Abstracts
PURPOSE: To analyze the otoacoustic emissions (OAE) of the newborn hearing screening of infants born to HIV-seropositive mothers. METHODS: It was carried out the Transient-Evoked OAE and the research of cochleopalpebral reflex in 247 full-term newborns with no risk factors for hearing. The Control Group (CG) comprised 167 infants, and the Research Group (RG), 80 infants that had been exposed to HIV during gestation. It was considered "failure" when the newborn had absence of TOAE in at least one ear. Data were statistically analyzed. RESULTS: In the, Eight infants (10%) from the Research Group and seven (4.2%) from the Control Group failed in the newborn hearing screening (p=0.09). Retest of the infants who failed showed persistence of the absence of OAE in one subject (12.5%) from the Research Group and two (28.6%) from the Control Group (p=0.6). Cochleopalpebral reflex was present in all subjects. CONCLUSION: There was no association between the absence of TOAE and the newborn's HIV exposure during gestation.
Ear, inner; Neonatal screening; HIV seropositivity; Hearing; Hearing disorders; HIV infections
OBJETIVO: Analisar as emissões otoacústicas de crianças nascidas de mães soropositivas para o HIV na triagem auditiva neonatal. MÉTODOS: Realizou-se a pesquisa das Emissões Otoacústicas Evocadas por Transiente (EOAT) e do reflexo cócleo-palpebral (RCP) em 247 neonatos, todos nascidos a termo e sem fatores de risco para a audição. O Grupo Controle (GC) foi composto por 167 neonatos e o Grupo Pesquisa (GP) por 80 neonatos expostos ao HIV durante a gestação. Considerou-se "falha" quando o neonato apresentava ausência de EOAT em pelo menos uma das orelhas. Os dados foram analisados estatisticamente. RESULTADOS: No Grupo Pesquisa, oito (10%) neonatos falharam na triagem auditiva neonatal e no Grupo Controle este número foi de sete (4,2%) (p=0,09). No reteste dos neonatos que falharam, houve a persistência da ausência das emissões otoacústicas em um neonato do Grupo Pesquisa (12,5%) e em dois neonatos (28,6%) do Grupo Controle (p=0,6). Em todos os neonatos houve a presença do RCP. CONCLUSÃO: Não houve associação entre ausência de EOA por transiente e a exposição do neonato ao HIV durante a gestação.
Orelha interna; Triagem neonatal; Soropositividade para HIV; Audição; Transtornos da audição; Infecções por HIV
ORIGINAL ARTICLE ARTIGO ORIGINAL
Alessandra Kerli da Silva ManfrediI; Patrícia Aparecida ZuanettiI; Fabíola MishimaII; Raphaela Barroso Guedes GranzottiIII
ISpeech-Language Pathology and Audiology Sector, Department of Otorhinolaryngology, Ophthalmology, and Head and Neck Surgery, School of Medicine of Ribeirão Preto, Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil
IIGraduate Program (Masters degree), Department of Otorhinolaryngology, Ophthalmology, and Head and Neck Surgery, School of Medicine of Ribeirão Preto, Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil
IIIRehabilitation Center of the University Hospital of Ribeirão Preto, Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil
Correspondence address
ABSTRACT
PURPOSE: To analyze the otoacoustic emissions (OAE) of the newborn hearing screening of infants born to HIV-seropositive mothers.
METHODS: It was carried out the Transient-Evoked OAE and the research of cochleopalpebral reflex in 247 full-term newborns with no risk factors for hearing. The Control Group (CG) comprised 167 infants, and the Research Group (RG), 80 infants that had been exposed to HIV during gestation. It was considered "failure" when the newborn had absence of TOAE in at least one ear. Data were statistically analyzed.
RESULTS: In the, Eight infants (10%) from the Research Group and seven (4.2%) from the Control Group failed in the newborn hearing screening (p=0.09). Retest of the infants who failed showed persistence of the absence of OAE in one subject (12.5%) from the Research Group and two (28.6%) from the Control Group (p=0.6). Cochleopalpebral reflex was present in all subjects.
CONCLUSION: There was no association between the absence of TOAE and the newborn's HIV exposure during gestation.
Keywords: Ear, inner; Neonatal screening; HIV seropositivity; Hearing; Hearing disorders; HIV infections
RESUMO
OBJETIVO: Analisar as emissões otoacústicas de crianças nascidas de mães soropositivas para o HIV na triagem auditiva neonatal.
