Abstracts
The aim of this study was to investigate if there is a relationship between the impact of Chronic Obstructive Pulmonary Disease (COPD) on health status and the level of dyspnea in Activities of Daily Living (ADL) and the mortality predictor index in patients undergoing Pulmonary Rehabilitation (PR). It is a cross-sectional study in which 32 patients with moderate to very severe COPD (23 men; 66.6±12.0 years; FEV1: 40.6±15.6% predicted) were assessed by: COPD Assessment Test (CAT), Body Mass Index (BMI), six-Minute Walking Test (6MWT), London Chest Activity of Daily Living Scale (LCADL), modified Medical Research Council (mMRC) and BODE Index (Body mass index, airflow Obstruction, Dyspnea and Exercise capacity). The CAT score presented moderate correlation with the mMRC questionnaire (r=0.35; p=0.048), total score of LCADL (r=0.60; p<0.001) and total score LCADL percentage (r=0.57; p=0.001). Only the total score of LCADL is able to predict the CAT questionnaire scores (p<0.05; r²=0.61). There were no significant correlations between CAT and BODE index, BMI, FEV1 and 6MWT. Thus, the higher the level of dyspnea in ADL, the greater the impact of COPD on the patient's health status. However, this is not true in relation to mortality prognosis in patients with COPD in PR.
Pulmonary Disease; Chronic Obstructive; Sickness Impact Profile; Activities of Daily Living
O objetivo do estudo foi investigar se há relação entre o impacto da Doença Pulmonar Obstrutiva Crônica (DPOC) no estado de saúde com o nível de dispneia nas atividades de vida diária (AVD) e o índice preditor de mortalidade em pacientes em reabilitação pulmonar (RP). Trata-se de um estudo transversal, em que foram avaliados 32 pacientes com DPOC moderada a muito grave (23 homens; 66,6±12,0 anos; VEF1: 40,6±15,6% previsto) por meio do COPD Assessment Test (CAT), Índice de Massa Corpórea (IMC), Teste de Caminhada de Seis Minutos (TC6), London Chest Activity of Daily Living Scale (LCADL), modified Medical Research Council (mMRC) e Índice BODE (Body mass index, airflow Obstruction, Dyspnea and Exercise capacity). Observaram-se correlações positivas moderadas do CAT com o questionário mMRC (r=0,35; p=0,048), a pontuação total da LCADL (r=0,60; p<0,001) e com a porcentagem da pontuação total da LCADL (r=0,57; p=0,001). Apenas a pontuação total da LCADL é capaz de predizer independentemente a pontuação do questionário CAT (p<0,05; r²=0,61). Não foram constatadas correlações significativas entre o CAT e o Índice BODE, IMC, TC6 e VEF1. Dessa forma, quanto maior o nível de dispneia nas AVD, maior o impacto da DPOC no estado de saúde do paciente, entretanto, o mesmo não ocorre em relação ao prognóstico de mortalidade nos pacientes com DPOC em RP.
Doença Pulmonar Obstrutiva Crônica; Perfil de Impacto da Doença; Atividades Cotidianas
El objetivo del estudio fue investigar si hay relación entre el impacto de la Enfermedad Pulmonar Obstructiva Crónica (EPOC) en el estado de salud con el nivel de disnea en las actividades de la vida diaria (AVD) y el índice predictor de mortalidad en pacientes en rehabilitación pulmonar (RP). Se trata de un estudio transversal, en el que fueron evaluados 32 pacientes con EPOC moderada a muy grave (23 hombres; 66,6±12,0 años; VEF1: 40,6±15,6% previsto) por medio del COPD Assessment Test (CAT), Índice de Masa Corpórea (IMC), Test de Caminata de Seis Minutos (TC6), London Chest Activity of Daily Living Scale (LCADL), mo dified Medical Research Council (mMRC) e Índice BODE (Body mass index, airflow Obstruction, Dyspnea and Exercise capacity). Se observaron correlaciones positivas moderadas del CAT con el cuestionario mMRC (r=0,35; p=0,048), la puntuación total de la LCADL (r=0,60; p<0,001) y con el porcentaje de la puntuación total de la LCADL (r=0,57; p=0,001). Apenas la puntuación total de la LCADL es capaz de predecir independientemente la puntuación del cuestionario CAT (p<0,05; r²=0,61). No fueron constatadas correlaciones significativas entre el CAT y el Índice BODE, IMC, TC6 e VEF1. De esa forma, cuanto mayor es el nivel de disnea en las AVD, mayor es el impacto de la EPOC en el estado de salud del paciente, entre tanto, lo mismo no ocurre en relación al pronóstico de mortalidad en los pacientes con EPOC en RP.
