Abstracts
INTRODUCTION: Ulcerative colitis (UC) is a chronic inflammatory disease that affects the rectum and colon, involving periods of exacerbation and remission. A considerable number of patients requires surgery during the course of this disease. OBJECTIVE: The purpose of this study is to analyze the profile and therapeutic approach of patients with UC. METHODS: This is a retrospective study that analyzed medical records of patients diagnosed with UC between 1999 and 2010. We selected 45 patients and analyzed the following variables: age, gender, ethnic group, interval between onset of symptoms and diagnosis, extraintestinal manifestations, extent of colonic involvement, disease complications, pharmacological treatment, indication for surgery, time between diagnosis and indication, surgical procedures, early and late complications and pathological results of surgical specimens. Data were analyzed descriptively and compared with other studies. RESULTS: The clinical profile of the patients was consistent with the literature. Nine patients underwent surgical treatment: seven were submitted to proctocolectomy with anastomosis in the ileo-anal pouch and two were submitted to total colectomy; in addition, eight were submitted to ileostomy. Postoperative complications occurred in 55.5% of patients. CONCLUSIONS: The study confirms data from the literature regarding the profile and therapeutic approach of patients with ulcerative colitis.
proctocolitis; colorectal surgery; postoperative complications; signs and symptoms; digestive; colonic pouches
INTRODUÇÃO: A retocolite ulcerativa (RCU) é uma doença inflamatória crônica que acomete reto e cólon, cursando com períodos de exacerbação e remissão. Uma parcela considerável de pacientes necessita de procedimento cirúrgico ao longo do curso dessa enfermidade. OBJETIVO: Este estudo objetiva analisar perfil e abordagem terapêutica de portadores de RCU. MÉTODOS: Trata-se de estudo retrospectivo realizado por meio da análise de prontuários de pacientes acompanhados com diagnóstico de RCU no período de 1999 a 2010. Foram selecionados 45 pessoas, sendo analisadas as variáveis: idade, sexo, raça, intervalo entre início dos sintomas e diagnóstico, sintomatologia, manifestações extraintestinais, extensão do acometimento colônico, complicações da doença, tratamento medicamentoso, indicação de cirurgia, tempo entre esta e o diagnóstico, procedimentos cirúrgicos, complicações precoces e tardias e resultado anatomopatológico das peças cirúrgicas. Os dados foram analisados de forma descritiva e comparados com outros estudos. RESULTADOS: O perfil clínico dos pacientes foi condizente com a literatura. Nove foram submetidos a tratamento cirúrgico, sendo realizadas sete proctocolectomias com anastomose em bolsa íleo-anal e duas colectomias totais, além de oito ileostomias. As complicações pós-operatórias ocorreram em 55,5% dos pacientes. CONCLUSÕES: O estudo corrobora com os dados da literatura referentes ao perfil e abordagem terapêutica dos pacientes com diagnóstico de RCU.
proctocolite; cirurgia colorretal; complicações pós-operatórias; sintomas e sinais digestórios; bolsas do colo
ORIGINAL ARTICLE
The surgical treatment of patients with ulcerative colitis from an university hospital at Natal, Brazil
Suelene Suassuna Silvestre de AlencarI; Romualdo da Silva CorrêaII; Cátia de França BezerraIII; Emanuela Simone Cunha de MenezesIV; Antonio Luiz do NascimentoIV; Davi Aragão Alves da CostaIV; Marcelo José Carlos AlencarIV
IMaster in Surgery at the Universidade Federal de Pernambuco (UFPE); Supervisor at the Medical Residency Program in General Surgery and Head of the Service of Coloproctology at the Hospital Universitário Onofre Lopes (HUOL) Natal (RN), Brazil
IIDoctor in Health Sciences at the Universidade Federal de São Paulo (UNIFESP); Assistant Professor of the Department of Integrated Medicine at the Universidade Federal do Rio Grande do Norte (UFRN) Natal (RN), Brazil
IIIGraduated in Medicine at the Universidade Federal da Paraíba (UFPB); Resident in General Surgery at the HUOL Natal (RN), Brazil
IVAcademician in Medicine at the UFRN; Trainee at the Service of Coloproctology at the HUOL Natal (RN), Brazil
Correspondence to Correspondence to: Suelene Suassuna Silvestre de Alencar Rua Jaguarari, 5.100, casa 76 59064-500 Natal (RN), Brasil E-mail: suelene@ufrnet.br
ABSTRACT
INTRODUCTION: Ulcerative colitis (UC) is a chronic inflammatory disease that affects the rectum and colon, involving periods of exacerbation and remission. A considerable number of patients requires surgery during the course of this disease.