MÉTODOS: Realizou-se a pesquisa das Emissões Otoacústicas Evocadas por Transiente (EOAT) e do reflexo cócleo-palpebral (RCP) em 247 neonatos, todos nascidos a termo e sem fatores de risco para a audição. O Grupo Controle (GC) foi composto por 167 neonatos e o Grupo Pesquisa (GP) por 80 neonatos expostos ao HIV durante a gestação. Considerou-se "falha" quando o neonato apresentava ausência de EOAT em pelo menos uma das orelhas. Os dados foram analisados estatisticamente.
RESULTADOS: No Grupo Pesquisa, oito (10%) neonatos falharam na triagem auditiva neonatal e no Grupo Controle este número foi de sete (4,2%) (p=0,09). No reteste dos neonatos que falharam, houve a persistência da ausência das emissões otoacústicas em um neonato do Grupo Pesquisa (12,5%) e em dois neonatos (28,6%) do Grupo Controle (p=0,6). Em todos os neonatos houve a presença do RCP.
CONCLUSÃO: Não houve associação entre ausência de EOA por transiente e a exposição do neonato ao HIV durante a gestação.
Descritores: Orelha interna; Triagem neonatal; Soropositividade para HIV; Audição; Transtornos da audição; Infecções por HIV
INTRODUCTION
The Acquired Immunodeficiency Syndrome (AIDS) is a chronic infectious disease. The first case was reported in 1981 by the Centers for Disease Control and Prevention (CDC) as an unexplained immunodeficiency characterized by the occurrence of opportunistic infections, and having the human immunodeficiency virus (HIV) as its etiologic agent(1).
At first, AIDS became known as the "gay plague" because it mainly affected a specific group of persons denoted "risk group" consisting of homosexual men, hemophiliacs and injecting drug users(2). Starting in the 1990 decade, it was possible to observe a "feminization" of the epidemic, i.e., a considerable increase of HIV-infected women, more than 80% of them in reproductive age.
Three million women give birth in Brazil every year. Estimates obtained in a 2006 study have pointed out a 0.42% prevalence of HIV infection among pregnant women, corresponding to approximately 13,000 women(3). In 2008, there were 33.4 million people living with HIV in the world, 2.1 million of them being children. In Brazil, 13,728 cases of HIV-infected children were notified from 1980 to June 2008, 84.5% of them infected by vertical transmission(4).
Among the forms of HIV contagion in children, vertical transmission from mother to child is the principal one, which may occur at three different times: during the intrauterine period through the maternal circulation, during delivery due to aspiration of blood or other secretion, and during the postpartum period due to breast-feeding. In most cases (65%), contagion occurs at the time of delivery and in the remaining ones (35%) transmission occurs during intrauterine life and during breast-feeding(3).
The clinical findings of HIV-infected children are nonspecific, with the clinical course of AIDS being more aggressive in this population, with a shorter latency period between infection and the onset of symptoms compared to adults (5).
The action of HIV in the organism of a child ranges from a decrease in immunity due to the destruction of CD4 cells, which makes an individual susceptible to opportunistic infection, to neurological alterations caused by the neurotropism of HIV in a developing brain(6). The most common neurological alterations are retarded neuropsychomotor development, delayed language acquisition, mental deficiency, hyporeflexia, and pyramidal syndrome(7). The incidence of these disorders ranges from 30% to 90% in pediatric patients, considering age, intensity and immunological involvement as important factors. Impairment of the motor, cognitive and behavioral levels varies according to brain maturation and time of onset of the neurological disease(8).
Among the many infections that can attack children with AIDS, those involving the upper airways, mainly sinusitis, otitis externa and otitis media, are responsible for the high incidence of conductive hearing deficits. Moreover, in these children hearing impairment may be related to other factors, among them the use of ototoxic medications and the damaging action of the virus itself on peripheral and central nervous structures. Thus, AIDS can be considered a risk factor for both peripheral and central hearing alterations(9,10).
An early diagnosis is highly desirable since the occurrence of hearing deficiency in the first few years of life may cause important functional damage to the development of the child. The first years of life correspond to the period of greatest plasticity of the central nervous system (CNS), whose early stimulation promotes a better rehabilitation. Thus, hearing screening is to be recommended for all newborns whether or not they present risks of deafness, using an objective technique as the method of evaluation(11-13).
