Abstract
Platynosomiasis is a common feline hepatic disease caused by Platynosomum fastosum (Trematoda - Dicrocoelidae), which is also known as ‘lizard poisoning’. Most reports of feline platynosomiasis show that this disease is sporadic and manifests with uncommon lesions; its pathogenicity is still not well understood. This study aimed to describe liver injuries and enzymatic changes associated with natural P. fastosum infection in 47 stray cats in an endemic area. Overall, 38.3% (18/47) of cats were parasitized, and 2,358 flukes (P. fastosum) were collected (131 – mean intensity of parasitism; 50.2 – mean abundance). The alanine transaminase (ALT) measure was significantly higher in parasitized animals, while alkaline phosphatase (ALP) showed no statistical difference between parasitized and non-parasitized animals. In infected animals, gross pathological lesions and microscopic liver injuries ranged from mild to severe, and were similar to those in previous descriptions of feline platynosomiasis. Nonetheless, the intensity of parasitism was not related to the severity of macroscopic or microscopic hepatic injuries. However, feline platynosomiasis should be considered in the differential diagnosis of feline liver disorders, as well as, in any program of helminth control, even if no clinical abnormalities are present.
Keywords:
Platynosomum fastosum; liver; lesions; ALT; ALP
Resumo
Platinossomiase é uma doença hepática felina comum causada por Platynosomum fastosum (Trematoda - Dicrocoelidae), também é conhecida como “envenenamento por lagartixa”. A maioria dos relatos de platinossomiase felina mostra que esta doença é esporádica e se manifesta com lesões incomuns; sua patogenicidade ainda não é bem compreendida. Este estudo objetivou descrever as lesões no fígado e alterações enzimáticas associadas à infecção natural por P. fastosum em 47 gatos errantes em uma área endêmica. No total, 38,3% (18/47) dos gatos estavam parasitados, e 2.358 trematódeos (P. fastosum) foram coletados (131 – intensidade média de parasitismo; 50,2 – abundância média). A quantidade de alanina transaminase (ALT) foi significativamente maior nos animais parasitados, enquanto a fosfatase alcalina (ALP) não apresentou diferença estatística entre os animais parasitados e não parasitados. Nos animais infectados, lesões patológicas macroscópicas e microscópicas hepáticas variaram de leve a grave, e foram semelhantes a descrições anteriores de platinossomiase felina. No entanto, a intensidade do parasitismo não foi relacionada à gravidade das lesões hepáticas macroscópicas ou microscópicas. Contudo, a platinossomiase felina deve ser considerada no diagnóstico diferencial de distúrbios hepáticos em felinos, assim como, em qualquer programa de controle de helmintos, mesmo que nenhuma anormalidade clínica esteja presente.
Palavras-chaves:
Platynosomum fastosum; fígado; lesões; ALT; ALP
Introduction
Platynosomiasis is a common hepatic disease in cats caused by Platynosomum fastosum, Looss, 1907 (Trematoda - Dicrocoelidae), which is also known as ‘lizard poisoning’ (CATCOTT, 1964Catcott EJ. Feline Medicine and Surgery (Flukes by Renaux, E.A.). Santa Barbara: American Veterinary Publication; 1964.). These liver flukes are found in tropical and sub-tropical regions and parasitize cats from the Pacific Islands, North America, South America, the Caribbean, Africa, Asia, and Oceania (BASU & CHARLES, 2014Basu AK, Charles RA. A review of the cat liver fluke Platynosomum fastosum Kossack, 1910 (Trematoda: Dicrocoeliidae). Vet Parasitol 2014; 200(1-2): 1-7. PMid:24412358. http://dx.doi.org/10.1016/j.vetpar.2013.12.016.
http://dx.doi.org/10.1016/j.vetpar.2013....
). A previous study described P. fastosum, P. concinnum and P. illiciens as synonymous and all affect the liver, gallbladder, and bile ducts in cats (MALDONADO, 1945Maldonado JF. The life history and biology of Kossak, 1910 (Trematoda, Dicrocoeliidae). Platynosomum fastosumPR J Public Health Trop Med 1945; 21(1): 17-39.). The life cycle involves the terrestrial mollusk Subulina octona (ASH, 1962Ash LR. Helminth parasites of dogs and cats in Hawaii. J Parasitol 1962; 48(1): 63-65. PMid:13862798. http://dx.doi.org/10.2307/3275412.
http://dx.doi.org/10.2307/3275412...
), as the first intermediate host, and reptiles and amphibians (MALDONADO, 1945Maldonado JF. The life history and biology of Kossak, 1910 (Trematoda, Dicrocoeliidae). Platynosomum fastosumPR J Public Health Trop Med 1945; 21(1): 17-39.) as paratenic hosts. Isopods can also be involved in the direct transmission of the parasite to the definitive or paratenic hosts, especially in South America (PINTO et al., 2014Pinto HA, Mati VLT, Melo AL. New insights into the life cycle of (Trematoda: Dicrocoeliidae). PlatynosomumParasitol Res 2014; 113(7): 2701-2707. PMid:24802870. http://dx.doi.org/10.1007/s00436-014-3926-5.
http://dx.doi.org/10.1007/s00436-014-392...
).
The importance of platynosomiasis in feline medicine is in strong contrast with the scarcity of studies describing the diagnosis and clinical presentation of this disease (RAMOS et al., 2013Ramos DGS, Scheremeta RGAC, Oliveira ACS, Sinkoc AL, Pacheco RC. Survey of helminth parasites of cats from the metropolitan area of Cuiabá, Mato Grosso, Brazil. Rev Bras Parasitol Vet 2013; 22(2): 201-206. PMid:23856737. http://dx.doi.org/10.1590/S1984-29612013000200040.
http://dx.doi.org/10.1590/S1984-29612013...
; BRAGA et al., 2016Braga RR, Teixeira AC, Oliveira JA, Cavalcanti LP. Prevalence of infection in free roaming cats in northeastern Brazil: fluke burden and grading of lesions. Platynosomum fastosumVet Parasitol 2016; 227: 20-25. PMid:27523932. http://dx.doi.org/10.1016/j.vetpar.2016.07.021.
http://dx.doi.org/10.1016/j.vetpar.2016....
). The most common microscopic lesions include cholangiectasis, cholangiohepatitis, atrophy of hepatocytes, and hyperplasia of the biliary duct epithelium, which results in thickening of the liver, fatty infiltration of hepatocytes, sections of flukes and/or eggs in the liver, and abundant hepatic infiltration of leukocytes and eosinophils (BASU & CHARLES, 2014Basu AK, Charles RA. A review of the cat liver fluke Platynosomum fastosum Kossack, 1910 (Trematoda: Dicrocoeliidae). Vet Parasitol 2014; 200(1-2): 1-7. PMid:24412358. http://dx.doi.org/10.1016/j.vetpar.2013.12.016.
http://dx.doi.org/10.1016/j.vetpar.2013....