OBJECTIVE: The purpose of this study is to analyze the profile and therapeutic approach of patients with UC.
METHODS: This is a retrospective study that analyzed medical records of patients diagnosed with UC between 1999 and 2010. We selected 45 patients and analyzed the following variables: age, gender, ethnic group, interval between onset of symptoms and diagnosis, extraintestinal manifestations, extent of colonic involvement, disease complications, pharmacological treatment, indication for surgery, time between diagnosis and indication, surgical procedures, early and late complications and pathological results of surgical specimens. Data were analyzed descriptively and compared with other studies.
RESULTS: The clinical profile of the patients was consistent with the literature. Nine patients underwent surgical treatment: seven were submitted to proctocolectomy with anastomosis in the ileo-anal pouch and two were submitted to total colectomy; in addition, eight were submitted to ileostomy. Postoperative complications occurred in 55.5% of patients.
CONCLUSIONS: The study confirms data from the literature regarding the profile and therapeutic approach of patients with ulcerative colitis.
Keywords: proctocolitis; colorectal surgery; postoperative complications; signs and symptoms, digestive; colonic pouches.
RESUMO
INTRODUÇÃO: A retocolite ulcerativa (RCU) é uma doença inflamatória crônica que acomete reto e cólon, cursando com períodos de exacerbação e remissão. Uma parcela considerável de pacientes necessita de procedimento cirúrgico ao longo do curso dessa enfermidade.
OBJETIVO: Este estudo objetiva analisar perfil e abordagem terapêutica de portadores de RCU.
MÉTODOS: Trata-se de estudo retrospectivo realizado por meio da análise de prontuários de pacientes acompanhados com diagnóstico de RCU no período de 1999 a 2010. Foram selecionados 45 pessoas, sendo analisadas as variáveis: idade, sexo, raça, intervalo entre início dos sintomas e diagnóstico, sintomatologia, manifestações extraintestinais, extensão do acometimento colônico, complicações da doença, tratamento medicamentoso, indicação de cirurgia, tempo entre esta e o diagnóstico, procedimentos cirúrgicos, complicações precoces e tardias e resultado anatomopatológico das peças cirúrgicas. Os dados foram analisados de forma descritiva e comparados com outros estudos.
RESULTADOS: O perfil clínico dos pacientes foi condizente com a literatura. Nove foram submetidos a tratamento cirúrgico, sendo realizadas sete proctocolectomias com anastomose em bolsa íleo-anal e duas colectomias totais, além de oito ileostomias. As complicações pós-operatórias ocorreram em 55,5% dos pacientes.
CONCLUSÕES: O estudo corrobora com os dados da literatura referentes ao perfil e abordagem terapêutica dos pacientes com diagnóstico de RCU.
Palavras-chave: proctocolite; cirurgia colorretal; complicações pós-operatórias; sintomas e sinais digestórios; bolsas do colo.
INTRODUCTION
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that spreads across the mucosa. It involves the rectum in about 95% of the cases and may extend in an ascending, symmetrical form, presenting a circumferential pattern, fully or partially affecting the colon1,2. It affects around 500,000 people in the United States, with annual incidence of 8 to 12 in 100,000 people, a constant index in the last five decades1. In Brazil, no concrete data are available, but growing incidence of the disease has been observed. It is the cause of 25,000 doctor's appointments annually, around 30,000 hospital admissions and over 1 million working days missed by people with this disease1. Its etiology is unknown, but it is believed to involve multiple factors, with patients genetically susceptible, associated with unbalanced immunological response, influenced by environmental factors1,2.