Transient-evoked otoacoustic emissions (TEOAE) represent a noninvasive and rapid procedure applicable at sites with no acoustic treatment, objective, and sensitive to hearing losses of mild to profound degree (uni- or bilateral). At present TEOAE correspond to the technique most indicated for hearing screening programs in populations at low risk for deafness(14).
Considering the risk of hearing losses in HIV-infected children, the current literature reports about intrauterine exposure and the changes these children may present in neurological exams and regarding neuropsychomotor development during the first years of life(7,15), the objective of the present study was to analyze the TEOAE of children born to HIV-seropositive mothers obtained as part of a newborn hearing screening (NHS) program, and to determine the association between hearing alterations and HIV exposure.
METHODS
The project was approved by the Research Ethics Committee of the University Hospital of Ribeirão Preto, Universdade de São Paulo (HCRP-USP), protocol no. 9107/2008. This was a retrospective study in which the authors analyzed the medical records of all neonates born to HIV-seropositive mothers between January 2005 and March 2010, and of all neonates with no hearing risk and not exposed to HIV born during the year of 2010 in the maternity of a University Hospital.
The neonates were divided into two groups as follows:
- Research Group (RG): composed of 80 neonates (42 girls and 38 boys) born to HIV-seropositive mothers, who participated in the NHS program, born at term and with no risk factor for hearing according to the Joint Committee on Infant Hearing(11).
- Control Group (CG): composed of 167 neonates (89 girls and 78 boys) born in 2010 who participated in the NHS program, born at term and with no risk factor for hearing according to the Joint Committee on Infant Hearing(11).
The procedure adopted for NHS was the TEOAE test and the determination of the cochleopalpebral reflex (CPR). A portable Madsen® AccuScreen instrument was used for hearing screening.
The protocol included the following procedures:
1) The stimulus used was the nonlinear click at the intensity of 70 dBNPS, presented individually and separately to each ear. The frequencies from 1.4 to 4 kHz were tested.
2) The stability of the probe and the level of noise of the exam were checked on the dial of the equipment, where "A" (value of rejection of the artifact) and "S" (value of stability of the stimulus) should indicate less than 20% and more than 80%, respectively.
3) PASS was the expected result (intact cochlear function) which indicated that the limits of "A" and "S" had not been exceeded.
4) The agogo musical instrument with a large bell stimulus elicited at approximately 100 dBNPS was used for the behavioral evaluation of the cochleopalpebral reflex.
NHS was performed in a cabin with acoustic treatment in the Speech-Language Pathology and Audiology Sector. All neonates were evaluated during the first 28 days of life. At the time of the exam, they lay on their mother's or caregiver's lap, preferentially in the postprandial condition. The absence of TEOAE in one or both ears was considered to be a failure of NHS and the neonate was scheduled for a retest within approximately 15 days. When failure persisted at retest, the neonate was referred for audiologic diagnosis.
Neonates who had not been exposed to HIV, premature babies and babies who, in addition to having been exposed to the virus presented any other of the established risks for hearing, were excluded from the RG. Premature babies and those having any risk factor were excluded from the CG(11).
We analyzed 92 medical records of neonates born to HIV-seropositive mothers, but 12 neonates were excluded because they were preterm or presented some risks for hearing loss according to pre-established criteria(11), with 80 neonates being left in the study.
The first TEOAE exam was performed, on average, on the 18th day of life both in RG and C G neonates, since in our institution NHS is performed in an ambulatory service. The TEOAE retest was applied, on average, on the 36th day.
The data obtained were analyzed in a descriptive manner and statistical comparisons were performed using the Fisher exact test, with the level of significance set at de 0.05.
RESULTS
Of the 80 neonates exposed to HIV in utero, eight (10%) did not present TEOAE responses. Seven of the 167 CG neonates (4.2%) did not present TEOAE responses. There was no difference in number of neonates who failed NHS between RG and CG (Figure 1).
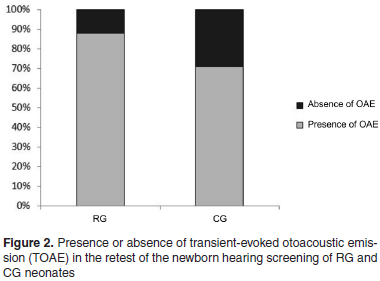
In the retest of RG neonates, only one (12.5%) failed again and was referred for audiologic diagnosis according to the protocol of the service. Two GC neonates (28.6%) failed the retest and were referred for audiologic analysis. No differences were observed between the two groups (Figure 2).
