in rat aorta and inhibit platelet aggregation. Life Sci. 2001;69(7):815-27. https://doi.org/10.1016/S0024-3205(01)01174-2
» https://doi.org/10.1016/S0024-3205(01)01174-2 -
104Notelovitz M, Kitchens CS, Ware MD. Coagulation and fibrinolysis in estrogen-treated surgically menopausal women. Obstet Gynecol. 1984;63(5):621-5.
-
105Nakano Y, Oshima T, Matsuura H, Kajiyama G, Kambe M. Effect of 17beta-estradiol on inhibition of platelet aggregation in vitro is mediated by an increase in NO synthesis. Arterioscler Thromb Vasc Biol. 1998;18(6):961-7. https://doi.org/10.1161/01.ATV.18.6.961
» https://doi.org/10.1161/01.ATV.18.6.961 -
106Becker DM, Segal J, Vaidya D, Yanek LR, Herrera-Galeano JE, Bray PF, et al. Sex differences in platelet reactivity and response to low-dose aspirin therapy. JAMA. 2006;295(12):1420-7. https://doi.org/10.1001/jama.295.12.1420
» https://doi.org/10.1001/jama.295.12.1420 -
107Valéra MC, Gratacap MP, Gourdy P, Lenfant F, Cabou C, Toutain CE, et al. Chronic estradiol treatment reduces platelet responses and protects mice from thromboembolism through the hematopoietic estrogen receptor α. Blood. 2012;120(8):1703-12. https://doi.org/10.1182/blood-2012-01-405498
» https://doi.org/10.1182/blood-2012-01-405498 -
108Ono H, Sasaki Y, Bamba E, Seki J, Giddings JC, Yamamoto J. Cerebral thrombosis and microcirculation of the rat during the oestrous cycle and after ovariectomy. Clin Exp Pharmacol Physiol. 2002;29(1-2):73-8. https://doi.org/10.1046/j.1440-1681.2002.03600.x
» https://doi.org/10.1046/j.1440-1681.2002.03600.x -
109Morrell ED, Tsai BM, Crisostomo PR, Hammoud ZT, Meldrum DR. Experimental therapies for hypoxia-induced pulmonary hypertension during acute lung injury. Shock. 2006;25(3):214-26. https://doi.org/10.1097/01.shk.0000191380.44972.46
» https://doi.org/10.1097/01.shk.0000191380.44972.46 -
110Cowman J, Dunne E, Oglesby I, Byrne B, Ralph A, Voisin B, et al. Age-related changes in platelet function are more profound in women than in men. Sci Rep. 2015;5:12235. https://doi.org/10.1038/srep12235
» https://doi.org/10.1038/srep12235 -
111Chiappelli F, Khakshooy A, Greenberg G. CoViD-19 Immunopathology and Immunotherapy. Bioinformation. 2020;16(3):219-22. https://doi.org/10.6026/97320630016219
» https://doi.org/10.6026/97320630016219 -
112Robinson DP, Hall OJ, Nilles TL, Bream JH, Klein SL. 17β-estradiol protects females against influenza by recruiting neutrophils and increasing virus-specific CD8 T cell responses in the lungs. J Virol. 2014;88(9):4711-20. https://doi.org/10.1128/JVI.02081-13
» https://doi.org/10.1128/JVI.02081-13 -
113Vermillion MS, Ursin RL, Attreed SE, Klein SL. Estriol Reduces Pulmonary Immune Cell Recruitment and Inflammation to Protect Female Mice From Severe Influenza. Endocrinology. 2018;159(9):3306-20. https://doi.org/10.1210/en.2018-00486
» https://doi.org/10.1210/en.2018-00486 -
114Wang SH, Yeh SH, Lin WH, Yeh KH, Yuan Q, Xia NS, et al. Estrogen receptor α represses transcription of HBV genes via interaction with hepatocyte nuclear factor 4α. Gastroenterology. 2012;142(4):989-998.e4. https://doi.org/10.1053/j.gastro.2011.12.045
» https://doi.org/10.1053/j.gastro.2011.12.045 -
115Magri A, Barbaglia MN, Foglia CZ, Boccato E, Burlone ME, Cole S, et al. 17,β-estradiol inhibits hepatitis C virus mainly by interference with the release phase of its life cycle. Liver Int. 2017;37(5):669-77. https://doi.org/10.1111/liv.13303
» https://doi.org/10.1111/liv.13303 -
