Abstracts
OBJECTIVE: The purpose of this study is to demonstrate the current picture of colorectal cancer in a public hospital of Rio Grande do Sul, focusing on aspects related to diagnosis, staging and surgical therapy addressed in these patients. METHODS: A descriptive and retrospective study that includes patients with colorectal cancer admitted to the Proctology Service of the Hospital Nossa Senhora da Conceição de Porto Alegre, from January 2009 to May 2011. RESULTS: This study investigated 61 patients, 65.6% were female. Their age ranged from 40 to 84 years. Colonoscopy was performed in 58 patients; 56.9% of them had over 50% impaired colon lumen. The carcinoembryonic antigen (CEA) was collected from 59 patients, 47.5% had CEA>5 ng/mL. Distant metastases were found in 23.3% of total 60 patients. Underwent surgical treatment 58 patients, of a curative intent was 84.5%. The presence of more than 12 lymph nodes per specimen was 73.1%. All 61 patients were classified as: Stage I (9.8%), Stage II (29.5%), Stage III (29.5%) and Stage IV (31.1%). CONCLUSION: The profile of the patients treated at our institution indicates disease in advanced stage; however, the methods employed have provided a curative surgical treatment in our oncology patients.
colorectal neoplasms; colorectal surgery; Unified Health System
OBJETIVO: O objetivo do presente estudo é demonstrar o panorama atual do câncer colorretal em um hospital público da capital do Rio Grande do Sul, enfocando aspectos relacionados ao diagnóstico, estadiamento e terapêutica cirúrgica abordada nesses respectivos pacientes. MÉTODOS: Estudo descritivo e retrospectivo que inclui os pacientes com câncer colorretal internados pelo Serviço de Coloproctologia do Hospital Conceição durante o período de janeiro de 2009 a maio de 2011. RESULTADOS: Foram estudados 61 pacientes, 65,6% mulheres. A idade variou de 40 a 84 anos. Realizaram colonoscopia 58 pacientes, desses 56,9% apresentavam mais de 50% de comprometimento da luz do cólon. O antígeno carcinoembrionário (CEA) foi coletado em 59 pacientes, 47,5% apresentavam CEA>5 ng/mL. Metástases à distância foram encontradas em 23,3% do total de 60 pacientes avaliados. Foram submetidos a tratamento cirúrgico 58 pacientes, desses a intenção curativa foi em 84,5%. A presença de mais de 12 linfonodos por peça foi de 73,1%. Os 61 pacientes estudados foram estratificados como 9,8% estádio I, 29,5% estádio II, 29,5% estádio III e 31,1% estádio IV. CONCLUSÃO: O perfil dos pacientes tratados em nossa instituição é de doença avançada; entretanto, os métodos curativos empregados têm ido ao encontro de um tratamento cirúrgico oncológico adequado.
neoplasias colorretais; cirurgia colorretal; SUS
ORIGINAL ARTICLE
Treatment of patients with colorectal cancer at a public hospital in Porto Alegre
Gabriel VolpatoI; Denize SchmittI; Cleber Antônio Nogueira Santos JúniorI; Luciano Pinto de CarvalhoII; Ruy Takashi koshimizuIII; Afonso Calil Mury MallmannIII
IAcademicians in the 7th semester of the Medical Science Course at the Universidade Luterana do Brasil (ULBRA) - Canoas (RS), Brazil
IIPhysician, Service of Coloproctology, Hospital Nossa Senhora da Conceição de Porto Alegre - Porto Alegre (RS), Brazil; Assistant Professor at ULBRA - Canoas (RS), Brazil
IIIPhysician, Service of Coloproctology, Hospital Nossa Senhora da Conceição de Porto Alegre - Porto Alegre (RS), Brazil
Correspondence to Correspondence to: Gabriel Volpato Travessa Vileta 230, apto 701, Jardim Botânico CEP 90690-150 - Porto Alegre (RS), Brazil E-mail: volpatinho@hotmail.com
ABSTRACT
OBJECTIVE: The purpose of this study is to demonstrate the current picture of colorectal cancer in a public hospital of Rio Grande do Sul, focusing on aspects related to diagnosis, staging and surgical therapy addressed in these patients.