). However, most cases of platynosomiasis in cats have been described as incidental findings during necropsies (O’SULLIVAN et al., 1976O’Sullivan BM, Rosenfeld LE, Green PE. Concurrent infection with Yersinia pseudotuberculosis and Platynosomum fastosum in a cat. Aust Vet J 1976; 52(5): 232-233. PMid:786240. http://dx.doi.org/10.1111/j.1751-0813.1976.tb00077.x.
http://dx.doi.org/10.1111/j.1751-0813.19...
; HANEY et al., 2006Haney DR, Christiansen JS, Toll J. Severe cholestatic liver disease secondary to liver fluke (Platynosomum concinnum) infection in three cats. J Am Anim Hosp Assoc 2006; 42(3): 234-237. PMid:16611937. http://dx.doi.org/10.5326/0420234.
http://dx.doi.org/10.5326/0420234...
; XAVIER et al., 2007Xavier FG, Morato GS, Righi DA, Maiorka PC, Spinosa HS. Cystic liver disease related to high Platynosomum fastosum infection in a domestic cat. J Feline Med Surg 2007; 9(1): 51-55. PMid:17241806. http://dx.doi.org/10.1016/j.jfms.2006.08.006.
http://dx.doi.org/10.1016/j.jfms.2006.08...
; CARREIRA et al., 2008Carreira VS, Vieira RF, Machado GF, Luvizotto MC. Feline cholangitis/cholangiohepatitis complex secondary to infection in a cat. Platynosomum fastosumRev Bras Parasitol Vet 2008;17(S1 Suppl 1): 184-187. PMid:20059845.; LENIS et al., 2009Lenis C, Navarro F, Velez I. First case of platinosomosis from Colombia: Platynosomum illiciens (Digenea: Dicrocoeliidae) in , Turbo, Antioquia. Felis catusRev Colom Cienc Pecua 2009; 22(4): 659-663.; ANDRADE et al., 2012Andrade RL, Dantas AF, Pimentel LA, Galiza GJ, Carvalho FK, Costa VM, et al. induced cholangiocarcinomas in cats. Platynosomum fastosum-Vet Parasitol 2012; 190(1-2): 277-280. PMid:22963714. http://dx.doi.org/10.1016/j.vetpar.2012.04.015.
http://dx.doi.org/10.1016/j.vetpar.2012....
). Therefore, the present study aimed to describe the macroscopic and microscopic liver injuries associated with natural P. fastosum infection in stray cats in an endemic area of midwestern Brazil, and to investigate an association between parasite burden and pathological and biochemical findings.
Materials and Methods
From January to July 2014, 47 adult (20 males and 27 females) stray cats (Felis silvestris catus, Linnaeus, 1758) from Várzea Grande municipality, Mato Grosso State in midwestern Brazil, classified according to dental development, maturation of genital structure and body size (SHARIF et al., 2007Sharif M, Nasrolahei M, Ziapour SP, Gholami S, Ziaei H, Daryani A, et al. infections in stray cats in northern Iran. Toxocara catiJ Helminthol 2007; 81(1): 63-66. PMid:17381869. http://dx.doi.org/10.1017/S0022149X07214117.
http://dx.doi.org/10.1017/S0022149X07214...
) were subjected to necropsy procedures. These animals were received or captured by the Zoonosis Control Center (CCZ) and then euthanized according to the protocol of the American Veterinary Medical Association (AVMA) Guidelines on Euthanasia (AVMA, 2001American Veterinary Medical Association – AVMA. Report of the AVMA panel on Euthanasia. J Am Vet Med Assoc 2001; 218(5): 669-696. PMid:11280396. http://dx.doi.org/10.2460/javma.2001.218.669.
http://dx.doi.org/10.2460/javma.2001.218...
). During necropsy, the liver and gallbladder were completed cut and the bile duct was mechanically expressed through a sieve (0.15 mm) to expel any flukes present (RODRÍGUEZ-VIVAS et al., 2004Rodriguez-Vivas RI, Williams JJ, Quijano-Novelo AG, Bolio GM, Torres-Acosta JF. Prevalence, abundance and risk factors of liver fluke (Platynosomum fastosum) infection in cats in Mexico. Vet Rec 2004; 154(22): 693-694. PMid:15200076. http://dx.doi.org/10.1136/vr.154.22.693.
http://dx.doi.org/10.1136/vr.154.22.693...
). All content was analyzed using a stereomicroscope under 10× magnification (RAMOS et al., 2013Ramos DGS, Scheremeta RGAC, Oliveira ACS, Sinkoc AL, Pacheco RC. Survey of helminth parasites of cats from the metropolitan area of Cuiabá, Mato Grosso, Brazil. Rev Bras Parasitol Vet 2013; 22(2): 201-206. PMid:23856737. http://dx.doi.org/10.1590/S1984-29612013000200040.
http://dx.doi.org/10.1590/S1984-29612013...
). Fragments of the distal portion of the right middle liver lobe were fixed in 10% formalin, submitted for routine processing techniques, and stained by hematoxylin-eosin for histopathological examination (PROPHET et al., 1992Prophet EB, Mills B, Arrington JB, Sobin LH. AFIP Laboratory Methods in Histotechnology. Washington, DC: Armed Force Registry of Pathology; 1992.). Before euthanasia, blood serum samples were collected and serum enzyme concentrations of alanine transaminase (ALT) and alkaline phosphatase (ALP) were assayed.
The sample size was assessed considering the prevalence of 26% (RAMOS et al., 2013Ramos DGS, Scheremeta RGAC, Oliveira ACS, Sinkoc AL, Pacheco RC. Survey of helminth parasites of cats from the metropolitan area of Cuiabá, Mato Grosso, Brazil. Rev Bras Parasitol Vet 2013; 22(2): 201-206. PMid:23856737. http://dx.doi.org/10.1590/S1984-29612013000200040.
http://dx.doi.org/10.1590/S1984-29612013...
) with 95% confidence level and 5% statistical error. Prevalence, mean intensity of parasitism (MIP), and mean abundance (MA) were calculated as described by Bush et al. (1997)Bush AO, Lafferty KD, Lotz JM, Shostak AW. Parasitology meets ecology on its own terms: Margolis et al. revisited. J Parasitol 1997; 83(4): 575-583. PMid:9267395. http://dx.doi.org/10.2307/3284227.
http://dx.doi.org/10.2307/3284227...
. Mean intensity statistical analysis were performed using the methodology of generalized linear models (GLM) and the statistical package R (R DEVELOPMENT CORE TEAM, 2011R Development Core Team. R: a language and environment for statistical computing, reference index version 2.14.0. Vienna: R Foundation for Statistical Computing; 2011 [cited 2016 Oct 18]. Available from http://www.r-project.org.
http://www.r-project.org...