Enfermedad Pulmonar Obstructutiva Crónica; Perfil de Impacto de Enfermedad; Actividades Cotidianas
ORIGINAL RESEARCH
Júlia Gianjoppe-Santos; Samantha Maria Nyssen; Bruna Varanda Pessoa; Renata Pedrolongo Basso-Vanelli; Mauricio Jamami; Valéria Amorim Pires Di Lorenzo
Graduate Program of Physical Therapy of UFSCar - São Carlos (SP), Brazil
Correpsondence to
ABSTRACT
The aim of this study was to investigate if there is a relationship between the impact of Chronic Obstructive Pulmonary Disease (COPD) on health status and the level of dyspnea in Activities of Daily Living (ADL) and the mortality predictor index in patients undergoing Pulmonary Rehabilitation (PR). It is a cross-sectional study in which 32 patients with moderate to very severe COPD (23 men; 66.6±12.0 years; FEV1: 40.6±15.6% predicted) were assessed by: COPD Assessment Test (CAT), Body Mass Index (BMI), six-Minute Walking Test (6MWT), London Chest Activity of Daily Living Scale (LCADL), modified Medical Research Council (mMRC) and BODE Index (Body mass index, airflow Obstruction, Dyspnea and Exercise capacity). The CAT score presented moderate correlation with the mMRC questionnaire (r=0.35; p=0.048), total score of LCADL (r=0.60; p<0.001) and total score LCADL percentage (r=0.57; p=0.001). Only the total score of LCADL is able to predict the CAT questionnaire scores (p<0.05; r2=0.61). There were no significant correlations between CAT and BODE index, BMI, FEV1 and 6MWT. Thus, the higher the level of dyspnea in ADL, the greater the impact of COPD on the patient's health status. However, this is not true in relation to mortality prognosis in patients with COPD in PR.
Keywords: Pulmonary Disease, Chronic Obstructive/mortality; Sickness Impact Profile; Activities of Daily Living.
RESUMEN
El objetivo del estudio fue investigar si hay relación entre el impacto de la Enfermedad Pulmonar Obstructiva Crónica (EPOC) en el estado de salud con el nivel de disnea en las actividades de la vida diaria (AVD) y el índice predictor de mortalidad en pacientes en rehabilitación pulmonar (RP). Se trata de un estudio transversal, en el que fueron evaluados 32 pacientes con EPOC moderada a muy grave (23 hombres; 66,6±12,0 años; VEF1: 40,6±15,6% previsto) por medio del COPD Assessment Test (CAT), Índice de Masa Corpórea (IMC), Test de Caminata de Seis Minutos (TC6), London Chest Activity of Daily Living Scale (LCADL), mo dified Medical Research Council (mMRC) e Índice BODE (Body mass index, airflow Obstruction, Dyspnea and Exercise capacity). Se observaron correlaciones positivas moderadas del CAT con el cuestionario mMRC (r=0,35; p=0,048), la puntuación total de la LCADL (r=0,60; p<0,001) y con el porcentaje de la puntuación total de la LCADL (r=0,57; p=0,001). Apenas la puntuación total de la LCADL es capaz de predecir independientemente la puntuación del cuestionario CAT (p<0,05; r2=0,61). No fueron constatadas correlaciones significativas entre el CAT y el Índice BODE, IMC, TC6 e VEF1. De esa forma, cuanto mayor es el nivel de disnea en las AVD, mayor es el impacto de la EPOC en el estado de salud del paciente, entre tanto, lo mismo no ocurre en relación al pronóstico de mortalidad en los pacientes con EPOC en RP.
Palabras clave: Enfermedad Pulmonar Obstructutiva Crónica/mortalidad; Perfil de Impacto de Enfermedad; Actividades Cotidianas.
