ABSTRACT
The assessment of inspiratory muscles through the inspiratory muscle endurance test (IME), defined as the ability to support this task over time, currently presents wide range of instruments and procedures for its measurement. This study aimed to identify the different equipment, procedures and assessments of IME tests among Brazilian physical therapists. It is a cross-sectional study carried out through a questionnaire sent individually by electronic mail to each participant. One hundred and thirteen physical therapists from different regions of the country, many practicing in the clinic and in the teaching field (52.1%), said they measured IME a few times (48.7%). The aneroid manovacuometer was used by 42.5% of the professionals. The nose clip and the hard plastic or paper tubular incentive spirometer were the most used accessories during the test, corresponding to 51.8% and 33%, respectively. The maximum voluntary ventilation test was used to assess the inspiratory endurance, reported by 23% of the respondents. The constant load test for endurance assessment was adopted by 51.2% of the physical therapists, and 54.9% associated verbal commands with the demonstration for the test application. The interpretation of the measured values was made with reference values by 25.7% of respondents. We identified that Brazilian physical therapists interviewed did not show the same conduct for IME tests. However, the equipment, procedures and assessment form are used based on the guidelines on the subject and according to the availability of resources of the service.
Keywords
Respiratory Functional Tests; Respiratory Muscle Endurance; Diagnostic Equipment; Physical Therapy
RESUMO
A avaliação da função dos músculos inspiratórios por meio do teste de endurance muscular inspiratória (EMI), definida como a capacidade de sustentação dessa tarefa ao longo do tempo, atualmente apresenta ampla variedade de instrumentos e procedimentos para sua mensuração. Este estudo teve como objetivo identificar os diferentes equipamentos, procedimentos e forma de avaliação dos testes de EMI entre fisioterapeutas brasileiros. É um estudo transversal realizado por meio de questionário enviado por correio eletrônico individualmente a cada participante. Cento e treze fisioterapeutas de diferentes regiões do país, grande parte com atuação conjunta na clínica e na docência (52,1%), responderam realizar poucas vezes a medida de EMI (48,7%). O manovacuômetro aneroide foi o aparelho mais utilizado por 42,5% dos profissionais. O clipe nasal e o bocal tubular de plástico rígido ou papel foram os acessórios mais utilizados durante o teste, correspondendo a 51,8% e 33%, respectivamente. O teste de ventilação voluntária máxima foi o mais utilizado para avaliação da endurance inspiratória, relatado por 23% dos respondentes. O teste de carga constante para avaliação da endurance foi adotado por 51,2% dos fisioterapeutas, sendo que 54,9% associaram comandos verbais à demonstração para explicação do teste. A interpretação dos valores aferidos era feita através de valores de referência por 25,7% dos entrevistados. Identificou-se que os fisioterapeutas brasileiros entrevistados não apresentaram a mesma conduta para os testes de EMI. No entanto os equipamentos, procedimentos e a forma de avaliação são utilizados com base nas diretrizes sobre o tema e de acordo com a disponibilidade de recursos do serviço.
Descritores
Testes de Função Respiratória; Resistência Muscular Respiratória; Equipamentos para Diagnóstico; Fisioterapia
RESUMEN
La evaluación de la función de los músculos inspiratorios a través del entrenamiento muscular inspiratorio (EMI), definida como la capacidad de sustentación de esta tarea a lo largo del tiempo, actualmente presenta una amplia variedad de instrumentos y procedimientos para su medición. Este estudio tuvo como objetivo identificar los diferentes equipos, procedimientos y forma de evaluación de las pruebas de EMI entre fisioterapeutas brasileños. Es un estudio transversal realizado por medio de un cuestionario enviado por correo electrónico a cada participante. Ciento trece fisioterapeutas de diferentes regiones del país, que en gran parte actúan a la vez en la clínica y en la enseñanza (52,1%), dijeron realizar pocas veces la medida de EMI (48,7%). El manovacuómetro aneroide fue el aparato más utilizado por el 42,5% de los profesionales. El clip nasal y la boquilla tubular de plástico rígido o papel fueron los accesorios más utilizados durante la prueba, correspondiendo al 51,8% y al 33%, respectivamente. La prueba de ventilación voluntaria máxima fue la más utilizada para la evaluación de la resistencia respiratoria, reportada por el 23% de los entrevistados. La prueba de carga constante para la evaluación de la resistencia se adoptó por el 51,2% de los fisioterapeutas, siendo que el 54,9% asoció comandos verbales a la demostración para la explicación de la prueba. La interpretación de los valores evaluados se hacía a través de valores de referencia por el 25,7% de los entrevistados. Se identificó que los fisioterapeutas brasileños entrevistados no presentaron la misma conducta para las pruebas de EMI. Sin embargo, los equipos, procedimientos y la forma de evaluación se utilizan con base en las directrices sobre el tema y de acuerdo con la disponibilidad de recursos del servicio.