) by comparing presence of injuries. For variable mean intensity, Poisson distribution (count of individuals) was used, with the logarithmic link function as a linear predictor. Serum enzyme concentrations of ALT and ALP from cats infected with P. fastosum were also compared using the Wilcoxon-Mann-Whitney test.
The Bioethical Committee for Animal Research of the Federal University of Mato Grosso approved the present study, under protocol no. 23108.011507/13-4.
Results
In total, 38.3% (18/47) of cats (8 males and 10 females) were parasitized by P. fastosum with no gender-specific association. There was a significant increase of serum activity of the hepatic enzyme ALT (reference range: 6-83 U/L; JAIN, 1993Jain NC. Essentials of veterinary hematology. Philadelphia: Lea & Febiger; 1993.) in parasitized animals (p-value= 0.029), while ALP showed no statistical difference from the normal values (Table 1). Overall, 2,358 flukes were collected (131-MIP; 50.2-MA), and cats harboring liver flukes showed different levels of infection: in 72.2% (13/18) of cats, less than 40 P. fastosum were found per animal; in 16.7% (3/18), more than 500 parasites/cat were observed; and in 11.1% (2/18) 147 (cat number 8) and 300 (cat number 15) flukes were found, as shown in Table 2.
Mean amount (U/L) of alanine transaminase (ALT) and alkaline phosphatase (ALP) from stray cats from Várzea Grande municipality, midwestern Brazil, naturally parasitized and non-parasitized with Platynosomum fastosum.
Macroscopic characteristics of livers from cats naturally parasitized with Platynosomum fastosum of Várzea Grande municipality, midwestern Brazil.
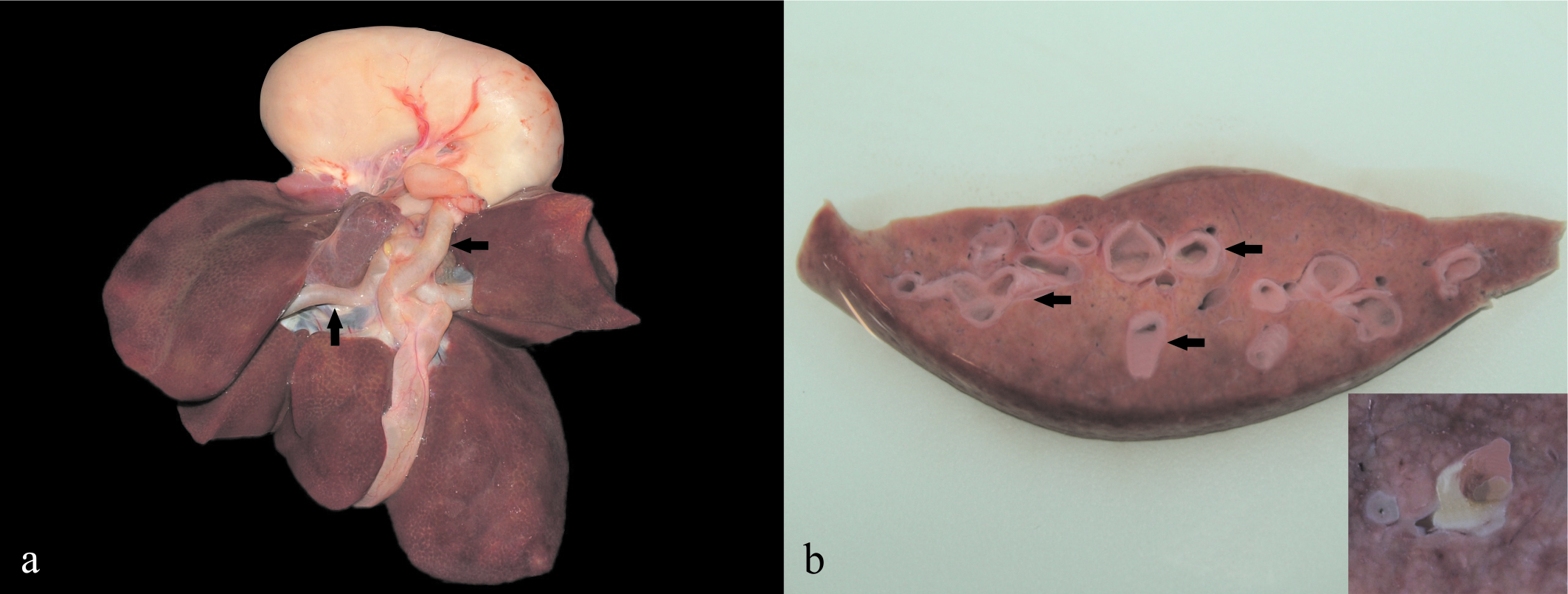
Macroscopic characteristics observed in livers infected with P. fastosum were extrahepatic and intrahepatic bile duct distension (Figure 1) in 61.1% (11/18) of livers sampled, visualization of bile ducts on the hepatic surface due to wall thickening of the bile duct in 33.3% (6/18), and jaundice in 16.7% (3/18) (Table 2). Furthermore, P. fastosum were also observed in the gallbladder and bile ducts (Figure 1) in 44.4% (8/18) of livers (Table 2), during necropsy.
Macroscopic lesions of livers from cats from Várzea Grande municipality, midwestern Brazil, naturally parasitized with Platynosomum fastosum. (a) Liver of Cat 1 with severe extra hepatic bile duct distension. (b) Liver cut surface of Cat 8 showing multifocal severe intrahepatic bile duct distension. Inset: liver cut surface of Cat 15 showing two specimens of Platynosomum fastosum in the lumen of a distended bile duct.
All histological changes are showed in Table 3, and the most common microscopic lesions observed in 94.4% (17/18) of the livers from infected cats included: periportal proliferation of the bile ducts; periportal fibrosis, and sometimes bridging fibrosis; periportal cholangitis consisting of infiltrates of lymphocytes, plasmocytes and eosinophils; and cholangioectasis (Figure 2). Additionally, hyperplasia of bile duct epithelium (Figure 2) was seen in 83.3% (15/18) of samples, while cholestasis was observed in lower frequency (16.7% [3/18]) as noted in Table 3. Cross-sections of adult P. fastosum (Figure 2) were seen in bile ducts/gallbladders of 27.8% (5/18) of livers (Table 3). Adult trematodes were characterized (BASU & CHARLES, 2014Basu AK, Charles RA. A review of the cat liver fluke Platynosomum fastosum Kossack, 1910 (Trematoda: Dicrocoeliidae). Vet Parasitol 2014; 200(1-2): 1-7. PMid:24412358. http://dx.doi.org/10.1016/j.vetpar.2013.12.016.
http://dx.doi.org/10.1016/j.vetpar.2013....
