Abstracts
The aim of the present study was to evaluate the efficacy of colocolonic anastomosis with and without preoperative bowel preparation. METHODS: The study compared 42 female dogs (Canis familiaris), divided into 2 groups of 21 animals: Group I (control) - submitted to bowel preparation - and Group II (study) - without previous bowel preparation -. All animals were submitted to laparotomy with sectioning of the descending colon and primary anastomosis using polypropylene thread. Following euthanasia on the 21st postoperative day (POD), a second laparotomy was performed to evaluate the anastomosis with regard to complications, intra-abdominal adhesions and anastomotic burst pressure. RESULTS: One animal from each group (4.5%) died. The death in Group I occurred on seventh POD due to anastomotic dehiscence. The death in Group II occurred on tenth POD due to deep incisional infection at the surgical site and complete dehiscence of the abdominal wall. The groups did not differ significantly with regard to adhesion grade or anastomotic burst pressure (one specimen burst in each group) (p>0.05). CONCLUSION: Colocolonic anastomosis without previous bowel preparation was shown to be safe and efficacious, suggesting it is not an indispensable procedure in colorectal anastomosis surgery.
colorectal surgery; postoperative complications; anastomotic leak
Esse estudo avaliou a eficácia da anastomose colocólica sem preparo intestinal prévio comparando-a com a anastomose realizada com preparo. MÉTODO: Foram utilizados 42 animais (Canis familiares) fêmeas distribuídos em 2 grupos com 21 animais em cada: Grupo I (controle) - com preparo intestinal - e Grupo II (estudo) - sem preparo intestinal prévio -. Os animais de ambos os grupos foram submetidos à laparotomia com secção do cólon descendente e à anastomose primária com fio de polipropileno, bem como à eutanásia no 21º dia de pós-operatório com laparotomia e à avaliação da anastomose colocólica quanto à presença de complicações, grau de aderências intestinais e pressão de ruptura da anastomose. RESULTADOS: Ocorreu um (4,5%) óbito em cada grupo, sendo o do Grupo I no sétimo dia pós-operatório em decorrência da deiscência da anastomose colocólica e o do Grupo II no décimo dia de pós-operatório por causa de infecção em sítio cirúrgico com deiscência total da parede abdominal. Não foi observada diferença estatisticamente significante no grau de aderências intestinais tampouco no teste de pressão de ruptura entre os grupos (um espécime sofreu ruptura em casa grupo) (p>0,05). CONCLUSÃO: A anastomose colocólica sem preparo intestinal apresentou a mesma segurança e eficácia da anastomose realizada com preparo prévio, sugerindo não ser indispensável na cirurgia colorretal com anastomose.
cirurgia colorretal; complicações pós-operatórias; fístula anastomótica
ORIGINAL ARTICLE
Role of bowel preparation on colocolonic anastomosis: experimental study in dogs
Francisco Sérgio Pinheiro RegadasI; Welligton Ribeiro FigueiredoII; Miguel Augusto Arcoverde NogueiraIII; Carlos Renato Sales BezerraIV; Péricles Cerqueira de SousaV
IFull Professor at Faculty of Medicine, Universidade Federal do Ceará (UFC) Fortaleza (CE), Brazil
IIDigestive Tract Surgeon, Master student in Surgery, UFC Fortaleza (CE), Brazil
IIIColoproctologist, Doctoral candidate in Surgery, UFC Fortaleza (CE), Brazil
IVDigestive Tract Surgeon, Doctoral candidate in Surgery, UFC Fortaleza (CE), Brazil
VDigestive Tract Surgeon, Master student in Surgery, UFC Fortaleza (CE), Brazil
Correspondence to Correspondence to: Francisco Sergio Pinheiro Regadas Faculdade de Medicina da Universidade Federal do Ceará Avenida Atilano de Moura, 430, apto. 200 CEP: 60810-180 Fortaleza (CE), Brazil E-mail: sregadas@hospitalsaocarlos.com.br
ABSTRACT
The aim of the present study was to evaluate the efficacy of colocolonic anastomosis with and without preoperative bowel preparation.
METHODS: The study compared 42 female dogs (Canis familiaris), divided into 2 groups of 21 animals: Group I (control) submitted to bowel preparation and Group II (study) without previous bowel preparation . All animals were submitted to laparotomy with sectioning of the descending colon and primary anastomosis using polypropylene thread. Following euthanasia on the 21st postoperative day (POD), a second laparotomy was performed to evaluate the anastomosis with regard to complications, intra-abdominal adhesions and anastomotic burst pressure.
