Abstract
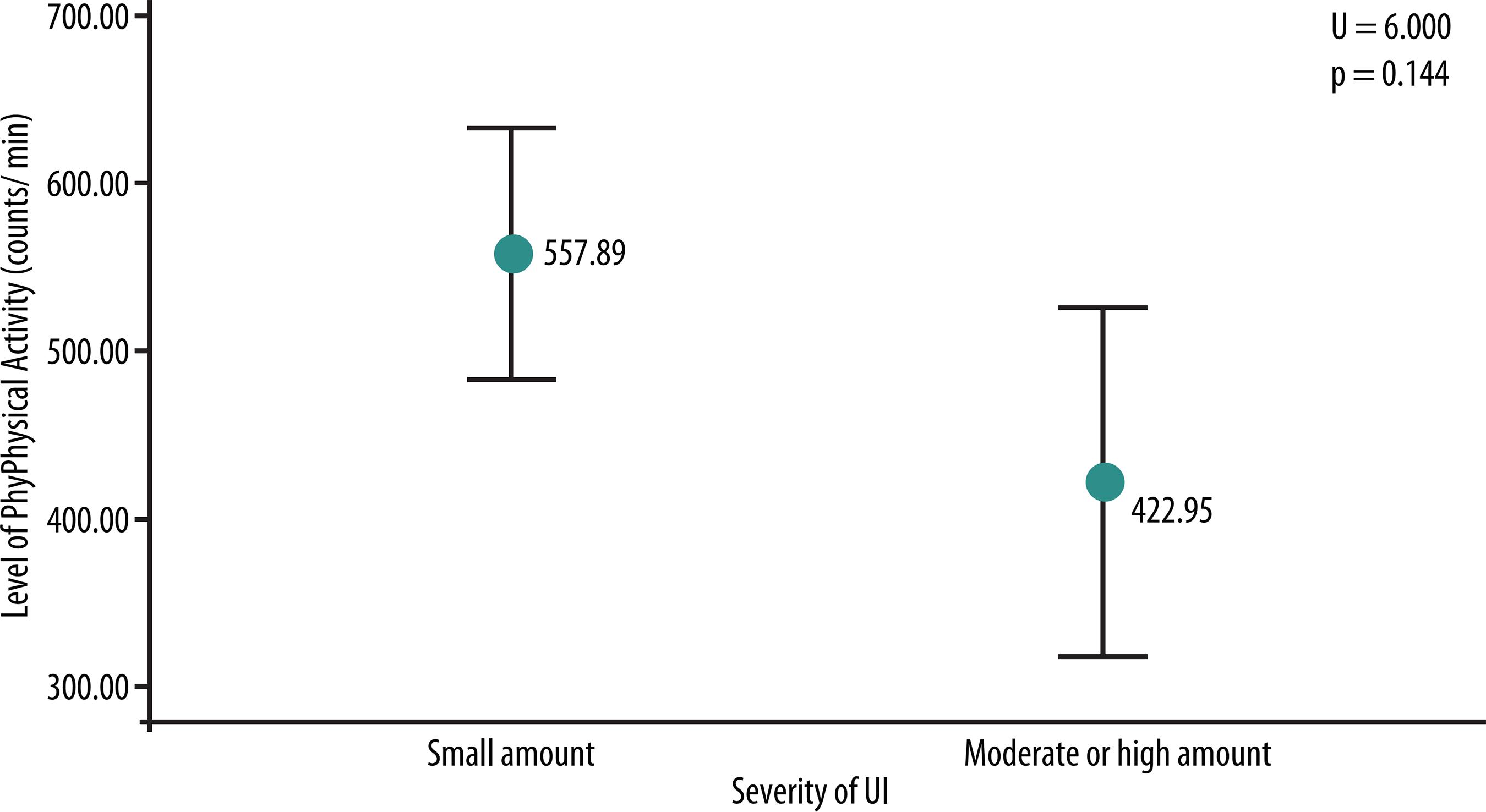
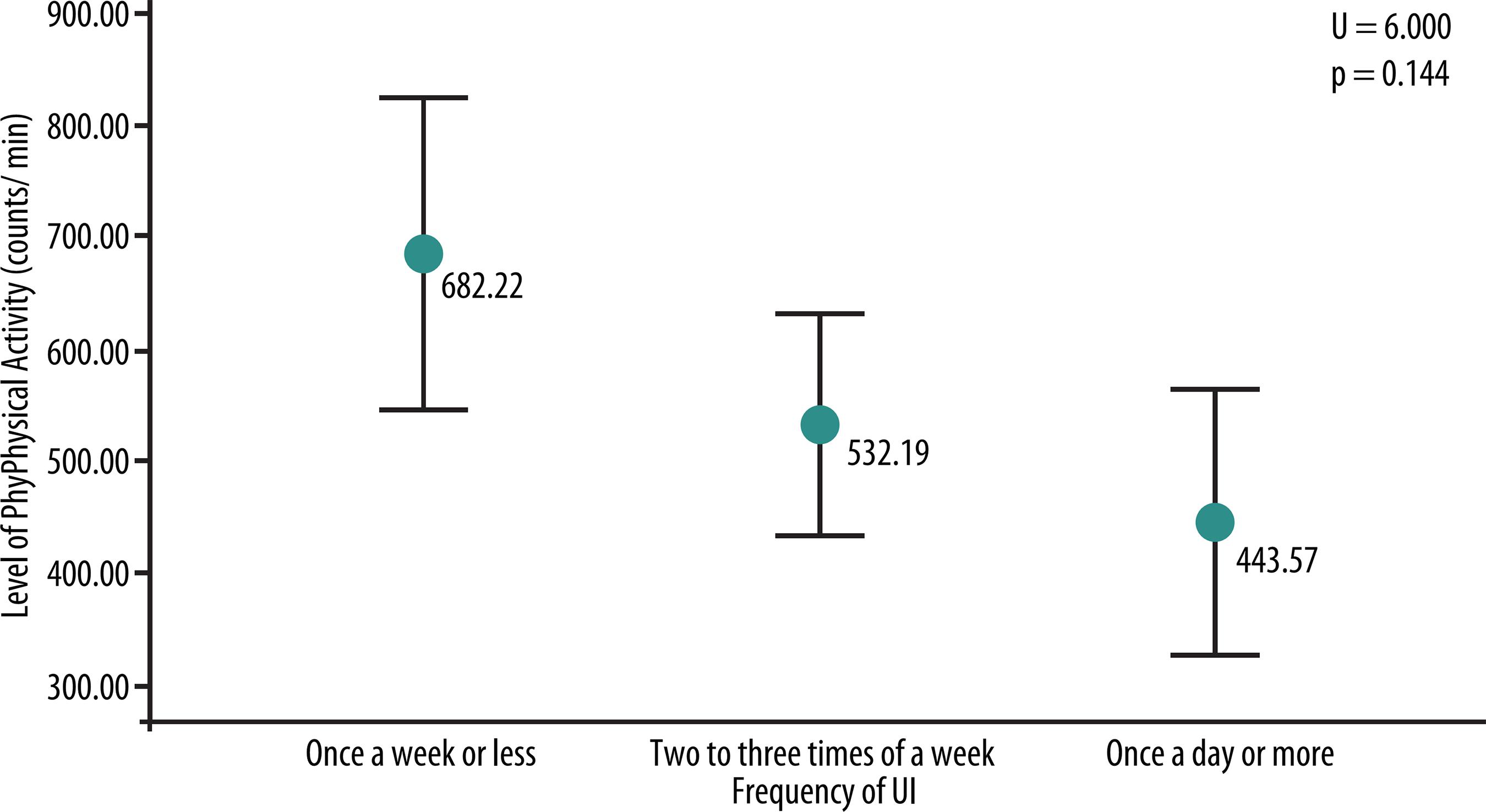
Urinary Incontinence (UI) is defined as any involuntary urinary loss. The relationship between physical activity and UI is undefined and bidirectional, where UI can cause physical inactivity and vice versa. The aim of this study was to verify and compare the level of physical activity with frequency and severity of urinary incontinence in older women. The study included 19 older women with stress or mixed UI. Data on the frequency and severity of UI were collected through the ICIQ-SF and the level of physical activity through triaxial accelerometer GT3-X brand ActiGrafh, used for seven consecutive days. Descriptive (mean, standard deviation, frequency and percentage) and inferential statistics (Mann-Whitney or way ANOVA with Bonferroni post hoc) was used. The majority of patients (n = 17; 89.5%) reported losing a small amount of urine. There was no difference between level of habitual physical activity and severity of UI (U = 6.000, p = 0.144). Regarding the frequency of urinary loss, 42.1% (n = 8) reported losing urine two or three times a week, 31.6% (n = 6) once a day or more and 26.3% (n = 5) once a week or less. Patients with more frequent urinary losses had lower levels of physical activity (F = 6.050; p = 0.011). In relation to the effect size, 43.1% of the variability of levels of PA can be explained by the frequency of urinary loss. It was concluded that the frequency of daily urinary loss is related to low levels of physical activity in older women.
