Abstracts
INTRODUCTION: Sleep bruxism (SB) is defined as a stereotyped and periodic movement disorder, characterized by tooth grinding and/or clenching occurring during sleep, associated with rhythmic masticatory muscle activity. This condition isn't a disease, but when exacerbated may cause an unbalance and changing of orofacial structures. Thus, it is necessary to obtain effective and safe treatments for the control and management of the bruxist patient. The treatment alternatives ranges from oral devices to pharmacological and cognitive-behavioral techniques. OBJECTIVES: This study, through a systematic literature review, having as research bases MEDLINE, Cochrane, EMBASE, Pubmed, Lilacs and BBO, between the years of 1990 and 2008, with focus in randomized and quasi-randomized clinical trials, systematic reviews and meta-analysis, had as objective to analyze and discuss possibilities of treatment for sleep bruxism. RESULTS: According to the analysis of literature there are a lot of treatment options for the SB, but many of the therapies have no scientific support. Thus, the chosen therapy should be based on scientific evidences and in clinical common sense, to an improvement in quality of life of the bruxist patient.
Sleep bruxism; Treatment; Oral devices; Drugs; Behavior
INTRODUÇÃO: o bruxismo do sono (BS) é uma desordem de movimentos estereotipados e periódicos, associados ao ranger e/ou apertar de dentes durante o sono, decorrentes da contração rítmica dos músculos mastigatórios. Essa condição não é uma doença, porém quando exacerbada pode ocasionar desequilíbrio e alteração das estruturas orofaciais. Dessa forma, surge a necessidade de se obter terapêuticas efetivas e seguras para o controle e o manejo do paciente bruxômano. As alternativas de tratamento variam desde terapêuticas orodentais e farmacológicas até técnicas comportamentais-cognitivas. OBJETIVOS: através de uma revisão sistemática da literatura, tendo como bases de pesquisa a Medline, Cochrane, Embase, Pubmed, Lilacs e BBO, no período compreendido entre 1990 e 2008, e com enfoque em estudos clínicos randomizados e quasi-randomizados, revisões sistemáticas e meta-análises, esse trabalho teve como objetivo analisar e discutir métodos de tratamento para o BS. RESULTADOS: pela análise da literatura verifica-se que existe uma grande quantidade de opções terapêuticas para o BS, porém muitas das terapias não têm suporte científico que as sustente. Assim, a escolha terapêutica deve ser pautada em evidências científicas e no bom senso clínico, objetivando uma melhora na qualidade de vida do paciente bruxômano.
Bruxismo do sono; Tratamento; Aparelhos orais; Medicamentos; Comportamental
ORIGINAL ARTICLE
Sleep bruxism: Therapeutic possibilities based in evidences
Eduardo MachadoI; Patricia MachadoII; Paulo Afonso CunaliIII; Cibele Dal FabbroIV
ISpecialist in Temporomandibular Disorders (TMD) and Orofacial Pain, Federal University of Paraná (UFPR). Graduated in Dentistry, Federal University of Santa Maria (UFSM)
II Specialist in Prosthetic Dentistry, Pontifical Catholic University of Rio Grande do Sul (PUCRS). Graduated in Dentistry, UFSM
IIIPhD in Sciences, Federal University of São Paulo (UNIFESP). Professor of Graduate and Post-graduate Course in Dentistry, Federal University of Paraná (UFPR). Coordinator of the Specialization Course in TMD and Orofacial Pain, UFPR
IV PhD in Sciences, UNIFESP and specialist in TMD and Orofacial Pain, Federal Dental Council.
Contact address
ABSTRACT
INTRODUCTION: Sleep bruxism (SB) is defined as a stereotyped and periodic movement disorder, characterized by tooth grinding and/or clenching occurring during sleep, associated with rhythmic masticatory muscle activity. This condition isn't a disease, but when exacerbated may cause an unbalance and changing of orofacial structures. Thus, it is necessary to obtain effective and safe treatments for the control and management of the bruxist patient. The treatment alternatives range from oral devices, pharmacological therapies to cognitive-behavioral techniques.
