ABSTRACT
Objective:
Lumbosacral fixation presents problems in its arthrodesis, mainly due to pseudoarthrosis. Iliac screws minimize this problem, however, they show problems in the operative wound. The S2-Alar-iliac (S2AI) screw presents a lower rate of these complications. The anatomical differences between the populations and the sexes analyzed in the literature justify the study of the S2AI screw technique in Brazilian women.
Methods:
A total of 14 adult female CT scans were analyzed by 4 evaluators.
Results:
The mean bone length was 131.8 mm, the largest bone diameter was 22.6 mm, and the smallest bone diameter was 22.6 mm.
Conclusions:
The data presented are compatible with the literature and may assist spine surgeons in choosing the best implant and surgical technique. Level of Evidence I; Diagnostic Studies — Investigating a Diagnostic Test (anatomical investigation).
Keywords:
Spinal diseases; Surgery; Fracture fixation, internal
RESUMO
Objetivos:
A fixação lombossacra apresenta problemas na sua artrodese, devido principalmente à pseudoartrose. Os parafusos de ilíaco minimizam esse problema, contudo mostram problemas na ferida operatória. Já o parafuso de S2-Alar-Ilíaco (S2AI) apresenta menor índice dessas complicações. As diferenças anatômicas entre as populações e os sexos analisados na literatura justificam o estudo da técnica de parafuso de S2AI em mulheres brasileiras.
Métodos:
Foram analisadas 14 tomografias de mulheres adultas por quatro avaliadores.
Resultados:
O comprimento ósseo médio foi de 131,8 mm, maior diâmetro ósseo foi de 22,6 mm, o menor diâmetro ósseo de 22,6 mm.
Conclusões:
Os dados apresentados são compatíveis com a literatura e podem ajudar os cirurgiões de coluna na escolha do melhor implante e na técnica cirúrgica. Nível de Evidência I; Investigação de um exame para diagnóstico (investigação anatômica).
Descritores:
Doenças da coluna vertebral; Cirurgia; Fixação interna de fraturas
RESUMEN
Objetivos:
La fijación lumbosacra presenta problemas en la artrodesis, principalmente a causa de la pseudoartrosis. Los tornillos del ilíaco minimizan este problema, pero causan problemas en la herida quirúrgica. El tornillo S2-Alar-ilíaco (S2AI) muestra un menor índice de estas complicaciones. Las diferencias anatómicas entre las poblaciones y los sexos analizados en la literatura justifican el estudio de la técnica del tornillo S2AI en mujeres brasileñas.
Métodos:
Cuatro evaluadores analizaron 14 tomografías de mujeres adultas.
Resultados:
La longitud ósea media fue de 131,8 mm, el mayor diámetro fue de 22,6 mm, el menor diámetro óseo fue 22,6 mm.
Conclusiones:
Los datos presentados son compatibles con la literatura y pueden ayudar a los cirujanos de columna en la elección del mejor implante y técnica quirúrgica. Nivel de Evidencia I; Estudios de diagnósticos - Investigación de un examen para diagnóstico (investigación anatómica).
Descriptores:
Enfermedades de la columna vertebral; Cirugía; Fijación interna de fracturas
INTRODUCTION
The lumbosacral area is an anatomical region where problems occur in arthrodesis, often associated with nonunion and loss of fixation. Several historical alternatives have been described for the fixation of this region, such as Gavelston rods,11. Peelle MW, Lenke LG, Bridwell KH, Sides B. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rod versus iliac and lumbosacral screws. Spine (Phila Pa 1976). 2006;31(20):2392–8. S1/S2 pedicle, S2-Alar, and iliac screws.22. Miladi LT, Ghanem IB, Draoui MM, Zeller RD, Dubousset JF. Iliosacral screw fixation for pelvic obliquity in neuromuscular scoliosis: A long-term follow-up study. Spine (Phila Pa 1976). 1997;22(15):1722–9. Although the latter method minimizes the fixation problem, it also gives rise to concerns regarding the surgical wound and the prominence of the screws.33. Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976). 2002;27(7):776–86.,44. Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006;31(3):303–8. The S2-Alar-iliac (S2AI) screw was described with a view to reducing these problems and maintaining the quality of the fixation technique.55. Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976). 2010;35(25):2245–51.,66. Sponseller PD. Innovative Techniques in Pediatric Deformity: Use of Temporary Internal Distraction and the Sacral Alar Iliac Technique in the Pediatric Population. Semin Spine Surg. 2012;24(3):180–5.
