Abstracts
Objective:
to evaluate the correlation between the auscultation test and X-ray when detecting the position of an enteral feeding tube.
Methods:
cross-sectional study in an intensive care unit in southern Brazil, in 2011. Clinical nurse and nurse researcher performed auscultation test recording the impressions regarding the placement of an enteral feeding tube in 80 patients. A doctor evaluated the X-ray. Kappa coefficient and PABAK reviewed the agreements.
Results:
The X-ray showed that 70% of the enteral tubes were in the stomach, 27.4% in the duodenum, 1.3% in the esophagus, and 1.3% in the right lung. There was a weak correlation between clinical nurses and nurse researchers (PABAK = 0.054; P = 0.103), clinical nurses and X-rays (PABAK = 0.188; P = 0.111) and nurse researchers and X-rays (PABAK = 0.128; P = 0.107) . The auscultation test did not detect two risk conditions, enteral feeding tube in the esophagus and the bronchus.
Conclusion:
the auscultation test showed little agreement with the X-ray on the enteral feeding tube location.
Auscultation; Gastrointestinal intubation; Nursing
Objetivo:
evaluar la concordancia entre test de ausculta y Rayo-X en la detección del posicionamiento de la sonda enteral.
Métodos:
estudio transversal en un Centro de Terapia Intensiva del sur de Brasil (2011). Enfermero asistencial y enfermero investigadora realizaron teste de ausculta y registraron sus impresiones en 80 pacientes. Una médica evaluó el Rayo-X. Coeficiente Kappa y PABAK evaluaron las concordancias.
Resultados:
Rayo-X mostro 70% de las sondas enterales en el estómago, 27,6% en el duodeno, 1,3% en el esófago y 1,3% en el pulmón derecho. Hubo débil concordancia entre enfermero asistencial y enfermero investigadora (PABAK =0,054; P=0,103), enfermero asistencial y Rayo-X (PABAK=0,188; P=0,111) y enfermero investigador y Rayo-X (PABAK =0,128; P=0,107). El teste de ausculta no ha detectado dos condiciones de riesgo, sonda enteral en el esófago y en el bronquio.
Conclusión:
teste de ausculta se ha mostrado poco concordante con el Rayo-X en la posición de la sonda enteral.
Auscultación; Intubación gastrointestinal; Enfermería
Objetivo:
Avaliar a concordância entre o teste de ausculta e o raio-X na detecção do posicionamento da sonda enteral.
Métodos:
Estudo transversal realizado
em um Centro de Terapia Intensiva do sul do Brasil, em 2011. Enfermeira assistencial e enfermeira pesquisadora realizaram teste de ausculta registrando suas impressões quanto ao posicionamento da sonda enteral em 80 pacientes. Uma médica avaliou o raio-X. Coeficiente Kappa e PABAK avaliaram as concordâncias.
Resultados:
O raio-X mostrou 70% das sondas enterais no estômago, 27,4% no duodeno, 1,3% no esôfago e 1,3% no pulmão direito. Houve fraca concordância entre enfermeira assistencial e enfermeira pesquisadora (PABAK =0,054; P=0,103), enfermeira assistencial e raio-X (PABAK=0,188; P=0,111) e enfermeira pesquisadora e raio-X (PABAK =0,128; P=0,107). O teste de ausculta não detectou duas condições de risco, sonda enteral no esôfago e no brônquio.
Conclusão:
O teste de ausculta mostrou-se pouco concordante com o raio-X na localização da sonda enteral.
Auscultação; Intubação gastrointestinal; Enfermagem
INTRODUCTION
The enteral feeding tube (FT) is the device used to provide calories to patients who are totally or partially unable to orally digest them(11. Kattelmann K, Hise M, Russell M, Charney P, Stokes M, Compher C. Preliminary evidence for a medical nutrition therapy protocol: enteral feedings for critically ill patients. J Am Diet Assoc. 2006;106:1226-41.). The insertion of the feeding tube is not a complication free procedure. Despite the frequency in which they occur, due to the potential damages, complications related to the poor positioning of the distal tip of the FT, with consequent diet administration to the respiratory tract, are those that represent the greatest risk(22. Agha R, Siddiqui MRS. Pneumotorax after nasogastric tube insertion. JRSM Rep. 2011;2(4):28.