OBJECTIVE: This study, a systematic literature review having as research bases MEDLINE, Cochrane, EMBASE, Pubmed, Lilacs and BBO, between the years of 1990 and 2008, with focus in randomized and quasi-randomized clinical trials, systematic reviews and meta-analysis, had as objective to analyze and discuss possibilities of treatment for sleep bruxism.
RESULTS: According to the literature analysis there is a lot of treatment options for the SB, but many of the therapies have no scientific support. Thus, the choice therapy should be based on scientific evidences and in clinical common sense, for an improvement in quality of life of the bruxist patient.
Keywords: Sleep bruxism. Treatment. Oral devices. Drugs. Behavior-cognitive.
INTRODUCTION
Sleep Bruxism (SB) is considered a movement disorder related to sleep.1 This parafunction is characterized by non-functional teeth contact, which can occur in a conscious or unconscious way, manifested by grinding or clenching of teeth. This condition is not a disease, but when exacerbated may cause a pathophysiological unbalance of the stomatognathic system. Several therapeutic modalities have been suggested, but there is no consensus on the most efficient.20
Due to its prevalence and injuries caused to the patients, the correct diagnosis shows great value to the development of appropriate treatment protocols, which include therapeutics using devices and oral therapies, pharmacological measures and cognitive-behavioral treatments (CBT). Thus, the objective of this systematic literature review is to discuss, based on scientific evidence, treatment alternatives for the control and management of SB.
MATERIAL AND METHODS
A computerized search in MEDLINE, Cochrane, EMBASE, PubMed, Lilacs and BBO was performed. The research descriptors used were "sleep bruxism", "treatment", "drugs", "medications" and "oral devices", which were crossed in search engines. The initial list of articles was submitted to review by two reviewers, who applied inclusion criteria to determine the final sample of articles.
Inclusion criteria for the selecting articles were:
» Articles published from January 1990 until July 2008.
» Within a context of an evidence-based Dentistry, only randomized clinical trials (RCTs) and quasi-randomized trials, systematic reviews and meta-analysis were included. Pilot studies were not included.
» Studies should include therapies for the treatment of SB involving orodental, pharmacological and/or cognitive-behavioral therapies.
» Studies written in English, Spanish or Portuguese.
RESULTS
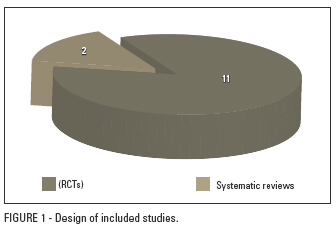
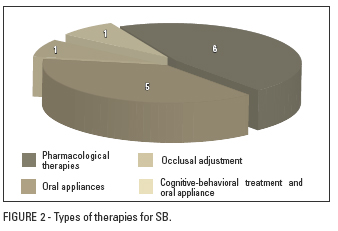
After applying the inclusion criteria 13 studies were selected and the Kappa index of agreement between reviewers was 1.00. Thus, these studies were grouped according to the therapeutic modalities: orodental, pharmacological or cognitive-behavioral (Figs 1 and 2).
Evidence-based Dentistry - Systematic Review
Orodental treatments: oral appliances and occlusal rehabilitations
In a systematic review, Tsukiyama et al21 evaluated the effects of occlusal adjustment as a treatment for bruxism, temporomandibular disorders (TMD), headaches and chronic cervical pain. Eleven studies met the inclusion criteria and three of these studies evaluated occlusal adjustment as a therapy for bruxism. The literature analysis concluded that there are no clinical studies showing that occlusal adjustment is superior to non-invasive therapies for the SB and TMD.
Dubé et al,2 in a controlled, double-blind and crossover RCT assessed the efficacy and safety of an occlusal splint and a palatal splint in the reduction of the muscle activity and teeth clenching in a sample of nine patients with SB. The patients, randomly, used an occlusal splint or a palatal splint for a period of two weeks, and then the treatments were swapped and the use was followed by another two weeks. The therapies were evaluated by polysomnographic examinations. The authors found that there was a statistically significant reduction in the number of episodes of SB with the use of both treatments, with no differences due to the design of the devices.