METHODS: A descriptive and retrospective study that includes patients with colorectal cancer admitted to the Proctology Service of the Hospital Nossa Senhora da Conceição de Porto Alegre, from January 2009 to May 2011.
RESULTS: This study investigated 61 patients, 65.6% were female. Their age ranged from 40 to 84 years. Colonoscopy was performed in 58 patients; 56.9% of them had over 50% impaired colon lumen. The carcinoembryonic antigen (CEA) was collected from 59 patients, 47.5% had CEA>5 ng/mL. Distant metastases were found in 23.3% of total 60 patients. Underwent surgical treatment 58 patients, of a curative intent was 84.5%. The presence of more than 12 lymph nodes per specimen was 73.1%. All 61 patients were classified as: Stage I (9.8%), Stage II (29.5%), Stage III (29.5%) and Stage IV (31.1%).
CONCLUSION: The profile of the patients treated at our institution indicates disease in advanced stage; however, the methods employed have provided a curative surgical treatment in our oncology patients.
Keywords: colorectal neoplasms; colorectal surgery; Unified Health System.
RESUMO
OBJETIVO: O objetivo do presente estudo é demonstrar o panorama atual do câncer colorretal em um hospital público da capital do Rio Grande do Sul, enfocando aspectos relacionados ao diagnóstico, estadiamento e terapêutica cirúrgica abordada nesses respectivos pacientes.
MÉTODOS: Estudo descritivo e retrospectivo que inclui os pacientes com câncer colorretal internados pelo Serviço de Coloproctologia do Hospital Conceição durante o período de janeiro de 2009 a maio de 2011.
RESULTADOS: Foram estudados 61 pacientes, 65,6% mulheres. A idade variou de 40 a 84 anos. Realizaram colonoscopia 58 pacientes, desses 56,9% apresentavam mais de 50% de comprometimento da luz do cólon. O antígeno carcinoembrionário (CEA) foi coletado em 59 pacientes, 47,5% apresentavam CEA>5 ng/mL. Metástases à distância foram encontradas em 23,3% do total de 60 pacientes avaliados. Foram submetidos a tratamento cirúrgico 58 pacientes, desses a intenção curativa foi em 84,5%. A presença de mais de 12 linfonodos por peça foi de 73,1%. Os 61 pacientes estudados foram estratificados como 9,8% estádio I, 29,5% estádio II, 29,5% estádio III e 31,1% estádio IV.
CONCLUSÃO: O perfil dos pacientes tratados em nossa instituição é de doença avançada; entretanto, os métodos curativos empregados têm ido ao encontro de um tratamento cirúrgico oncológico adequado.
Palavras-chave: neoplasias colorretais; cirurgia colorretal; SUS.
INTRODUCTION
Colorectal cancer (CRC) is one of the most prevalent malignant neoplasms around the globe. Each year, one million new cases are diagnosed, and it is considered the third most frequent cause of cancer in the world, affecting both genders, and the second cause in developed countries1. Around 142,570 new cases of large bowel cancer are diagnosed each year in the United States, 102,900 of which are colorectal cancer and the rest refers to rectal cancer2.
The number of new cases of colorectal and rectal cancer in Brazil in 2010 is estimated to be 13,310 cases in males and 14,800 in females. These numbers correspond to estimated risks of 14 new cases in each 100,000 men and 15 in each 100,000 women. Not considering non-melanoma skin tumors, colorectal and rectal cancer is the third most frequent cancer in men in the South (21/100,000) and Southeast (19/100,000) regions of Brazil. In the Midwest (11/100,000) region, it is the fourth most frequent cancer. In the Northeast (5/100,000) and North (4/100.000) regions, it is the fifth. In women, it is the second most frequent cancer in the South (22/100,000) and Southeast (21/100,000) regions; the third in the Midwest (11/100,000) and Northeast (6/100,000) regions and the fifth in the North (4/100,000) region.
Rio Grande do Sul has the estimated rate of 27.07 cases to each 100,000 men and 27.69 cases to each 100,000 women. Porto Alegre, the State capital, has the estimated rate of 43.59 cases to each 100,000 men and 44.45 cases to each 100,000 women3.