3. Takwoingi YM. Inadvertent insertion of a nasogastric tube into both main bronchi of an awake patient: a case report. Cases J. 2009;2:6914.-44. Stayner JL, Bhatnagar A, McGinn AN, Fang JC. Feeding tube placement: errors and complications. Nutr Clin Pract. 2012;27(6):738-48.).
In critically ill patients who are frequent users of these devices, even greater attention should be given, as common factors such as the adoption of the supine position, presence of gastric residue, vomiting and mechanical ventilation use can contribute to the aspiration of gastric contents(55. Sparks DA, Chase DM, Coughlin LM, Perry E. Pulmonary complications of 9931 narrow-bore nasoenteric tubes during blind placement: a critical review. JPEN J Parenter Enteral Nutr. 2011;35(5):625-9.). The risk of aspiration also increases when the FT is positioned near the esophagogastric junction, stimulating gastroesophageal reflux, or when shifting occurs after coughing, nausea and vomiting(66. Malta MA, Carvalho-Junior AF, Andreollo NA, Freitas MIP. Medidas antropométricas na introdução da sonda nasogástrica para nutrição enteral empregando esofagogastroduodenoscopia. Arq Bras Cir Dig. 2013;26(2):107-11.).
There are only a few studies on the insertion technique and confirmation of the positioning of the FT(77. Leães MD, Mello E, Beghetto M, de Silva Assis MC. Enteral feeding tubes: are insertion techniques and positioning based on anatomical evidence? Nutr Health. 2012;21(3)193-200.). In practice, enteral feeding tube placement is described in different ways. Although the common recommendation is that the insertion be made blindly (i.e. without the nurse viewing the path that the FT travels) In these cases there is not, for example, a standard single FT length to be introduced in order for the distal tip reach the stomach(44. Stayner JL, Bhatnagar A, McGinn AN, Fang JC. Feeding tube placement: errors and complications. Nutr Clin Pract. 2012;27(6):738-48.,66. Malta MA, Carvalho-Junior AF, Andreollo NA, Freitas MIP. Medidas antropométricas na introdução da sonda nasogástrica para nutrição enteral empregando esofagogastroduodenoscopia. Arq Bras Cir Dig. 2013;26(2):107-11.
7. Leães MD, Mello E, Beghetto M, de Silva Assis MC. Enteral feeding tubes: are insertion techniques and positioning based on anatomical evidence? Nutr Health. 2012;21(3)193-200.-88. Chen YC, Wang LY, Chang YJ, Yang CP, Wu TJ, Lin FR, et al. Potential risk of malposition of nasogastric tube using nose-ear-xiphoid measurement. PLoS One. 2014;9(2):1-7.).
In an attempt to minimize complications related to improper placement of the FT after insertion and prior to diet administration, clinical bedside trials are adopted to estimate if the distal tip of the FT is, in fact, in the stomach or intestine. The auscultation test is the most used verification method among nurses in clinical practice(77. Leães MD, Mello E, Beghetto M, de Silva Assis MC. Enteral feeding tubes: are insertion techniques and positioning based on anatomical evidence? Nutr Health. 2012;21(3)193-200.). Another test used is pH measurement (hydrogen potential) of the waste sucked through the FT(99. Stock A, Gilbertson HR, Babi FE. Confirming nasogastric tube position in the emergency department: pH testing is reliable. Pediatr Emerg Care. 2008;24(12):805-9.-1010. Simons SR, Abdallah LM. Bedside assessment of enteral tube placement: aligning practice with evidence. AJN. 2012;112(2):40-6.). Isolated results of these tests, or their combination, supports the opinion given by the nurse regarding the anatomical location of the distal tip of the FT. However, there are no studies that document the validation and diagnostic accuracy of these tests to adequately predict the anatomical location of the distal tip of the FT. Thus, the X-ray diagnosis is still the reference method for this purpose(1010. Simons SR, Abdallah LM. Bedside assessment of enteral tube placement: aligning practice with evidence. AJN. 2012;112(2):40-6.).