In a controlled, double-blind and parallel RCT, Van der Zaag et al22 compared the effects of occlusal and palatal splints in the management of SB. A sample of 21 patients were divided randomly between the occlusal splint (n = 11) and the palatal splint (n = 10) groups. In these individuals two polysomnographic evaluations were performed, one conducted before the beginning of therapy and another after a treatment period of four weeks. The study results showed that neither the occlusal splint, nor the palatal splint had an influence on the SB or in relation to patient sleep.
Harada et al,5 in a controlled and crossover RCT, compared the effects of a stabilization splint and a palatal splint in the management of SB. The sample consisted of 16 patients with bruxism who were divided randomly into two groups (n = 8) according to the splint used, and muscle activity was evaluated by an electromyographic portable device. After a period of use of the splint by six weeks, followed by two months without using any splint, the individuals were swapped between groups and started using the splint that had not yet been used for another six weeks. The results of this study showed that both the occlusal splint and the palatal splint reduced the masseter muscle activity during the night immediately after appliance installation. However, no effects were observed after 2, 4 and 6 weeks of use, and no differences were noted due to the splints designs.
Landry et al9 performed a RCT controlled and crossover comparing the effects of two therapies in the management of SB: in one patients received a mandibular advancement device (MAD), which involved two arches; and in the other therapy patients received a traditional occlusal splint. The sample consisted of 13 participants who underwent polysomnographic examination, with diagnosis of SB. Based on these results, the authors concluded that short-term temporary use of the MAD is associated with a notable reduction in motor activity of SB, and to a lesser order the occlusal splint also found a reduction of SB. However, the use of MAD in eight patients caused adverse effects, such as pain and discomfort.
In a systematic review published in Cochrane, Macedo et al,12 evaluated the effectiveness of occlusal splints as an alternative treatment for the SB. The authors conducted a computerized search, from 1966 to May 2007, including only randomized or quasi-randomized trials. The final sample of articles consisted of five RCTs. Occlusal splint therapy was compared to: palatal splint, mandibular advancement device, transcutaneous electrical neural stimulation (TENS) and no treatment. The authors concluded that there is not enough evidence to affirm that the occlusal splint is effective in the treatment of SB.
Pharmacological treatments
Etzel et al3 evaluated the effects of L-tryptophan on the SB in a double-blind RCT. Using a portable electromyography device, a sample of eight patients identified as nocturnal bruxists, received tryptophan (50 mg/kg) or placebo for 8 days, followed by further 8 days with the drugs inverted. Diet and alimentary habits were monitored during the experimental period. The study results showed no significant differences between therapies, suggesting that supplementation with L-tryptophan is ineffective in the treatment of SB.
In a double-blind randomized clinical trial, Mohamed et al13 evaluated 10 patients with SB, which received 25 mg of amitriptyline and 25 mg of placebo for one week each. The results showed that neither the intensity nor location of pain, and electromyographic activity of the masseter muscle were significantly affected by the tricyclic antidepressant therapy. Based on this study, low doses of amitriptyline are not recommended for the control of sleep bruxism, or for the discomforts associated with this sleep disorder.
In another double-blind RCT involving amitriptyline, Raigrodski et al17 assessed the effects of this antidepressant on nocturnal activity of the masseter muscle and in duration of sleep in patients with bruxism. The sample consisted of 10 women who received active treatment (amitriptyline 25 mg/night) and inactive (placebo, 25 mg/night) for a period of four weeks each. To assess the activity of masseter muscle a portable electromyography device was used. The results showed that administration of amitriptyline did not significantly decrease the activity of the masseter muscle, neither significantly increase sleep duration.
The role of the dopaminergic system in the SB was studied by Lobbezoo et al,11 in a controlled, double-blind and crossover RCT. A sample of 10 patients with SB received low doses of L-dopa associated with benserazide and was evaluated in a sleep laboratory. After the first night of adaptation, the second and third nights the patients received two doses (100 mg) of L-dopa or placebo, in a crossed design, with a dose one hour before bedtime and another four hours after the first. It was found that the use of L-dopa resulted in a decrease in the average number of bruxism episodes per hour of sleep, but this reduction proved to be modest, being only of the order of 26%.