INTRODUCTION
Patients with Chronic Obstructive Pulmonary Disease (COPD) present with decreased functional capacity and increased minimal effort dyspnea as the disease develops, thus compromising the performance of Activities of Daily Living (ADL), with negative consequences for the quality of life1,2.
In order to define the health status of these patients, some specific instruments are necessary for each of the presented limitations. The mortality risk for patients with COPD has been assessed by the BODE index (Body mass index, airflow obstruction, dyspnea and exercise capacity), considered to be the best survival predictor for these patients3.
With regard to dyspnea, it can be quantified by means of several instruments, among which are the modified Medical Research Council scale (mMRC), which is a component of the BODE index, and the London Chest Activity of Daily Living scale (LCADL), validated for the Brazilian population, with the objective of assessing the sensation of dyspnea in actions of personal hygiene, household chores, physical and leisure activities4,5.
However, these instruments are often complex and require time and technical experience to be used, which makes their use more difficult in the clinical practice6. Therefore, the questionnaire Chronic Obstructive Pulmonary Disease (COPD) Assessment Test (CAT) was created to make the interpretation of health status easier with regard to patients with COPD7. It is a simple questionnaire, easy to apply, with questions concerning general symptoms and the limitations of ADL. Its score was included in the new classification of patients with COPD8, in order to address the drug treatment and define the mortality risk. Scores higher than ten represent patients with greater risks.
However, even though this instrument has been more and more used to characterize the health status of patients with COPD, there are no studies showing if there is a relationship between its score with the ones from specific questionnaires for dyspnea in ADL, and also with mortality risk, verified by the scores in the BODE index and the variables that compose it.
Therefore, the objective of this study was to investigate if there is a relationship between the impact of COPD on health status and the level of dyspnea in ADL, with the scores of BODE index and the variables that compose it.
METHODOLOGY
It is an observational, cross-sectional study, with convenience sample, in which patients diagnosed with COPD were assessed. All of the patients signed the Informed Consent Form after understanding the process, according to resolution 196/96 of the National Health Council. The study was approved by the Research Ethics Committee of the institution.
Patients included were: those with clinical diagnosis of COPD observed in pre and post-bronchodilator spirometry, performed by the pneumologist in charge, classified according to the Global Obstructive Lung Disease (GOLD) from moderate to very severe cases8; the ones who had been clinically stable in the two months prior to the study; those depending or not on oxygen; former smokers; patients with no associated heart, rheumatic, osteomuscular, and orthopedic conditions nor neuromuscular sequelae that could compromise the tests; and the ones who had been on pulmonary rehabilitation (PR) for at least eight weeks. During PR, all of the patients stretched and performed a symptom-limited aerobic training, as well as lower limb and upper lib strengthening exercises (MMII and MMSS) and relaxation. The excluded patients were the ones who did not sign the informed consent form or those who did not fulfill all of the evaluations.
Experimental Procedure
All of the patients were submitted to the following assessments on the same day: collection of anthropometric data, application of the CAT questionnaire, LCADL scale and dyspnea scale mMRC, by means of interviews; besides, there was the Six Minute Walking Test (6MWT), and afterwards the BODE index was calculated.
Anthropometric test
Data such as weight and height were collected with an anthropometric scale from Welmy®, and the Body Mass Index was calculated [BMI = weight (kg)/ height2 (meters)].
Chronic Obstructive Pulmonary Disease Assessment Test
The CAT questionnaire aims at determining the impact of COPD on health status. It is composed of 8 items related to cough, secretion, chest tightness, breathlessness when going up a hill, limitations in activities of daily living, confidence to leave the house, sleep and energy. Scores range from 0 to 5 points for each item, accounting for 40 points. The version in Portuguese was used, since it is validated for the Brazilian population9. Lower scores correspond to the low impact of the disease on health status7. Total score was used for the statistical analysis.
London Chest Activity of Daily Living scale
In order to assess the sensation of dyspnea in ADL, the LCADL scale was used, since it was validated to Portuguese by Pitta et al.5. The scale presents domains concerning personal hygiene, household chores, physical and leisure activities, and the scores range from 0 to 75 points4,5. The higher the score, the greater the limitation caused by dyspnea to perform ADL. Data analysis considered the values for each domain, the total score of LCADL and the percentage of the total score of LCADL (%LCADL) calculated by dividing the total score of LCADL by the number of possible points, when the score is different from zero, and then multiplying it by 100.