) by a thin cuticle without spines, no celomatic cavity, oral and ventral suckers, intestines, testes, ovaries vitellaries and uterus; operculated eggs were observed throughout delimitation of the uterus (Figure 2). No association was observed between the severity of the macroscopic or microscopic hepatic lesions and the parasitic burden by P. fastosum.
Histologic characteristics of livers from cats naturally parasitized with Platynosomum fastosum of Várzea Grande municipality, midwestern Brazil.
Microscopic lesions of livers from cats naturally parasitized with Platynosomum fastosum of Várzea Grande municipality, midwestern Brazil. (a) Liver of Cat 8 showing periportal fibrosis forming bridges between portal areas, proliferation of bile ducts, periportal cholangitis and cholangioectasis. Hematoxylin and eosin (10x objective lens). (b) Liver of Cat 8 showing periportal proliferation of the bile ducts, periportal fibrosis, severe cholangioectasis and four specimens of P. fastosum in the lumen of the distended bile duct. One of them is attached to the bile duct epithelium. Note the parasite thin cuticle without spines (c), no celomatic cavity, ventral sucker (vs), testes (t) and uterus (u) with eggs (e). Hematoxylin and eosin (10x objective lens).
Statistical analysis showed no significant relationship between mean intensity of parasitism and presence of injuries (jaundice, p=0.1941; visualization of the bile ducts on the hepatic surface, p=0.3308; extrahepatic bile ducts distension, p=0.1050; intrahepatic bile duct distension, p=0.1050; periportal proliferation of bile ducts, p=0.4364; periportal fibrosis, p=0.4364; cholestasis, p=0.1512; hyperplasia of the bile duct epithelium, p=0.5846; cholangiectasis, p=0.4364; periportal cholangitis, p=0.4364).
Discussion
Prevalence of the liver fluke, P. fastosum, in cats has been described as ranging from 0.07 to 81% worldwide (BASU & CHARLES, 2014Basu AK, Charles RA. A review of the cat liver fluke Platynosomum fastosum Kossack, 1910 (Trematoda: Dicrocoeliidae). Vet Parasitol 2014; 200(1-2): 1-7. PMid:24412358. http://dx.doi.org/10.1016/j.vetpar.2013.12.016.
http://dx.doi.org/10.1016/j.vetpar.2013....
). In Brazil, the occurrence of parasitic infection with P. fastosum is commonly described as being related to sporadic cases of liver disorders (XAVIER et al., 2007Xavier FG, Morato GS, Righi DA, Maiorka PC, Spinosa HS. Cystic liver disease related to high Platynosomum fastosum infection in a domestic cat. J Feline Med Surg 2007; 9(1): 51-55. PMid:17241806. http://dx.doi.org/10.1016/j.jfms.2006.08.006.
http://dx.doi.org/10.1016/j.jfms.2006.08...
; CARREIRA et al., 2008Carreira VS, Vieira RF, Machado GF, Luvizotto MC. Feline cholangitis/cholangiohepatitis complex secondary to infection in a cat. Platynosomum fastosumRev Bras Parasitol Vet 2008;17(S1 Suppl 1): 184-187. PMid:20059845.; ANDRADE et al., 2012Andrade RL, Dantas AF, Pimentel LA, Galiza GJ, Carvalho FK, Costa VM, et al. induced cholangiocarcinomas in cats. Platynosomum fastosum-Vet Parasitol 2012; 190(1-2): 277-280. PMid:22963714. http://dx.doi.org/10.1016/j.vetpar.2012.04.015.
http://dx.doi.org/10.1016/j.vetpar.2012....
), and few previous surveys having determined the prevalence or frequency of occurrence of P. fastosum in cats. Ferreira et al. (1999)Ferreira AMR, Almeida ECP, Labarthe NV. Liver fluke infection (Platynosomum concinnum) in Brazilian cats: prevalence and pathology. Feline Pract 1999; 27(2): 19-22. observed 37.27% of prevalence in Rio de Janeiro, southeast Brazil, Ramos et al. (2013)Ramos DGS, Scheremeta RGAC, Oliveira ACS, Sinkoc AL, Pacheco RC. Survey of helminth parasites of cats from the metropolitan area of Cuiabá, Mato Grosso, Brazil. Rev Bras Parasitol Vet 2013; 22(2): 201-206. PMid:23856737. http://dx.doi.org/10.1590/S1984-29612013000200040.
http://dx.doi.org/10.1590/S1984-29612013...
26.03% in Mato Grosso, midwest Brazil, while Braga et al. (2016)Braga RR, Teixeira AC, Oliveira JA, Cavalcanti LP. Prevalence of infection in free roaming cats in northeastern Brazil: fluke burden and grading of lesions. Platynosomum fastosumVet Parasitol 2016; 227: 20-25. PMid:27523932. http://dx.doi.org/10.1016/j.vetpar.2016.07.021.
http://dx.doi.org/10.1016/j.vetpar.2016....
showed overall prevalence of P. fastosum in free roaming domestic cats of 42.6% in Ceará, northeast Brazil. According to Braga et al. (2016)Braga RR, Teixeira AC, Oliveira JA, Cavalcanti LP. Prevalence of infection in free roaming cats in northeastern Brazil: fluke burden and grading of lesions. Platynosomum fastosumVet Parasitol 2016; 227: 20-25. PMid:27523932. http://dx.doi.org/10.1016/j.vetpar.2016.07.021.
http://dx.doi.org/10.1016/j.vetpar.2016....
many of these observed prevalences could have been higher, if a more sensitive diagnostic method had been used. The authors observed that bile microscopic egg detection was shown to be 1.6 times more sensitive than manual collection of trematodes by necropsy. Here, we described a higher prevalence (38.3%) of P. fastosum in stray cats compared to that in a previous study (RAMOS et al., 2013Ramos DGS, Scheremeta RGAC, Oliveira ACS, Sinkoc AL, Pacheco RC. Survey of helminth parasites of cats from the metropolitan area of Cuiabá, Mato Grosso, Brazil. Rev Bras Parasitol Vet 2013; 22(2): 201-206. PMid:23856737. http://dx.doi.org/10.1590/S1984-29612013000200040.
http://dx.doi.org/10.1590/S1984-29612013...
), performed in the same study area. This may be attributed to the sample population (adult stray cats), as animals aged 2 years or older are more frequently infected (FOLEY, 1994Foley RH. Platynosomum concinnum infection in cats. Compend Contin Educ Pract Vet 1994; 16(10): 1271-1277.; RODRIGUEZ-VIVAS et al., 2004Rodriguez-Vivas RI, Williams JJ, Quijano-Novelo AG, Bolio GM, Torres-Acosta JF. Prevalence, abundance and risk factors of liver fluke (Platynosomum fastosum) infection in cats in Mexico. Vet Rec 2004; 154(22): 693-694. PMid:15200076. http://dx.doi.org/10.1136/vr.154.22.693.
http://dx.doi.org/10.1136/vr.154.22.693...