RESULTS: One animal from each group (4.5%) died. The death in Group I occurred on seventh POD due to anastomotic dehiscence. The death in Group II occurred on tenth POD due to deep incisional infection at the surgical site and complete dehiscence of the abdominal wall. The groups did not differ significantly with regard to adhesion grade or anastomotic burst pressure (one specimen burst in each group) (p>0.05).
CONCLUSION: Colocolonic anastomosis without previous bowel preparation was shown to be safe and efficacious, suggesting it is not an indispensable procedure in colorectal anastomosis surgery.
Keywords: colorectal surgery; postoperative complications; anastomotic leak.
RESUMO
Esse estudo avaliou a eficácia da anastomose colocólica sem preparo intestinal prévio comparando-a com a anastomose realizada com preparo.
MÉTODO: Foram utilizados 42 animais (Canis familiares) fêmeas distribuídos em 2 grupos com 21 animais em cada: Grupo I (controle) com preparo intestinal e Grupo II (estudo) sem preparo intestinal prévio . Os animais de ambos os grupos foram submetidos à laparotomia com secção do cólon descendente e à anastomose primária com fio de polipropileno, bem como à eutanásia no 21º dia de pós-operatório com laparotomia e à avaliação da anastomose colocólica quanto à presença de complicações, grau de aderências intestinais e pressão de ruptura da anastomose.
RESULTADOS: Ocorreu um (4,5%) óbito em cada grupo, sendo o do Grupo I no sétimo dia pós-operatório em decorrência da deiscência da anastomose colocólica e o do Grupo II no décimo dia de pós-operatório por causa de infecção em sítio cirúrgico com deiscência total da parede abdominal. Não foi observada diferença estatisticamente significante no grau de aderências intestinais tampouco no teste de pressão de ruptura entre os grupos (um espécime sofreu ruptura em casa grupo) (p>0,05).
CONCLUSÃO: A anastomose colocólica sem preparo intestinal apresentou a mesma segurança e eficácia da anastomose realizada com preparo prévio, sugerindo não ser indispensável na cirurgia colorretal com anastomose.
Palavras-chave: cirurgia colorretal; complicações pós-operatórias; fístula anastomótica.
INTRODUCTION
Colorectal surgery with primary anastomosis is associated with a range of mild to severe complications, from simple surgical site infection to anastomotic dehiscence and fistula. Thus, the postoperative recovery of patients submitted to colorectal surgery remains a major challenge for surgeons.
Mechanical bowel preparation of the colon prior to elective surgery was first proposed over a hundred years ago. It has since been used to reduce or eliminate the fecal mass, thereby minimizing infection and complications in perianastomotic tissues and ensuring more esthetic outcomes1.
Bowel preparation involves a set of procedures designed to completely remove fecal residues and significantly reduce the bacterial flora in the colon with the least possible discomfort and risk for the patient2.
Thorough bowel cleansing is by most surgeons considered one of the most important factors in the prevention of complications3. In fact, since the days of Halsted, the presence of feces inside the colon has been viewed as a major cause of anastomotic dehiscence4. Not surprisingly, many authors believe preoperative bowel preparation is essential in the prevention of infectious complications following colorectal surgery5-8.
Based on the literature, it is difficult to determine exactly when preoperative bowel preparation became a standard procedure in colorectal surgery, but the earliest studies on colon and rectum cleansing were carried out by Maunsell in the early 1890s9.
However, in the 1990s, the use of bowel preparation as an indispensable preoperative procedure came into question, and criteria for when it ought to be avoided was proposed10. In addition, a number of studies documented the favorable evolution of patients submitted to emergency left colon resection with primary anastomosis without previous colon preparation, raising doubts about its indispensability11. It has been shown that under certain circumstances mechanical bowel preparation can actually stimulate bacterial growth and translocation, both of which favor the emergence of septic complications from colorectal surgery12. Other researchers believe mechanical colon preparation does not improve postoperative morbidity rates and may even increase the incidence of infectious complications, fistulas and hydroelectrolyte imbalance10. In a study with five years of follow-up, Fillmann, in 2001, reported lower fistula and infection rates among patients who were not submitted to preoperative bowel preparation13. Thus, to a number of authors, anastomosis may be performed safely without preoperative bowel preparation14,15.