Considering the large number of patients undergoing enteral survey procedures, and the potential damage related to diet and medication deposited out of the stomach or intestines, as well as small amount of literature on the reliability of the means adopted by nurses to establish the anatomical location of the FT, this study, derived from a thesis(1111. Leães DM. Avaliação do procedimento de inserção de sonda enteral [dissertação]. Porto Alegre (RS): Faculdade de Medicina, Universidade Federal do Rio Grande do Sul; 2012.), aimed to evaluate the correlation between the auscultation test and X-rays to detect the positioning of enteral feeding tube.
METHOD
This is a cross-sectional study conducted in the adult Intensive Care Unit (ICU) at a university teaching hospital in Porto Alegre / RS. Data collection took place in 2011.
Adults (≥ 18 years), of both sexes, with enteral feeding tube recomendations, were consecutively included. Patients undergoing head and neck surgery, diagnosed with esophageal and / or stomach cancer or other anatomical changes that could interfere with the insertion procedure of the FT.
After the attending physician prescribes the enteral feeding tube, the attending nurse (AN), following the standard institutional recommendation for the insertion, installed the FT, performed a bedside auscultation test, and issued an opinion, in writing, about the impression regarding the anatomical location of the FT, registered on own form provided. The nurse researcher (NR) accompanied all FT inserts. The insertions were carried out blindly, for purposes of the AN opinion, and the auscultation test was also performed, with the results being recorded in the independent form used by the AN. All patients were subjected, in sequence, to x-rays to confirm the location of the FT, since this test is the reference standard for identifying the position of the distal tip of the FT. Independently, without information about patients or knowing the impressions of the nurses, a doctor examined each x-ray, and recorded the anatomic location of the FT positioning in a specific form (reference standard). All patients used the same type of radiopaque FT, with a tungsten distal tip and 10 Fr steel guidewire (MEDICONER(r), Brazil).
In order to evaluate the correlation between the impressions of the nurses and the anatomical location of the FT, as evidenced by the X-rays, the Kappa coefficient and PABAK (Prevalence and Bias Adjusted Kappa) were measured.
The sample size calculation was based on data obtained in a study of corpses(1212. Hanson RL. Predictive criteria for length of nasogastric tube insertion for tube feeding. JPEN J Parenter Enteral Nutr. 1979;3(3):160-3.), which found that 72% of success in the FT insertions into gastric portion using the same standardized technique at the headquarters of the institution that carried out this study. To obtain the 0.8 Kappa with a confidence interval of 0.3, significance level of 5% and 80% power, the need to include 79 patients (158 observation pairs) was estimated. The final sample consisted of 80 patients.
The research received prior approval by the Ethics Committee of the institution (Protocol 100314/2010) regarding its ethical and methodological aspects. The Free and Informed Consent Form (FICF) was signed by assistant nurses who participated in the survey. The FICF was dismissed for patients due to the fact that no additional risks, beyond those associated with the enteral tube insertion procedure itself, (a procedure that occured regardless of this study) were expected. The consent for use of the data was signed by the researchers and the host institution of the study.
RESULTS
80 procedures were evaluated in 80 patients, whose age was 55.8 ± 18.1 years, being predominantly men (61.3%) in use of mechanical ventilation (61.3%).
The X-ray control showed that 70% (n = 56) of the distal tip FT were located in the stomach, 27.4% (n = 22) in the duodenum, 1.3% (n = 1) in the third portion of esophagus and 1.3% (n = 1) in the right lung. There was very weak correlation between the impression of a attending nurse and the location of the distal tip of the FT, as evidenced by X-ray (PABAK = 0.188; P = 0.111) between the nurse researcher impressions and the position of the FT confirmed by X-ray (PABAK = 0.128; P = 0.107) and between the impressions of the attending nurse and nurse researcher (PABAK = 0.054; P = 0.103), as shown in Chart 1.