; SALOMÃO et al., 2005Salomão M, Souza-Dantas LM, Almeida FM, Branco AS, Bastos OPM, Sterman F, et al. Ultrasonography in hepatobiliary evaluation of domestic cats (Felis catus, L., 1758) infected by Looss, 1907. PlatynosomumIntern J Appl Res Vet Med 2005; 3(3): 271-279.; BRAGA et al., 2016Braga RR, Teixeira AC, Oliveira JA, Cavalcanti LP. Prevalence of infection in free roaming cats in northeastern Brazil: fluke burden and grading of lesions. Platynosomum fastosumVet Parasitol 2016; 227: 20-25. PMid:27523932. http://dx.doi.org/10.1016/j.vetpar.2016.07.021.
http://dx.doi.org/10.1016/j.vetpar.2016....
). Furthermore, free living cats have a higher probability of being infected with any of the intermediate hosts (SALOMÃO et al., 2005Salomão M, Souza-Dantas LM, Almeida FM, Branco AS, Bastos OPM, Sterman F, et al. Ultrasonography in hepatobiliary evaluation of domestic cats (Felis catus, L., 1758) infected by Looss, 1907. PlatynosomumIntern J Appl Res Vet Med 2005; 3(3): 271-279.; ANDRADE et al., 2012Andrade RL, Dantas AF, Pimentel LA, Galiza GJ, Carvalho FK, Costa VM, et al. induced cholangiocarcinomas in cats. Platynosomum fastosum-Vet Parasitol 2012; 190(1-2): 277-280. PMid:22963714. http://dx.doi.org/10.1016/j.vetpar.2012.04.015.
http://dx.doi.org/10.1016/j.vetpar.2012....
). Considering that platynosomiasis has been frequent among stray cats in the study area, it should be considered as a differential diagnosis in feline liver disorders (RAMOS et al., 2013Ramos DGS, Scheremeta RGAC, Oliveira ACS, Sinkoc AL, Pacheco RC. Survey of helminth parasites of cats from the metropolitan area of Cuiabá, Mato Grosso, Brazil. Rev Bras Parasitol Vet 2013; 22(2): 201-206. PMid:23856737. http://dx.doi.org/10.1590/S1984-29612013000200040.
http://dx.doi.org/10.1590/S1984-29612013...
), as well as, in helminth control programs, mainly in adult stray cats, even if no clinical abnormalities are present.
Signs of hepatic dysfunction have been reported including changes in serum ALT, with ALP usually remaining unaffected (FOLEY, 1994Foley RH. Platynosomum concinnum infection in cats. Compend Contin Educ Pract Vet 1994; 16(10): 1271-1277.; TAYLOR & PERRI, 1977Taylor D, Perri SF. Experimental infection of cats with the liver fluke Platynosomum concinnum.Am J Vet Res 1977; 38(1): 51-54. PMid:402094.; CARREIRA et al., 2008Carreira VS, Vieira RF, Machado GF, Luvizotto MC. Feline cholangitis/cholangiohepatitis complex secondary to infection in a cat. Platynosomum fastosumRev Bras Parasitol Vet 2008;17(S1 Suppl 1): 184-187. PMid:20059845.). A marked increase of ALT was detected, as described in a previous study (TAYLOR & PERRI, 1977Taylor D, Perri SF. Experimental infection of cats with the liver fluke Platynosomum concinnum.Am J Vet Res 1977; 38(1): 51-54. PMid:402094.) after 1 to 4 months in severely parasitized cats (~1,000 flukes), indicating damage to the parenchymal cells, thereby allowing leakage of the cytosol contents into circulation. As seen in other studies of feline platynosomiasis, serum ALP was within normal values (FOLEY, 1994Foley RH. Platynosomum concinnum infection in cats. Compend Contin Educ Pract Vet 1994; 16(10): 1271-1277.; TAYLOR & PERRI, 1977Taylor D, Perri SF. Experimental infection of cats with the liver fluke Platynosomum concinnum.Am J Vet Res 1977; 38(1): 51-54. PMid:402094.; CARREIRA et al., 2008Carreira VS, Vieira RF, Machado GF, Luvizotto MC. Feline cholangitis/cholangiohepatitis complex secondary to infection in a cat. Platynosomum fastosumRev Bras Parasitol Vet 2008;17(S1 Suppl 1): 184-187. PMid:20059845.). Usually, increase of ALP is associated with severe cholestasis (ALLISON, 2012Allison RW. Laboratory evaluation of the liver. In: Thrall MA, Weiser G, Allison RW, Campbell TW. Veterinary Hematology and Clinical Chemistry. 2nd ed. New Jersey: Wiley-Blackwell; 2012. 346 p.), which was observed in low frequency (16.6%), despite this clinical sign having been previously described in association to P. fastosum infection (HANEY et al., 2006Haney DR, Christiansen JS, Toll J. Severe cholestatic liver disease secondary to liver fluke (Platynosomum concinnum) infection in three cats. J Am Anim Hosp Assoc 2006; 42(3): 234-237. PMid:16611937. http://dx.doi.org/10.5326/0420234.
http://dx.doi.org/10.5326/0420234...
; BRAGA et al., 2016Braga RR, Teixeira AC, Oliveira JA, Cavalcanti LP. Prevalence of infection in free roaming cats in northeastern Brazil: fluke burden and grading of lesions. Platynosomum fastosumVet Parasitol 2016; 227: 20-25. PMid:27523932. http://dx.doi.org/10.1016/j.vetpar.2016.07.021.
http://dx.doi.org/10.1016/j.vetpar.2016....
).
Platynosomiasis is frequently considered an asymptomatic infection (TAYLOR & PERRI, 1977Taylor D, Perri SF. Experimental infection of cats with the liver fluke Platynosomum concinnum.Am J Vet Res 1977; 38(1): 51-54. PMid:402094.; FOLEY, 1994Foley RH. Platynosomum concinnum infection in cats. Compend Contin Educ Pract Vet 1994; 16(10): 1271-1277.). Previous studies have reported that the severity of clinical signs and lesions depends on the parasitic burden (TAYLOR & PERRI, 1977Taylor D, Perri SF. Experimental infection of cats with the liver fluke Platynosomum concinnum.Am J Vet Res 1977; 38(1): 51-54. PMid:402094.; FOLEY, 1994Foley RH. Platynosomum concinnum infection in cats. Compend Contin Educ Pract Vet 1994; 16(10): 1271-1277.; SALOMÃO et al., 2005Salomão M, Souza-Dantas LM, Almeida FM, Branco AS, Bastos OPM, Sterman F, et al. Ultrasonography in hepatobiliary evaluation of domestic cats (Felis catus, L., 1758) infected by Looss, 1907. PlatynosomumIntern J Appl Res Vet Med 2005; 3(3): 271-279.). Despite Braga et al. (2016)Braga RR, Teixeira AC, Oliveira JA, Cavalcanti LP. Prevalence of infection in free roaming cats in northeastern Brazil: fluke burden and grading of lesions. Platynosomum fastosumVet Parasitol 2016; 227: 20-25. PMid:27523932. http://dx.doi.org/10.1016/j.vetpar.2016.07.021.