The aim of the present study was to evaluate the efficacy of colocolonic anastomosis in dogs with and without preoperative bowel preparation.
MATERIALS AND METHODS
This study included 42 female dogs (Canis familiaris) weighing 8.416.9 kg, distributed at random in two groups of 21 animals each:
• Group I (control) animals with preoperative bowel preparation;
• Group II (study) animals not submitted to preoperative bowel preparation.
The animals in Group I (control) were submitted to preoperative bowel preparation with a 12% glycerin solution administered rectally one day before surgery.
Surgical technique once the animals were anesthetized, a digital rectal examination was performed individually to determine bowel preparation according to the classification proposed by O'Dweyr: excellent (absence of feces); good (presence of minimal fecal residue); acceptable (presence of liquid feces); soiled (presence of solid feces)16. The procedure consisted of a median transumbilical laparotomy, identification of the descending colon at 20 cm from the anal margin, and colotomy with sectioning of the entire colon circumference. In both groups, the colotomy was closed manually with a continuous single-layer extramucosal suture using polypropylene 30 thread.
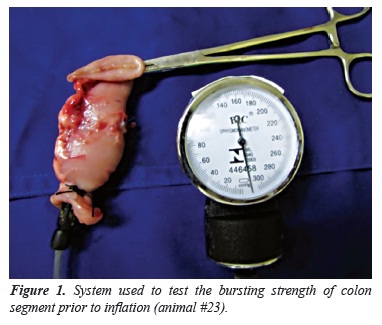
The animals were evaluated during the first 21 days after surgery concerning the presence of signs and symptoms of surgical site infection and other complications. On the 21st postoperative day (POD 21), the animals were euthanized and a second laparotomy was performed through the same incision. The anastomoses were evaluated with regard to integrity and the presence of fistulas and dehiscence, while the abdominal cavity was evaluated for adhesions using the classification proposed by Knightly: 0=no adhesions, 1=single thin and easily separable adhesion, 2=less extensive but weak adhesions which withstand traction poorly, 3=extensive visceral adhesions extending to abdominal wall, 4=numerous extensive and visceral adhesions involving the mesentery, bowel, omentum and abdominal wall17. A 6 cm-colon segment centered on the anastomosis was resected and cauterized at the proximal extremity using a urethral probe (#8.0). In order to determine the anastomotic bursting pressure, the proximal extremity of the colon segment was tied to a sphygmomanometer with two cotton threads (size 20) while the distal extremity was closed with Kelly forceps to prevent air from escaping (Figure 1).
Then the colon segment was inflated continuously with a manual bulb to a maximum pressure of 300 mmHg, or until the suture burst (Figure 2). The site of anastomotic disruption, if any, was examined and the respective pressure was registered.
The weight, colon preparation, postoperative clinical evolution, intra-abdominal adhesion score and anastomotic bursting pressure were registered for all the animals, and the two groups were compared.
RESULTS
One animal in each group (4.5%) died. The death in Group I (study) occurred on POD 7 due to anastomotic dehiscence. The death in Group II (control) occurred on POD 10 due to deep incisional infection at the surgical site and complete dehiscence of the abdominal wall with evisceration and intact anastomosis. The two groups did not differ with regard to dehiscence (p>0.05). Likewise, the observed difference in average weight did not reach statistical significance (p>0.05).
According to the O'Dweyr classification, bowel preparation was considered good in 70% and excellent in 30% of the animals in Group II.
The distribution of the animals according to intra-abdominal adhesion grade is shown in Graph 1. In Group I, adhesions were predominantly grade 2 (35%) and grade 3 (25%), while the distribution was more homogenous in Group II (grades 1, 2 and 3=25%; grade 4=20%). However, the difference was not statistically significant (p=0.5685). (Figure 3)
When testing the bursting strength by inflation at up to 300 mmHg, one colon segment from each group (5.0%) was disrupted, one at 270 mmHg (Group I) and one at 220 mmHg (Group II). The difference was not statistically significant (p>0.05) (Figure 4).
DISCUSSION
Female dogs were used in this study because they are easy to obtain and handle, their bowels are relatively similar to human bowels, and the size of the pelvic cavity is appropriate to test the procedure18. In addition, canine and human bowels also feature relatively similar intestinal microflora, blood supply and descending colon anatomy16.