Lavigne et al,10 in a controlled, double-blind and crossover RCT, evaluated the effects of bromocriptine on the SB. The study sample consisted of seven patients with SB, evaluated by polysomnography. These patients underwent two weeks of active treatment or placebo and then remained a week with no treatment, after the treatments were crossed in the sample. The doses of bromocriptine ranged from 1.25 mg to 7.5 mg (six days) up to 7.5 mg dose (8 days). Examining the results, bromocriptine did not reduce the frequency of episodes of bruxism during the night or the amplitude of contractions of the masseter muscle.
Assessing the effects of clonidine (0.3 mg) and propranolol (120 mg) on the SB, Huynh et al6 conducted a controlled, double-blind and crossover RCT comparing these drugs to placebo. A sample of 25 patients with a history and diagnosis of SB, was divided randomly into the groups, participating in this study and were monitored by polysomnographic examination. The results showed that propranolol (n = 10) did not affect the SB, whereas clonidine (n = 16) decreased sympathetic tone in the minute preceding the onset of SB, reducing the SB by preventing activation of the sequence of autonomic and motor events characteristics of the same. Hypotension was also observed in the morning in 19% of the studied patients.
A study not selected by the inclusion criteria, as it was not randomized, but with interesting findings, was of Saletu et al,18 in which a blind and controlled study investigated the acute effects of clonazepam on the SB. The sample consisted of 10 patients who received prior treatment with occlusal splint. Polysomnography and psychometry were used to evaluate the patients who received placebo or clonazepam. The administration of 1 mg of clonazepam significantly improved the index of SB and also the quality of sleep, with a good tolerability to drug.
Cognitive-behavioral treatments
Ommerborn et al15 conducted a RCT comparing the occlusal splint (n = 29) to a cognitive-behavioral therapy (CBT) (n = 28) in the management of the SB. The CBT consisted of measures such as problem solving, progressive muscle relaxation, nocturnal biofeedback and recreation training. Treatment for both groups lasted 12 weeks, and patients were examined pre and post-treatment and 6 months after conclusion of the study. The findings showed a significant reduction in activity of the SB in the two groups, but the effects were small. Moreover, the CBT group had a tendency to return to baseline of the study when compared to occlusal splint.
DISCUSSION
Considerations about the subject should always be performed through a critical reading of the methodology used by different authors. The use of the basic research principles allows the researchers to try to control as best as possible the biases of the study, generating higher levels of evidence. Thus, methodological criteria such as sample size calculation, randomization, blinding, control of involved factors and calibration intra and inter-examinators, become important tools to qualify the level of the generated scientific evidence.19
Within this context, of an evidence-based dentistry, it appears that the most common types of studies published in Brazilian journals correspond to studies of low potential for direct clinical application: in vitro studies (25%), narrative reviews (24%) and case reports (20%). The low number of studies with greater strength of evidence shows the necessity to increase knowledge of evidence-based methods among Brazilian researchers.14
According to the systematic literature review, it appears when evaluating therapeutic modalities for the control and management of the SB, that the selected studies presented in this article showed, for the most part, short samples and a short follow-up time. Thus, with small and unrepresentative samples, it is difficult to extrapolate the results to the general population. Moreover, many of the selected studies had a relatively short follow-up time, demonstrating the necessity for a larger longitudinal follow-up time to evaluate the real efficacy and safety of proposed treatments, whether orodental, pharmacological or cognitive-behavioral therapies. This becomes important because many drugs can cause tolerance and dependence effects in patients when used for long periods.