Sporadic colorectal cancer (SCRC) accounts for 90% of all large bowel cancers that occur annually and most of them develop from an adenomatous polyp, the pre-malign phase of the anorectal adenocarcinoma4.
Age is an important risk factor for SCRC. It is a rare diagnosis before 40 years of age; the incidence starts to increase considerably between 40 and 50 years of age, and the incidence rates increase at each decade and in general they are not related to genetic or environmental risk factors5.
The periodic preventive exam - colonoscopy - can reduce the mean risk of death due to colorectal cancer by 90%6. In addition, most colorectal tumors, when diagnosed early, can be completely healed.
Although innumerous studies have addressed the prognostic meaning of various histological and molecular types, as well as clinical characteristics, the pathological stage at the diagnosis is still the best indicator of long-term prognosis to both colon and rectal cancer. The most important characteristics are presence of distant metastases, local extension of tumor, node positivity (number of lymph nodes involved) and residual disease7.
Surgery is the only curative therapy for focal colon cancer and a potentially curative option for selected patients with limited metastatic disease in the liver and/or lung. In addition, even patients that are not eligible to curative resection can benefit from palliative surgical procedures to relieve the obstruction symptoms and primary tumor bleeding8.
The purpose of this study is to show the current picture of colorectal cancer at a public hospital in Rio Grande do Sul operates only through the Unified Health System (SUS), providing patients with services focused on aspects related to diagnosis, staging and surgical therapy.
METHODS
This descriptive and retrospective study included patients with colorectal cancer admitted to the Coloproctology Service of the Hospital Nossa Senhora da Conceição, from January 2009 to May 2011. Patients with rectal cancer were excluded from the study.
The patients' data were obtained from their clinical records and histopathological reports of colonoscopy and surgical specimens.
The information collected were: gender, age, carcinoembryonic antigen (CEA), primary tumor location, lesion macroscopy, colon circumference involvement during colonoscopy, the surgery performed - whether curative or palliative, involvement of adjacent organs and whether they have been resected or not and if they presented any malignancy or inflammation, tumor staging, histological type, degree of tumor differentiation, nodal positivity, number of lymph nodes per surgical specimen, presence and location of metastases.
The information was entered in a database especially built for this purpose, on a spreadsheet using Microsoft Excel 2007 and later exported to SPSS v.17.0 for analysis. The quantitative variables were described using the mean value and standard deviation and the categorical variables were described through the frequency.
The study was analyzed and submitted to the approval of the Research Ethics Committee (CEP) of the Hospital Nossa Senhora da Conceição.
RESULTS
The study investigated 61 patients, 21 were male (34.4%) and 40 were female (65.6%). The patients' age ranged from 40 to 84 years, mean of 65.81±11.95 years.
Regarding the location, most patients presented sigmoid colon tumor (n=28; 45.9%), followed by ascending colon (n=12; 19.7%), cecum (n=6; 9.8%), splenic flexure (n=5; 8.2%), descending colon (n=5; 8.2%), hepatic flexure (n=3; 4.9%) and transverse colon (n=2; 3.3%).
Among the 61 analyzed patients, 58 were submitted to colonoscopy. None of them presented perforation and 28 (48.3%) had obstruction in the intestinal lumen that blocked the flow of intestinal contents. Ulcerovegetating lesions (48.3%) were the most prevalent and 56.9% of the patients showed more than 50% circumference involvement due to the lesion size (Table 1).
CEA was collected from 59 patients at the pathology diagnosis; the mean value was 210.97±1401.32 ng/mL (0.22-10754 ng/mL), with 47.5% of them with CEA over 5 ng/mL (Table 2).
Sixty patients were submitted to computed tomography; 14 (23.3%) of them with distant metastases, with liver as the most affected organ in 8 patients (57.1%), followed by lung in 5 cases (35.7%) and bone tissue in 1 case (7.1%).
Fifty-eight patients (95.1%) were submitted to surgical procedures. The surgery was curative in 49 (84.5%) and the palliative treatment was adopted in 9 patients (15.5%). Involvement of adjacent organs was observed in 19 patients (32.8%); in 12 (63.2%) of them, the anatomopathological result confirmed the presence of malignance, 4 (21.1%) showed organ inflammation only and 3 (15.8%) did not show any alteration, with resection of 11 (57.9%) of total 19 involved organs.
