ABSTRACT
This research had the objective of reporting a clinical case in which the rehabilitation of tongue strength with biofeedback strategy was performed. This case report addresses a 20-year-old patient whose orofacial myofunctional evaluation revealed a severe decrease in the force of the anterior third of the tongue and changes in lingual mobility and coordination. The measurement of tongue pressure was performed using the Iowa Oral Performance Instrument (IOPI) during elevation, protrusion and lateralization, and it was verified a reduction in the values obtained in all measured directions, compared with normality patterns. We performed 11 sessions of therapy, with weekly frequency, using a biofeedback strategy that consisted of computer games controlled by the tongue. An instrument embedded in the oral cavity functioned as a joystick as the input method for specific digital games. The patient performed at home the isometric exercises of pressing the tip of the tongue against a spatula, exaggerated retraction of tongue, tongue tapering, and isotonic exercise of touching the commissures and lips alternately, daily. After eight sessions, in relation to the elevation pressure, there was an improvement of 28.6% for the apex and 7.1% for the dorsum. As for protrusion, there was an improvement of 123.5%. In the measurements of left and right lateralization, the values increased 53.8% and 7.4%, respectively. After twelve sessions, it was observed an improvement of 35.7%, 7.4%, 164%, 76.9% and 40.7% in relation to the initial evaluation, for apex elevation, dorsum elevation, protrusion, and lateralization to left and right, respectively. Despite the increase, values recommended in the literature as normal for sex and age were not reached after 12 therapy sessions.
Keywords
Tongue; Exercise Therapy; Rehabilitation; Muscle Strength; Speech, Language and Hearing Sciences
RESUMO
Esta pesquisa teve o objetivo de relatar um caso clínico em que foi realizada a reabilitação da força lingual com estratégia de biofeedback. Trata-se de uma paciente de 20 anos de idade, cuja avaliação miofuncional orofacial evidenciou diminuição grave de força do terço anterior da língua e alterações na mobilidade e na coordenação linguais. A quantificação da pressão lingual foi realizada por meio do Iowa Oral Performance Instrument durante a elevação, a protrusão e a lateralização, tendo se verificado redução nos valores obtidos em todas as direções medidas em comparação aos padrões de normalidade. Foram realizadas 11 sessões de terapia, com frequência semanal, utilizando estratégia de biofeedback que consistia em jogos computacionais acionados pela língua. Um instrumento encaixado na cavidade oral funcionava como um joystick, sendo método de entrada para jogos digitais específicos. Em casa, a paciente realizou exercícios isométricos de pressão de ponta de língua contra espátula, retração exagerada de língua, afilamento lingual e isotônico de tocar comissuras e lábios alternadamente, diariamente. Após oito sessões, em relação à pressão na elevação, houve melhora de 28,6% para o ápice e 7,1% para o dorso. Quanto à protrusão, houve melhora de 123,5%. Nas medidas de lateralizações esquerda e direita, os valores aumentaram 53,8% e 7,4%, respectivamente. Após 12 sessões, percebeu-se melhora, em relação à avaliação inicial, de 35,7%, 7,4%, 164%, 76,9% e 40,7%, para elevação de ápice, de dorso, protrusão, lateralizações esquerda e direita, respectivamente. Apesar do aumento, valores preconizados na literatura, como normalidade para o sexo e a idade, não foram atingidos com 12 sessões.
Descritores
Língua; Terapia por Exercício; Reabilitação; Força Muscular; Fonoaudiologia
INTRODUCTION
The tongue is an organ of the stomatognathic system with active participation in the functions of mastication, deglutition and speaking. It is composed of intrinsic and extrinsic muscles that act in synergy, promoting changes in its shape and position(11 Gilbert RJ, Napadow VJ, Gaige TA, Wedeen VJ. Anatomical basis of lingual hydrostatic deformation. J Exp Biol. 2007;210(23):4069-82. http://dx.doi.org/10.1242/jeb.007096. PMid:18025008.
http://dx.doi.org/10.1242/jeb.007096...
).
It is considered a muscular-hydrostat, as the trunk of elephants and the tentacles of cephalopod mollusks(22 Kier WM, Smith KK. Tongues, tentacles and trunks: the biomechanics and movement of muscular hydrostats. Zool J Linn Soc. 1985;83(4):307-24. http://dx.doi.org/10.1111/j.1096-3642.1985.tb01178.x.
http://dx.doi.org/10.1111/j.1096-3642.19...