- Agreement between the opinions expressed by observers: (a) Doctor (columns) vs. Attending Nurse (lines), (b) Doctor (columns) vs. Nurse Researcher (rows) and (c) Nurse Researcher (columns) vs. Attending Nurse (lines) and the anatomical location of the distal tip enteral feeding tube. Porto Alegre/RS, Brasil, 2011
In one of enteral insertions, based on bedside tests, AN stated that the location of the FT was unknown, a fact that did not occur with the nurse researcher. Both did not identified two high risk conditions for patients: FT insertion in the distal esophagus (n = 1) and the right bronchus (n = 1). While the nurse researcher identified a greater number of FT positioned in the stomach (n = 50), the attending nurse disagreed less about when the tip of the FT was located in the intestine (n = 10).
In order to identify whether the bedside test performed by nurses and repeated by the researcher was able to estimate the alimentary tract of the segment in which the distal tip of the FT was positioned, only the results that determined that the distal tip FT was in the stomach or intestine were analyzed, excluding the location in the esophagus, lung, or "do not know". The same low incidence of agreement between doctor and AN (Kappa = 0.215; P = 0.118), doctor and NR (Kappa = 0.142; P = 0.114) and between NR and AN (Kappa = 0.052; P = 0.107) (Chart 2) was identified.
- Agreement between the opinions expressed by observers: (a) Doctor (columns) vs. Attending Nurse (lines), (b) Doctor (columns) vs. Nurse Researcher (lines) and (c) Nurse Researcher (columns) vs. Attending Nurse (lines) regarding the anatomical location of the distal tip of the enteral feeding tube. Porto Alegre/RS, Brasil, 2011
DISCUSSION
In the present study, we found that the bedside auscultation test showed little consistency with the image (X-ray) in the identification of the anatomical location of the distal tip of the enteral feeding tube. In two of the 80 patients, the use of the FT without radiological confirmation of its critical position could have caused damages to patients, such as diet aspiration or infusion into the respiratory tract, which did not occur.
Although the use of enteral feeding tubes is common in hospitals, there are few studies that describe complication rates related to poor positioning and diet and / or drug administration through this device. A study(1313. Sorokin R, Gottlieb JE. Enhancing patient safety during feeding-tube insertion: a review of more than 2000 insertions. JPEN J Parenter Enteral Nutr. 2006;30(5):135-42.) performed in different units of a tertiary hospital in the United States, reviewed radiographic reports evaluating the placement of enteral feeding tubes. In 3789 enteral feeding intubations conducted from 2001 to 2004, in 1.3% (n = 50), the distal tip of the FT invaded tracheopulmonary sites. The similarities with our findings are not only found in the proportion of poor positioning, but in the fact that the majority of patients were also on mechanical ventilation (n = 26) and the distal tip of the FT was located in the right bronchus (n = 34).
Other studies(1414. Metheny NA, Stewart BJ, McClave SA. Relationship between feeding tube site and respiratory outcomes. JPEN J Parenter Enteral Nutr. 2011;35(3):346-55.-1515. Marco J, Barba R, Lazaro M, Matía P, Plaza S, Canora J, et al. Bronchopulmonary complications associated to enteral nutrition devices in patients admitted to internal medicine departments. Rev Clin Esp. 2013;213(5):223-8.) show the association between the use of FT and the occurrence of aspiration pneumonia. In retrospective analyzes, one of these studies(1414. Metheny NA, Stewart BJ, McClave SA. Relationship between feeding tube site and respiratory outcomes. JPEN J Parenter Enteral Nutr. 2011;35(3):346-55.) found that one in three patients using FT had pulmonary complications, and a 59% increase in the probability of dying during hospitalization when compared to patients using gastrostomy or jejunostomy. Although the theme is relevant, scientific production, mainly of prospective studies, is scarce. Case studies and case series reporting tension pneumothorax, acute respiratory distress syndrome, aspiration pneumonia, tracheoesophageal fistula, among other complications related to the use of FT(22. Agha R, Siddiqui MRS. Pneumotorax after nasogastric tube insertion. JRSM Rep. 2011;2(4):28.
3. Takwoingi YM. Inadvertent insertion of a nasogastric tube into both main bronchi of an awake patient: a case report. Cases J. 2009;2:6914.-44. Stayner JL, Bhatnagar A, McGinn AN, Fang JC. Feeding tube placement: errors and complications. Nutr Clin Pract. 2012;27(6):738-48.,1616. Freeberg SY, Carrigan TP, Culver DA, Guzman JA. Case series: tension pneumothorax complicating narrow-bore enteral feeding tube placement. J Intensive Care Med. 2010;25(5):281-5.) are found in greater proportion medical literature, but these publications still generate low level of evidence.