All neonates studied presented a cochleopalpebral reflex, including those who failed the TEOAE test. Regarding the neonates of both groups who were referred for diagnosis after failing the retest, no hearing loss was detected in any case.
DISCUSSION
NHS involves behavioral and electrophysiological procedures for the early identification of hearing deficiency. If the screening is performed only in infants with indicators of risk of hearing deficiency, the condition will be identified in only 50% of cases. For this reason, universal screening is recommended(11,12).
Programs of Universal Newborn Hearing Screening (UNHS) have been implemented since 1994, proposing that all babies be evaluated by three months of age and that intervention be started before six months of age in cases of a diagnosis of deafness(11-13). UNHS is not yet a reality throughout Brazil, with only 20% of low-risk babies and 80% of high-risk babies being screened in some places(14).
The incidence of bilateral hearing loss is estimated at three for every 1,000 births among healthy newborns and at about 2 to 4% among newborns from Intensive Care Units(12). In Brazilian studies, the confirmation of hearing loss in babies ranges from 0.3 to 1.8% of the infants screened, while the rate of adequate responses to NHS in both ears (test or retest) is 90%to 98%among no-risk newborns(16,17), in agreement with the data of the present study.
The time when cochlear function starts is variables, possibly occurring early during intrauterine life, or later, after birth. In addition, knowledge about the active processes that occur in the cochlea and culminate with the transduction of the mechanical signal to the electrical one have also led to the understanding that these processes are not fully developed at the beginning of cochlear activity. Maturation occurs slowly over a period of a few weeks after the beginning of the functioning of the inner ear, with the development of the contractile capacity of outer hair cells (OHCs), the adjustment of the tune curves of spiral ganglion neurons and of cochlear neurons, and the development of otoacoustic emissions(18).
We cannot rule out the possibility that the reasons for the lack of responses in the first test observed in the present study may have been related to difficulties in the sealing of the external acoustic meatus or to the presence of vernix caseosa in the conduit. However, we should consider the question of hearing maturity and we should suspect that this initial lack of responses may have also been the result of immaturity of the contractile capacity of the OHCs. Thus, in the TEOAE retest performed about 15 days after the first test, the responses were present.
Various studies have already investigated the direct and indirect effects of HIV on the central nervous system of vertically infected children and have reported important manifestations such as delayed neuropsychomotor development, delayed language acquisition, and cognitive changes. However, we already know that the effects of HIV on neurodevelopment go beyond a direct action of the virus on the central nervous system due to the viral neurotropism for neuronal cells(7,8,19,20.22).
It should be pointed out that that there are additional factors related to AIDS that may interfere with neurodevelopment, such as maternal factors (stage of maternal disease, opportunistic infections related to AIDS, nutritional status, and use of drugs and alcohol), intrauterine factors (prematurity, neonatal anoxia, intrauterine malnutrition, congenital and perinatal infections), and environmental factors (precarious socioeconomic condition, family disorders, being an orphan, and frequent hospitalizations)(7,8,19-22).
On this basis, the pediatric consensus of the Health Ministry recommends that all babies born to HIV-infected mothers should be attended in specialized units at least until the definition of their diagnosis. Those found to be infected should continue to be monitored in these units, while those who are not infected can be referred for follow-up at basic health units. The committee recommends that even non-infected children should be followed up periodically until the end of adolescence, not only because they were exposed to HIV, but also because, during intrauterine life and the first months of life, they were exposed to antiretroviral drugs whose possible effects on the central nervous system and consequently on childhood neurodevelopment are still unknown(23-26).
The newborns exposed to HIV during intrauterine life do not necessary acquire the virus and develop the disease. In the absence of any intervention, vertical HIV transmission reaches a frequency of 25 to 30%. With the institution of prophylactic measures aiming at the reduction of vertical transmission (universal offer of the anti-HIV test with pre- and post-test counseling, administration of antiretroviral medicine to pregnant women and to their newborns during the first six weeks of life, replacement of breast-feeding and choice of the route of delivery) it is possible to reach rates as low as 1.0 to 2.0%(27).