). A muscular-hydrostat has its muscles arranged in three directions and presents constant volume. Thus, any shortening in one direction causes compensatory elongation in at least one other direction of the organ. For instance, the contraction of the transverse muscle causes elongation, which decreases the cross-section and increases the length, whereas the contraction of the longitudinal muscle causes shortening, which increases the height and width of the tongue(22 Kier WM, Smith KK. Tongues, tentacles and trunks: the biomechanics and movement of muscular hydrostats. Zool J Linn Soc. 1985;83(4):307-24. http://dx.doi.org/10.1111/j.1096-3642.1985.tb01178.x.
http://dx.doi.org/10.1111/j.1096-3642.19...
).
Most tongue movements, regardless of direction, require the simultaneous contraction of several muscle groups(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
), and for each direction that the tongue exerts force, different muscle groups are activated, with constant interaction between the extrinsic and intrinsic muscles in all functions performed by the tongue(44 Pittman LJ, Bailey EF. Genioglossus and intrinsic electromyographic activities in impeded and unimpeded protrusion tasks. J Neurophysiol. 2009;101(1):276-82. http://dx.doi.org/10.1152/jn.91065.2008. PMid:18987117.
http://dx.doi.org/10.1152/jn.91065.2008...
).
Given the importance of the tongue for the stomatognathic functions, speech-language pathologists perform detailed assessment of this structure in clinical practice, which usually includes the investigation of habitual posture, morphological aspects, frenulum, tonus and mobility(55 Marchesan IQ, Berretin-Félix G, Genaro KF. MBGR protocol of myofunctional evaluation with scores. Int J Orof Myol. 2012;38:38-77. PMid:23362752.).
Tongue tonus is defined as a natural state of muscle contraction(66 SBFa: Sociedade Brasileira de Fonoaudiologia. Comitê de Motricidade Orafacial [Internet]. Vocabulário técnico - cientifico em motricidade orofacial [citado em 2018 Ago 5]. Disponível em: http://www.sbfa.org.br/portal/pdf/dicionario_mfo.pdf
http://www.sbfa.org.br/portal/pdf/dicion...
). In skeletal muscles, such as those that compose the tongue, the tonus assists with maintaining posture(66 SBFa: Sociedade Brasileira de Fonoaudiologia. Comitê de Motricidade Orafacial [Internet]. Vocabulário técnico - cientifico em motricidade orofacial [citado em 2018 Ago 5]. Disponível em: http://www.sbfa.org.br/portal/pdf/dicionario_mfo.pdf
http://www.sbfa.org.br/portal/pdf/dicion...
). The strength of a muscle can be observed during contraction. In general, tongue strength is assessed qualitatively through the resistance protrusion task, where patients are asked to protrude their tongue and push it against the examiner's gloved finger and/or against a spatula vertically positioned a few centimeters away from the mouth(77 Rezende BA, Furlan RMMM, Las Casas EB, Motta AR. Avaliação clínica da língua em adultos jovens. Rev CEFAC. 2016;18(3):559-67. http://dx.doi.org/10.1590/1982-021620161832516.
http://dx.doi.org/10.1590/1982-021620161...
). Tongue strength, or force, can also be assessed by quantitative methods(88 Araújo TG, Rodrigues TM, Furlan RMMM, Las Casas EB, Motta AR. Avaliação da reprodutibilidade de um instrumento para medição da força axial da língua. CoDAS. 2018;30(3):1-7. http://dx.doi.org/10.1590/2317-1782/20182017191.
http://dx.doi.org/10.1590/2317-1782/2018...
), using instruments containing sensors that provide the value of the force exerted by the tongue against a surface. There are also instruments that provide the value of the pressure exerted by the tongue(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
), with pressure defined as the force exerted in a given direction per unit area(99 Doebelin EO. Measurement systems, application and design. 5th ed. New York: McGraw Hill; 2004.).
Tongue weakness is one of the causes of changes in function(1010 Stierwalt JAG, Youmans SR. Tongue measures in individuals with normal and impaired swallowing. Am J Speech Lang Pathol. 2007;16(2):148-56. http://dx.doi.org/10.1044/1058-0360(2007/019). PMid:17456893.
http://dx.doi.org/10.1044/1058-0360(2007...