Key words:
Accelerometer; Physical activity; Elderly; Urinary incontinence
Resumo
O objetivo do estudo foi verificar e comparar o nível de AF habitual com a frequ- ência e a gravidade da perda urinária em idosas. Participaram deste estudo, 19 idosas com IU de esforço ou mista. Foram coletados dados referentes à frequência e gravidade da IU por meio do ICIQ-SF e sobre o nível de AF habitual por meio do acelerômetro triaxial GT3-X marca ActiGrafh, utilizado durante sete dias consecutivos. Utilizou-se estatística descritiva (média, desvio padrão, frequência e porcentagem) e inferencial (U de Mann-Whitney ou ANOVA unifatorial com post hoc de Bonferroni). A maioria (n=17; 89,5%) relatou perder uma pequena quantidade de urina. Não houve diferença entre o nível de AF habitual e a gravidade da IU (U=6,000; p=0,144). Em relação à frequência das perdas urinárias, 42,1% (n= 8) relataram perder urina duas ou três vezes por semana, 31,6% (n= 6) uma vez ao dia ou mais e 26,3% (n= 5) uma vez por semana ou menos. As idosas com perdas urinárias mais frequentes apresentaram menor nível de AF habitual (F=6,050; p=0,011). Conforme o tamanho do efeito, 43,1% da variabilidade do nível de AF pode ser explicada pela frequência das perdas urinárias. Foi concluído que a frequência de perda urinária cotidianamente está relacionada com baixo nível de AF habitual de idosas.
Palavras-chave:
Acelerometria; Atividade física; Idoso; Incontinência urinária
INTRODUCTION
With the aging process, some changes occur in the female pelvic floor, especially reduced capacity of contracting the muscles of the perineal region11 Grewar H, McLean L. The integrated continence system: A manual therapy approach to the treatment of stress urinary incontinence. Man Ther 2008;13(5):375-86.. These changes contribute to the prevalence of urinary incontinence (UI), which affects approximately 30% of the elderly population of several countries such as United States22 Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter KL, et al. Prevalence and Trends of Symptomatic Pelvic Floor Disorders in US Women. Obstet Gynecol 2014;123(1):141-8., Spain33 Espunã-Pons M, Guiteras PB, Sampere DC, Bustos AM, Penina AM. Prevalência de incontinência urinaria en Cataluña. Med Clin 2009;133(18):702-5. Norway44 Ebbesen MH, Hunskaar S, Rortveit G, Hannestad YS. Prevalence, incidence and remission of urinary incontinence in women: longitudinal data from the Norwegian HUNT study (EPINCONT). BMC Urology 2013;13(27)1-10. and Brazil55 Tamanini JTN, Lebrão ML, Duarte YAO, Santos JLF, Laurenti R. Analysis of the prevalence of and factors associated with urinary incontinence among elderly people in the Municipality of São Paulo, Brazil: SABE Study (Health, Wellbeing and Aging). Cad Saúde Pública 2009;25(8):1756-62..
In addition, the prevalence of physical inactivity also increases with age66 Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Vigitel Brasil 2013: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico / Ministério da Saúde, Secretaria de Vigilância em Saúde. Brasília: Ministério da Saúde, 2014. 120p., affecting 46.5% of the elderly population worldwide77 Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380(9838):247-57., being considered one of the major public health problems of modern society88 Gualano B, Tinucci T. Sedentarismo, exercício físico e doenças crônicas. Rev Bras Educ Fís Esporte. 2011;25:37-43.. Thus, this study highlights the importance of investigating the level of physical activity in older women with urinary incontinence.
Studies that relate UI and the practice of physical activity (PA) or physical exercises indicate that impact activities such as gymnastics and ballet may increase the prevalence of the disease99 Thyssen HH, Clevin L, Olesen S, Lose G. Urinary Incontinence in Elite Female Athletes and Dancers. Int Urogynecol J Pelvic Floor Dysfunct 2002;13(1):15-7. and damage the pelvic floor structures1010 Jiang K, Novi JM, Darnell S, Arya LA. Exercise and urinary incontinence in women. Obstet Gynecol Surv 2004;59(10):717-21.. Other studies claim that the practice of moderate physical activity can minimize the reduction in the strength of pelvic floor muscles1111 Virtuoso JF, Mazo GZ, Menezes, EC. Urinary incontinence and perineal muscle function in physically active and sedentary elderly women. Rev Bras Fisioter 2011;15(4):310-7. or even reduce the occurrence of UI with increasing age1212 Devore EE, Minassian VA, Grodstein F. Factors associated with persistent urinary incontinence. Am J Obstet Gynecol 2013;209(2):145e1-6..