When analysing oral appliances as a treatment for the SB, it appears that there is no significant scientific evidences that the occlusal splint treats the SB, but benefits as the reduction in tooth wear are observed.12,22 Only two studies found a reduction in episodes of SB and in the masseter electromyographic condition with the use of splints, but one of these studies had a follow-up time of just two weeks, while the other only found an improvement immediately after installing the appliance, being that in subsequent evaluations improvements have not been observed.2,5 Still, when comparing the occlusal splint to palatal splint (without occlusal covering) there is similarity in results between the two treatment modalities.2,5
On the other hand, the mandibular advancement device, similar to appliances used for treatment of snoring and obstructive sleep apnea syndrome (OSAS), showed a greater reduction in episodes of SB when compared to occlusal splint. However, the exact mechanism that explains this reduction continues to be investigated. The hypotheses are focused on the size and configuration of the device, presence of pain, reduction in freedom of movement or change in upper airway patency.9
In patients with Sleep Bruxism the treatment option for minimally invasive and reversible therapies should be first choice in treatment protocols. Already the option for irreversible treatments, such as occlusal adjustment, have no scientific basis to support it, as there is no scientific evidence that occlusal adjustment treats or prevents Sleep Bruxism and TMD.8,21
Regarding to the pharmacological treatments, clonidine has a major role, but is associated with secondary adverse effects, demonstrating the necessity for further controlled RCTs with longer follow-up time to verify its real efficacy and safety.6 Thus, clonazepam becomes a safer alternative and with satisfactory results in the short term.7,18 It is important to mention here that the clonazepam, like other benzodiazepine drugs, may exacerbate OSAS. In other words, if the patient has a diagnosis of bruxism and OSAS, the clonazepam may be contraindicated. Another drug that also shows good results in the control and management of SB is L-dopa.11 In relation to amitriptyline, there is no scientific evidence to justify its use in patients with SB,13,17 same fact occurs with propranolol,6 tryptophan3 and bromocriptine.10
Target of many current studies in the Orofacial Pain investigations, due to its analgesic and antinociceptive properties, botulinum toxin has yet no RCTs analyzing its role in the treatment of SB. What is observed in the literature are studies evaluating botulinum toxin in situations associated with bruxism, such as muscle hyperactivity and myofascial pain,4 or studies without significant levels of evidence. In the future, with the performance of controlled RCTs, with representative samples and long follow-up time, botulinum toxin can be assessed as to its real effectiveness and safety for the treatment of SB.
Alternative cognitive-behavioral treatments may act in combination with other therapies, proceeding as an adjunct in the management of the SB. The awareness and patient education about their situation and the importance of changing habits that may be influencing and perpetuating their condition is important. Measures such as problem solving, muscle relaxation, nocturnal biofeedback, sleep hygiene and recreation, in other words, alternatives that reduce anxiety and stress, become tools for optimal results in situations of SB.15,16
CONCLUSIONS
» The occlusal splint seems to be an acceptable and safe treatment alternative in the short and medium terms, while the clonazepam, among pharmacological treatments, stood out as a therapeutic option in the short term, because in the long term it can cause dependence.
» The results of this systematic literature review seems to indicate that the mandibular advancement device and clonidine are the most promising experimental treatments for the SB, however both are associated with secondary adverse effects.
» There is need for further randomized clinical trials, based on representative samples and long follow-up time, to assess the effectiveness and safety of proposed treatments for the control and management of the SB.
» Cognitive-behavioral therapies such as psychotherapy, biofeedback, physical exercise and lifestyle changes, which are aimed at stress reduction, may be auxiliary in the treatment of SB.
» The SB continues to be a condition of complex etiology, associated with numerous treatments with often undefined prognosis. Thus, conservative treatments, minimally invasive and safe should be first choice, with the patient assisted by a multidisciplinary team, aiming at restoring quality of life.
References
-
1American Academy of Sleep Medicine. International Classification of Sleep Disorders. 2nd ed. Westchester: American Academy of Sleep Medicine; 2005.
- 2. Dubé C, Rompre PH, Manzini C, Guitard F, De Grandmont P, Lavigne GJ. Quantitative polygraphic controlled study on efficacy and safety of oral splint devices in tooth-grinding subjects. J Dent Res. 2004 May; 83(5):398-403.
- 3. Etzel KR, Stockstill JW, Rugh JD, Fisher JG. Tryptophan supplementation for nocturnal bruxism: report of negative results. J Craniomandib Disord. 1991 Spring;5(2):115-20.
- 4. Guarda-Nardini L, Manfredini D, Salamone M, Salmaso L, Tonello S, Ferronato G. Efficacy of botulinum toxin in treating myofascial pain in bruxers: a controlled placebo pilot study. Cranio. 2008 Apr;26(2):126-35.
- 5. Harada T, Ichiki R, Tsukiyama Y, Koyano K. The effect of oral splint devices on sleep bruxism: a 6-week observation with an ambulatory electromyographic recording device. J Oral Rehabil. 2006 Jul;33(7):482-8.