). Counter-resistance exercises have been proven effective in rehabilitating tongue force, resulting in improved deglutition strength and functional performance in individuals with post-stroke dysphagia(1111 Robbins J, Kays SA, Gangnon RE, Hind JÁ, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88(2):150-8. http://dx.doi.org/10.1016/j.apmr.2006.11.002. PMid:17270511.
http://dx.doi.org/10.1016/j.apmr.2006.11...
). In healthy individuals, elevation, protrusion and lateralization exercises associated with counter-resistance resulted in increased tongue force in all three directions(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
).
Biofeedback technological resources can also be employed as an effective therapeutic strategy, and can increase patient compliance with treatment. In tongue exercise therapy, electromyography biofeedback(1212 Freitas GS, Mituuti CT, Furkim AM, Busanello-Stella AR, Stefani FM, Arone MMAS, et al. Electromyography biofeedback in the treatment of neurogenic orofacial disorders: systematic review of the literature. Audiol Commun Res. 2016;21:e1671. http://dx.doi.org/10.1590/2317-6431-2016-1671.
http://dx.doi.org/10.1590/2317-6431-2016...
) and the biofeedback provided by the Iowa Oral Performance Instrument (IOPI), an instrument that measures the pressure exerted by the oral structures(1111 Robbins J, Kays SA, Gangnon RE, Hind JÁ, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88(2):150-8. http://dx.doi.org/10.1016/j.apmr.2006.11.002. PMid:17270511.
http://dx.doi.org/10.1016/j.apmr.2006.11...
), stand out.
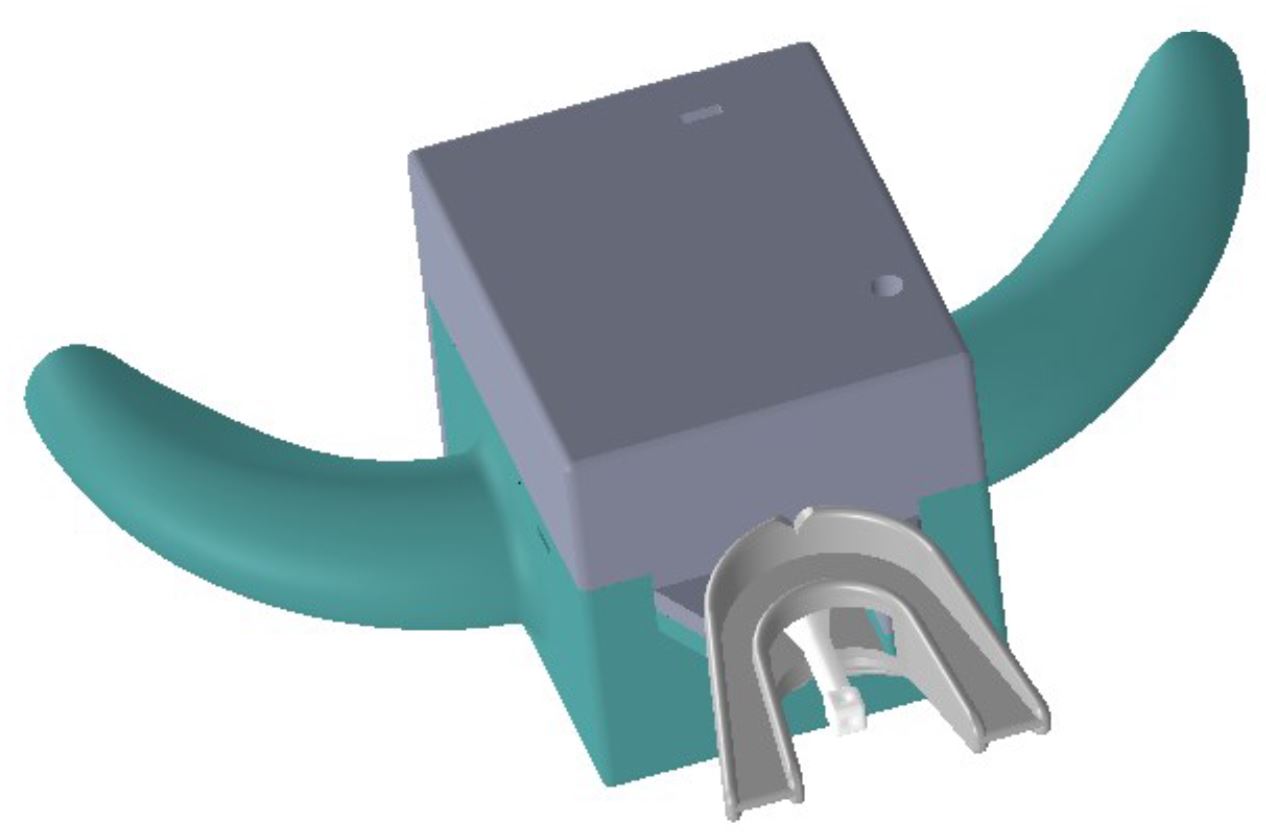
Recently, a Brazilian research group developed a biofeedback instrument that transforms traditional exercises into tongue-driven electronic games, motivated by the possibility of making myotherapy more enjoyable and improving patient adherence to treatment. Patients use an intraoral instrument that functions as a tongue-controlled joystick. On a computer monitor, the patient locates targets that appear in different regions of the screen and needs to move the cursor from the screen center to these targets. During the exercises, the patients perform tongue movements by pushing the joystick intraoral rod in the same direction of the target that appears on the screen, and the movement of the rod is proportional to that of the cursor on the screen. The speech-language pathologist can previously adjust the force to be exerted by the tongue to reach the targets, the force duration, and the number of movements to be performed.
Although the literature have cited biofeedback resources for tongue muscle rehabilitation, few studies show results using quantitative data. In this context, this study aimed to report a clinical case with the therapeutic purpose of rehabilitating tongue strength using a biofeedback instrument.
CASE REPORT