Thus, it was observed that the level of scientific evidence on the influence of physical activity on urinary incontinence is still undefined and bidirectional1313 Nygaard I, Shaw J, Egger MJ. Exploring the association between lifetime physical activity and pelvic floor disorders: study and design challenges. Contemp Clin Trials 2012;33(4):819-27., as it may be a risk factor (OR = 1.37; CI 95% = 1.09-0.71)1515 Nygaard IE, Shaw JM, Bardsley T, Egger MJ. Lifetime physical activity and female stress urinary incontinence. Am J Obstet Gynecol 2015;212:1.e1-1.e10. or a protection factor for urinary incontinence (OR = 0.62; CI 95% = 0.44-0.89)1414 Morrisroe SN, Rodriguez LV, Wang PC, Smith AL, Trejo L, Sarkisian CA. Correlates of 1-year Incidence of Urinary Incontinence in Latino Seniors Enrolled in a Community-Based Physical Activity Trial. J Am Geriatr Soc 2014;62(4):740-6.. Moreover, according to the theoretical model proposed by Nygaard et al.1313 Nygaard I, Shaw J, Egger MJ. Exploring the association between lifetime physical activity and pelvic floor disorders: study and design challenges. Contemp Clin Trials 2012;33(4):819-27., the fact that the influence of physical activity on UI and vice versa is controversial is also due to the use of different public targets with distinct risk factors and levels of physical activity. Kikuchi et al.1616 Kikuchi A, Niu K, Ikeda Y, Hozawa A, Nakagawa H, Guo H, et al. Association between physical activity and urinary incontinence in a community-based elderly population aged 70 years and over. Eur Urol 2007;52(3):868-74. used subjective measures and found that high levels of PA had a protective factor for UI in older Japanese women (OR = 0.37; CI 95% = 0.18-0.71).
Furthermore, the increase in the frequency and severity of urinary incontinence can result in social isolation1717 Elbiss HM, Osman N, Hammad FT. Social impact and healthcare-seeking behavior among women with urinary incontinence in the United Arab Emirates. Int J Gynaecol Obstet 2013;122(2):136-9., contributing to the belief that UI is a barrier to the practice of physical activity1818 NygaardI, Girts T, Fultz NH, Kinchen K, Pohl G, Sternfeld B. Is Urinary Incontinence a Barrier to Exercise in Women? Obstet Gynecol 2005;106(2):307-14.. In addition, some studies1616 Kikuchi A, Niu K, Ikeda Y, Hozawa A, Nakagawa H, Guo H, et al. Association between physical activity and urinary incontinence in a community-based elderly population aged 70 years and over. Eur Urol 2007;52(3):868-74.,1919 Lee AH, Hirayama F. Physical Activity and Urinary Incontinence in Older Adults: A Community-Based Study. Curr Aging Sci 2012;5(1):35-40. have investigated the relationship of UI and physical activity during leisure time, stressing the need for research using objective measures for habitual physical activity. Therefore, it is clear that UI is associated with low levels of physical activity in older women, which can lead to public health impacts.
Thus, the hypothesis of this study is that the frequency and severity of UI are related to the level of physical activity in older women. Therefore, the aim of this study was to verify and compare the level of physical activity with the frequency and severity of urinary incontinence in older women.
METHODOLOGICAL PROCEDURES
Study type and sample
This study is characterized as applied research since it aims at acquiring new knowledge aimed at application in a particular situation and has descriptive cross-section design, as it intends to describe the characteristics of a certain population and identify possible relationships between variables2020 Gil AC. Como elaborar projetos de pesquisa. 5ª ed. São Paulo: Atlas; 2010..
Study participants were intentionally and voluntarily recruited. Inclusion criteria were: being female, because urinary incontinence presents risk factors and is more prevalent in females22 Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter KL, et al. Prevalence and Trends of Symptomatic Pelvic Floor Disorders in US Women. Obstet Gynecol 2014;123(1):141-8.
3 Espunã-Pons M, Guiteras PB, Sampere DC, Bustos AM, Penina AM. Prevalência de incontinência urinaria en Cataluña. Med Clin 2009;133(18):702-5.-44 Ebbesen MH, Hunskaar S, Rortveit G, Hannestad YS. Prevalence, incidence and remission of urinary incontinence in women: longitudinal data from the Norwegian HUNT study (EPINCONT). BMC Urology 2013;13(27)1-10., being 60 years or older, due to the higher prevalence of this disease with increasing age44 Ebbesen MH, Hunskaar S, Rortveit G, Hannestad YS. Prevalence, incidence and remission of urinary incontinence in women: longitudinal data from the Norwegian HUNT study (EPINCONT). BMC Urology 2013;13(27)1-10.,1212 Devore EE, Minassian VA, Grodstein F. Factors associated with persistent urinary incontinence. Am J Obstet Gynecol 2013;209(2):145e1-6. and physical inactivity66 Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Vigitel Brasil 2013: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico / Ministério da Saúde, Secretaria de Vigilância em Saúde. Brasília: Ministério da Saúde, 2014. 120p.,77 Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380(9838):247-57.; presence of stress or mixed urinary incontinence; frequency of urinary incontinence of at least once a month; and living in the region of Florianópolis, SC. Those showing only urge urinary incontinence were excluded. Participants were invited to participate in the study by television and printed media.