Taking into consideration the rate of vertical transmission, we may assume that, among the children evaluated in the present study, a reduced number will really be infected with HIV, a fact that may explain the absence of an association between NHS changes in the RG. However, it is important to mention that even children with a confirmed diagnosis of HIV seropositivity may present adequate responses to NHS since the action of the virus and of antiretroviral drugs on the auditory pathways does not occur immediately after infections.
HCRP-USP provides audiologic follow-up regardless of NHS result until the diagnosis is confirmed, a fact that occurs at about 18 months of age. If the child is not HIV infected and does not present any other risk factor for hearing loss, he is discharged from the Speech-Language Pathology and Audiology Sector. If HIV seropositivity is confirmed, the child continues to be submitted to periodic audiologic exams. This is done because it is common to identify conductive hearing loss due to changes in the ears(28-30) and sensorineural hearing loss due to the direct action of the virus or of antirretroviral drugs(8,9). In addition, changes in the hearing process are common, with some authors suggesting that HIV infection should be considered as a risk factor for hearing changes(30).
The introduction of antiretroviral therapy for the treatment of AIDS is causing an increasingly larger number of children and adolescents to live with the disease and with quality of life. On this basis, the epidemic is posing new challenges: with the use of antiretrovirals since birth, what will be the consequences for hearing function when these children reach adult age? And when they are vertically infected?
In view of the above data, we emphasize that treatment of children with AIDS should be performed by an interdisciplinary team so that all aspects involving HIV-infected infants may be considered. The prognosis regarding the quality of life of these children depends on a clear understanding of the disease on the part of the whole team and on frequent updates, demonstrating the importance of a larger number of studies in all professional areas involved in the care for this population.
CONCLUSION
We observed no association between HIV exposure during pregnancy and the absence of otoacoustic emissions. Neonates born to HIV-seropositive mothers did not present changes in cochlear function. We recommend an audiologic follow-up of these children until at least the time of confirmation of the diagnosis since HIV-infected children present various factors that predispose them to alterations of the central and peripheral auditory system.
REFERENCES
- 1. Barré-Sinoussi F, Chermann JC, Rey F, Nugeyre MT, Chamaret S, Gruest J, et al. Isolation of a T-Iymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science. 1983;220(4599):868-71.
- 2. Aoki FH. Síndrome da imunodeficiência adquirida: epidemia e evolução do tratamento. In: Colombrini MR, Figueredo RM, Paiva MC. Leito-dia em AIDS: experiência multiprofissional na assistência dos doentes. São Paulo: Atheneu; 2001. p.1-12.
- 3. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Programa Nacional de DST e AIDS. Critérios de definição de casos de AIDS em adultos e crianças. Brasília (DF): Ministério da Saúde; 2003. [Manuais, 60]
- 4. Joint United Nations Programme on HIV/AIDS - UNAIDS. Situação da epidemia de AIDS 2009 [Internet]. [citado 2008 Nov 30]. Disponível em: (http://www.onu-brasil.org.br/agencias_unAIDS.php).
- 5. Sculerati N, Borkowsky W. Pediatric human immunodeficiency virus infection: an otolaryngologist's perspective. J Otolaryngol. 1990;19(3):182-8.
- 6. Tardieu M, Le Chenadec J, Persoz A, Meyer L, Blanche S, Mayaux MJ. HIV-1 related encephalopathy in infants compared with children and adults. Neurology. 2000;54(5):1089-95.
- 7. Rocha C, Golvêa A, Machado D, Cunegundes K, Beltrão S, Boloni F, Succi RC. Manifestações neurológicas em crianças e adolescentes infectados e expostos ao HIV-1. Arq Neuropsiquiatr. 2005;63(3B):828-31.
- 8. Belman AL. Acquirid immunodeficiency syndrome and child's central nervous system. Pediatr Clin North Am. 1992;39(4):691-714.
- 9. Madriz JJ, Herrera G. Human immunodeficiency virus and acquired immune deficiency syndrome AIDS-related hearing disorders. J Am Acad Audiol. 1995;6(5):358-64.
- 10. Kozlowski LC. Perfil audiológico de um grupo de crianças HIV positivas. Acta ORL. 2006;24(4):277-80.
- 11. American Academy of Pediatrics. Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hering detection and intervention programs. Pediatrics. 2007;120(4):898-921.