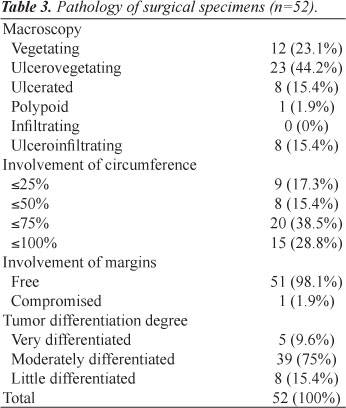
Table 3 shows the analysis of the 52 surgical specimens. Regarding the tumor macroscopy, 44.2% were ulcerovegetating and 67.3% affected more than 50% of the colon lumen. The mean tumor size was 5.2±2.12 cm (1.2-12 cm). Regarding the resection margin, 51 patients (98.15%) had free margins. The mean number of lymph nodes found per specimen was 17.69±9.92 (0-59), and positivity of 50%. More than 12 lymph nodes per specimen were found in 73.1% of the surgical specimens, with 66.7% of them from patients classified as Stage II (Table 2).
In relation to staging, the patients presented the following distribution: 9.8% were Stage I, 29.5% Stage II, 29.5% Stage III and 31.1% Stage IV (Table 4).
DISCUSSION
The purpose of the colon cancer surgery is to perform the complete removal of the tumor, with the main vascular pedicle of the affected segment of the colon and its lymphatic drainage area. While the segment resection is sometimes enough to remove the primary tumor, a larger resection is usually required for a satisfactory lymphadenectomy. The blood vessels should be separated at their origin point to allow wider resection and maximize the number of lymph nodes in the specimen. Block resection of adjacent structures is indicated in case of tumor ligation or adhesion to any other organ or structure.
For a surgery to be oncologically correct, it prioritizes resection with free margins8. In our study, 98.1% of all resected tumors had free distal, proximal and radial margins.
Regional lymphadenectomy provides important prognostic and therapeutic information that guide the adjuvant treatment. In a systematic review, the number of lymph nodes evaluated after the surgical resection was positively associated with survival of patients classified as Stage II and Stage III for colon cancer9. Established guidelines recommend that at least 12 lymph nodes should be analyzed for a proper staging10-12. The American Society of Clinical Oncology (ASCO) encourages the use of adjuvant chemotherapy in patients with colon cancer and negative lymph nodes if the surgical specimen has less than 12 lymph nodes13. Although the use of adjuvant chemotherapy has not been established in Stage II patients, in our study, 66.7% of the surgical specimens of Stage II patients had more than 12 lymph nodes and 73.1% of total analyzed specimens had more than 12 lymph nodes14.
A number of serum markers has been associated with CRC, especially CEA and carbohydrate antigen (CA) 19-9. However, these markers have a low diagnostic capability to detect primary CRC due to the significant overlap with benign disease (gastritis, peptic ulcer, diverticulitis, liver disease, chronic obstructive pulmonary disease, diabetes or any acute or chronic inflammatory condition) and low sensitivity to the disease in its early phase15-18.
However, the serum levels of CEA are useful to the prognosis of patients with recently diagnosed CRC. Patients with serum CEA >5 ng/mL in the preoperative period have worse prognosis than those with lower levels. In addition, higher levels of preoperative CEA that do not normalize after the surgical resection require a deeper evaluation to investigate the persistent disease. ASCO guidelines recommend that the serum levels of CEA, when obtained in the preoperative period from patients with colorectal cancer, should help in the surgical treatment preparation and planning and in the prognosis evaluation15. In our study, 47.5% of the patients that had their CEA analyzed presented serum level of >5 ng/mL at the pathological diagnosis.