It is clinically characterized by diarrhea mixed with blood, associated with symptoms of rectal urgency and tenesmus. The clinical course of the disease involves periods of exacerbation and remission, which may occur spontaneously or as a response to treatment3. Most treatments use pharmacological options; however, estimates say that around 20 to 30% of the affected individuals will require surgical interventions, which may be curative, with most of them within the period of 10 years from the initial diagnosis. The surgery has elective or emergency indication when it occurs as a result of disease complications2.
When the disease has indication for surgery, the intervention is selected from a number of surgical options. The benefits of a more extensive procedure that enhances the disease cure, reduces the long-term risk of cancer and improves the functional result should be analyzed versus a less extensive procedure, which may be safer in specific clinical situations. It is important to emphasize that most patients want to avoid a definitive ileostomy. In addition, the development of an intestinal restorative technique with ileal pouch-anal anastomosis (IPAA) is the procedure of choice to treat patients with UC4.
The purpose of this study was to analyze the profile and therapeutic approach of patients with UC from 1999 to 2010 seen at the Service of Gastroenterology and Coloproctology of the Hospital Universitário Onofre Lopes (HUOL), in Natal, comparing the results with those presented in the medical literature, for possible practice reviews.
METHODS
This is a retrospective study based on chart reviews of patients diagnosed with ulcerative colitis seen at the Service of Gastroenterology and Coloproctology of the HUOL from 1999 to 2010.
A bibliographic review regarding the disease was performed, using Pubmed, Lilacs and Scielo database.
The variables collected were: age, gender, race, interval between onset of symptoms and diagnosis, extraintestinal manifestations, extent of colonic involvement, disease-related complications, pharmacological treatment, indication for surgery, time between diagnosis and surgical indication, surgical procedures, early and late postoperative complications (up to 30 days and more than 30 days after the surgery, respectively) and pathological results of surgical specimens.
Fifty-three patients were found and 45 of them were selected for this study. The exclusion criterion was the inadequate completion of patient records.
Data collected were stored in Microsoft Excel 2007TM spreadsheets for the analysis of variables, elaboration of charts and tables and subsequent comparison with data published in the global medical literature.
The protocol of this study was approved by the Research Ethics Committee of the HUOL, with a certificate CAAE (Certificado de Apresentação para Apreciação Ética) nº 0069.0.294.000-11.
RESULTS
The analysis of 45 patient records showed that both genders were affected, with a small predominance in men (53.33%; n=24). The most affected age group was over 40 years of age (57.78%; n=26), followed by the age group between 31 and 40 years old (28.89%; n=13). The group between 21 and 30 years old represented 8.89% (n=4) of patients and the group of patients under 20 years old, 4.44% (n=2), as illustrated in Chart 1. Regarding the onset of symptoms and diagnosis, the predominance was in the group between 31 and 40 years old and above 60 years old.
In terms of race, white patients were predominant (51%; n=23), followed by brown patients (42.2%; n=19) and, in a small proportion, black patients (6.7%; n=3), no indigenous patient was included in the study. Positive family history was observed in 7% of the cases.
The main symptoms presented were chronic diarrhea and bleeding of variable intensity, both presented in 100% of the cases. Other important symptoms were: weight loss (86.67%), followed by abdominal pain, tenesmus and anorexia, in equal proportions (73.33%). The patients presented other symptoms, as illustrated in Chart 2.
Extraintestinal manifestations were present in 35.56% (n=16) of the patients, with predominance of osteoarticular manifestations, followed by dermatological manifestations and, in small proportions, by ophthalmic, hepatobiliary, nutritional and metabolic manifestations.
From all patients, 13.33% (n=6) had complications related to UC, such as rectal bleeding, fulminant colitis, toxic megacolon, perforation, delayed growth and dysplasia (Table 1).