Palabras clave
Pruebas de Función Respiratoria; Resistencia Muscular Respiratoria; Equipo para Diagnóstico; Fisioterapia
INTRODUCTION
The assessment of the inspiratory muscle function can be measured through the properties of strength and endurance, which, operationally, are investigated by tests of maximal inspiratory pressure (MIP) and inspiratory muscle endurance (IME)11. Macklem PT. The diaphragm in health and disease. J Lab Clin Med. 1982;99(5):601-10.. The MIP test infers about the ability of the inspiratory muscles group to generate maximum strength, and IME reflects the buoyancy of a certain task over time11. Macklem PT. The diaphragm in health and disease. J Lab Clin Med. 1982;99(5):601-10.),(22. Clanton T, Calverly PM, Celli BR. Tests of respiratory muscle endurance. Am J Respir Crit Care Med. 2002;166(4):559-70. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
. Although both measures are closely related to some health conditions, and MIP is widely accepted and used, the measurement of inspiratory endurance is important for clinical assessment and investigation of specific populations in response to treatments and rehabilitation programs, for example, in individuals with asthma, cystic fibrosis, chronic obstructive pulmonary disease (COPD)33. American Thoracic Society, European Respiratory Society. ATS/ERS Statement on Respiratory Muscle Testing. Am J Respir Crit Care Med. 2002;166(4):518-624. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
, after myocardial infarction44. Neves LMT, Karsten M, Neves VR, Beltrame T, Borghi-Silva A, Catai AMC. Respiratory muscle endurance is limited by lower ventilatory efficiency in post-myocardial infarction patients. Braz J Phys Ther. 2014;18(1):1-8. doi: 10.1590/S1413-35552012005000134
https://doi.org/10.1590/S1413-3555201200...
, and in studies with children and adolescents55. Woszezenki CT, Heinzmann-Filho JP, Vendrusculo FM, Piva TC, Levices I, Donadio MVF. Reference values for inspiratory muscle endurance in healthy children and adolescents. PLoS ONE. 2017;12(1):1-12. doi: 10.1371/journal.pone.0170696
https://doi.org/10.1371/journal.pone.017...
.
The wide variety of procedures to measure IME differs on the type of task performed, being characterized by different motor recruitment patterns and muscle synergy. The task is maintained up to the point of disability, being defined as failure. Under this concept, a few repetitions of a task are held at high levels of intensity; on the contrary, with the decrease of the load, the task can be sustained for a longer time. Another estimate of IME is done by increasing the intensity of the task for a period of time to identify the peak, i.e. the maximum overload. In this case, failure is also defined as the inability to maintain the task22. Clanton T, Calverly PM, Celli BR. Tests of respiratory muscle endurance. Am J Respir Crit Care Med. 2002;166(4):559-70. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
.
According to the guidelines of the scientific societies American Thoracic Society and European Respiratory Society (ATS/ERS)33. American Thoracic Society, European Respiratory Society. ATS/ERS Statement on Respiratory Muscle Testing. Am J Respir Crit Care Med. 2002;166(4):518-624. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
, despite the variety of procedures, the main ones for this purpose are the measures of respiratory muscle activity, ventilation tests, external load tests and those specific to the diaphragm22. Clanton T, Calverly PM, Celli BR. Tests of respiratory muscle endurance. Am J Respir Crit Care Med. 2002;166(4):559-70. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
),(66. Sturdya GA, Hillman DR, Green DJ, Jenkinsc SC, Cecins NM, Eastwood PR. The effect of learning on ventilatory responses to inspiratory threshold loading in COPD. Respir Med. 2004;98(1):1-8. doi: 10.1016/j.rmed.2003.07.005
https://doi.org/10.1016/j.rmed.2003.07.0...
. Among the external load tests, the most employed type of overload is linear, in which a particular pressure is required for the opening of the inspiratory valve, regardless of flow and volume. In this kind of technique, there can be constant or incremental load exercises. There are still three other types of overload: the resistive one, in which the pressure required depends on the flow, being necessary to achieve target pressure so that the intensity of load is adequate; the elastic one, in which the pressure depends on the tidal volume; and, finally, the one of constant flow22. Clanton T, Calverly PM, Celli BR. Tests of respiratory muscle endurance. Am J Respir Crit Care Med. 2002;166(4):559-70. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
),(77. Gosselink R, Wagenaar RC, Decramer M. Reliability of a commercially available threshold loading device in healthy subjects and in patients with chronic obstructive pulmonary disease. Thorax. 1996;51(6):601-5..
Among the types of equipment used in the assessment of IME, there are those of nonlinear and linear resistance. In the first category, holes of different sizes are used, and the respiratory pattern adopted by the individual is proportional to the resistance and to the load applied to the inspiratory muscles. The size of the hole has influence over the inspiratory pressure generated and also over the inspired flow rate88. Belman MJ, Thomas SG, Lewis MI. Resistive breathing training in patients with chronic obstructive pulmonary disease. Chest. 1986;90(5):662-9. doi: 10.1378/chest.90.5.662
https://doi.org/10.1378/chest.90.5.662...
. In the linear resistors, the inspiratory pressure does not depend on the flow, since this model has a calibrated valve. The individual generates limit pressure, predetermined at each breath, which is able to open the valve and allow air flow. This last model, through threshold loading, is recommended and used in clinical practice and more frequently in studies for assessment and of inspiratory muscle training99. Johnson PH, Cowley AJ, Kinnear WJM. Evaluation of the Threshold(r) trainer for inspiratory muscle endurance training: comparison with the weighted plunger method. Eur Respir J. 1996;9(12):2681-4. doi: 10.1183/09031936.96.09122681
https://doi.org/10.1183/09031936.96.0912...
(IMT), with continuous or incremental load exercises1010. Alves LA, Brunetto AF. Adaptação do Threshold(r) IMT para teste de resistência dos músculos inspiratórios. Rev Bras Fisioter. 2006;10(1):105-12. doi: 10.1590/S1413-35552006000100014
https://doi.org/10.1590/S1413-3555200600...
.
As an alternative to approach the limitations of the techniques and equipment currently available, a new device whose overload is provided by an electronically controlled valve and dynamically adjusted has been studied and developed, providing representative variables of the magnitude of the task subject to the inspiratory muscles, such as external work and inspiratory power. This device has been validated by a gold standard equipment through an endurance test with a representative load of 55±13% of its MIP. The valve performs real-time adjustments to accommodate changes of respiratory airflow and keep the same relative intensity (percentage of MIP) in the spectrum of the vital capacity1111. Langer D, Jacome C, Charusin N, Scheer H, McConnel A, Decramer M, et al. Measurement validity of an electronic inspiratory loading device during a loaded breathing task in patients with COPD. Respir Med. 2013;107(4):633-5. doi: 10.1016/j.rmed.2013.01.020
https://doi.org/10.1016/j.rmed.2013.01.0...