This case report addresses a 20-year-old female patient assisted by undergraduate students of the Speech-language Pathology Course at the Universidade Federal de Minas Gerais under the supervision of a SLP teacher with experience in the treatment of orofacial myofunctional disorders (OMD). The therapy occurred during a curricular internship in Orofacial Motricity. The Research Ethics Committee of the aforementioned Institution under protocol CAAE – 67187417.5.0000.5149, approved this case report and the patient signed an Informed Consent Form.
The patient started SLP therapy one month after being affected by idiopathic peripheral facial nerve palsy (formerly Bell’s palsy) on the left side, and progressed to full recovery of face movements, without synkinesis or contractures, after two months of therapy. During this period, she did not perform any exercises to repair changes in tongue tonus or mobility. The therapy, which comprised eight weekly held sessions, focused on performing movement-inducing massage associated with isometric contraction of the face muscles(1313 Goffi-Gomez MVS, Vasconcelos LGE, Bernardes DFF. Intervenção fonoaudiológica na paralisia facial. In: Ferreira LP, Befi-Lopes DM, Limongi SCO, organizadores. Tratado de fonoaudiologia. São Paulo: Roca; 2004. p. 512-26.), and the patient was instructed to alternate bilateral mastication as she showed preference for right-side chewing. When the patient returned for reevaluation after recovering face movements, the following changes were evidenced: severe decrease in strength of the anterior third of the tongue, incoordination of tongue movement, lowered tongue posture and complaints that suggested temporomandibular joint (TMJ) disorders associated with discomfort in the masticatory muscles, and cracking during mouth opening, in addition to decreased mandible laterality, presence of mandibular deviation during mouth opening and closing, and articulatory inaccuracy. The patient had neither muscular nor neurological diseases of genetic or degenerative origin. The protocol of Orofacial Myofunctional Evaluation MBGR was used in the pre- and post-therapy assessments.
Assessment of the tongue using the MBGR protocol(55 Marchesan IQ, Berretin-Félix G, Genaro KF. MBGR protocol of myofunctional evaluation with scores. Int J Orof Myol. 2012;38:38-77. PMid:23362752.) included the following assessment: habitual posture, symmetry, width, height, mucosa, frenulum, mobility and tonus. Evaluation of the frenulum showed extension and fixation on the tongue and floor of the mouth. As for mobility, the following tasks were requested: protrusion, touching the apex sequentially on the right and left commissures and upper and lower lips, touching the apex on the incisive papilla and right and left cheeks, snapping the apex, sucking the tongue on the palate and vibrating it. In addition, it was verified tongue force through sustained protrusion against a spatula.