On the average, the animals in Group I weighed more than the animals in Group II, but the difference was not statistically significant. Thus, body weight cannot be considered a determining factor in our sample.
The bowel preparation of the animals in Group I was successful, indicating that bowel cleansing with 12% glycerin solution 24 hours prior to surgery is efficient in dogs19.
There is still some discussion about the most appropriate way to perform anastomosis, whether to use a continuous single-layer suture or separate stitches, and which thread to use. The method adopted in this study (continuous single-layer extramucosal suture) is simple, swift and inexpensive. It is associated with impermeability and low levels of tissue inflammation, and is considered as safe as separate stitches20,21. Monofilament thread is preferred to multifilament thread which is known to favor the development of infections and inflammatory reactions14. The polypropylene thread used in this study is monofilament, has high tensile strength and is associated with very little inflammatory reaction22.
The mortality rate was similar in the two groups. Both the observed deaths were the result of infectious complications. One animal in Group I presented anastomotic dehiscence evolving towards peritonitis and died on POD 7. Another animal in Group II presented deep incisional infection at the surgical site leading to complete dehiscence of the abdominal wall and died on POD 10. These results suggest that mechanical bowel preparation prior to surgery does not reduce mortality in dogs submitted to colorectal anastomosis surgery14,15,23.
The grade of adhesions is an indirect measure of anastomotic complications and, consequently, of wound healing. Based on Knightly's classification of adhesions17, no significant differences between the groups were observed, indicating that mechanical bowel preparation did not influence the development of adhesions. This finding contradicts the notion that preoperative colon cleansing reduces the risk of contamination of the peritoneum and perianastomotic tissues, thereby minimizing the development and severity of adhesions2.
Studies on healing of intestinal sutures often employ mechanical parameters such as burst tension testing in which a bowel segment is distended with liquid or air up to a predetermined pressure level, or until it bursts17,24. In this study, the bowel segments tested were carefully centered on the anastomosis. Burst pressure is an efficient parameter to evaluate the healing of intestinal anastomoses provided the disruption occurs at the site of the anastomosis17,24. In our study, disruption occurred in one specimen from each group, thus no significant difference was observed. In conclusion, colocolonic anastomosis without previous bowel preparation was shown to be safe and efficacious, suggesting it is not an indispensable procedure in colorectal anastomosis surgery.
Submitted on: 11/27/2011
Approved on: 11/06/2011
Study carried out at Post-graduation program stricto sensu in Surgery, Surgery Department, School of Medicine, Universidade Federal do Ceará Fortaleza (CE), Brazil.
Financing source: none.
Conflict of interest: nothing to declare.
- 1. Hares MM, Alexander-Williams J. The effect of bowel preparation on colonic surgery. World J Surg 1982;2(6):175-81.
- 2. Habr-Gama A, Gama-Rodrigues JJ, Teixeira MG, Alves PRA, Ventura TCM, Quintanilha AG, et al. Preparo intestinal pela ingestão de manitol a 10%. Rev Bras Coloproct 1981;1(2):84-94.
- 3. Güenaga KF, Matos D, Wille-Jørgensen P. Preoperative mechanical bowel preparation in elective colorectal surgery. An update of systematic review of the literature and meta-analysis. J Coloproctol 2012;1(32):7-17.
- 4. Ravo B, Metwally N, Castera P, Polasnky PJ, Ger R. The importance of intraluminal anastomotic fecal contact and peritonitis in colonic anastomotic leakages. An experimental study. Dis Colon Rectum 1988;1(31):868-71.
- 5. Rosenberg IL, Graham NG, Dombal FT, Goligher JC. Preparation of the intestine in patients undergoing major large-bowel surgery, mainly for neoplasmas of the colon and rectum. Br J Surg 1971;58(4):266-9.
- 6. Irvin TT, Goligher JC. Aetiology of disruption of intestinal anastomoses. Br J Surg 1973;60(6):461-4.
- 7. Buffara JR, Brenner S, Souza FJ, Marchesini JB, Malafia O. Infecção em cirurgia colorretal. Estudo retrospectivo de 621 casos. Rev Bras Colo-Proct 1988;3(8):94-7.
- 8. Pitrez FAB. Pré e pós-operatório em cirurgia geral e especializada. 2a ed. Porto Alegre: Artmed; 2003. 266 p.