.
The IME test, added to the lack of methodological standardization and to the lack of commercially available devices, is still incipient in the clinical practice of physical therapists. Considering this, the aim of this study was to identify the different equipment, procedures and forms of assessment of IME tests among Brazilian physical therapists who work in clinical practice and/or research in the field of cardiorespiratory physical therapy and in intensive care.
METHODOLOGY
This is a cross-sectional study, conducted through the application of a questionnaire prepared in the website SurveyMonkey® and individually sent via e-mail to each participant. Previously, the participants were informed about the content and the purpose of the questionnaire, which was answered only after they read and signed the informed consent form (ICF). In ICF there was the option to decline participation in the study. The research project has been approved by the Research Ethics Committee of Universidade Federal de Minas Gerais (UFMG).
The questionnaire, based on specific literature on the IME tests, contains the total of 19 questions, 18 of them were multiple choice questions (most with four alternatives and only one response option) and one was a discursive question. The initial questions (from number 1 to 9) were related to the characterization of the professionals, followed by questions concerning equipment, procedures, and interpretation of the measures (from number 10 to 19). On questions concerning the accessories used for the test and the load used for assessment more than one response was possible, among seven and five, alternatives, respectively. At the end, a space was reserved for possible comments. Prior to its submission, the questionnaire was assessed separately by four specialists regarding the criteria of comprehensiveness, objectivity and relevance. After the assessment, the instrument underwent minor changes according to the criticisms and suggestions expressed, resulting in the final version used.
The questionnaire was sent to members of the Brazilian Association of Cardiorespiratory Physiotherapy and Physical Therapy in Intensive Care (Assobrafir). Initially, we made contact with the scientific board of the association to facilitate the direction of the questionnaire to professionals, which was sent back after 30 days to encompass a greater number of physical therapists.
The response data extracted from the website SurveyMonkey® were converted to Microsoft Office Excel spreadsheets (Excel®, Redmond, WA, USA), version 10.0, and then analyzed in the Statistical Package for Social Science software (SPSS®, Chicago, IL, USA), version 15.0. In the descriptive analysis, data were represented in frequency (absolute, n, and/or relative, %).
RESULTS
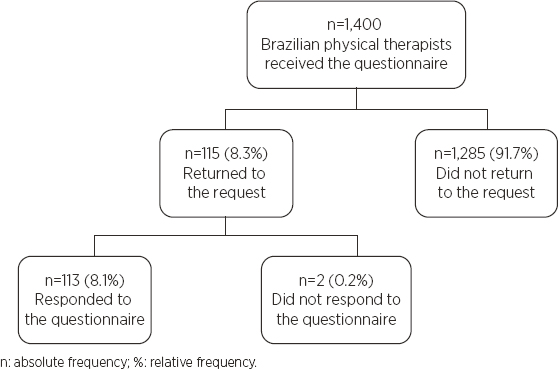
The questionnaire was sent to 1,400 physical therapists, of which 115 returned the contact, 113 (8.1%) answering the questionnaire and two refusing to participate through the ICF, as the flowchart in Figure 1 illustrates.
Regarding the area of practice, most physical therapists who answered the questionnaire work in the clinic and in the teaching field (52.1%), and the average time of professional performance was 12.3±8.1 years. As for the professional education, professionals with specialization and master’s degrees totaled 77% of the sample. Table 1 shows data concerning the professional characterization of the participants.
Although 48.7% of professionals have claimed to measure IME only a few times, 52.2% often perform the IMT, as shown in Chart 1. Regarding the development of research related to the theme, 69.1% of the physical therapists answered they had never participated in one.
Relative frequency of the inspiratory muscle endurance measure and inspiratory muscle training
Table 2 presents the characteristics of the equipment and accessories used for the IME test. We observed that the aneroid manovacuometer was the most used model by professionals, just as the nose clip and the hard plastic or paper tubular incentive spirometer are the most used accessories during the test.
Regarding the equipment used for the measure of endurance, 25.8% of the physical therapists use the same device for measurement and training of inspiratory muscle; however, the majority of the sample (53.9%) does not use the same equipment for measurement of IME and IMT.
The maximum voluntary ventilation test is the most used to assess IME, being reported by 23% of the physical therapists, followed by the external load tests with maximum incremental load and constant inspiratory load (Table 3). Regarding the load (% of MIP) used to assess endurance, 51.2% of the physical therapists adopt the constant load test, 42.5% use the initial percentage of MIP in the incremental load test, and 28.7% reported using the successive increase of MIP; the remaining 35%, however, use another type of test or do not apply any.
Regarding the explanation passed on to the individuals before the IME test, 54.9% (52) of the physical therapists associated verbal commands with the demonstration, while 16.9% (19) only gave verbal command, and less than 1% (1) only used demonstration; the others, 27.4% (30), responded “not applicable.” During the test run, only 63.7% (71) of the respondents used some kind of verbal command. However, 46.1% (52) did not use any stimulus during the IME test. And 35.4% (40) of the professionals were under some sort of guidance in relation to the breathing pattern during the test run.
As to the interpretation of the values measured, 73.5% (83) of the individuals responded. Of these, 25.7% (29) of respondents used reference values, while 21.2% (24) adopted predictive equations, and the others used another form of interpretation or said the question did not apply - 8.9% (10) and 17.7% (20), respectively.