- 6. Huynh N, Lavigne GJ, Lanfranchi PA, Montplaisir JY, Champlain J. The effect of 2 sympatholytic medications-propranolol and clonidine-on sleep bruxism: experimental randomized controlled studies. Sleep. 2006 Mar 1;29(3):307-16.
- 7. Huynh NT, Rompré PH, Montplaisir JY, Manzini C, Okura K, Lavigne GJ. Comparison of various treatments for sleep bruxism using determinants of number needed to treat and effect size. Int J Prosthodont. 2006 Sep-Oct;19(5):435-41.
- 8. Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular disorders: Cochrane Review. In: The Cochrane Library; 2007. Oxford: Update Software; 2007. Issue 4.
- 9. Landry ML, Rompré PH, Manzini C, Guitard F, Grandmont P, Lavigne GJ. Reduction of sleep bruxism using a mandibular advancement device: an experimental controlled study. Int J Prosthodont. 2006 Nov-Dec;19(6):549-56.
- 10. Lavigne GJ, Soucy JP, Lobbezoo F, Manzini C, Blanchet PJ, Montplaisir JY. Double-blind, crossover, placebo-controlled trial of bromocriptine in patients with sleep bruxism. Clin Neuropharmacol. 2001 May-Jun;24(3):145-9.
- 11. Lobbezoo F, Lavigne GJ, Tanguay R, Montplaisir JY. The effect of catecholamine precursor L-dopa on sleep bruxism: a controlled clinical trial. Mov Disord. 1997 Jan;12(1):73-8.
- 12. Macedo CR, Silva AB, Machado MA, Saconato H, Prado GF. Occlusal splints for treating sleep bruxism (tooth grinding): Cochrane Review. In: The Cochrane Library. Oxford: Update Software; 2007. Issue 4.
- 13. Mohamed SE, Christensen LV, Penchas J. A randomized double-blind clinical trial of the effect of amitriptyline on nocturnal masseteric motor activity (sleep bruxism). Cranio. 1997 Oct;15(4):326-32.
- 14. Oliveira GJ, Oliveira ES, Leles CR. Tipos de delineamento de pesquisa de estudos publicados em periódicos odontológicos brasileiros. Rev Odonto Ciênc. 2007 jan-mar;22(55):42-7.
- 15. Ommerborn MA, Schneider C, Giraki M, Schäfer R, Handschel J, Franz M, et al. Effects of an occlusal splint compared with cognitive-behavioral treatment on sleep bruxism activity. Eur J Oral Sci. 2007 Feb;115(1):7-14.
- 16. Pereira RPA, Negreiros WA, Scarparo HC, Pigozzo MN, Consani RLX, Mesquita MF. Bruxismo e qualidade de vida. Rev Odonto Ciênc. 2006 abr-jun;21(52):185-90.
- 17. Raigrodski AJ, Christensen LV, Mohamed SE, Gardiner DM. The effect of four-week administration of amitriptyline on sleep bruxism. A double-blind crossover clinical study. Cranio. 2001 Jan;19(1):21-5.
- 18. Saletu A, Parapatics S, Saletu B, Anderer P, Prause W, Putz H, et al. On the pharmacotherapy of sleep bruxism: placebo-controlled polysomnographic and psychometric studies with clonazepam. Neuropsychobiology. 2005;51(4):214-25.
- 19. Susin C, Rosing CK. Praticando odontologia baseada em evidências. 1Ş ed. Canoas: ULBRA; 1999.
- 20. Tan EK, Jankovic J. Treating severe bruxism with botulinum toxin. J Am Dent Assoc. 2000 Feb;131(2):211-6.
- 21. Tsukiyama Y, Baba K, Clark GT. An evidence-based assessment of occlusal adjustment as a treatment for temporomandibular disorders. J Prosthet Dent. 2001 Jul;86(1):57-66.
- 22. Van der Zaag J, Lobbezoo F, Wicks DJ, Visscher CM, Hamburger HL, Naeije M. Controlled assessment of the efficacy of occlusal stabilization splints on sleep bruxism. J Orofac Pain. 2005 Spring;19(2):151-8.
Endereço para correspondência
Publication Dates
-
Publication in this collection
18 July 2011 -
Date of issue
Apr 2011
History
-
Accepted
Mar 2009 -
Received
Aug 2008