116Villa E, Karampatou A, Cammè C, Di Leo A, Luongo M, Ferrari A, et al. Early menopause is associated with lack of response to antiviral therapy in women with chronic hepatitis C. Gastroenterology. 2011;140(3):818-29. https://doi.org/10.1053/j.gastro.2010.12.027
» https://doi.org/10.1053/j.gastro.2010.12.027 -
117Yu JW, Sun LJ, Zhao YH, Kang P, Yan BZ. Impact of sex on virologic response rates in genotype 1 chronic hepatitis C patients with peginterferon alpha-2a and ribavirin treatment. Int J Infect Dis. 2011;15(11):e740-6. https://doi.org/10.1016/j.ijid.2011.05.018
» https://doi.org/10.1016/j.ijid.2011.05.018 -
118Escribese MM, Kraus T, Rhee E, Fernandez-Sesma A, López CB, Moran TM. Estrogen inhibits dendritic cell maturation to RNA viruses. Blood. 2008;112(12):4574-84. https://doi.org/10.1182/blood-2008-04-148692
» https://doi.org/10.1182/blood-2008-04-148692 -
119Montoya MC, Krysan DJ. Repurposing Estrogen Receptor Antagonists for the Treatment of Infectious Disease. mBio. 2018;9(6). pii: e02272-18. https://doi.org/10.1128/mBio.02272-18
» https://doi.org/10.1128/mBio.02272-18 -
120Laurence J, Cooke H, Sikder SK. Effect of tamoxifen on regulation of viral replication and human immunodeficiency virus (HIV) long terminal repeat-directed transcription in cells chronically infected with HIV-1. Blood. 1990;75(3):696-703. https://doi.org/10.1182/blood.V75.3.696.696
» https://doi.org/10.1182/blood.V75.3.696.696 -
121Watashi K, Inoue D, Hijikata M, Goto K, Aly HH, Shimotohno K. Anti-hepatitis C virus activity of tamoxifen reveals the functional association of estrogen receptor with viral RNA polymerase NS5B. J Biol Chem. 2007;282(45):32765-72. https://doi.org/10.1074/jbc.M704418200
» https://doi.org/10.1074/jbc.M704418200 -
122Murakami Y, Fukasawa M, Kaneko Y, Suzuki T, Wakita T, Fukazawa H. Selective estrogen receptor modulators inhibit hepatitis C virus infection at multiple steps of the virus life cycle. Microbes Infect. 2013;15(1):45-55. https://doi.org/10.1016/j.micinf.2012.10.003
» https://doi.org/10.1016/j.micinf.2012.10.003 -
123Dyall J, Coleman CM, Hart BJ, Venkataraman T, Holbrook MR, Kindrachuk J, et al. Repurposing of clinically developed drugs for treatment of Middle East respiratory syndrome coronavirus infection. Antimicrob Agents Chemother. 2014;58(8):4885-93. https://doi.org/10.1128/AAC.03036-14
» https://doi.org/10.1128/AAC.03036-14 -
124Johansen LM, Brannan JM, Delos SE, Shoemaker CJ, Stossel A, Lear C, et al. FDA-approved selective estrogen receptor modulators inhibit Ebola virus infection. Sci Transl Med. 2013;5(190):190ra79. https://doi.org/10.1126/scitranslmed.3005471
» https://doi.org/10.1126/scitranslmed.3005471 -
125Nelson EA, Barnes AB, Wiehle RD, Fontenot GK, Hoenen T, White JM. Clomiphene and Its Isomers Block Ebola Virus Particle Entry and Infection with Similar potency: Potential Therapeutic Implications. Viruses. 2016;8(8). pii: E206. https://doi.org/10.3390/v8080206
» https://doi.org/10.3390/v8080206 -
126Madrid PB, Panchal RG, Warren TK, Shurtleff AC, Endsley AN, Green CE, et al. Evaluation of Ebola Virus Inhibitors for Drug Repurposing. ACS Infect Dis. 2015;1(7):317-26. https://doi.org/10.1021/acsinfecdis.5b00030
» https://doi.org/10.1021/acsinfecdis.5b00030 -
127Zhao Y, Ren J, Harlos K, Jones DM, Zeltina A, Bowden TA, et al. Toremifene interacts with and destabilizes the Ebola virus glycoprotein. Nature. 2016;535(7610):169-72. https://doi.org/10.1038/nature18615
» https://doi.org/10.1038/nature18615
Publication Dates
-
Publication in this collection
29 May 2020 -
Date of issue
2020
History
-
Received
5 May 2020 -
Accepted
5 May 2020