Finally, the space intended for any comments (optional) was filled by 20.3% (23) of the sample. In the comments, the physical therapists mentioned the lack of necessary equipment to carry out the measure of endurance and IMT, mainly on the public network (8.9%). Other 6.9% say they only measure maximal expiratory and inspiratory pressure (MIP and MEP), and not that of IME. In addition, the difficulty of adopting protocols in intensive care units (ICU) was mentioned, as well as the absence of trained professionals for carrying out the procedures (4.5%).
DISCUSSION
This study, whose objective was to identify the equipment, procedures and interpretation form of IME tests adopted between Brazilian physical therapists, showed that the professionals who filled and answered the questionnaire do not present a similar conduct in their work routine. In addition, it was possible to present a brief overview to these professionals regarding the applicability of IME in the country.
The professionals, the majority being (31%) resident in the southeastern region of the country, have specialization and master’s degree as their main academic qualification, in addition to working partly in teaching and in the clinic field, especially in the public network. These results, in similarity with other studies1212. Coury HJCG, Vilella I. Profile of the Brazilian physical therapy researcher. Braz J Phys Ther. 2009;13(4):356-63. doi: 10.1590/S1413-35552009005000048
https://doi.org/10.1590/S1413-3555200900...
),(1313. Costa D. Ten years of stricto sensu postgraduate programs in physical therapy in Brazil: what has changed? Braz J Phys Ther. 2007;11(1):1-2. doi: 10.1590/S1413-35552007000100001
https://doi.org/10.1590/S1413-3555200700...
, reflect the region of the country with the highest concentration of professionals and of centers of teaching and research in physical therapy.
As to the conditions of strength and IME, MIP was also the test most frequently used by the professionals interviewed in this study. It is a test used to assess global inspiratory muscle strength1414. Green M, Road J, Sieck GC, Similowski C. Tests of respiratory muscle strenght. Am J Respir Crit Care Med. 2002;166(4):528-47. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
),(1515. Montemezzo D, Velloso M, Britto RR, Parreira VF. Pressões respiratórias máximas: equipamentos e procedimentos usados por fisioterapeutas brasileiros. Fisioter Pesq. 2010;17(2):147-52. doi: 10.1590/S1809-29502010000200010
https://doi.org/10.1590/S1809-2950201000...
and suggested as diagnostic parameter for inspiratory muscle weakness1616. Charususin N, Gosselink R, Decramer M, McConnell A, Saey D, Maltais F, et al. Inspiratory muscle training protocol for patients with chronic obstructive pulmonary disease (IMTCO study): a multicentre randomised controlled trial. BMJ Open. 2013;3(8):1-7. doi: 10.1136/bmjopen-2013-003101
https://doi.org/10.1136/bmjopen-2013-003...
).(1717. Lötters F, van Tol B, Kwakkel G, Gosselink R. Effects of controlled inspiratory muscle training in patients with COPD: a meta-analysis. Eur Respir. 2002;20(3):570-6. doi: 10.1183/09031936.02.00237402
https://doi.org/10.1183/09031936.02.0023...
. The relevance of MIP as a single measure appears to be insufficient to portray the inspiratory muscle function, since from the clinical and physiological point of view, individuals rarely need to generate maximum pressures during the activities of daily living (ADV). As the demands for these muscles during the ADV are submaximal and, for the most part, require a longer time of muscular activity, measures of inspiratory muscle function over time possibly have a higher clinical and functional relevance than the measures of force made separately66. Sturdya GA, Hillman DR, Green DJ, Jenkinsc SC, Cecins NM, Eastwood PR. The effect of learning on ventilatory responses to inspiratory threshold loading in COPD. Respir Med. 2004;98(1):1-8. doi: 10.1016/j.rmed.2003.07.005
https://doi.org/10.1016/j.rmed.2003.07.0...
),(1818. Hill K, Jenkins SC, Philippe DL, Shepherd KL, Hillman DR, Eastwood PR. Comparison of incremental and constant load tests of inspiratory muscle endurance in COPD. Eur Respir J. 2007;30(3):479-86. doi: 10.1183/09031936.00095406
https://doi.org/10.1183/09031936.0009540...
. Therefore, considering the submaximal demand of the inspiratory muscles, endurance tests have a higher relevance from the functional point of view1818. Hill K, Jenkins SC, Philippe DL, Shepherd KL, Hillman DR, Eastwood PR. Comparison of incremental and constant load tests of inspiratory muscle endurance in COPD. Eur Respir J. 2007;30(3):479-86. doi: 10.1183/09031936.00095406
https://doi.org/10.1183/09031936.0009540...
.
For the type of equipment used for IME measurement, the results corroborate with the study by Montemezzo et al.1515. Montemezzo D, Velloso M, Britto RR, Parreira VF. Pressões respiratórias máximas: equipamentos e procedimentos usados por fisioterapeutas brasileiros. Fisioter Pesq. 2010;17(2):147-52. doi: 10.1590/S1809-29502010000200010
https://doi.org/10.1590/S1809-2950201000...
, according to whom analog is the most used type of manovacuometer in Brazil. The model most commonly used for the measurement of endurance1010. Alves LA, Brunetto AF. Adaptação do Threshold(r) IMT para teste de resistência dos músculos inspiratórios. Rev Bras Fisioter. 2006;10(1):105-12. doi: 10.1590/S1413-35552006000100014
https://doi.org/10.1590/S1413-3555200600...
),(1919. Johnson PH, Cowley AJ, Kinnear WJM. Incremental threshold loading: a standard protocol and establishment of a reference range in naïve normal subjects. Eur Respir J. 1997;10(12):2868-71. doi: 10.1183/09031936.97.10122868
https://doi.org/10.1183/09031936.97.1012...