Given this scenario, and the wide use of auscultation tests to confirm the anatomical location of the FT(1010. Simons SR, Abdallah LM. Bedside assessment of enteral tube placement: aligning practice with evidence. AJN. 2012;112(2):40-6.) in clinical practice, this study aligns with recent publications(1717. Turgay AS, Khorshid L. Effectiveness of the auscultatory and pH methods in predicting feeding tube placement. J Clin Nurs. 2010;19(11/12):1553-9.-1818. Boeykens K, Steeman E, Duysburgh I. Reliability of pH measurement and the auscultatory method to confirm the position of a nasogastric tube. Int J Nurs Stud. 2014;51(11):1427-33.) that compared the use of bedside tests (auscultation test and pH) to X-rays (reference standard). The first study(17) evaluated 44 patients admitted to an Intensive Care Unit (ICU), undergoing enteral intubation by nurses, who also performed the auscultation test and issued their opinion. The authors found data that is consistent with the data herein presented. Of all the procedures, the nurses said that the tip of FT was in the stomach in 40 cases (90.9%) when the X-ray showed 39 (88.6%) FT in this location, resulting in a weak agreement (K = 0.112, p = 0.453). The authors emphasize that of the five FTs that were not in the stomach (three in the pylorus and two in the esophagus), four were confirmed by the nurses as being located in the stomach.
In another study(1818. Boeykens K, Steeman E, Duysburgh I. Reliability of pH measurement and the auscultatory method to confirm the position of a nasogastric tube. Int J Nurs Stud. 2014;51(11):1427-33.), which also evaluated the auscultation and pH tests, 331 enteral intubations were performed in 314 patients, where 24.2% (n = 76) were admitted to ICU. The auscultation test was performed in all procedures, whereas X-rays were performed on 301. A sensitivity of 79% and specificity of 61% of the auscultation test to correctly identify the gastric position of FT was identified. It is interesting to note that the authors relate the clarity of auscultation (noise volume) with the probability of correctness in locating the position of the FT. They report that in cases where low sound or no sound was heard, the distal tip of FT was located in the esophagus (n = 9), lung (n = 3); in the duodenum (n = 2) and the trachea (n = 5). The authors of these last two studies(1717. Turgay AS, Khorshid L. Effectiveness of the auscultatory and pH methods in predicting feeding tube placement. J Clin Nurs. 2010;19(11/12):1553-9.-1818. Boeykens K, Steeman E, Duysburgh I. Reliability of pH measurement and the auscultatory method to confirm the position of a nasogastric tube. Int J Nurs Stud. 2014;51(11):1427-33.) discourage the use of the auscultation test, suggesting the adoption of pH measurement of gastric residue as a more reliable alternative to the auscultation test, at the bedside, to determine the location of the distal tip of the FT.
In the latter(1818. Boeykens K, Steeman E, Duysburgh I. Reliability of pH measurement and the auscultatory method to confirm the position of a nasogastric tube. Int J Nurs Stud. 2014;51(11):1427-33.), the authors suggest that tests resulting in gastric residue pH values ≤5,5 are predictive of the FT being located in the stomach. However, they admit that this pH value can also be found when the FT tip in the esophageal position. In the study mentioned above(1717. Turgay AS, Khorshid L. Effectiveness of the auscultatory and pH methods in predicting feeding tube placement. J Clin Nurs. 2010;19(11/12):1553-9.), the authors categorically recommend the use of pH test, although the study conducted by them included a small number of patients and the role of co-variables involved in the residue pH values have not been evaluated. Therefore, it is important to note that despite the fact that these clinical studies suggest good accuracy of the pH test, in practice, it can be affected by various conditions as alkalosis or metabolic acidosis, use of antacids (proton pump inhibitors and H2 receptor antagonists) or the volume of gastric residue, which was not adjusted or isolated in recent studies.
In a systematic review(19) on the accuracy of pH and other biochemical markers as predictors of the FT location, the evidence was considered limited, mainly because there are no studies with methodological robustness or consensus regarding the cutoff point for the pH value.