Thus, 19 older women with stress or mixed urinary incontinence with frequency of urinary loss of at least once a month and who live in the region of Florianópolis, SC participated in this study.
Ethical aspects
The ethical principles of Resolution 196 of the National Health Council have been complied with and this study was approved by the Ethics Committee of Research with Human Beings of the State University of Santa Catarina under No. 498.443.
Instruments and data collection
To characterize study participants, questions related to sociodemographic data (age, marital status, educational level and current situation) were applied in the form of interview in a closed room on the premises of the University. To check the presence of urinary incontinence (UI), which is defined as “complaint of any involuntary urinary loss”, according to the International Society of Continence2121 Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the Standardisation sub -committee of the International continence society. Urology 2003;61(1):37-49., the following question was made: “During the last year, did you lose urine (unintentionally, in panties) at least once a month?2222 Huang AJ, Brown JS, Thom DH, Fink HA, Yaffe K. Urinary incontinence in older community-dwelling women: the role of cognitive and physical function decline. Obstet Gynecol 2007;109(4):909-16.. If so, the presence of UI symptoms has been identified and interview was held to verify type, frequency and severity of urinary loss.
The type of UI was identified through the following questions: a) Do you lose urine when you cough, sneeze or carry weight? b) Do you lose urine before reaching the toilet after feeling strong urge to urinate or without perceiving it? To an affirmative answer to question “a” stress UI was considered and to question “b” urge UI. Mixed urinary incontinence was characterized in case of affirmative answer to both questions2222 Huang AJ, Brown JS, Thom DH, Fink HA, Yaffe K. Urinary incontinence in older community-dwelling women: the role of cognitive and physical function decline. Obstet Gynecol 2007;109(4):909-16..
To check the frequency and severity of urinary loss, the International Consultation on Incontinence Questionnaire - Short Form (ICIQ-SF) was applied. This questionnaire consists of six questions for evaluating the impact of urinary incontinence on quality of life, detect some everyday situations that cause losses and quantify the frequency and severity of UI2323 Avery K, Donovan J, Abrams P. Validation of a new questionnaire for incontinence: the International Consultation on Incontinence Questionnaire (ICIQ). Abstract nº 86 of the International Continence Society 31st annual meeting. Seoul, Korea. Neurourol Urodynamics 2001;20:510-1.,2424 Tamanini JTN, Dambros M, D'Ancona CAL, Palma PCR, Netto Jr NR. Validação para o português do "Internationa lConsultationon Incontinence Questionnaire - Short Form" (ICIQ-SF). Rev Saúde Pública 2004;38(3):438-44.. This questionnaire was originally developed and validated in English2323 Avery K, Donovan J, Abrams P. Validation of a new questionnaire for incontinence: the International Consultation on Incontinence Questionnaire (ICIQ). Abstract nº 86 of the International Continence Society 31st annual meeting. Seoul, Korea. Neurourol Urodynamics 2001;20:510-1. and validated to Portuguese2424 Tamanini JTN, Dambros M, D'Ancona CAL, Palma PCR, Netto Jr NR. Validação para o português do "Internationa lConsultationon Incontinence Questionnaire - Short Form" (ICIQ-SF). Rev Saúde Pública 2004;38(3):438-44., with reliability greater than or equal to 0.72 in all questions. The severity of UI was categorized into two levels: small, moderate or large amount. The frequency of urinary loss was categorized into three levels: once or less per week; two or three times per week; once a day or more.
The level of habitual physical activity of participants was measured by GT3-X triaxial accelerometer brand ActiGrafh. Older women used the device on the right hip, positioned near the iliac crest over a period of seven consecutive days. Also, the accelerometer was provided along with a folder with instructions for use and the researchers' phone numbers to contact them with any questions. For quality control, two phone calls were performed (second and fifth day of use) to verify if participants were using the device properly and to make sure the device was working well. Data were recorded with one-second epochs. For data analysis, the use of the equipment for at least 600 minutes (10 hours) was considered a valid day2525 Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical Activity in the United States Measured by Accelerometer. Med Sci Sports Exerc 2008;40(1):181-8.,2626 Matthews CE, Hagströmer M, Pober DM, Bowles HR. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. 2012; 44(1 Suppl 1): S68-S76..
In addition to the nonwear period to sleep and to perform water activities, periods of at least 60 consecutive minutes of zero counts were also considered as nonwear time. To characterize sedentary behavior, cutoff of <100 counts per minute was adopted 2727 Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of Time Spent in Sedentary Behaviors in the United States, 2003-2004. Am J Epidemiol 2008;167(7):875-81.. This study included the results of participants with at least five valid days from use of the equipment, one day during the weekend2525 Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical Activity in the United States Measured by Accelerometer. Med Sci Sports Exerc 2008;40(1):181-8..