, Threshold® IMT, was adopted by 15% of respondents, but has as limiting factor the range of inspiratory pressure application restricted to 40 cmH2O22. Clanton T, Calverly PM, Celli BR. Tests of respiratory muscle endurance. Am J Respir Crit Care Med. 2002;166(4):559-70. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
; while the model whose load is adjusted electronically was used by 10.6% of the physical therapists of the sample. These results reflect the reality of clinical practice of Brazilian professionals: although digital equipment present considerable advantages33. American Thoracic Society, European Respiratory Society. ATS/ERS Statement on Respiratory Muscle Testing. Am J Respir Crit Care Med. 2002;166(4):518-624. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
, they still are not accessible.
As to the accessories, studies have verified the influence of the shape of different types of incentive spirometer used in measurements of MIP and MEP. Gibson2020. Gibson GJ. Measurement of respiratory muscle strength. Respir Med. 1995;89(8):529-35. doi: 10.1016/0954-6111(95)90153-1
https://doi.org/10.1016/0954-6111(95)901...
has developed a review study on respiratory muscle strength measurements and concluded that the measurement of maximum respiratory pressure (MRP) is strongly influenced by incentive spirometers; however, the results of this review do not suggest a most appropriate type for carrying out the measurements. Studies by Koulouris et al.2121. Koulouris N, Mulvey DA, Laroche CM, Green M, Moxham J. Comparison of two different mouthpieces for the measurement of PImax and PEmax in normal and weak subjects. Eur Respir J. 1988;1(9):863-7. and Rubinstein et al.2222. Rubinstein I, Slutsky AS, Rebuck AS, McClean PA, Boucher R, Szeinberg A, et al. Assessment of maximal expiratory pressure in healthy adults. J Appl Physiol. 1988;64(5):2215-9. doi: 10.1152/jappl.1988.64.5.2215
https://doi.org/10.1152/jappl.1988.64.5....
concluded that the interface between the individual and the manovacuometer influence the values of MRP, since, according to the used incentive spirometer, there is a difference regarding the activation and the coordination of muscle groups. In this sense, a recent study2323. Montemezzo D, Vieira DS, Tierra-Criollo CJ, Britto RR, Velloso M, Parreira VF. Influence of 4 interfaces in the assessment of maximal respiratory pressures. Respir Care. 2012;57(3):392-8. doi: 10.4187/respcare.01078
https://doi.org/10.4187/respcare.01078...
suggests the use of incentive spirometers that ensure greater comfort to the individual during the test run. To date no studies that examined the influence of interfaces on IME measurements were found. However, there is speculation that there may be contribution to the accessory use in the capacity developed in IME tests. Future studies are needed to address this issue.
In relation to IME tests, although 23% of the volunteers have reported using the maximum voluntary ventilation test, added, 36.3% of the physical therapists reported using external load tests, with incremental or constant load exercise. According to Hill et al.1818. Hill K, Jenkins SC, Philippe DL, Shepherd KL, Hillman DR, Eastwood PR. Comparison of incremental and constant load tests of inspiratory muscle endurance in COPD. Eur Respir J. 2007;30(3):479-86. doi: 10.1183/09031936.00095406
https://doi.org/10.1183/09031936.0009540...
, external resistance tests have as outcome the maximum sustained load pressure in the protocol for incremental load or the time until exhaustion in the protocol for constant-load exercise. An advantage of these types of IME test is to control the outcome variable, i.e. the sustained load and the time spent for its execution22. Clanton T, Calverly PM, Celli BR. Tests of respiratory muscle endurance. Am J Respir Crit Care Med. 2002;166(4):559-70. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
),(66. Sturdya GA, Hillman DR, Green DJ, Jenkinsc SC, Cecins NM, Eastwood PR. The effect of learning on ventilatory responses to inspiratory threshold loading in COPD. Respir Med. 2004;98(1):1-8. doi: 10.1016/j.rmed.2003.07.005
https://doi.org/10.1016/j.rmed.2003.07.0...
.
For the type of overload used for IME evaluation there are various protocols described in the literature. Johnson, Cowley and Kinnear1919. Johnson PH, Cowley AJ, Kinnear WJM. Incremental threshold loading: a standard protocol and establishment of a reference range in naïve normal subjects. Eur Respir J. 1997;10(12):2868-71. doi: 10.1183/09031936.97.10122868
https://doi.org/10.1183/09031936.97.1012...
established a protocol with progressive linear load sustainable for two minutes. The technique with initial pressure of 10 cmH2O, consisted of progressive increases of 5 cmH2O pressure every two minutes, which was interrupted when the individual could not open the relief valve for two consecutive respiratory incursions. This type of protocol, with incremental load exercise, was reported by 28.7% of the sample. Martyn et al.2424. Martyn JB, Moreno RH, Paré PD, Pardy RL. Measurement of inspiratory muscle performance with incremental threshold loading. Am Respir Dis. 1987;135(4):919-23. used a linear inspiratory resistance with progressive increases to measure the performance of the inspiratory muscles. The protocol consists of inspiration from 30% of MIP with increased load every two minutes, from 5 to 10% of MIP. The largest load maintained for two minutes was recorded. This type of protocol was adopted by 42.5% of respondents and is considered more advantageous for not depending on the individual’s prolonged training2424. Martyn JB, Moreno RH, Paré PD, Pardy RL. Measurement of inspiratory muscle performance with incremental threshold loading. Am Respir Dis. 1987;135(4):919-23..
As well as in the study for identification of equipment and procedures for measurements of maximal inspiratory pressure1515. Montemezzo D, Velloso M, Britto RR, Parreira VF. Pressões respiratórias máximas: equipamentos e procedimentos usados por fisioterapeutas brasileiros. Fisioter Pesq. 2010;17(2):147-52. doi: 10.1590/S1809-29502010000200010
https://doi.org/10.1590/S1809-2950201000...