The predominant UC location was the distal colon (proctitis/proctosigmoiditis), in 53.33% (n=24) of the cases, followed by left colitis in 26.67% (n= 12) and pancolitis in 20% (n=9) (Chart 3).
In terms of treatment, the most frequent medications were salicylates (82.22%), oral corticosteroids (51.11%) and, in small proportions, azathioprine, infliximab, antibiotics, topical corticosteroid and tacrolimus (Table 2).
Twenty per cent of patients (n=9) had indication for surgery, 67% (n=6) of them were submitted to elective surgery and 33% (n=3) to emergency surgery.
In all cases, the interval between diagnosis and indication for surgery was 10 years or less, in the majority of cases the interval was within the first five years of the disease (Chart 4).
The indications that led to surgery were clinical intractability (67%; n=6), side effects/drug intolerance (22%; n=2) and dysplasia (11%; n=1) (Chart 5).
Among surgical procedures, total proctocolectomy with "J" ileal pouch-anal anastomosis was the most common procedure (78%; n=7), followed by total colectomy (22%; n=2) (Chart 6). Six patients with a ileal pouch-anal anastomosis underwent diverted ileostomy.
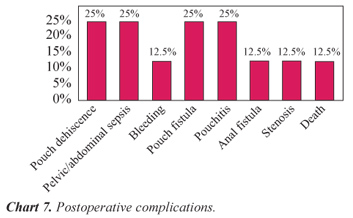
Postoperative complications occurred in 55.5% (n=5) of the patients, four patients had early complications (<30 days), and late (>30 days) complications were observed in five patients. The main early complications were: anastomotic dehiscence (two patients), pelvic/abdominal sepsis (two) and bleeding (one). Late complications were: pouch fistula (two), pouchitis (two), IPAA stenosis (one), anal fistula (one) and death (one) (Chart 7).
After the anatomopathological analysis, UC diagnosis was confirmed in 89% (n=8) of the cases and Crohn's disease in one patient (11%; n=1), who was later submitted to abdominoperineal amputation due to the presence of disease in the rectal stump and dysplasia during the follow-up period.
DISCUSSION
The disease extension was, in descending order, distal colitis, left-side colitis and pancolitis. These data are compatible with those found in the medical literature, which show predominance of distal colitis in 34 to 70% of the cases, followed by left colitis in 8 to 40% and pancolitis in 14 to 56%1.
Extraintestinal manifestations (EIM) may occur in up to 30% of the cases ophthalmic manifestations, arthritis and dermatological manifestations are associated with the disease activity, while axial arthropathy and primary sclerosing cholangitis (PSC) occur regardless of the disease activity1. In our study, EIMs occurred in 35.5%.
According to international references, the most common drugs used to induce remission of acute disease are salicylates and corticosteroids and, in more severe or refractory cases, thiopurines, azathioprine, 6-mercaptopurine and immunobiological agents (infliximab). For maintenance, salicylates, thiopurines and immunobiological agents are the most recommended drugs1,5. Our study has agreed with the literature, as salicylates were the most common drugs, followed by oral corticosteroids, azathioprine and infliximab.
Regarding the treatment, we had 20% of surgical indication (n=9), all within the first 10 years of the disease, with predominance (77%) in the first 5 years. These results are similar to current literature, which indicates that 20 to 30% of patients with UC are submitted to surgical resection, most of them within the first 10 years from the initial diagnosis1,2,4-6. The progress of surgical techniques has allowed fecal stream restoration with anal continence preservation, reinforcing the importance of surgery in UC cure. The indications for surgery in our study were clinical intractability (67%), drug intolerance (22%) and dysplasia (11%). Among these patients, 67% (n=6) were submitted to elective surgery and 33% (n=3) to emergency surgery due to UC complications (fulminant colitis, toxic megacolon, perforation and bleeding). One patient submitted to elective surgery had delayed growth. Such indications are reported in the medical literature1,2,4,5.