Modified Medical Research Concil scale
Patients were asked as to the level of dyspnea by the validated version of the mMRC scale for patients with COPD. Each person chose only one alternative with regard to the sensation of dyspnea, and the higher scores refer to more incapacity. The score is limited to five levels, characterizing the different activities that lead to breathlessness, ranging from zero to four3,10.
Six Minute Walking test
The 6MWT was performed according to the recommendations by ATS11, and patients should walk the longest possible distance in the period of six minutes, with the objective of assessing functional capacity. Two tests were performed on the same day in order to rule out the learning effect, but there was an interval between them so that the values of Heart Rate (HR), Blood Pressure (BP) and Saturation of Peripheral Oxygen (SpO2) could return to the base levels that were obtained prior to the first test, and minimal time was of 30 minutes. The best walked distance (WD) between both tests was considered for analysis.
Body mass index, airflow Obstruction, Dyspnea and Exercise capacity index
In order to calculate the BODE index, the following variables were considered: BMI, forced expiratory volume in one second, as the percentage of the predicted value (pred FEV1 %), mMRC score and WD in the 6MWT (WD6MWT). The score was considered according to the results obtained from the four variables (0-3 for FEV1; 0-3 for mMRC; 0-3 for WD6MWT and 0-1 for BMI)3, and total score ranged from 0 to 10 (higher scores indicate more severity). Patients were also classified in quartiles by the BODE index3.
Statistical Analysis
The Shapiro-Wilk test was performed in order to check the parametric and non-parametric data distribution. For the correlation analysis, the Pearson or Spearman's correlation coefficient was used. For the variables that had a significant correlation with the CAT score, the stepwise linear regression analysis was conducted to identify which variable is able to independently predict the CAT score. The statistical software Statistical Package for the Social Sciences (SPSS) for Windows, version 20.0, was used, and the adopted significance level was p<0.05. After the statistical analysis, the test power was calculated with the software G*Power, version 3.0.10.
RESULTS
Out of the 42 patients who agreed to participate in the study, 10 did not fulfill the evaluations, and the final sample was comprised of 32 patients. Out of these, only seven scored less than 10 in the CAT questionnaire, that is, they presented low impact of COPD on health status.
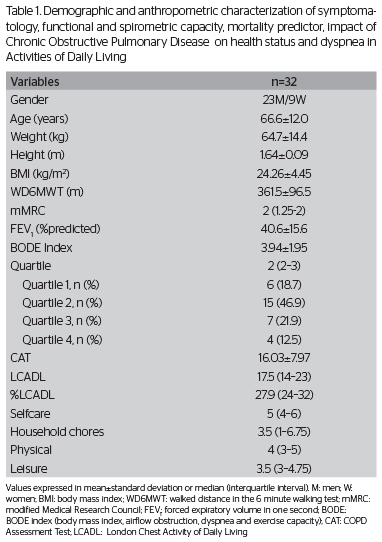
Table 1 presents the anthropometric data, the WD6MWT, the score and the classification of the BODE index and the variables that composse it, besides the total CAT and LCADL score in their domains.