To start, download and filtering of data, ActiLife software version 6.11.4 was used. The counts per minute of the magnitude vector were considered as the result of the level of physical activity.
Statistical Analysis
Data were stored and analyzed in Statistical Package for Social Sciences (SPSS) version 20.0. All categorical variables were descriptively analyzed through simple frequency and percentages and numeric variables through position and dispersion measures. The normal distribution of data was verified by the Shapiro-Wilk test.
In the inferential analysis, the Mann-Whitney U test was used to compare the level of physical activity and severity of UI. To compare the level of physical activity with the frequency of UI, one-factor ANOVA with post hoc Bonferroni was used. The significance level adopted was 5%.
RESULTS
The average age of study participants (n = 19) was 69.32 ± 6.0 years. As for sociodemographic data, 36.8% (n = 7) had completed high school, 36.8% (n = 7) were married and 73.7% (n = 14) were retired. Regarding UI, according to the exclusion criteria, no patient presented urge UI, 15.8% (n = 3) reported stress UI and 84.2% (n = 16) had mixed UI. All older women reported to lose urine when coughing or sneezing, with stress UI and 15.8% (n = 3) also lose urine during physical activity, as shown in Table 1.
Regarding the frequency of urinary loss, 42.1% (n = 8) reported losing urine two or three times a week, 31.6% (n = 6) once a day or more and 26.3% (n = 5) once a week or less.
By analyzing the severity of UI, the majority (n = 17; 89.5%) reported losing a small amount of urine. There was no difference between level of habitual physical activity and severity of UI (U = 6.000, p = 0.144), as shown in Figure 1.
Figure 2 shows that older women with frequent urinary incontinence (once or more a day) had lower level of physical activity (F = 6.050; p = 0.011) when compared with those with lower frequency of urinary loss (once a week or less, two or three times a week). Post hoc Bonferroni test revealed that the level of physical activity is significantly smaller among women who lose urine once per day or more, compared with those who lose once a week or less (p = 0.010). Furthermore, according to the effect size, 43.1% of the variability of the level of physical activity can be explained by the frequency of urinary loss.
DISCUSSION
This study verified the relationship between frequency and severity of UI and level of physical activity in older women. It was observed that patients with urinary losses of once a day or more had low levels of physical activity. Although this study had a reduced number of participants and cross-sectional design, it does not allow establishing causality and uses an objective measure to assess the level of physical activity, minimizing measurement biases of this variable. Furthermore, it is believed that the need to understand in more detail the relationship of UI (frequency and severity) with levels of habitual PA (objective measure) justifies the intentional selection of the study participants.
Physical activity can be influenced by different factors, called individual, social or environmental determinants2828 Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJF, Martin BW. Correlates of physical activity: why are some people physically active and others not? Lancet 2012;380(9838):258-71.. This study showed that the frequency of urinary loss is an important factor, influencing by 43.1% the level of physical activity of older women. Nygaard et al.1818 NygaardI, Girts T, Fultz NH, Kinchen K, Pohl G, Sternfeld B. Is Urinary Incontinence a Barrier to Exercise in Women? Obstet Gynecol 2005;106(2):307-14. investigated how the severity of UI affects in practice and adherence to physical exercises by women (mean age 44.4 ± 9.8 years) and found that 27.9% of those who reported losing urine in the last 30 days considered UI as a barrier to this practice, compared with only 1.7% of those that lost urine for more than 30 days. Another important fact is that one out of 10 women does not exercise because of UI and 11.3% decreased the practice of exercises because of this disease1818 NygaardI, Girts T, Fultz NH, Kinchen K, Pohl G, Sternfeld B. Is Urinary Incontinence a Barrier to Exercise in Women? Obstet Gynecol 2005;106(2):307-14..
Similarly to the study of Nygaard et al.1818 NygaardI, Girts T, Fultz NH, Kinchen K, Pohl G, Sternfeld B. Is Urinary Incontinence a Barrier to Exercise in Women? Obstet Gynecol 2005;106(2):307-14., this study found that the daily frequency of urinary loss is a factor contributing to low levels of physical activity. The frequent episodes of urinary loss can impact the daily lives of women in the religious, social and sexual contexts and in and practice of PA1717 Elbiss HM, Osman N, Hammad FT. Social impact and healthcare-seeking behavior among women with urinary incontinence in the United Arab Emirates. Int J Gynaecol Obstet 2013;122(2):136-9., leading to decreased level of physical activity and physical inactivity.