, most respondents associate verbal command with the demonstration to explain the IME test and use it during its implementation. However, only 26% of respondents have some type of feedback during the test run, while 46.1% does not adopt this practice. As the test depended on effort, it is possible that these stimuli influence the performance of the individual. Regarding the type of breathing pattern adopted during the test, used by just over one-third of professionals, the individuals are commonly instructed to keep a diaphragmatic breathing from 15 to 20 respiratory incursions per minute, as used by Dall’Ago et al.2525. Dall'Ago P, Chiappa GR, Guths H, Stein R, Ribeiro JP. Inspiratory muscle training in patients with heart failure and inspiratory muscle weakness: a randomized trial. J Am Coll Cardiol. 2006;47(4):757-63. doi: 10.1016/j.jacc.2005.09.052
https://doi.org/10.1016/j.jacc.2005.09.0...
.
Unlike MIP and MEP measures, which present reference equations for the Brazilian adult population2626. Souza RB. Pressões respiratórias estáticas máximas. J Pneumol. 2002;28(Supl 3):S155-65.),(2727. Pessoa IMBS, Neto MH, Montemezzo D, Silva LAM, Andrade AM, Parreira VF. Predictive equations for respiratory muscle strength according to international and Brazilian guidelines. Braz J Phys Ther. 2014;18(5):410-8. doi: 10.1590/bjpt-rbf.2014.0044
https://doi.org/10.1590/bjpt-rbf.2014.00...
; inspiratory endurance measures do not seem to have normative values. However, ATS/ERS33. American Thoracic Society, European Respiratory Society. ATS/ERS Statement on Respiratory Muscle Testing. Am J Respir Crit Care Med. 2002;166(4):518-624. doi: 10.1164/rccm.166.4.518
https://doi.org/10.1164/rccm.166.4.518...
guidelines provide equations and reference values used for IME measurement. In common, these references present studies with small sample number. Average values were reported between 52 and 77% of MIP for the maximum sustained load method and between 80 and 94% of MIP with the incremental method. However, a cross-sectional and observational study55. Woszezenki CT, Heinzmann-Filho JP, Vendrusculo FM, Piva TC, Levices I, Donadio MVF. Reference values for inspiratory muscle endurance in healthy children and adolescents. PLoS ONE. 2017;12(1):1-12. doi: 10.1371/journal.pone.0170696
https://doi.org/10.1371/journal.pone.017...
conducted with 462 Brazilian children and healthy adolescents, aged from 4 to 18 years, established references for IME after two protocols. In the protocol of incremental load exercise a fixed charge of 30% of the MIP was used with increment of 10% every two minutes. In the protocol of maximum load a fixed charge of 70% of MIP was used and the time limit reached until exhaustion was measured. We observed that IME can be explained as a function of age (r=0.51; p=0.0001), height (r=0.53; p=0.0001) and MIP (r=0.79; p=0.0001), and that the first protocol presented better results and should be the model of choice for IME evaluation between children and adolescents.
Hart et al.2828. Hart N, Hawkins P, Hamnegård CH, Green M, Moxham J, Polkey MI. A novel clinical test of respiratory muscle endurance. Eur Respir J. 2002;19(2):232-239. doi: 10.1183/09031936.02.00247602
https://doi.org/10.1183/09031936.02.0024...
proposed a new clinical trial whose goal was to develop a clinically viable method for IME measurement using negative inspiratory pressure. The study was conducted with 30 healthy individuals exposed to the same target pressure (70% of maximum esophageal pressure). Eight patients with systemic sclerosis/interstitial lung disease were studied to evaluate the validity and acceptability of the technique. The results confirm that the time of endurance can be expressed as a function of the load/respiratory capacity ratio in a number of respiratory strategies, using a constant load and submaximal negative pressure. The use of this ratio can detect changes in the respiratory muscle endurance of individuals with cardiorespiratory disorders. In addition, the pressure of the mouth accurately reflects the esophageal data, and non-invasive IME will allow, in the future, normal values to be established on a larger population.
As for the IMT frequency in clinical practice, although little more than half the sample reported performing it frequently, 34.6% claimed to train a few times, and 7.9% never used. These results coincide with a transversal study2929. Bonnevie T, Villiot-Danger JC, Gravier FE, Dupuis J, Prieur G, Médrinal C. Inspiratory muscle training is used in some intensive care units, but many training methods have uncertain efficacy: a survey of French physiotherapists. J Physiother. 2015;61(4):204-9. doi: 10.1016/j.jphys.2015.08.003
https://doi.org/10.1016/j.jphys.2015.08....
carried out in France with 265 physical therapists of ICU. Through a specific questionnaire, only 36% of the professionals interviewed declared using the IMT. Among the main reasons for not using it, 64% indicated the lack of knowledge of this technique in ventilated patients. In general, the study identified that most respondents who use IMT also use uncertain methods without assessing the maximal inspiratory pressure (p<0.0001).
The limitation of this qualitative study was the low rate of accession of professionals who received the questionnaire by e-mail - only 8.1% of respondents. The utilization rate was lower than in other studies3030. Carling C. International questionnaire postal response rate: an experiment comparing no return postage to provision of International Postage Vouchers - "Coupon-Réponse International". BMC Health Serv Res. 2004;4:16[3 p.]. doi: 10.1186/1472-6963-4-16
https://doi.org/10.1186/1472-6963-4-16...
),(3131. Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2009;3: MR000008 [527 p.]. doi: 10.1002/14651858.MR000008.pub4
https://doi.org/10.1002/14651858.MR00000...