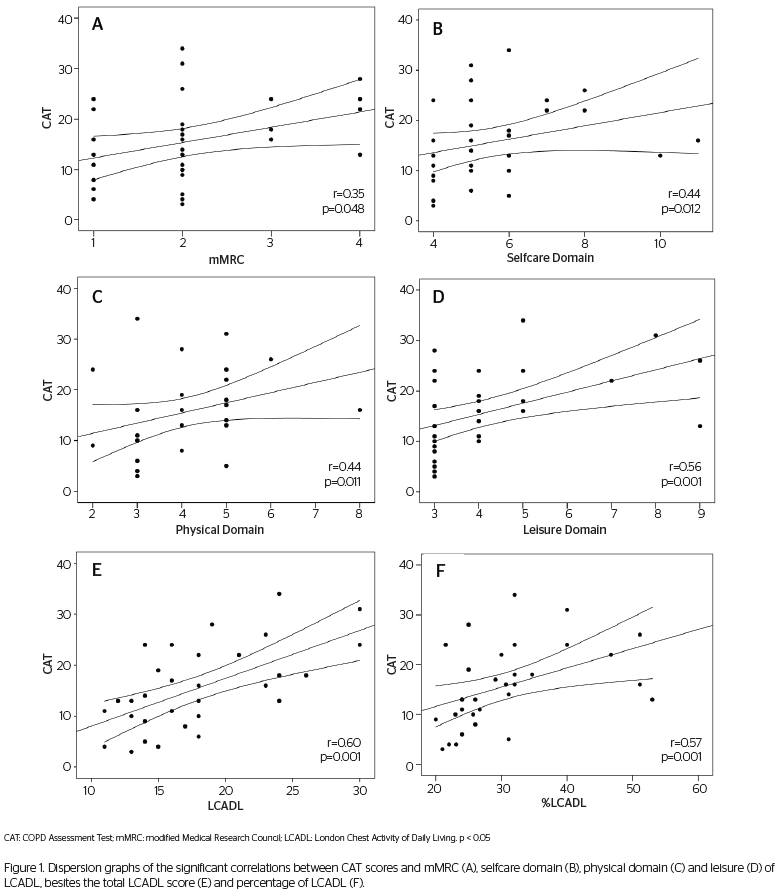
Statistically significant positive correlations were found between the total CAT score with mMRC (r=0.035), total LCADL score (r=0.60), LCADL% (r=0.57), and the domains selfcare (r=0.44), physical care (r=0.44) and leisure (r=0.56) (Table 2). No significant correlations were found between the total CAT score and the other variables. By calculating the test power for these correlations, power stronger than 80% was found in the correlation between CAT with LCADL (98%), LCADL% (96%), and the leisure domain (95%); for the other correlations, the test power was between 50 and 80%, that is, a larger sample would be necessary to provide more consistent results. Figure 1 shows the dispersion graphs of the significant correlations that were found.
After the stepwise linear regression with the independent variables mMRC, LCADL, LCADL%, and the domains of selfcare, physical care and leisure, for the dependent CAT variable, only the LCADL was able to independently predict the score of the CAT questionnaire (p<0.05), and explaining 61% of the total CAT variation (r2=0.61).
DISCUSSION
Our study investigated the relationship between the impact of COPD on health status with the level of dyspnea in ADL, with the score of the BODE index and with the variables that compose it in patients with COPD in PR. The main findings of this study were:
1) moderate correlations between the CAT questionnaire score and the total LCADL score and the percentage of the total LCADL score; 2) the total LCADL score is able to explain 61% of the total variation of the CAT questionnaire score; 3) no relationship was found between the CAT questionnaire and the BODE index, and the variables that compose it (pred FEV1%, WD6MWT and BMI) presented only a slight correlation with mMRC.
The scales and the questionnaire LCADL, mMRC and CAT are instruments that assess the subjective perception of the symptoms among patients with COPD, thus assisting the interpretation of health professionals as to the impact of COPD on activities of daily living, quality of life and well-being of the patients.
In this study, even though there was a relationship between CAT and mMRC, LCADL, %LCADL and the domains of selfcare, physical care and leisure, only the total LCADL score was able to independently predict the CAT score, representing 61% of the CAT variation in the patients inserted in a PR program. These results show that the limitations found in ADL, with regard to dyspnea, reflect the important influence on the impact of COPD on health status, even among patients who already practice regular physical exercises, with time to generate beneficial effects in the performance of the exercise and the reduction of dyspnea12.
The activities involved in the LCADL scale are daily actions, involving personal care, household chores, physical and leisure activities. It is known that patients with COPD avoid activities related to gait development due to the sensation of dyspnea1. Besides, the performance of actions involving MMSS, especially those which present elevation above the shoulder line, results in thoracoabdominal asynchrony and sensation of dyspnea among these patients. As the disease progresses, the symptoms become more intense and more frequent, even at minimal effort, so most severe patients cannot perform daily activities, such as brushing their hair, changing clothes or even caring for personal hygiene13,14. Consequently, patients presenting more perception of dyspnea who perform these activities with difficulties, or can no longer perform them due to the progression of the chronic disease, are the ones who feel the impact of local or systemic consequences of the disease the most, as demonstrated by the results of this study, despite the beneficial effects of PR for our patients. The fact that this study assessed only patients who were participating in a PR program, which produces positive effects in relation to the sensation of dyspnea and functional capacity12,15, may have decreased the strength of the relationships we found. The study by Kovelis et al.15 showed that an intensive training was able to produce significant improvement in the WD6MWT and in the total LCADL score, concerning the domains of selfcare, household chores and leisure.