In patients that developed peritonitis or perforation due to toxic colitis refractory to clinical treatment, the surgery performed was subtotal colectomy with ileostomy. Better medical support and more aggressive surgical intervention led to significant reduction of mortality caused by toxic colitis to levels below 3%4,7. Bleeding occurred in 10% of all emergency colectomy for UC. In patients with massive bleeding and malnourished, the best option is subtotal colectomy and terminal ileostomy4.
Around 70% of the patients with UC are submitted to surgery due to chronic problems4. These people have persistent symptoms, with negative impact on their quality of life. Malnourishment and delayed growth are significant problems in pediatric patients. In more severe chronic cases, restorative proctocolectomy is frequently performed in stages. Debilitating extraintestinal manifestations are rarely indications for colectomy. Although most of these conditions will spontaneously improve in the postoperative period, the response is not always predictable. Long-term complications from the use of steroids are another frequent indication for surgical resection4.
Among patients with UC, 10% are submitted to surgery due to cancer or dysplasia4. The risk factors for the development of colorectal cancer are long-term disease, pancolitis, early age at onset, concomitant PSC and dysplasia. Dysplasia is still the main risk factor available for malignancy potential, and it is reasonable for patients with UC for more than eight years to be submitted to surveillance colonoscopy with sequential biopsy. Patients diagnosed with dysplasia or cancer should be submitted to surgical resection1,4,5,8.
Proctocolectomy with "J" ileal pouch-anal anastomosis was performed in six patients and urgent total colectomy in three patients in our study. One patient was submitted to permanent ileostomy, after the anatomopathological diagnosis of Crohn's disease, and one patient to temporary ileostomy due to toxic colitis, with subsequent intestinal reconstruction with IPAA.
With the advent of restorative proctocolectomy with IPAA as the procedure of choice, total colectomy with ileostomy has been mainly indicated to emergency cases, incontinent patients and cases of indetermined colitis4. Many studies indicate that a restorative proctocolectomy with IPAA can be performed in a safer manner, with operative mortality less than 1%. Postoperative complications are frequent, but controllable. They are of mechanical, inflammatory, functional, neoplastic and metabolic nature, ranging from 10 to 60%9.
The main early postoperative complications presented in this study were anastomotic dehiscence, pelvic/abdominal sepsis and bleeding, and late complications were pouch fistula, pouchitis, IPAA stenosis, anal fistula and death. All these results are similar to those of other studies published in the medical literature4,10.
Sepsis occurs in 3 to 15% of patients after restorative proctocolectomy with IPAA, and it is the most frequent early complication4,10. The causes include pouch or anastomotic leak, with consequent contamination of peritoneal cavity, and it may affect up to 34% of the cases11 and lead to death in 3%10,11. Other less frequent complications include deep vein thrombosis, pulmonary embolism, intestinal bleeding from ileostomy or pouch and pouch ischemia.
Pouchitis is the most frequent late complication, affecting 23 to 46% of patients4,10. In this situation, clinical treatment is indicated and, in some cases, ileal bypass or pouch excision is necessary. Pouch fistulas occur in 3 to 17% of the cases4,10 and stenosis of the pouch anastomosis in 7.8 to 14%4,10,12.
In our study, all ileal pouches were constructed in "J" shape, as recommended by other studies13, and, in six cases, a diverted ileostomy was performed, despite its controversial indication in medical literature14. Although diverted ileostomy does not prevent dehiscence, it minimizes the degree of pelvic contamination, which may result in pouch dysfunction, requiring pouch removal. Some authors emphasize the benefit of protective ileostomy in specific cases4.
When analyzing the long-term functional results of the pouch and the quality of life of patients after restorative proctocolectomy, we can say that, according to prior studies, most patients are satisfied15,16. In our study, all of our patients are in outpatient clinic follow-up, with good function and excellent pouch acceptance.
CONCLUSION
After analyzing data from this case series, we can conclude that our study results are similar to those reported in the medical literature and this was important to review the care delivered in our service.