The original description of the technique was made in the American pediatric and adult population.55. Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976). 2010;35(25):2245–51.,66. Sponseller PD. Innovative Techniques in Pediatric Deformity: Use of Temporary Internal Distraction and the Sacral Alar Iliac Technique in the Pediatric Population. Semin Spine Surg. 2012;24(3):180–5. There is also a description in the Asian population, comprising mainly Chinese subjects, with 120 patients analyzed in the sum of two available studies.77. Zhu F, Bao HD, Yuan S, Wang B, Qiao J, Zhu ZZ, et al. Posterior second sacral alar iliac screw insertion: Anatomic study in a Chinese population. Eur Spine J. 2013;22(7):1683–9.,88. Kwan MK, Jeffry A, Chan CYW, Saw LB. A radiological evaluation of the morphometry and safety of S1, S2 and S2-ilium screws in the Asian population using three dimensional computed tomography scan: An analysis of 180 pelvis. Surg Radiol Anat. 2012;34(3):217–27. The studies describe the male and female population in the proportion of 50% each, showing little difference between sexes.77. Zhu F, Bao HD, Yuan S, Wang B, Qiao J, Zhu ZZ, et al. Posterior second sacral alar iliac screw insertion: Anatomic study in a Chinese population. Eur Spine J. 2013;22(7):1683–9.–99. Chang TL, Sponseller PD, Kebaish KM, Fishman EK. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976). 2009;34(5):436–40. Despite these data, there is sufficient information in the literature to suggest a difference in the pelvic anatomy between male/female subjects and between populations.1010. Fischer B, Mitteroecker P. Allometry and Sexual Dimorphism in the Human Pelvis. Anat Rec (Hoboken). 2017;300(4):698–705.–1313. Handa VL, Lockhart ME, Fielding JR, Catherine S, Brubakery L, Cundiffy GW, et al. NIH Public Access. Victoria. 2008;111:914–20.
Taking into account differences in the sacropelvic anatomy between sexes and ethnicities, further studies describing the passage of the S2AI screw in populations, other than those described above, are relevant. This study therefore aims to demonstrate the tomographic parameters of passage of the S2AI screw in a population of brazilian women.
METHODS
Following approval by the Institutional Review Board, IRB – 1,726,509, we retrospectively analyzed normal elective CT scans of the pelvis taken to investigate intra-abdominal pathologies. All the scans had to undergo reconstruction in the axial, sagittal and coronal sections with the possibility of three-dimensional reconstruction. The computed tomography equipment consisted of helical multichannel scanners. The scans were collected non-consecutively from 25 patients aged between 18 and 65 years, randomly selected from the year 2016. Of the total 25 patients, 11 were men and were excluded from the study. None of the patients selected had any bone deformity in the lumbosacral spine and pelvis.
The scans were analyzed by Isite (Phillips)®, a company of Dutch origin, through three-dimensional reconstruction of the CT scans by two orthopedic and trauma residents, and two spinal surgery residents in their 5th year. All the measurements were taken bilaterally. The mean of the measurements taken by the analyzers was calculated.