The correlation found between CAT and the mMRC scale in our study, even with 53% test power, corroborates the results of the study by Jones et al.16, who also found a weak correlation coefficient (r=0.42; p=0.0007) between the CAT score and the mMRC in 63 patients with COPD, and 95% power for this relationship. However, this same study showed a significant statistically weak correlation (r=-0.24; p=0.009) between CAT score and WD6MWT for 121 with COPD, which is different from the result of this study, which did not find this correlation with the WD6MWT. Such difference is attributed to the size of the studied sample, and because our patients were attending a PR program.
The same was true for the CAT score with the BODE index, the BMI and the pred FEV1%. These results suggest that the CAT questionnaire may not be able to reflect objective measurements of functional capacity, pulmonary function and mortality prognosis of these patients on PR. Even though the lower pulmonary function has a negative influence on the health status of the patients, the sensation of dyspnea and the impact of the disease on health status perceived by the patients themselves may not correspond to the severity of the pulmonary obstruction and functional capacity below the expected, since these variables do not directly correspond to the symptoms.
No correlation was found between the impact of COPD on health status and pulmonar function, which corroborates the study by Jones et al.16, who did not see a significant correlation between CAT and pred FEV1 % (n=61; r=-0.23; p=0.07). However, our result is not completely in accordance with another one by Jones et al.17, who found a weak negative correlation between CAT score and pred FEV1% (n=1817; r=0.23; p<0.001). However, these interpretations should be carefully analyzed, since the test power was lower than 80% for our results, and our patients were participating in the PR, which suggests the conduction of new studies with a larger sample in order to obtain more consistent results for these variables.
Therefore, it is suggested that the level of obstruction of patients with COPD does not reflect the impact of COPD on health status, which means other assessment instruments are necessary to build a broader vision concerning the condition in each patient, similar to the CAT questionnaire, thus being able to offer relevant information by means of more complex questions.
The GOLD 20118 version incorporated the CAT questionnaire or the mMRC scale complementary to spirometry to classify patients with COPD, thus demonstrating the importance of the symptoms in order to assess the severity of the disease, especially among patients with mild to moderate airflow limitation17. Raghavan et al.18 suggested that the CAT could be successfully used to identify patients with COPD in the general population, and it could also assist and address specific assessments and optimized treatment during the clinical practice conducted by health professionals.
In our study, we did not find a relationship between the score in the CAT questionnaire and the BODE index score, that is, patients with higher mortality risk are not the ones who perceive the strongest impact of COPD on health status.
These results are in accordance with another one by Tsiligianni et al.19. Even though the authors did not investigate the correlation between these variables, they assessed the variation of CAT scores in the quartiles of the BODE index and found a major variation of the CAT score in each quartile. In this case, the patients in the third quartile presented worse health status when being assessed by CAT than patients in the fourth quartile with worse prognosis. This could be explained by the fact that patients may adapt their lifestyle to the progression of the disease, thus performing fewer activities that cause dyspnea in relation to those patients with the less severe disease19.
Study limitations
The sample size was not sufficient for some variables, which compromised the maintenance of the results, especially with regard to the BODE index and its variables. New studies are required, involving more patients, so that the results can be more consistent.
CONCLUSION
The perception of dyspnea reported in ADL is related to the impact of COPD on the health status of patients with moderate do very severe COPD in PR, so, it does not necessarily occur in relation to objective measurements of obstruction, functional capacity and prognosis. Therefore, only the level of dyspnea in ADL, but not the mortality prognosis, can tell us about the health status of these patients.
REFERENCES
- 1. Dourado VZ, Antunes LC, Tanni SE, de Paiva SA, Padovani CR, Godoy I. Relationship of upper-limb and thoracic muscle strength to 6-min walk distance in COPD patients. Chest. 2006;129(3):551-7.