Around 20% of the patients have metastatic disease at the moment they search for care19. The colon cancer can spread through lymphatic and hematogenical dissemination, and through contiguous and transperitoneal pathways. The most frequent areas affected by metastasis are regional lymph nodes, liver, lung and peritoneum, and the patients can show signs or symptoms related to any of these areas. As the venous drainage of the intestinal tract is through the portal system, the first area of hematogenical dissemination is usually the liver, followed by the lungs, bones and many other sites, including the brain19. In our study, 23.3% of the patients had metastatic diseases at the moment of diagnosis, and the most affected areas were: liver (57.1%), lung (35.7%) and bone (7.1%); in agreement with the literature.
Most of our patients were in advanced stages of the disease, with more than 60% of them classified as Stages III and IV, in agreement with the absence of tracking measures in our population.
CONCLUSION
After evaluating the characteristics of patients with colorectal cancer treated in our service, we conclude that most of them are reaching an advanced stage of the disease. However, the methods employed have provided a curative surgical treatment in our oncology patients.
Submitted on: 08/08/2011
Approved on: 09/09/2011
Financing source: none.
Conflict of interest: nothing to declare.
Study carried out at the Service of Coloproctology, Hospital Nossa Senhora da Conceição de Porto Alegre - Porto Alegre (RS), Brazil.
- 1. Andrade SMS, Pereira FL. Câncer colorretal sincrônico - relato de caso e revisão de literatura. J Coloproctol 2007;27(1):69-79.
- 2. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin 2010;60(5):277-300.
-
3INCA. Estimativa 2010 - Incidência de câncer no Brasil [cited 2011 Feb. 22]. Available from: http://www.inca.gov.br/estimativa/2010
- 4. Wills JC, Burt RW. Hereditary aspects of colon cancer. Ochsner J 2002;4:129-38.
- 5. Eddy DM. Screening for colorectal cancer. Ann Intern Med 1990;113(5):373-84.
- 6. Obrand DI, Gordon PH. Continued change in the distribution of colorectal carcinoma. Br J Surg 1998;85(2):246-8.
- 7. Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, et al (Eds). AJCC (American Joint Committee on Cancer). Cancer staging manual. 6th ed. New York: Springer; 2002. p. 113.
- 8. Nelson H, Petrelli N, Carlin A, Couture J, Fleshman J, Guillem J, et al. Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst 2001;93(8):583-96.
- 9. Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst 2007;99(6):433-41.
- 10. Compton CC, Fielding LP, Burgart LJ, Conley B, Cooper HS, Hamilton SR, et al. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 2000;124(7):979-94.
- 11. McGory ML, Shekelle PG, Ko CY. Development of quality indicators for patients undergoing colorectal cancer surgery. J Natl Cancer Inst 2006;98(22):1623-33.
- 12. Otchy D, Hyman NH, Simmang C, Anthony T, Buie WD, Cataldo P, et al. Practice parameters for colon cancer. Dis Colon Rectum 2004;47(8):1269-84.
- 13. Benson AB 3rd, Schrag D, Somerfield MR, Cohen AM, Figueredo AT, Flynn PJ, et al. American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol 2004;22(16):3408-19.
- 14. Benson AB III, Schrag D, Somerfield MR, Cohen AM, Figueredo AT, Flynn PJ, et al. American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol 2004;22(16):3408-19.
- 15. Locker GY, Hamilton S, Harris J, Jessup JM, Kemeny N, Macdonald JS, et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J Clin Oncol 2006;24(33):5313-27.
- 16. Macdonald JS. Carcinoembryonic antigen screening: pros and cons. Semin Oncol 1999;26(5):556-60.
- 17. Palmqvist R, EngarÅs B, Lindmark G, Hallmans G, Tavelin B, Nilsson O, et al. Prediagnostic levels of carcinoembryonic antigen and CA 242 in colorectal cancer: a matched case-control study. Dis Colon Rectum 2003;46(11):1538-44.
- 18. Van der Schouw YT, Verbeek AL, Wobbes T, Segers MF, Thomas CM. Comparison of four serum tumour markers in the diagnosis of colorectal carcinoma. Br J Cancer 1992;66(1):148-54.
- 19. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin 2009;59(4):225-49.
Correspondence to:
Publication Dates
-
Publication in this collection
07 May 2012 -
Date of issue
Dec 2011
History
-
Received
08 Aug 2011 -
Accepted
09 Sept 2011