The data were standardized as follows: age in years; diameter, length and width measured in millimeters; angle measured in degrees. The S2AI screw parameters were measured as follows:
-
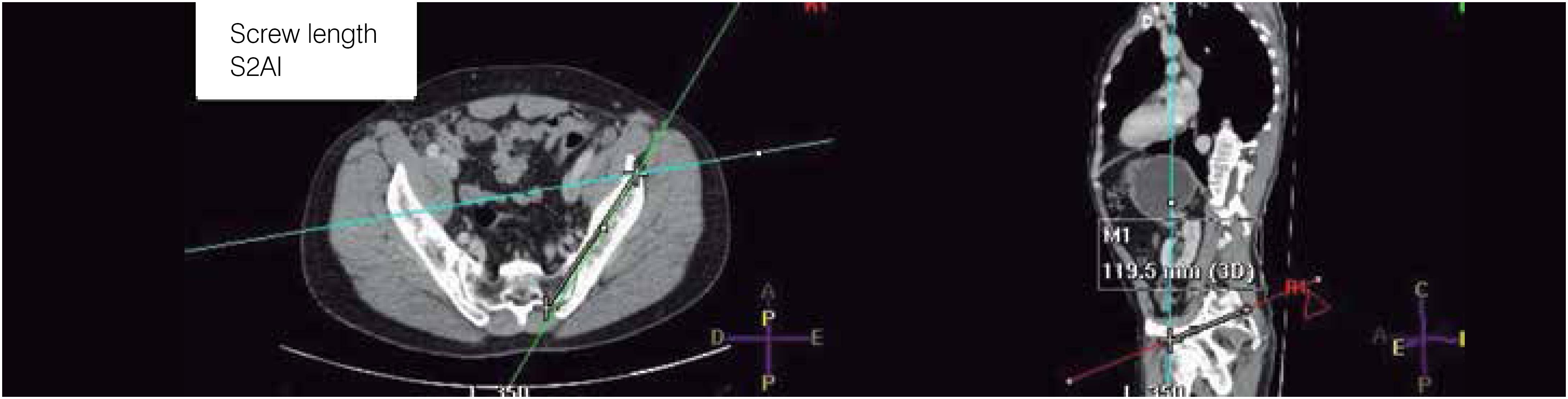
Length: distance between the S2AI screw insertion point (between S1 and S2, 2 mm lateral to the paramedian sacral crest) and the anterior inferior iliac spine; (Figure 1)
-
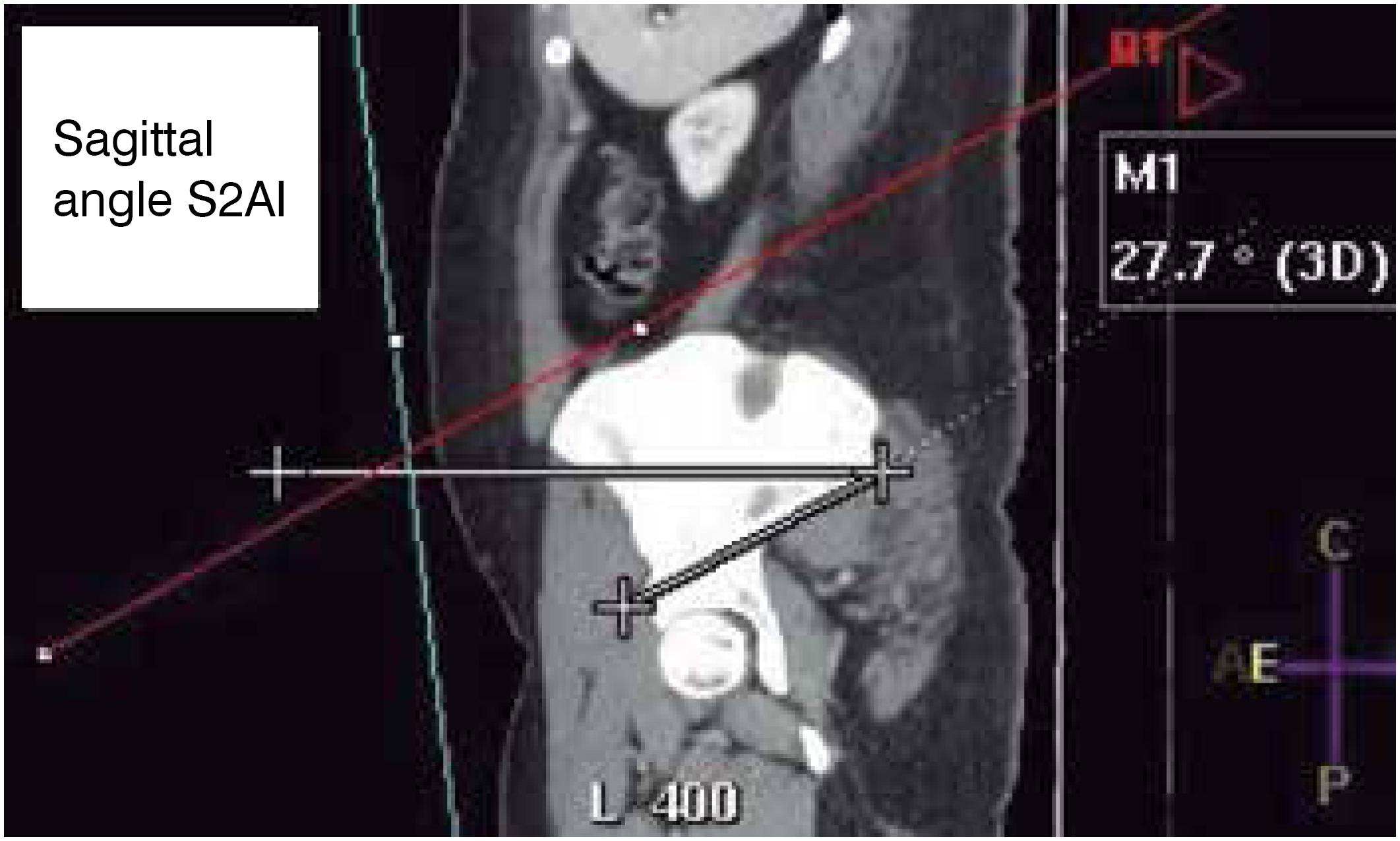
Sagittal angle: angle of inclination of the S2AI screw in the sagittal section of the CT scan; (Figure 2)
-
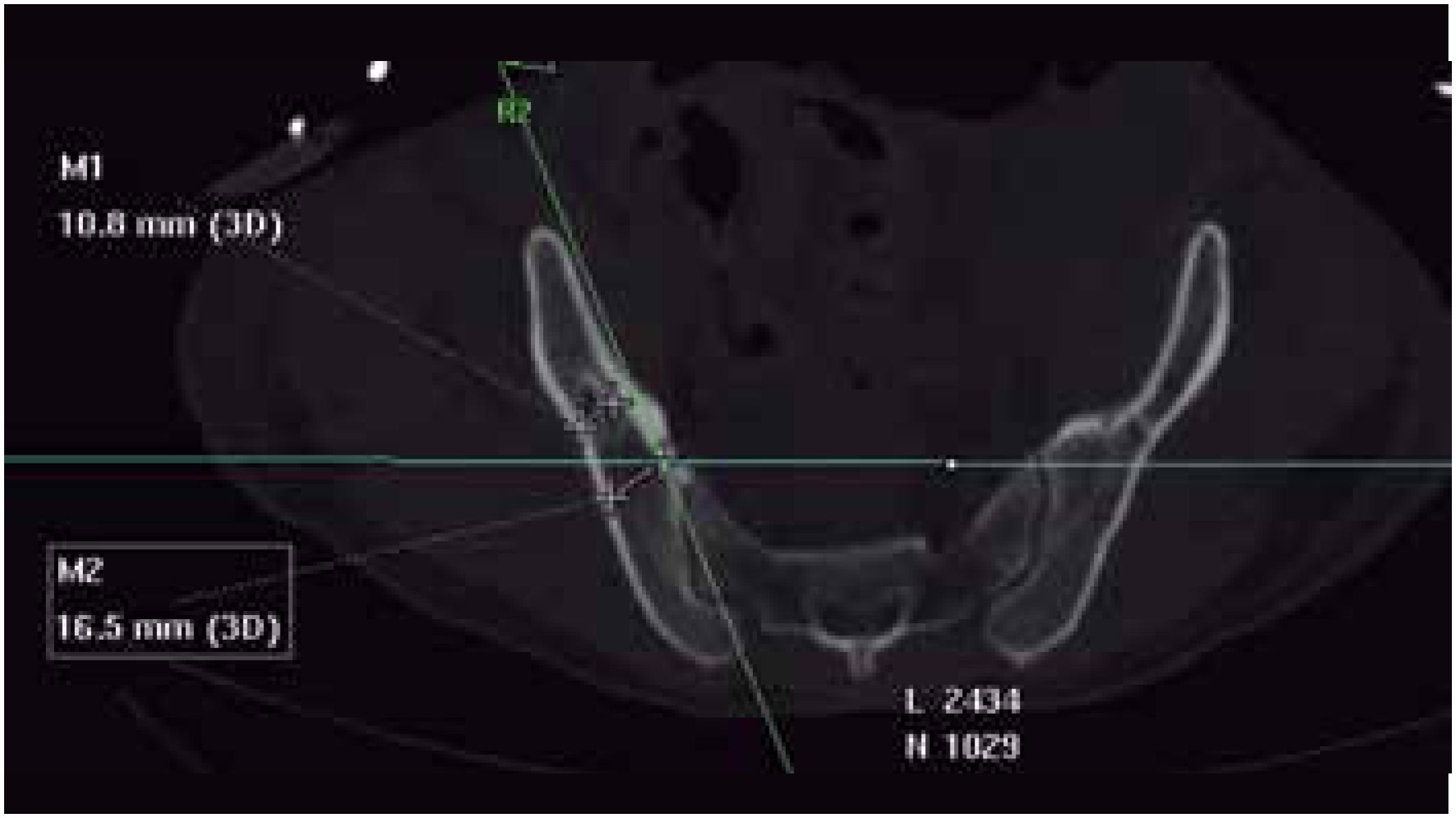
Axial angle: angle of inclination of the S2AI screw in the axial section of the CT scan; (Figure 3)
-
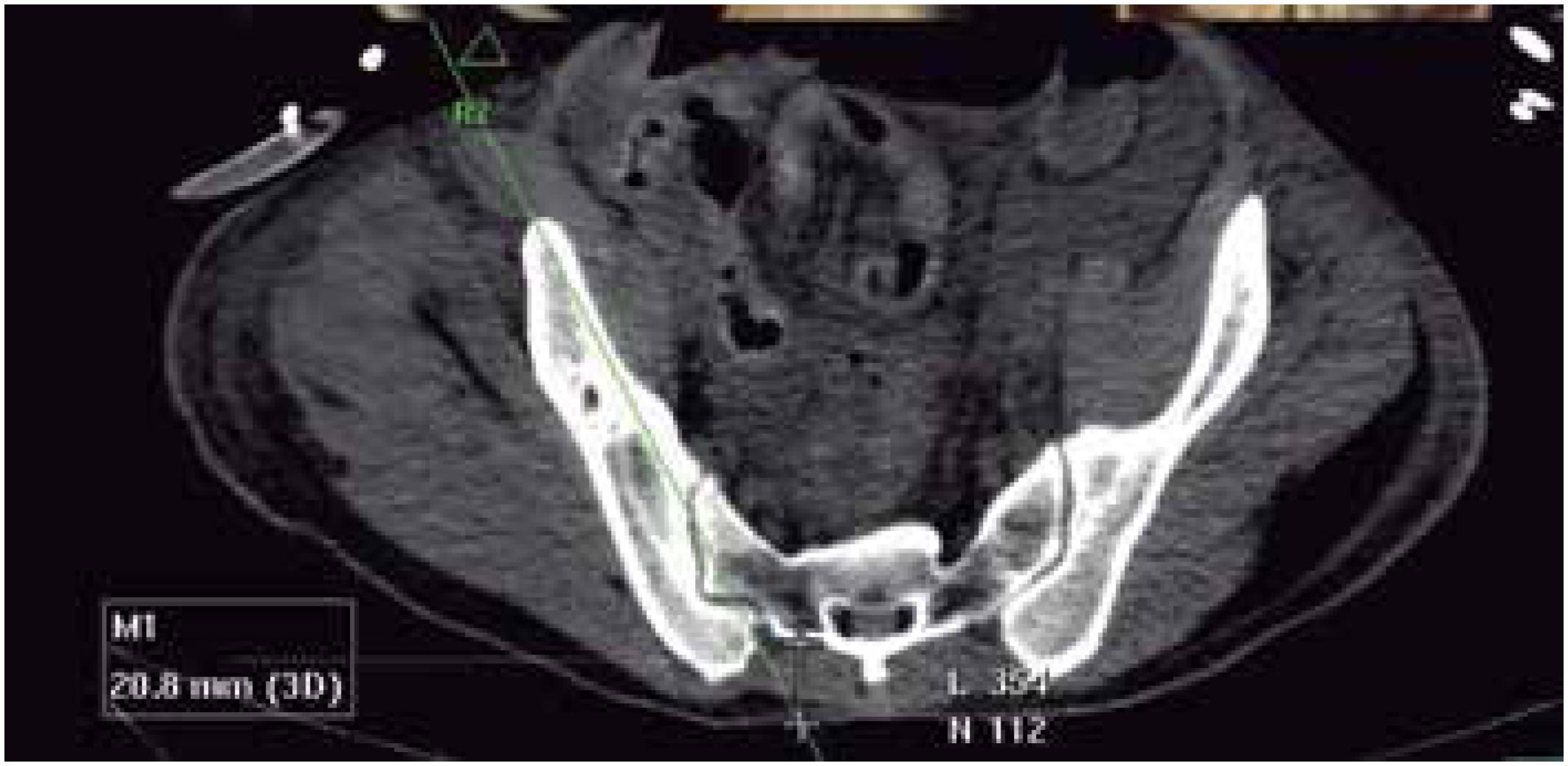
Largest diameter: largest diameter between the external and internal iliac cortices; (Figures 4 and 5)
-
Smallest diameter: smallest diameter between the external and internal iliac cortices in its isthmic region; (Figures 4 and 5)
-