In practice, inserting, identifying and maintaining the FT in the appropriate anatomical site can be a challenge. A technology that is more available in hospitals is the ultrasound. There have not yet been sufficiently robust studies to determine the accuracy of this diagnostic test in confirming the positioning of the FT. But, the researches available(2020. Kim HM, So BH, Jeong WJ, Choi SM, Park KN. The effectiveness of ultrasonography in verifying the placement of a nasogastric tube in patients with low consciousness at an emergency center. Scand J Trauma Resusc Emerg Med. 2012;38(20):1-6.-2121. Chenaitia H, Brun PM, Querellou E, Leyral J, Bessereau J, Aimé C, et al. Ultrasound to confirm gastric tube placement in prehospital management. Resuscitation. 2012;83(4):447-51.) suggests that this technology is promising for clinical practice (close to 100% sensitivity and specificity between 67% and 100%).
In one of these studies(2020. Kim HM, So BH, Jeong WJ, Choi SM, Park KN. The effectiveness of ultrasonography in verifying the placement of a nasogastric tube in patients with low consciousness at an emergency center. Scand J Trauma Resusc Emerg Med. 2012;38(20):1-6.), the auscultation the test and ultrasound were compared with the reference pattern (X-ray). Interestingly, the authors found higher agreement with our study when compared to the auscultation test vs. X-ray (K = 0.484). In this study, ultrasonography was considered by the authors as an efficient method to confirm the results of the auscultation test in the FT insertion in patients with sensorial loss. Bedside ultrasonography would have the advantage of reducing radiation exposure, the time between insertion and confirmation of the FT positioning and enables the daily verification of the FT's distal tip location, adding patient safety.
Because this is the evaluation of an agreement among professionals, the limitations of this study may be related to experience both of the attending nurses and nurse researchers in the detection of the placement of enteral feeding tubes through the auscultation test. It may be necessary to conduct studies to isolate the effects of variables such as years of experience or number of enteral feeding tube insertions in a given period of time, which are not objects in this study.
New clinical studies, with the inclusion of more patients and adoption of methodologies that promote higher levels of evidence, should be conducted in order to describe and test other technologies in the identification of the position of FTs. It is necessary to establish routine performance standards for nursing activities focusing on the improvement in patient safety, given the quality of policies. In this sense, the findings of this study contribute to support nursing education, with regard to the safety of the enteral feeding tube insertion procedure, extending the research perspective in this area.
CONCLUSION
In the present study, we found that the impression of the attending nurse and nurse researcher for the clinical trial of beside auscultation showed little consistency with the image (X-ray) in identifying the anatomical location of the distal tip of enteral feeding tube. Although the auscultation test is widely used in clinical practice and taught in nursing education, it should not be used alone, which maintans the X-ray as a standard examination in that condition.
REFERENCES
-
1Kattelmann K, Hise M, Russell M, Charney P, Stokes M, Compher C. Preliminary evidence for a medical nutrition therapy protocol: enteral feedings for critically ill patients. J Am Diet Assoc. 2006;106:1226-41.
-
2Agha R, Siddiqui MRS. Pneumotorax after nasogastric tube insertion. JRSM Rep. 2011;2(4):28.
-
3Takwoingi YM. Inadvertent insertion of a nasogastric tube into both main bronchi of an awake patient: a case report. Cases J. 2009;2:6914.
-
4Stayner JL, Bhatnagar A, McGinn AN, Fang JC. Feeding tube placement: errors and complications. Nutr Clin Pract. 2012;27(6):738-48.
-
5Sparks DA, Chase DM, Coughlin LM, Perry E. Pulmonary complications of 9931 narrow-bore nasoenteric tubes during blind placement: a critical review. JPEN J Parenter Enteral Nutr. 2011;35(5):625-9.
-
6Malta MA, Carvalho-Junior AF, Andreollo NA, Freitas MIP. Medidas antropométricas na introdução da sonda nasogástrica para nutrição enteral empregando esofagogastroduodenoscopia. Arq Bras Cir Dig. 2013;26(2):107-11.