http://dx.doi.org/10.1016/j.vetpar.2016....
have characterized the influence of fluke burden on the formation of lesions, and reported significant association with increasing degrees of ductular proliferation, here the same lesion was observed in 94.4% (17/18) of the livers from infected cats, but there was not observed association between the severity and the parasitic burden by P. fastosum. Unlike, in the present study severe lesions were observed in animals with low intensity of parasitism (less than 40 parasites in animals 1 and 7). Additionally, we observed cats with high parasite burdens (more than 500 flukes in animals 2 and 12) that showed mild injuries. In these cases, we believe that although these cats had a high intensity of parasitism at the time of death, they may have been only recently infected, and therefore, did not have sufficient time to develop lesions. Taylor & Perri (1977)Taylor D, Perri SF. Experimental infection of cats with the liver fluke Platynosomum concinnum.Am J Vet Res 1977; 38(1): 51-54. PMid:402094. recovered P. fastosum from livers of experimentally infected cats after the first week; however, microscopic changes were not noticed until 3 weeks following infection, indicating that platynosomiasis is a chronic and progressive disease (FERREIRA et al., 1999Ferreira AMR, Almeida ECP, Labarthe NV. Liver fluke infection (Platynosomum concinnum) in Brazilian cats: prevalence and pathology. Feline Pract 1999; 27(2): 19-22.; HEADLEY et al., 2012Headley SA, Gillen MA, Sanches AW, Satti MZ. Platynosomum fastosum- induced chronic intrahepatic cholangitis and spp. infections in feral cats from Grand Cayman. SpirometraJ Helminthol 2012; 86(2): 209-214. PMid:21729387. http://dx.doi.org/10.1017/S0022149X11000265.
http://dx.doi.org/10.1017/S0022149X11000...
; CARREIRA et al., 2008Carreira VS, Vieira RF, Machado GF, Luvizotto MC. Feline cholangitis/cholangiohepatitis complex secondary to infection in a cat. Platynosomum fastosumRev Bras Parasitol Vet 2008;17(S1 Suppl 1): 184-187. PMid:20059845.). Another variant that must be considered is variability in individual immune responses. Hosts adapted to parasites can show no immunological response, resulting in low grade or no pathological lesions even if affected by high infestation levels. Alternately, unadapted hosts, can suffer minimal parasite infestations, but exhibit severe inflammatory responses causing accentuated lesions (SPITHILL et al., 1997Spithill TW, Piedrafita D, Smooker PM. Immunological approaches for the control of fasciolosis. Int J Parasitol 1997; 27(10): 1221-1235. PMid:9394193. http://dx.doi.org/10.1016/S0020-7519(97)00120-3.
http://dx.doi.org/10.1016/S0020-7519(97)...
).
Gross pathological lesions observed in the livers of infected cats were similar to previous descriptions of lesions in feline platynosomiasis (HANEY et al., 2006Haney DR, Christiansen JS, Toll J. Severe cholestatic liver disease secondary to liver fluke (Platynosomum concinnum) infection in three cats. J Am Anim Hosp Assoc 2006; 42(3): 234-237. PMid:16611937. http://dx.doi.org/10.5326/0420234.
http://dx.doi.org/10.5326/0420234...
; HEADLEY et al., 2012Headley SA, Gillen MA, Sanches AW, Satti MZ. Platynosomum fastosum- induced chronic intrahepatic cholangitis and spp. infections in feral cats from Grand Cayman. SpirometraJ Helminthol 2012; 86(2): 209-214. PMid:21729387. http://dx.doi.org/10.1017/S0022149X11000265.
http://dx.doi.org/10.1017/S0022149X11000...
; BASU & CHARLES, 2014Basu AK, Charles RA. A review of the cat liver fluke Platynosomum fastosum Kossack, 1910 (Trematoda: Dicrocoeliidae). Vet Parasitol 2014; 200(1-2): 1-7. PMid:24412358. http://dx.doi.org/10.1016/j.vetpar.2013.12.016.
http://dx.doi.org/10.1016/j.vetpar.2013....
; BRAGA et al., 2016Braga RR, Teixeira AC, Oliveira JA, Cavalcanti LP. Prevalence of infection in free roaming cats in northeastern Brazil: fluke burden and grading of lesions. Platynosomum fastosumVet Parasitol 2016; 227: 20-25. PMid:27523932. http://dx.doi.org/10.1016/j.vetpar.2016.07.021.
http://dx.doi.org/10.1016/j.vetpar.2016....
). Milder injuries such as jaundice, parasites in the bile duct and gallbladder, and visualization of bile ducts on the hepatic surface were the abnormalities most commonly observed, while bile duct distension was the most remarkable lesion present in 61.1% of livers from infected animals. Despite marked jaundice is one the main macroscopic changes described in necropsy studies (FERREIRA et al., 1999Ferreira AMR, Almeida ECP, Labarthe NV. Liver fluke infection (Platynosomum concinnum) in Brazilian cats: prevalence and pathology. Feline Pract 1999; 27(2): 19-22.; HEADLEY et al., 2012Headley SA, Gillen MA, Sanches AW, Satti MZ. Platynosomum fastosum- induced chronic intrahepatic cholangitis and spp. infections in feral cats from Grand Cayman. SpirometraJ Helminthol 2012; 86(2): 209-214. PMid:21729387. http://dx.doi.org/10.1017/S0022149X11000265.
http://dx.doi.org/10.1017/S0022149X11000...
), Braga et al. (2016)Braga RR, Teixeira AC, Oliveira JA, Cavalcanti LP. Prevalence of infection in free roaming cats in northeastern Brazil: fluke burden and grading of lesions. Platynosomum fastosumVet Parasitol 2016; 227: 20-25. PMid:27523932. http://dx.doi.org/10.1016/j.vetpar.2016.07.021.
http://dx.doi.org/10.1016/j.vetpar.2016....
did not observed significant association of this symptom (mild jaundice) with prevalence of P. fastosum in free roaming domestic cats in northeastern Brazil.
The microscopic liver injuries described, ranging from mild to severe, are similar to commonly reported findings (IKEDE et al., 1971Ikede BO, Losos GJ, Isoun TT. infection in cats in Nigeria. Platynosomum concinnumVet Rec 1971; 89(24): 635-638. PMid:5150808. http://dx.doi.org/10.1136/vr.89.24.635.
http://dx.doi.org/10.1136/vr.89.24.635...