, in which printed questionnaires were sent via conventional mail and whose utilization rate of the responses ranged between 12 and 25%; in a survey conducted by telephone, the response rate reached 99%2929. Bonnevie T, Villiot-Danger JC, Gravier FE, Dupuis J, Prieur G, Médrinal C. Inspiratory muscle training is used in some intensive care units, but many training methods have uncertain efficacy: a survey of French physiotherapists. J Physiother. 2015;61(4):204-9. doi: 10.1016/j.jphys.2015.08.003
https://doi.org/10.1016/j.jphys.2015.08....
. In addition to the low rate of accession, some questions have not been fully answered by participants, being left blank. Also, the literature that discusses the subject is restricted, and it is assumed that the lack of methodological standardization regarding the IME measurement can lead to conflicting results in the surveys and also in clinical practice.
CONCLUSION
Although the Brazilian physical therapists interviewed do not show a similar conduct in relation to tests for IME measurement, the questionnaire adopted allowed us to identify that the tests have been carried out by part of the sample, based on the guidelines published on the subject and according to the availability of resources for each service. And, even with different conduct, the equipment, procedures and the form of assessment adopted presented data for the proposed review. Before the impact of these results, further study is required toward a recommendation of equipment and testing methods of IME, such as MIP and MEP tests, contributing positively to the physical therapeutic practice in practice clinic and for advances in research.
ACKNOWLEDGEMENTS
We thank the physical therapists Verônica Franco Parreira, PhD; Giane Amorin Ribeiro-Samora, PhD; Liliane Patrícia Souza Mendes, MSc; e Letícia Silva Gabriel, MSc. for their availability and valuable contributions to the construction of the questionnaire used in this study. We also thank Assobrafir for the important aid in targeting the material to professional partners.
REFERÊNCIAS
-
1Macklem PT. The diaphragm in health and disease. J Lab Clin Med. 1982;99(5):601-10.
-
2Clanton T, Calverly PM, Celli BR. Tests of respiratory muscle endurance. Am J Respir Crit Care Med. 2002;166(4):559-70. doi: 10.1164/rccm.166.4.518
» https://doi.org/10.1164/rccm.166.4.518 -
3American Thoracic Society, European Respiratory Society. ATS/ERS Statement on Respiratory Muscle Testing. Am J Respir Crit Care Med. 2002;166(4):518-624. doi: 10.1164/rccm.166.4.518
» https://doi.org/10.1164/rccm.166.4.518 -
4Neves LMT, Karsten M, Neves VR, Beltrame T, Borghi-Silva A, Catai AMC. Respiratory muscle endurance is limited by lower ventilatory efficiency in post-myocardial infarction patients. Braz J Phys Ther. 2014;18(1):1-8. doi: 10.1590/S1413-35552012005000134
» https://doi.org/10.1590/S1413-35552012005000134 -
5Woszezenki CT, Heinzmann-Filho JP, Vendrusculo FM, Piva TC, Levices I, Donadio MVF. Reference values for inspiratory muscle endurance in healthy children and adolescents. PLoS ONE. 2017;12(1):1-12. doi: 10.1371/journal.pone.0170696
» https://doi.org/10.1371/journal.pone.0170696 -
6Sturdya GA, Hillman DR, Green DJ, Jenkinsc SC, Cecins NM, Eastwood PR. The effect of learning on ventilatory responses to inspiratory threshold loading in COPD. Respir Med. 2004;98(1):1-8. doi: 10.1016/j.rmed.2003.07.005
» https://doi.org/10.1016/j.rmed.2003.07.005 -
7Gosselink R, Wagenaar RC, Decramer M. Reliability of a commercially available threshold loading device in healthy subjects and in patients with chronic obstructive pulmonary disease. Thorax. 1996;51(6):601-5.
-
8Belman MJ, Thomas SG, Lewis MI. Resistive breathing training in patients with chronic obstructive pulmonary disease. Chest. 1986;90(5):662-9. doi: 10.1378/chest.90.5.662
» https://doi.org/10.1378/chest.90.5.662 -
9Johnson PH, Cowley AJ, Kinnear WJM. Evaluation of the Threshold(r) trainer for inspiratory muscle endurance training: comparison with the weighted plunger method. Eur Respir J. 1996;9(12):2681-4. doi: 10.1183/09031936.96.09122681
» https://doi.org/10.1183/09031936.96.09122681 -
10Alves LA, Brunetto AF. Adaptação do Threshold(r) IMT para teste de resistência dos músculos inspiratórios. Rev Bras Fisioter. 2006;10(1):105-12. doi: 10.1590/S1413-35552006000100014
» https://doi.org/10.1590/S1413-35552006000100014 -
11Langer D, Jacome C, Charusin N, Scheer H, McConnel A, Decramer M, et al. Measurement validity of an electronic inspiratory loading device during a loaded breathing task in patients with COPD. Respir Med. 2013;107(4):633-5. doi: 10.1016/j.rmed.2013.01.020
» https://doi.org/10.1016/j.rmed.2013.01.020 -
12Coury HJCG, Vilella I. Profile of the Brazilian physical therapy researcher. Braz J Phys Ther. 2009;13(4):356-63. doi: 10.1590/S1413-35552009005000048
» https://doi.org/10.1590/S1413-35552009005000048 -
13Costa D. Ten years of stricto sensu postgraduate programs in physical therapy in Brazil: what has changed? Braz J Phys Ther. 2007;11(1):1-2. doi: 10.1590/S1413-35552007000100001
» https://doi.org/10.1590/S1413-35552007000100001 -