Distance from the skin: distance between the S2AI screw insertion point and the skin; (Figure 6)
RESULTS
The study population consisted of 14 female patients aged 28-65 years (mean age 48.7 years). Table 1 shows the mean of the analyses performed by the four evaluators. The greatest bone length of the trajectory of the right and left screws was respectively 147.5 and 149.9 mm (final mean of 131.8 mm). The mean of the largest diameter of the bone through which the screw passes was 22.6 mm. The variation of the means was 24.4-19.2 mm on the right side and 26.9-19.7 mm on the left. The evaluation of the smallest diameter of the bone, through which the screw passes in the iliac, showed that the final mean was 17.6 mm.
The mean angle on the axial plane for the right screw was 34.7°, ranging from 38.1 to 29.8 degrees, while the mean angle on the left side was 32.3 degrees, ranging from 36.4 to 27.2 degrees. The final mean angle was 33.5 degrees. The final mean angle on the sagittal plane was 31.5 degrees, measuring 30.3 degrees on the right side and 32.7 degrees on the left. The maximum angle was 37.9 degrees for the right side and 41.8 degrees for the left, while the minimum angle was 25.2 degrees and 27.3 degrees, respectively. The distance from the skin had a final mean of 59.9 mm, with the mean ranging from 59.7 mm on the right to 60.1 mm on the left. Table 1
DISCUSSION
The pelvic fixation technique described by Kebaish55. Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976). 2010;35(25):2245–51. and Sponseller,66. Sponseller PD. Innovative Techniques in Pediatric Deformity: Use of Temporary Internal Distraction and the Sacral Alar Iliac Technique in the Pediatric Population. Semin Spine Surg. 2012;24(3):180–5. S2AI, appeared as an alternative in the attempt to resolve the problems of existing techniques. L5-S1 fixation has a high rate of pseudoarthrosis, and Kim et al. demonstrated a rate of 24% in the correction of adult scoliosis.1414. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006;31(20):2329–36. A technique that minimized this problem was iliac fixation.1515. Kuklo TR, Bridwell KH, Lewis SJ, Baldus C, Blanke K, Iffrig TM, et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976). 2001;26(18):1976–83. However, this technique was not without problems. One of the complaints submitted is the prominence of the screw, with a withdrawal rate of 22% at one year33. Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976). 2002;27(7):776–86. and a much higher rate after 5 years.44. Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006;31(3):303–8. Another drawback of the technique is the need for extensive soft tissue dissection, predisposing patients to a higher rate of infections and alignment with the rods. In the series of Kuklo et al,1515. Kuklo TR, Bridwell KH, Lewis SJ, Baldus C, Blanke K, Iffrig TM, et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976). 2001;26(18):1976–83. 4% of patients presented with surgical wound infection within 2 years.