Submitted on: 03/26/2012
Approved on: 03/29/2012
Study carried out at the Department of Integrated Medicine at the Universidade Federal do Rio Grande do Norte Natal (RN), Brazil.
Financing source: none.
Conflict of interest: nothing to declare.
- 1. Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults: American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol 2010; 105(3):501-23.
- 2. Ikeuchi H, Uchino M, Matsuoka H, Bando T, Matsumoto T, Tomita N, et al. Surgery for ulcerative colitis in 1,000 patients. Int J Colorectal Dis 2010;25(8):959-65.
- 3. Kornbluth AA, Salomon P, Sacks HS, Mitty R, Janowitz HD. Meta-analysis of the effectiveness of current drug therapy of ulcerative colitis. J Clin Gastroenterol 1993;16(3):215-8.
- 4. Blumberg D, Beck DE. Surgery for ulcerative colitis. Gastroenterol Clin North Am 2002;31(1):219-35.
- 5. Beauchamp RD, Evers BM, Townsend CM. Sabiston fundamentos de cirurgia. 17Ş ed. Rio de Janeiro (RJ): Campus; 2006.
- 6. Dhillon S, Loftus EV, Tremaine WJ, Jewell DA, Harmsen WS, Zinsmeister AR, et al. The natural history of surgery for ulcerative colitis in a population-based cohort from Olmsted County, Minnesota. Am J Gastroenterol 2005;100:S-303.
- 7. Pinna-Pintor M, Arese P, Bona R, Falletto E, Schieroni R, Villata E, et al. Severe steroid-unresponsive ulcerative colitis: outcomes of restorative proctocolectomy in patients undergoing cyclosporin treatment. Dis Colon Rectum 2000;43(5):609-13.
- 8. Marchesa P, Lashner BA, Lavery IC, Milsom J, Hull TL, Strong SA, et al. The risk of cancer and dysplasia among ulcerative colitis patients with primary sclerosing cholangitis. Am J Gastroenterol 1997;92(8):1285-8.
- 9. Tulchinsky H, Dotan I, Alper A, Brazowski E, Klausner JM, Halpern Z, et al. Comprehensive pouch clinic concept for follow-up of patients after ileal pouch anal anastomosis: report of 3 years' experience in a tertiary referral center. Inflamm Bowel Dis 2008;14(8):1125-32.
- 10. Shen B, Remzi FH, Lavery IC, Lashner BA, Fazio VW. A proposed classification of ileal pouch disorders and associated complications after restorative proctocolectomy. Clin Gastroenterol Hepatol 2008;6(2):145-58.
- 11. Sagap I, Remzi FH, Hammel JP, Fazio VW. Factors associated with failure in managing pelvic sepsis after ileal pouch-anal anastomosis (IPAA) a multivariate analysis. Surgery 2006;140(4):691-703.
- 12. Prudhomme M, Dozois RR, Godlewski G, Mathison S, Fabbro-Peray P. Anal canal strictures after ileal pouch-anal anastomosis. Dis Colon Rectum 2003;46(1):20-3.
- 13. Tekkis PP, Nicholls RJ. Ileal pouch dysfunction: diagnosis and management. Gastroenterol Clin North Am 2008;37(3):669-83.
- 14. Grobler SP, Hosie KB, Keighley MR. Randomized trial of loop ileostomy in restorative proctocolectomy. Br J Surg 1992;79(9):903-6.
- 15. Provenzale D, Shearin M, Phillips-Bute BG, Drossman DA, Li Z, Tillinger W, et al. Health-related quality of life after ileoanal pull-through evaluation and assessment of new health status measures. Gastroenterology 1997;113(1):7-14.
- 16. Pemberton JH, Phillips SF, Ready RR, Zinsmeister AR, Beahrs OH. Quality of life after Brooke ileostomy and ileal pouch-anal anastomosis. Comparison of performance status. Ann Surg 1989;209(5):620-6.
Publication Dates
-
Publication in this collection
08 Jan 2013 -
Date of issue
Sept 2012
History
-
Received
26 Mar 2012 -
Accepted
29 Mar 2012