-
7Leães MD, Mello E, Beghetto M, de Silva Assis MC. Enteral feeding tubes: are insertion techniques and positioning based on anatomical evidence? Nutr Health. 2012;21(3)193-200.
-
8Chen YC, Wang LY, Chang YJ, Yang CP, Wu TJ, Lin FR, et al. Potential risk of malposition of nasogastric tube using nose-ear-xiphoid measurement. PLoS One. 2014;9(2):1-7.
-
9Stock A, Gilbertson HR, Babi FE. Confirming nasogastric tube position in the emergency department: pH testing is reliable. Pediatr Emerg Care. 2008;24(12):805-9.
-
10Simons SR, Abdallah LM. Bedside assessment of enteral tube placement: aligning practice with evidence. AJN. 2012;112(2):40-6.
-
11Leães DM. Avaliação do procedimento de inserção de sonda enteral [dissertação]. Porto Alegre (RS): Faculdade de Medicina, Universidade Federal do Rio Grande do Sul; 2012.
-
12Hanson RL. Predictive criteria for length of nasogastric tube insertion for tube feeding. JPEN J Parenter Enteral Nutr. 1979;3(3):160-3.
-
13Sorokin R, Gottlieb JE. Enhancing patient safety during feeding-tube insertion: a review of more than 2000 insertions. JPEN J Parenter Enteral Nutr. 2006;30(5):135-42.
-
14Metheny NA, Stewart BJ, McClave SA. Relationship between feeding tube site and respiratory outcomes. JPEN J Parenter Enteral Nutr. 2011;35(3):346-55.
-
15Marco J, Barba R, Lazaro M, Matía P, Plaza S, Canora J, et al. Bronchopulmonary complications associated to enteral nutrition devices in patients admitted to internal medicine departments. Rev Clin Esp. 2013;213(5):223-8.
-
16Freeberg SY, Carrigan TP, Culver DA, Guzman JA. Case series: tension pneumothorax complicating narrow-bore enteral feeding tube placement. J Intensive Care Med. 2010;25(5):281-5.
-
17Turgay AS, Khorshid L. Effectiveness of the auscultatory and pH methods in predicting feeding tube placement. J Clin Nurs. 2010;19(11/12):1553-9.
-
18Boeykens K, Steeman E, Duysburgh I. Reliability of pH measurement and the auscultatory method to confirm the position of a nasogastric tube. Int J Nurs Stud. 2014;51(11):1427-33.
-
19Fernandez RS, Chau JPC, Thompson DR. Accuracy of biochemical markers for predicting nasogastric tube placement in adults: a systematic review of diagnostic studies. Int J Nurs Stud. 2010;47(8):1037-46.
-
20Kim HM, So BH, Jeong WJ, Choi SM, Park KN. The effectiveness of ultrasonography in verifying the placement of a nasogastric tube in patients with low consciousness at an emergency center. Scand J Trauma Resusc Emerg Med. 2012;38(20):1-6.
-
21Chenaitia H, Brun PM, Querellou E, Leyral J, Bessereau J, Aimé C, et al. Ultrasound to confirm gastric tube placement in prehospital management. Resuscitation. 2012;83(4):447-51.
Publication Dates
-
Publication in this collection
Oct-Dec 2015
History
-
Received
03 June 2015 -
Accepted
31 Aug 2015


 Source: Research data, 2011. The intersections of the same category express the concordance between the evaluators. Data expressed in absolute numbers.
Source: Research data, 2011. The intersections of the same category express the concordance between the evaluators. Data expressed in absolute numbers.
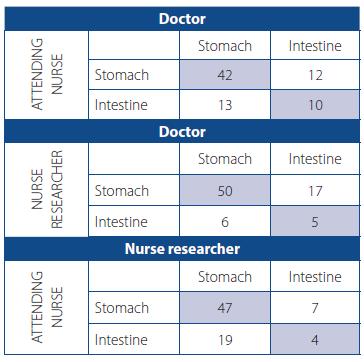 Source: Research data, 2011. The intersections of the same category express the concordance between the evaluators. Data expressed in absolute numbers.
Source: Research data, 2011. The intersections of the same category express the concordance between the evaluators. Data expressed in absolute numbers.