; RETNASABAPATHY & PRATHAP, 1971Retnasabapathy A, Prathap K. The liver-fluke Platynosomum fastosum in domestic cats. Vet Rec 1971; 88(3): 62-65. PMid:5100594. http://dx.doi.org/10.1136/vr.88.3.62.
http://dx.doi.org/10.1136/vr.88.3.62...
; FERREIRA et al., 1999Ferreira AMR, Almeida ECP, Labarthe NV. Liver fluke infection (Platynosomum concinnum) in Brazilian cats: prevalence and pathology. Feline Pract 1999; 27(2): 19-22.; HEADLEY et al., 2012Headley SA, Gillen MA, Sanches AW, Satti MZ. Platynosomum fastosum- induced chronic intrahepatic cholangitis and spp. infections in feral cats from Grand Cayman. SpirometraJ Helminthol 2012; 86(2): 209-214. PMid:21729387. http://dx.doi.org/10.1017/S0022149X11000265.
http://dx.doi.org/10.1017/S0022149X11000...
). Histopathological comparison is difficult, since stray cats used during this study had no known medical history, and possibly with natural infections which could be ongoing for different period of times. However, we can highlight that the periportal proliferation of the bile ducts and periportal fibrotic lesions observed in 94.4% of cat livers reveal chronic exposure to P. fastosum. Taylor & Perri (1977)Taylor D, Perri SF. Experimental infection of cats with the liver fluke Platynosomum concinnum.Am J Vet Res 1977; 38(1): 51-54. PMid:402094. noted extensive fibrous connective tissue in the bile ducts in the chronic stage (6 months after infection or beyond). Herein, we observed that naturally infected stray cats in an endemic region to platynosomiasis did not present severe pathological conditions such as cystic liver disease, severe cholestatic liver disease, cholangitis and cholangiohepatitis, cholangiocarcinoma, mesenteric lymphadenopathy, and hepatomegaly (O’SULLIVAN et al., 1976O’Sullivan BM, Rosenfeld LE, Green PE. Concurrent infection with Yersinia pseudotuberculosis and Platynosomum fastosum in a cat. Aust Vet J 1976; 52(5): 232-233. PMid:786240. http://dx.doi.org/10.1111/j.1751-0813.1976.tb00077.x.
http://dx.doi.org/10.1111/j.1751-0813.19...
; HANEY et al., 2006Haney DR, Christiansen JS, Toll J. Severe cholestatic liver disease secondary to liver fluke (Platynosomum concinnum) infection in three cats. J Am Anim Hosp Assoc 2006; 42(3): 234-237. PMid:16611937. http://dx.doi.org/10.5326/0420234.
http://dx.doi.org/10.5326/0420234...
; XAVIER et al., 2007Xavier FG, Morato GS, Righi DA, Maiorka PC, Spinosa HS. Cystic liver disease related to high Platynosomum fastosum infection in a domestic cat. J Feline Med Surg 2007; 9(1): 51-55. PMid:17241806. http://dx.doi.org/10.1016/j.jfms.2006.08.006.
http://dx.doi.org/10.1016/j.jfms.2006.08...
; CARREIRA et al., 2008Carreira VS, Vieira RF, Machado GF, Luvizotto MC. Feline cholangitis/cholangiohepatitis complex secondary to infection in a cat. Platynosomum fastosumRev Bras Parasitol Vet 2008;17(S1 Suppl 1): 184-187. PMid:20059845.; ANDRADE et al., 2012Andrade RL, Dantas AF, Pimentel LA, Galiza GJ, Carvalho FK, Costa VM, et al. induced cholangiocarcinomas in cats. Platynosomum fastosum-Vet Parasitol 2012; 190(1-2): 277-280. PMid:22963714. http://dx.doi.org/10.1016/j.vetpar.2012.04.015.
http://dx.doi.org/10.1016/j.vetpar.2012....
; BRAGA et al., 2016Braga RR, Teixeira AC, Oliveira JA, Cavalcanti LP. Prevalence of infection in free roaming cats in northeastern Brazil: fluke burden and grading of lesions. Platynosomum fastosumVet Parasitol 2016; 227: 20-25. PMid:27523932. http://dx.doi.org/10.1016/j.vetpar.2016.07.021.
http://dx.doi.org/10.1016/j.vetpar.2016....
). Morover, the intensity of parasitism was not related to the severity of macroscopic or microscopic hepatic injuries. An increase in serum ALT can be suggestive of infection by P. fastosum in endemic areas, where adult stray cats are chronically exposed; nonetheless, other liver diseases should be discarded.
Acknowledgements
Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for the financial support; to Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for the scholarship of R.C. Pacheco; Fundação de Amparo à Pesquisa do Estado de Mato Grosso (FAPEMAT).
-
Financial support: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Fundação de Amparo à Pesquisa do Estado de Mato Grosso (FAPEMAT).
References
- Allison RW. Laboratory evaluation of the liver. In: Thrall MA, Weiser G, Allison RW, Campbell TW. Veterinary Hematology and Clinical Chemistry. 2nd ed. New Jersey: Wiley-Blackwell; 2012. 346 p.
- American Veterinary Medical Association – AVMA. Report of the AVMA panel on Euthanasia. J Am Vet Med Assoc 2001; 218(5): 669-696. PMid:11280396. http://dx.doi.org/10.2460/javma.2001.218.669
» http://dx.doi.org/10.2460/javma.2001.218.669 - Andrade RL, Dantas AF, Pimentel LA, Galiza GJ, Carvalho FK, Costa VM, et al. induced cholangiocarcinomas in cats. Platynosomum fastosum-Vet Parasitol 2012; 190(1-2): 277-280. PMid:22963714. http://dx.doi.org/10.1016/j.vetpar.2012.04.015
» http://dx.doi.org/10.1016/j.vetpar.2012.04.015 - Ash LR. Helminth parasites of dogs and cats in Hawaii. J Parasitol 1962; 48(1): 63-65. PMid:13862798. http://dx.doi.org/10.2307/3275412
» http://dx.doi.org/10.2307/3275412 - Basu AK, Charles RA. A review of the cat liver fluke Platynosomum fastosum Kossack, 1910 (Trematoda: Dicrocoeliidae). Vet Parasitol 2014; 200(1-2): 1-7. PMid:24412358. http://dx.doi.org/10.1016/j.vetpar.2013.12.016
» http://dx.doi.org/10.1016/j.vetpar.2013.12.016 - Braga RR, Teixeira AC, Oliveira JA, Cavalcanti LP. Prevalence of infection in free roaming cats in northeastern Brazil: fluke burden and grading of lesions. Platynosomum fastosumVet Parasitol 2016; 227: 20-25. PMid:27523932. http://dx.doi.org/10.1016/j.vetpar.2016.07.021
» http://dx.doi.org/10.1016/j.vetpar.2016.07.021 - Bush AO, Lafferty KD, Lotz JM, Shostak AW. Parasitology meets ecology on its own terms: Margolis et al. revisited. J Parasitol 1997; 83(4): 575-583. PMid:9267395. http://dx.doi.org/10.2307/3284227
» http://dx.doi.org/10.2307/3284227 - Carreira VS, Vieira RF, Machado GF, Luvizotto MC. Feline cholangitis/cholangiohepatitis complex secondary to infection in a cat. Platynosomum fastosumRev Bras Parasitol Vet 2008;17(S1 Suppl 1): 184-187. PMid:20059845.