- 9. Graney MJ, Graney CM. Colorectal surgery from antiquity to the modern era. Dis Colon Rectum 1980;23(6):432-41.
- 10. Fillmann EEP, Fillmann LS, Fillmann HS. Cirurgia colorretal eletiva sem preparo. In: Habr-Gama A, Barone B. Atualização em coloproctologia. São Paulo: Sociedade Brasileira de Coloproctologia e Associação Latino-americana de Coloproctologia; 1995. p. 269-71.
- 11. Koruth NM, Krukowski ZH, Youngson GG, Hendry WS, Logie JR, Jones PF, et al. Intra-operative colonic irrigation in the management of left-sided large bowel emergencies. Br J Surg 1985;72(9):708-11.
- 12. Valarini R, Lemos R, Quintana LFC, Cordova LF, Cabrera PFA, Repka JD, et al. Estudo da translocação bacteriana após sutura primária do colo com e sem limpeza mecânica: trabalho experimental em cães. Rev Bras Coloproct 1998;18(1):22-9.
- 13. Fillmann LS, Perondi F, Fillmann HS, Fillmann EEP. Cirurgia eletiva para o câncer colo-retal sem preparo mecânico da luz intestinal: Análise após 5 anos de acompanhamento. Rev Bras Coloproct 2001;4(21):246-9.
- 14. Torres Neto JR, Fakhouri R, Menezes MVA, Santos JS, Prudente ACL, Monteiro JTS, et al. Estudo Histomorfométrico de Anastomoses Primárias de Cólon em Coelhos, Com e Sem Preparo Intestinal. Rev Bras Coloproct 2007;4(27):384-90.
- 15. Scabini S, Rimini E, Romairone E, Scordamaglia R, Damiani G, Pertile D, et al. Colon and rectal surgery for câncer without mechanical bowel preparation: onecenter ramdomized prospective trial. World J Surg Oncol 2010;8:35.
- 16. O'Dwyer PJ, Conway MC, McDermott EW, O'Higgins NJ. Effect of mechanical bowel preparation on anastomotic integrity following low anterior resection in dog. Br J Surg 1989;76(7):756-8.
- 17. Knigthly JJ, Agostino D, Cliffton EE. The effect of fibrinolisyn and heparin on the formation of peritoneal adhesions. Surgery 1962;52(4):250-8.
- 18. Regadas SMM, Regadas FSP, Rodrigues LV, Carvalho MCGS, Regadas Filho FSP. Modelo experimental de sutura manual em cólon de cão por vídeo-laparoscopia. Acta Cir Bras 2005;20(4):323-8.
- 19. Bezerra CRS. Fechamento do coto distal do cólon sigmóide comparando sutura contínua com lacre plástico. Estudo experimental em cães. [dissertation]. Fortaleza (CE): Universidade Federal do Ceará; 2010.
- 20. Regadas FSP, Castro Filho HF, Nicodemo AM, Morano JCOD, Sampaio ZS. Estudo comparativo entre sutura contínua e separada em anastomose cólica. Estudo experimental em ratos. Acta Cir Bras 1990;4:141-5.
- 21. Figueiredo AF. Efeitos da suplementação nutricional com glicina e com glutamina na cicatrização colônica em coelhos [dissertation]. Belo Horizonte (MG): Universidade Federal de Minas Gerais; 2007.
- 22. Ribeiro FJC. Avaliação qualitativa e quantitativa da resposta inflamatória comparando a ação do fio de polipropileno com o fio de poligliconato em anastomoses realizadas em colon de ratos [dissertation]. Fortaleza (CE): Universidade Federal do Ceará; 1998.
- 23. Feres O, Santos Jr JCM, Andrade JI. The role of mechanical bowel preparation for colonic resection and anastomosis: an experimental study. Int J Colorectal Dis 2001;16(6):353-6.
- 24. Gonçalves CG. Cicatrização de anastomose colônica e nutrição pré-operatória em ratos desnutridos: estudo tensiométrico e de deposição de colágeno [dissertation]. Curitiba (PR): Universidade Federal do Paraná; 2005.
Correspondence to:
Publication Dates
-
Publication in this collection
02 July 2013 -
Date of issue
Dec 2012
History
-
Received
27 Nov 2011 -
Accepted
11 June 2011