14Green M, Road J, Sieck GC, Similowski C. Tests of respiratory muscle strenght. Am J Respir Crit Care Med. 2002;166(4):528-47. doi: 10.1164/rccm.166.4.518
» https://doi.org/10.1164/rccm.166.4.518 -
15Montemezzo D, Velloso M, Britto RR, Parreira VF. Pressões respiratórias máximas: equipamentos e procedimentos usados por fisioterapeutas brasileiros. Fisioter Pesq. 2010;17(2):147-52. doi: 10.1590/S1809-29502010000200010
» https://doi.org/10.1590/S1809-29502010000200010 -
16Charususin N, Gosselink R, Decramer M, McConnell A, Saey D, Maltais F, et al. Inspiratory muscle training protocol for patients with chronic obstructive pulmonary disease (IMTCO study): a multicentre randomised controlled trial. BMJ Open. 2013;3(8):1-7. doi: 10.1136/bmjopen-2013-003101
» https://doi.org/10.1136/bmjopen-2013-003101 -
17Lötters F, van Tol B, Kwakkel G, Gosselink R. Effects of controlled inspiratory muscle training in patients with COPD: a meta-analysis. Eur Respir. 2002;20(3):570-6. doi: 10.1183/09031936.02.00237402
» https://doi.org/10.1183/09031936.02.00237402 -
18Hill K, Jenkins SC, Philippe DL, Shepherd KL, Hillman DR, Eastwood PR. Comparison of incremental and constant load tests of inspiratory muscle endurance in COPD. Eur Respir J. 2007;30(3):479-86. doi: 10.1183/09031936.00095406
» https://doi.org/10.1183/09031936.00095406 -
19Johnson PH, Cowley AJ, Kinnear WJM. Incremental threshold loading: a standard protocol and establishment of a reference range in naïve normal subjects. Eur Respir J. 1997;10(12):2868-71. doi: 10.1183/09031936.97.10122868
» https://doi.org/10.1183/09031936.97.10122868 -
20Gibson GJ. Measurement of respiratory muscle strength. Respir Med. 1995;89(8):529-35. doi: 10.1016/0954-6111(95)90153-1
» https://doi.org/10.1016/0954-6111(95)90153-1 -
21Koulouris N, Mulvey DA, Laroche CM, Green M, Moxham J. Comparison of two different mouthpieces for the measurement of PImax and PEmax in normal and weak subjects. Eur Respir J. 1988;1(9):863-7.
-
22Rubinstein I, Slutsky AS, Rebuck AS, McClean PA, Boucher R, Szeinberg A, et al. Assessment of maximal expiratory pressure in healthy adults. J Appl Physiol. 1988;64(5):2215-9. doi: 10.1152/jappl.1988.64.5.2215
» https://doi.org/10.1152/jappl.1988.64.5.2215 -
23Montemezzo D, Vieira DS, Tierra-Criollo CJ, Britto RR, Velloso M, Parreira VF. Influence of 4 interfaces in the assessment of maximal respiratory pressures. Respir Care. 2012;57(3):392-8. doi: 10.4187/respcare.01078
» https://doi.org/10.4187/respcare.01078 -
24Martyn JB, Moreno RH, Paré PD, Pardy RL. Measurement of inspiratory muscle performance with incremental threshold loading. Am Respir Dis. 1987;135(4):919-23.
-
25Dall'Ago P, Chiappa GR, Guths H, Stein R, Ribeiro JP. Inspiratory muscle training in patients with heart failure and inspiratory muscle weakness: a randomized trial. J Am Coll Cardiol. 2006;47(4):757-63. doi: 10.1016/j.jacc.2005.09.052
» https://doi.org/10.1016/j.jacc.2005.09.052 -
26Souza RB. Pressões respiratórias estáticas máximas. J Pneumol. 2002;28(Supl 3):S155-65.
-
27Pessoa IMBS, Neto MH, Montemezzo D, Silva LAM, Andrade AM, Parreira VF. Predictive equations for respiratory muscle strength according to international and Brazilian guidelines. Braz J Phys Ther. 2014;18(5):410-8. doi: 10.1590/bjpt-rbf.2014.0044
» https://doi.org/10.1590/bjpt-rbf.2014.0044 -
28Hart N, Hawkins P, Hamnegård CH, Green M, Moxham J, Polkey MI. A novel clinical test of respiratory muscle endurance. Eur Respir J. 2002;19(2):232-239. doi: 10.1183/09031936.02.00247602
» https://doi.org/10.1183/09031936.02.00247602 -
29Bonnevie T, Villiot-Danger JC, Gravier FE, Dupuis J, Prieur G, Médrinal C. Inspiratory muscle training is used in some intensive care units, but many training methods have uncertain efficacy: a survey of French physiotherapists. J Physiother. 2015;61(4):204-9. doi: 10.1016/j.jphys.2015.08.003
» https://doi.org/10.1016/j.jphys.2015.08.003 -
30Carling C. International questionnaire postal response rate: an experiment comparing no return postage to provision of International Postage Vouchers - "Coupon-Réponse International". BMC Health Serv Res. 2004;4:16[3 p.]. doi: 10.1186/1472-6963-4-16
» https://doi.org/10.1186/1472-6963-4-16 -
31Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2009;3: MR000008 [527 p.]. doi: 10.1002/14651858.MR000008.pub4
» https://doi.org/10.1002/14651858.MR000008.pub4
-
Study developed in the Laboratory of Assessment and Research in Cardiorespiratory Performance of the Department of Physical Therapy, of the School of Physical Education, Physical Therapy and Occupational Therapy at Universidade Federal de Minas Gerais (UFMG) - Belo Horizonte (MG), Brazil.
-
Finance source: Fundação de Amparo à Pesquisa do Estado de Minas Gerais (Fapemig), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Capes), and Pró-Reitoria de Pesquisa da Universidade Federal de Minas Gerais
-
Approved by the Research Ethics Committee at Universidade Federal de Minas Gerais (COEP-UFMG) under the protocol number CAAE: 21864913.7.0000.5149.
Publication Dates
-
Publication in this collection
Jul-Sep 2018
History
-
Received
13 Aug 2017 -
Accepted
09 Feb 2018