- Catcott EJ. Feline Medicine and Surgery (Flukes by Renaux, E.A.). Santa Barbara: American Veterinary Publication; 1964.
- Ferreira AMR, Almeida ECP, Labarthe NV. Liver fluke infection (Platynosomum concinnum) in Brazilian cats: prevalence and pathology. Feline Pract 1999; 27(2): 19-22.
- Foley RH. Platynosomum concinnum infection in cats. Compend Contin Educ Pract Vet 1994; 16(10): 1271-1277.
- Haney DR, Christiansen JS, Toll J. Severe cholestatic liver disease secondary to liver fluke (Platynosomum concinnum) infection in three cats. J Am Anim Hosp Assoc 2006; 42(3): 234-237. PMid:16611937. http://dx.doi.org/10.5326/0420234
» http://dx.doi.org/10.5326/0420234 - Headley SA, Gillen MA, Sanches AW, Satti MZ. Platynosomum fastosum- induced chronic intrahepatic cholangitis and spp. infections in feral cats from Grand Cayman. SpirometraJ Helminthol 2012; 86(2): 209-214. PMid:21729387. http://dx.doi.org/10.1017/S0022149X11000265
» http://dx.doi.org/10.1017/S0022149X11000265 - Ikede BO, Losos GJ, Isoun TT. infection in cats in Nigeria. Platynosomum concinnumVet Rec 1971; 89(24): 635-638. PMid:5150808. http://dx.doi.org/10.1136/vr.89.24.635
» http://dx.doi.org/10.1136/vr.89.24.635 - Jain NC. Essentials of veterinary hematology. Philadelphia: Lea & Febiger; 1993.
- Lenis C, Navarro F, Velez I. First case of platinosomosis from Colombia: Platynosomum illiciens (Digenea: Dicrocoeliidae) in , Turbo, Antioquia. Felis catusRev Colom Cienc Pecua 2009; 22(4): 659-663.
- Maldonado JF. The life history and biology of Kossak, 1910 (Trematoda, Dicrocoeliidae). Platynosomum fastosumPR J Public Health Trop Med 1945; 21(1): 17-39.
- O’Sullivan BM, Rosenfeld LE, Green PE. Concurrent infection with Yersinia pseudotuberculosis and Platynosomum fastosum in a cat. Aust Vet J 1976; 52(5): 232-233. PMid:786240. http://dx.doi.org/10.1111/j.1751-0813.1976.tb00077.x
» http://dx.doi.org/10.1111/j.1751-0813.1976.tb00077.x - Pinto HA, Mati VLT, Melo AL. New insights into the life cycle of (Trematoda: Dicrocoeliidae). PlatynosomumParasitol Res 2014; 113(7): 2701-2707. PMid:24802870. http://dx.doi.org/10.1007/s00436-014-3926-5
» http://dx.doi.org/10.1007/s00436-014-3926-5 - Prophet EB, Mills B, Arrington JB, Sobin LH. AFIP Laboratory Methods in Histotechnology. Washington, DC: Armed Force Registry of Pathology; 1992.
- R Development Core Team. R: a language and environment for statistical computing, reference index version 2.14.0. Vienna: R Foundation for Statistical Computing; 2011 [cited 2016 Oct 18]. Available from http://www.r-project.org
» http://www.r-project.org - Ramos DGS, Scheremeta RGAC, Oliveira ACS, Sinkoc AL, Pacheco RC. Survey of helminth parasites of cats from the metropolitan area of Cuiabá, Mato Grosso, Brazil. Rev Bras Parasitol Vet 2013; 22(2): 201-206. PMid:23856737. http://dx.doi.org/10.1590/S1984-29612013000200040
» http://dx.doi.org/10.1590/S1984-29612013000200040 - Retnasabapathy A, Prathap K. The liver-fluke Platynosomum fastosum in domestic cats. Vet Rec 1971; 88(3): 62-65. PMid:5100594. http://dx.doi.org/10.1136/vr.88.3.62
» http://dx.doi.org/10.1136/vr.88.3.62 - Rodriguez-Vivas RI, Williams JJ, Quijano-Novelo AG, Bolio GM, Torres-Acosta JF. Prevalence, abundance and risk factors of liver fluke (Platynosomum fastosum) infection in cats in Mexico. Vet Rec 2004; 154(22): 693-694. PMid:15200076. http://dx.doi.org/10.1136/vr.154.22.693
» http://dx.doi.org/10.1136/vr.154.22.693 - Salomão M, Souza-Dantas LM, Almeida FM, Branco AS, Bastos OPM, Sterman F, et al. Ultrasonography in hepatobiliary evaluation of domestic cats (Felis catus, L., 1758) infected by Looss, 1907. PlatynosomumIntern J Appl Res Vet Med 2005; 3(3): 271-279.
- Sharif M, Nasrolahei M, Ziapour SP, Gholami S, Ziaei H, Daryani A, et al. infections in stray cats in northern Iran. Toxocara catiJ Helminthol 2007; 81(1): 63-66. PMid:17381869. http://dx.doi.org/10.1017/S0022149X07214117
» http://dx.doi.org/10.1017/S0022149X07214117 - Spithill TW, Piedrafita D, Smooker PM. Immunological approaches for the control of fasciolosis. Int J Parasitol 1997; 27(10): 1221-1235. PMid:9394193. http://dx.doi.org/10.1016/S0020-7519(97)00120-3
» http://dx.doi.org/10.1016/S0020-7519(97)00120-3 - Taylor D, Perri SF. Experimental infection of cats with the liver fluke Platynosomum concinnum.Am J Vet Res 1977; 38(1): 51-54. PMid:402094.
- Xavier FG, Morato GS, Righi DA, Maiorka PC, Spinosa HS. Cystic liver disease related to high Platynosomum fastosum infection in a domestic cat. J Feline Med Surg 2007; 9(1): 51-55. PMid:17241806. http://dx.doi.org/10.1016/j.jfms.2006.08.006
» http://dx.doi.org/10.1016/j.jfms.2006.08.006
Publication Dates
-
Publication in this collection
16 Mar 2017 -
Date of issue
Jan-Mar 2017
History
-
Received
18 Oct 2016 -
Accepted
02 Feb 2017