In the pediatric population, the technique described by Sponseller66. Sponseller PD. Innovative Techniques in Pediatric Deformity: Use of Temporary Internal Distraction and the Sacral Alar Iliac Technique in the Pediatric Population. Semin Spine Surg. 2012;24(3):180–5. defines the entry point as being approximately 25 mm caudal to the upper endplate of S1 and 22 mm lateral to the midline, positioned at an angle of 40º laterally and caudally. His peer described the same technique55. Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976). 2010;35(25):2245–51. as being 2 to 4 mm lateral and 4 to 8 mm distal to the dorsal sacral foramen of S1. Despite the original descriptions, we noted minor variations in the medical literature showing the entry point, including studies in which the actual authors of the technique participated.1616. Matteini LE, Kebaish KM, Volk WR, Bergin PF, Yu WD, O’Brien JR. An S-2 alar iliac pelvic fixation. Technical note. Neurosurg Focus. 2010;28(3):E13.,1717. O’Brien JR, Yu WD, Bhatnagar R, Sponseller P, Kebaish KM. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976). 2009;34(12):E439-42. Our entry point was between the midline between S1 and S2 and 2 mm lateral to the foramen, which closely resembles the technique described by Kebaish, going in the direction of the anterior inferior iliac spine.88. Kwan MK, Jeffry A, Chan CYW, Saw LB. A radiological evaluation of the morphometry and safety of S1, S2 and S2-ilium screws in the Asian population using three dimensional computed tomography scan: An analysis of 180 pelvis. Surg Radiol Anat. 2012;34(3):217–27. The purpose of this method of measurement was to facilitate the passage of the screw during the surgical procedure, with anatomical parameters that are easy to locate, thus avoiding the use of radioscopy.
The study by Kwan et al,88. Kwan MK, Jeffry A, Chan CYW, Saw LB. A radiological evaluation of the morphometry and safety of S1, S2 and S2-ilium screws in the Asian population using three dimensional computed tomography scan: An analysis of 180 pelvis. Surg Radiol Anat. 2012;34(3):217–27. which analyzes the S2A1 screw trajectory in the Asian population (Chinese, Malaysians and Indians), showed a variation of 122.2 to 86.4 in the screw trajectory in women. Axial angles ranged from 39.5 to 50.2 degrees, depending on the longest or shortest screw trajectory. Another study that described 30 Chinese women obtained the following results: maximum diameter of 115.21 mm, mean sagittal angle of 35 degrees and mean axial angle of 36 degrees, and a mean diameter of 14.85 mm.77. Zhu F, Bao HD, Yuan S, Wang B, Qiao J, Zhu ZZ, et al. Posterior second sacral alar iliac screw insertion: Anatomic study in a Chinese population. Eur Spine J. 2013;22(7):1683–9. Another study which shows the population of adolescents obtained results that are similar to the studies described,99. Chang TL, Sponseller PD, Kebaish KM, Fishman EK. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976). 2009;34(5):436–40. such as a mean angle of 39 degrees on the axial plane and 38 degrees on the sagittal plane. In our study, the mean greatest screw length was 131.8 mm, the largest diameter 22.6 mm, and the mean axial and sagittal angles were, respectively, 33.5 and 31.5 degrees. Note that the difference shown is in millimeters, yet there is still a difference. This difference can be explained by the fact that the study subjects are of different races, presenting minor variations that may justify the result. Another possibility is the difference in size between the study participants; however, as not all studies present these data, it cannot be stated with more certainty whether this is indeed one of the justifications.