It has been evidenced in literature that physical inactivity in the population is a public health problem 77 Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380(9838):247-57.,88 Gualano B, Tinucci T. Sedentarismo, exercício físico e doenças crônicas. Rev Bras Educ Fís Esporte. 2011;25:37-43.. Physical inactivity has a relative risk of 1.47 for all causes of death2929 Lee, IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380(9838):219-29.. It was observed that UI can impact the daily lives of older women, contributing to low levels of PA and may be an adjunct to a public health problem. Delarmelindo et al.3030 Delarmelindo RCA, Parada CMGL, Rodrigues RAP, Bocchi SCM. Estratégias Enaiane Cristina Menezes. de enfrentamento da incontinência urinária por mulheres. Ver Esc Enferm USP 2013;47(2):296-303. claim that UI is invisible and actions and public policies are often neglected in clinical evaluations and by patients themselves.
Another aspect related to UI is that regular physical activity helps to reduce body weight, which is an important risk factor in the genesis of UI1212 Devore EE, Minassian VA, Grodstein F. Factors associated with persistent urinary incontinence. Am J Obstet Gynecol 2013;209(2):145e1-6. and minimizes the decline in muscle strength, including pelvic floor muscles (PFM) in older women1111 Virtuoso JF, Mazo GZ, Menezes, EC. Urinary incontinence and perineal muscle function in physically active and sedentary elderly women. Rev Bras Fisioter 2011;15(4):310-7..
Lee and Hirayama1919 Lee AH, Hirayama F. Physical Activity and Urinary Incontinence in Older Adults: A Community-Based Study. Curr Aging Sci 2012;5(1):35-40. assessed the relationship of physical activity with UI and found that the practice of walking an average of 5 hours a week is a protective factor for UI (OR = 0:43; CI 95% = 0.20-0.96) and Kikuchi et al.1616 Kikuchi A, Niu K, Ikeda Y, Hozawa A, Nakagawa H, Guo H, et al. Association between physical activity and urinary incontinence in a community-based elderly population aged 70 years and over. Eur Urol 2007;52(3):868-74. analyzed the relationship of physical activity in the leisure domain with UI and found that moderate (OR = 0.63; CI 95% = 0.42-0.94) and high levels (OR = 0 43; CI 95% = 0.26-0.68) of physical activity are protective factors for UI.
The relationship between PA and the UI is still controversial, reflecting the need to understand the effects of physical activity in the long term1313 Nygaard I, Shaw J, Egger MJ. Exploring the association between lifetime physical activity and pelvic floor disorders: study and design challenges. Contemp Clin Trials 2012;33(4):819-27.. It is necessary to understand how the frequency of urinary incontinence can impact the level of PA so that health professionals have mechanisms to lower the barrier imposed by UI in the daily life of older women. In addition, this study contributes to scientific knowledge in the area, as it established the relationship of severity and frequency of UI with levels of habitual physical activity in older women using physical activity in all contexts and differentiating patients with urinary incontinence according to its severity.
CONCLUSION
This study found that older women with more frequent urinary incontinence had lower levels of physical activity, i.e., the frequency of urinary loss can be a factor that influences the low levels of physical activity in older women.
Physical activity, influenced by several factors (determinants), can also be influenced by the frequency of urinary loss possibly due to the impact that UI has on the daily life of these individuals. Thus, there is need for public policies and intervention studies to minimize interference of urinary incontinence on the level of physical activity of older women.
Future studies should investigate the causality and the influence of UI on the levels of physical activity and vice versa, especially in the long term. The influence of sedentary behavior on UI and its impact on the daily life of older women should be investigated, since often this disease is invisible for public policies.
REFERENCES
-
1Grewar H, McLean L. The integrated continence system: A manual therapy approach to the treatment of stress urinary incontinence. Man Ther 2008;13(5):375-86.
-
2Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter KL, et al. Prevalence and Trends of Symptomatic Pelvic Floor Disorders in US Women. Obstet Gynecol 2014;123(1):141-8.
-
3Espunã-Pons M, Guiteras PB, Sampere DC, Bustos AM, Penina AM. Prevalência de incontinência urinaria en Cataluña. Med Clin 2009;133(18):702-5.
-
4Ebbesen MH, Hunskaar S, Rortveit G, Hannestad YS. Prevalence, incidence and remission of urinary incontinence in women: longitudinal data from the Norwegian HUNT study (EPINCONT). BMC Urology 2013;13(27)1-10.
-
5Tamanini JTN, Lebrão ML, Duarte YAO, Santos JLF, Laurenti R. Analysis of the prevalence of and factors associated with urinary incontinence among elderly people in the Municipality of São Paulo, Brazil: SABE Study (Health, Wellbeing and Aging). Cad Saúde Pública 2009;25(8):1756-62.