- 2. Orozco-Levi, M. Structure and function of the respiratory muscles in patients with COPD: impairment or adaptation? Eur Respir J Suppl. 2003;46:41s-51s.
- 3. Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005-12.
- 4. Garrod R, Bestall JC, Paul EA, Wedzicha JA, Jones PW. Development and validation of a standardized measure of activity of daily living in patients with severe COPD: the London Chest Activity of Daily Living scale (LCADL). Respir Med. 2000;94(6):589-96.
- 5. Pitta F, Probst VS, Kovelis D, Segretti NO, Mt Leoni A, Garrod R, et al. Validation of the Portuguese version of the London Chest Activity of Daily Living Scale (LCADL) in chronic obstructive pulmonary disease patients. Rev Port Pneumol. 2008;14(1):27-47.
- 6. Dodd JW, Hogg L, Nolan J, Jefford H, Grant A, Lord VM, et al. The COPD assessment test (CAT): response to pulmonary rehabilitation. A multicentre, prospective study. Thorax. 2011;66(5):425-9.
- 7. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648-54.
- 8. Global Initiative for Chronic Obstructive Lung Disease [Internet]. 2010. [cited 2012 Fev 5]. Available from: http://www.goldcopd.org
- 9. da Silva GP, Morano MT, Viana CM, Magalhães CB, Pereira ED. Portuguese-language version of the COPD Assessment Test: validation for use in Brazil. J Bras Pneumol. 2013;39(4):402-8.
- 10. Kovelis D, Segretti NO, Probst VS, Lareau SC, Brunetto AF, Pitta F. Validation of the Modified Pulmonary Functional Status and Dyspnea Questionnaire and the Medical Research Council scale for use in Brazilian patients with chronic obstructive pulmonary disease. J Bras Pneumol. 2008;34(12):1008-18.
- 11. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111-7.
- 12. Spruit MA, Singh SJ, Garvey C, Zuwallack R, Nici L, Rochester C, et al. An offcial american thoracic society/european respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13-64.
- 13. Regueiro EMG, Lorenzo VAP, Parizotto APD, Negrini F, Sampaio LMM. Análise da demanda metabólica e ventilatória durante a execução de atividades de vida diária em indivíduos com doença pulmonar obstrutiva crônica. Rev Latino-am Enfermagem. 2006;14(1):41-7.
- 14. Velloso M, Stella SG, Cendon S, Silva AC, Jardim JR. Metabolic and ventilatory parameters of four activities of daily living accomplished with arms in COPD patients. Chest. 2003;123(4):1047-53.
- 15. Kovelis D, Zabatiero J, Oldemberg N, Colange AL, Barzon D, Nascimento CH, et al. Responsiveness of three instruments to assess self-reported functional status in patients with COPD. COPD. 2011;8(5):334-9.
- 16. Jones PW, Harding G, Wiklund I, Berry P, Tabberer M, Yu R, et al. Tests of the responsiveness of the COPD assessment test following acute exacerbation and pulmonary rehabilitation. Chest. 2012;142(1):134-40.
- 17. Jones PW, Brusselle G, Dal Negro RW, Ferrer M, Kardos P, Levy MlL, et al. Properties of the COPD assessment test in a cross-sectional European study. Eur Respir J. 2011;38(1):29-35.
- 18. Raghavan N, Lam YM, Webb KA, Guenette JA, Amornputtisathaporn N, Raghavan R, et al. 2012. Components of the COPD Assessment Test (CAT) associated with a diagnosis of COPD in a random population sample. COPD. 2012;9(2):175-83.
- 19. Tsiligianni IG, van der Molen T, Moraitaki D, Lopez I, Kocks JW, Karagiannis K, et al. Assessing health status in COPD. A head-to-head comparison between the COPD assessment test (CAT) and the clinical COPD questionnaire (CCQ). BMC Pulm Med. 2012;12:20.
Chronic obstructive pulmonary disease assessment test in assessing of patients with chronic obstructive pulmonary disease: there is a relationship with activities of daily living and mortality predictor index? A cross-sectional study
Publication Dates
-
Publication in this collection
23 Jan 2014 -
Date of issue
Dec 2013
History
-
Received
June 2013 -
Accepted
Nov 2013