-
12Comitê Brasileiro de Perda Auditivas na Infância (CBPAI) - 1ª recomendação (Período neonatal). Recomendação 01/99. Jornal do CFFª. 2000;(5):3-7.
- 13. Yoshinaga-Itano C, Sedey AL. Language, speech and social-emotional development of children who are deaf or hard of hearing: the early years. The Volta Review. 2000;100(5):1-236.
- 14. Durante AS, Carvallo RM, Costa FS, Soares JC. Características das emissões otoacústicas por transientes em programa de triagem auditiva neonatal. Pró-Fono. 2005;17(2):133-40.
- 15. Williams PL, Marino M, Malee K, Brogly S, Hughes MD, Mofenson LM, et al. Neurodevelopment and in utero antiretroviral exposure of HIV-exposed uninfected infants. Pediatrics. 2010;125(2):e250-60.
- 16. Freitas VS, Alvarenga KF, Bevilacqua MC, Martinez MA, Costa OA. Análise crítica de três protocolos de triagem auditiva neonatal. Pró-Fono. 2009;21(3):201-6.
- 17. Hilú MR, Zeigelboim BS. O conhecimento, a valorização da triagem auditiva neonatal e a intervenção precoce da perda auditiva. Rev CEFAC. 2007;9(4):563-70.
- 18. Dum N. Postnatal development of the auditory evoked brainstem potentials in the guinea pig. Acta Otolaryngol. 1984;97(1-2):63-8.
- 19. Guedes RB. Estudo dos aspectos fonológicos e lexicais da linguagem em crianças com idade entre 3 a 7 anos portadores de HIV [dissertação]. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo; 2007.
- 20. Van Rie A, Harrington PR, Dow A, Robertson K. Neurologic and neurodevelopmental manifestations of pediatric HIV/AIDS: a global perspective. Eur J Pediatr Neurol. 2007;11(1):1-9.
- 21. Steele RG, Nelson TD, Cole BP. Psychosocial functioning of children with HIV infection: review of the literature from a socioecological framework. J Dev Behav Pediatr. 2007;28(1):58-69.
- 22. Dobrova-Krol NA, van IJzendoorn MH, Bakermans-Kranenburg MJ, Juffer F. Effects of perinatal HIV infection and early institutional rearing on physical and cognitive development of children in Ukraine. Child Dev. 2010;81(1):237-51.
- 23. Brasil. Ministério da saúde. Secretaria de Vigilância em Saúde. Programa Nacional de DST e AIDS. Guia de tratamento clínico da infecção pelo HIV em crianças. 3a ed. Brasília: Ministério da Saúde; 2006. [Série Manuais, 18]
- 24. Oleske JM. When should we treat children with HIV? J Pediatr (Rio J). 2006;82(4):243-5.
- 25. Resino S, Resino R, Micheloud D, Gurbindo Gutiérrez D, Leon JA, Ramos JT, et al. Long-term effects of highly active antiretroviral therapy in pretreated, vertically HIV type1-infected children: 6 years of follow-up. Clin Infect Dis. 2006;42(6):862-9.
- 26. Shanbhag MC, Rutstein RM, Zaoutis T, Zhao H, Chao D, Radcliffe J. Neurocognitive functioning in pediatric human immunodeficiency virus infection: effects of combined therapy. Arch Pediatr Adolesc Med. 2005;159(7):651-6.
- 27. World Health Organization. Antiretroviral therapy of HIV infection in infants and children in resource-limited settings: towards universal access. Recommendations for a public health approach. Geneva: WHO; 2006.
- 28. Bankaitis AE, Keith RW. Audiological changes associated with HIV infection. Ear NoseThroat J. 1995;74(5):353-9.
- 29. Matas CG, Leite RA, Magliaro FC. Avaliação audiológica e eletrofisiológica em crianças portadoras da síndrome da imunodeficiência adquirida. Acta ORL. 2005;23(4):160-4.
- 30. Matas CG, Iorio MC, Succi RC. Auditory disorders and acquisition of the ability to çocalize sound in children born to HIV-positive mothers. Brazi J Infect Dis. 2008;12(1):10-4.
Newborn hearing screening in infants born to HIV-seropositive mothers
Publication Dates
-
Publication in this collection
09 Feb 2012 -
Date of issue
Dec 2011
History
-
Accepted
24 Aug 2011 -
Received
27 Mar 2011