This study has limitations that must be taken into account for the interpretation of the data. The limited number of patients analyzed may not actually represent the Brazilian female population, leading to the difficulty of external validation. The data collection method, which is not uniform across all studies, also needs to be taken into account. Another point to be highlighted is that the programs used to analyze the CT scans are different, and may have differences between them, such as magnification. Non-inclusion of the weight and height of the patients undergoing the scan is a flaw in the data interpretation, as it makes it impossible to adequately match the size of the measurements with the size of the subject evaluated.
CONCLUSIONS
Despite the problems inherent to the study method, it has proven useful in describing data relating to the S2AI screw passage technique in Brazilian women and showing that the technique is possible in this population, allowing the use of suitable implants and good fixation. The following mean measurements were found: greatest length of 131.8 mm, largest bone diameter of 22.6 mm, smallest bone diameter of 17.6 mm, axial angle of 33.5 mm, sagittal angle of 31.5 mm and distance from the skin of 59.9 mm. The information published in this study, taking all the appropriate considerations into account, should help spine surgeons choose the best implant and carry out the screw insertion technique.
-
Study Instituto de Ortopedia e Traumatologia of the Hospital das Clínicas of the Universidade de São Paulo – IOTHCFMUSP, São Paulo, SP, Brazil.
REFERENCES
-
1Peelle MW, Lenke LG, Bridwell KH, Sides B. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rod versus iliac and lumbosacral screws. Spine (Phila Pa 1976). 2006;31(20):2392–8.
-
2Miladi LT, Ghanem IB, Draoui MM, Zeller RD, Dubousset JF. Iliosacral screw fixation for pelvic obliquity in neuromuscular scoliosis: A long-term follow-up study. Spine (Phila Pa 1976). 1997;22(15):1722–9.
-
3Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976). 2002;27(7):776–86.
-
4Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006;31(3):303–8.
-
5Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976). 2010;35(25):2245–51.
-
6Sponseller PD. Innovative Techniques in Pediatric Deformity: Use of Temporary Internal Distraction and the Sacral Alar Iliac Technique in the Pediatric Population. Semin Spine Surg. 2012;24(3):180–5.
-
7Zhu F, Bao HD, Yuan S, Wang B, Qiao J, Zhu ZZ, et al. Posterior second sacral alar iliac screw insertion: Anatomic study in a Chinese population. Eur Spine J. 2013;22(7):1683–9.
-
8Kwan MK, Jeffry A, Chan CYW, Saw LB. A radiological evaluation of the morphometry and safety of S1, S2 and S2-ilium screws in the Asian population using three dimensional computed tomography scan: An analysis of 180 pelvis. Surg Radiol Anat. 2012;34(3):217–27.
-
9Chang TL, Sponseller PD, Kebaish KM, Fishman EK. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976). 2009;34(5):436–40.
-
10Fischer B, Mitteroecker P. Allometry and Sexual Dimorphism in the Human Pelvis. Anat Rec (Hoboken). 2017;300(4):698–705.
-
11Kurki HK. Bilateral Asymmetry in the Human Pelvis. Anat Rec (Hoboken). 2017;300(4):653–65.
-
12Mallard AM, Savell KR, Auerbach BM. Morphological Integration of the Human Pelvis with Respect to Age and Sex. Anat Rec (Hoboken). 2017;300(4):666–74.
-
13Handa VL, Lockhart ME, Fielding JR, Catherine S, Brubakery L, Cundiffy GW, et al. NIH Public Access. Victoria. 2008;111:914–20.
-
14Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006;31(20):2329–36.
-
15Kuklo TR, Bridwell KH, Lewis SJ, Baldus C, Blanke K, Iffrig TM, et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976). 2001;26(18):1976–83.
-
16Matteini LE, Kebaish KM, Volk WR, Bergin PF, Yu WD, O’Brien JR. An S-2 alar iliac pelvic fixation. Technical note. Neurosurg Focus. 2010;28(3):E13.
-
17O’Brien JR, Yu WD, Bhatnagar R, Sponseller P, Kebaish KM. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976). 2009;34(12):E439-42.
Publication Dates
-
Publication in this collection
Oct-Dec 2018
History
-
Received
26 Apr 2017 -
Accepted
01 June 2018