-
6Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Vigitel Brasil 2013: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico / Ministério da Saúde, Secretaria de Vigilância em Saúde. Brasília: Ministério da Saúde, 2014. 120p.
-
7Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380(9838):247-57.
-
8Gualano B, Tinucci T. Sedentarismo, exercício físico e doenças crônicas. Rev Bras Educ Fís Esporte. 2011;25:37-43.
-
9Thyssen HH, Clevin L, Olesen S, Lose G. Urinary Incontinence in Elite Female Athletes and Dancers. Int Urogynecol J Pelvic Floor Dysfunct 2002;13(1):15-7.
-
10Jiang K, Novi JM, Darnell S, Arya LA. Exercise and urinary incontinence in women. Obstet Gynecol Surv 2004;59(10):717-21.
-
11Virtuoso JF, Mazo GZ, Menezes, EC. Urinary incontinence and perineal muscle function in physically active and sedentary elderly women. Rev Bras Fisioter 2011;15(4):310-7.
-
12Devore EE, Minassian VA, Grodstein F. Factors associated with persistent urinary incontinence. Am J Obstet Gynecol 2013;209(2):145e1-6.
-
13Nygaard I, Shaw J, Egger MJ. Exploring the association between lifetime physical activity and pelvic floor disorders: study and design challenges. Contemp Clin Trials 2012;33(4):819-27.
-
14Morrisroe SN, Rodriguez LV, Wang PC, Smith AL, Trejo L, Sarkisian CA. Correlates of 1-year Incidence of Urinary Incontinence in Latino Seniors Enrolled in a Community-Based Physical Activity Trial. J Am Geriatr Soc 2014;62(4):740-6.
-
15Nygaard IE, Shaw JM, Bardsley T, Egger MJ. Lifetime physical activity and female stress urinary incontinence. Am J Obstet Gynecol 2015;212:1.e1-1.e10.
-
16Kikuchi A, Niu K, Ikeda Y, Hozawa A, Nakagawa H, Guo H, et al. Association between physical activity and urinary incontinence in a community-based elderly population aged 70 years and over. Eur Urol 2007;52(3):868-74.
-
17Elbiss HM, Osman N, Hammad FT. Social impact and healthcare-seeking behavior among women with urinary incontinence in the United Arab Emirates. Int J Gynaecol Obstet 2013;122(2):136-9.
-
18NygaardI, Girts T, Fultz NH, Kinchen K, Pohl G, Sternfeld B. Is Urinary Incontinence a Barrier to Exercise in Women? Obstet Gynecol 2005;106(2):307-14.
-
19Lee AH, Hirayama F. Physical Activity and Urinary Incontinence in Older Adults: A Community-Based Study. Curr Aging Sci 2012;5(1):35-40.
-
20Gil AC. Como elaborar projetos de pesquisa. 5ª ed. São Paulo: Atlas; 2010.
-
21Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the Standardisation sub -committee of the International continence society. Urology 2003;61(1):37-49.
-
22Huang AJ, Brown JS, Thom DH, Fink HA, Yaffe K. Urinary incontinence in older community-dwelling women: the role of cognitive and physical function decline. Obstet Gynecol 2007;109(4):909-16.
-
23Avery K, Donovan J, Abrams P. Validation of a new questionnaire for incontinence: the International Consultation on Incontinence Questionnaire (ICIQ). Abstract nº 86 of the International Continence Society 31st annual meeting. Seoul, Korea. Neurourol Urodynamics 2001;20:510-1.
-
24Tamanini JTN, Dambros M, D'Ancona CAL, Palma PCR, Netto Jr NR. Validação para o português do "Internationa lConsultationon Incontinence Questionnaire - Short Form" (ICIQ-SF). Rev Saúde Pública 2004;38(3):438-44.
-
25Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical Activity in the United States Measured by Accelerometer. Med Sci Sports Exerc 2008;40(1):181-8.
-
26Matthews CE, Hagströmer M, Pober DM, Bowles HR. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. 2012; 44(1 Suppl 1): S68-S76.
-
27Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of Time Spent in Sedentary Behaviors in the United States, 2003-2004. Am J Epidemiol 2008;167(7):875-81.
-
28Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJF, Martin BW. Correlates of physical activity: why are some people physically active and others not? Lancet 2012;380(9838):258-71.
-
29Lee, IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380(9838):219-29.
-
30Delarmelindo RCA, Parada CMGL, Rodrigues RAP, Bocchi SCM. Estratégias Enaiane Cristina Menezes. de enfrentamento da incontinência urinária por mulheres. Ver Esc Enferm USP 2013;47(2):296-303.
Publication Dates
-
Publication in this collection
Sep-Oct 2015
History
-
Received
25 May 2015 -
Accepted
19 July 2015