In the clinical evaluation of the tongue, it was not possible to observe the habitual posture because the lips were at closed position, but its width, height and mucosa were adequate. There were no changes observed in the lingual frenulum. In the intraoral examination, the patient had a score of zero out of 17 in the MBGR.
In the mobility assessment, it was verified incoordination of tongue movements, evidenced by difficulty touching the apex sequentially in the right and left commissures and upper and lower lips, and difficulty in sucking and snapping the tongue. In the mobility examination, the patient had a score of 3 out of 16 in the MBGR. Sensitivity was reduced at the apex of the tongue. The patient reported not feeling this part of the tongue, and performed all movements with the tongue dorsum. Tongue tonus was decreased. We also observed severe reduction in force on the anterior third of the tongue in the counter-resistance task, as shown in Figure 1.
Regarding speech, the patient presented difficulty in producing vibrating and lingual alveolar phonemes. The production of such phonemes was adapted, with contact of the tongue dorsum with the alveolus and absence of movement of the apex of the tongue.
Tongue pressure was quantified using the Iowa Oral Performance Instrument (IOPI). The following pressure measurements were performed: anterior and posterior elevation, lateralization to the right and left, and protrusion. In order to measure anterior tongue pressure at elevation, the IOPI bulb was positioned over the tongue immediately behind the incisor teeth, and to measure posterior tongue pressure at elevation, the bulb was positioned so that its anterior border coincided with the mesial extremity of first molar(1414 Gingrich LL, Stierwalt JAG, Hageman CF, LaPointe LL. Lingual propulsive pressures across consistencies generated by the anteromedian and posteromedian tongue by healthy young adults. J Speech Lang Hear Res. 2012;55(3):960-72. http://dx.doi.org/10.1044/1092-4388(2011/10-0357). PMid:22232400.
http://dx.doi.org/10.1044/1092-4388(2011...
). Measurements of tongue pressure during lateralization and protrusion were performed with the bulb fixed to a support using double-sided adhesive tape. The support had a base where the bulb was fixed and two soft silicone surfaces that were bitten by the patient, stabilizing it. For lateralization, the support was positioned between the maxillary and mandibular premolars with the surface containing the bulb facing the tongue, whereas for protrusion, the support was positioned between the maxillary and mandibular incisors with the surface containing the bulb facing the tongue(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
). In all these measurements, we instructed the patient to press the bulb with the tongue as hard as possible for two seconds. The patient was not allowed to view the pressure values generated, which were shown on the IOPI screen.
For control purposes, pressure of the cheeks was also assessed using the IOPI. Evaluation of the cheeks aimed at knowing whether the strength of this structure would increase only with the effect of motor learning for the use of IOPI. Measurement of cheek pressure was performed with the bulb positioned between the maxillary and mandibular premolars with the surface containing the bulb facing the cheeks(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
), and the patient was asked to contract the cheeks pressing the bulb with maximum force for two seconds. The same speech-language pathologist with expertise in Orofacial Motricity, who also participated in the patient's rehabilitation process, performed all assessments and measurements.
For each of these measurements, three measures were obtained at 30-second intervals, and the highest value was considered. Tongue and cheek pressure measurements were performed at four moments: initial assessment, 8th and 12th weeks of intervention, and six months after SLP therapy discharge.
Assessment of tongue pressure using IOPI in the 1st session (Table 1) showed reduction in the values obtained in all measured directions compared with the normality standards(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
,1414 Gingrich LL, Stierwalt JAG, Hageman CF, LaPointe LL. Lingual propulsive pressures across consistencies generated by the anteromedian and posteromedian tongue by healthy young adults. J Speech Lang Hear Res. 2012;55(3):960-72. http://dx.doi.org/10.1044/1092-4388(2011/10-0357). PMid:22232400.
http://dx.doi.org/10.1044/1092-4388(2011...
). We also observed asymmetry in pressure, which means smaller values on the left and similar values in the anterior and posterior regions of the tongue, with probable influence of the tongue dorsum in the anterior measurement, as reported by the patient.
The therapy consisted on eleven weekly sessions, in which biofeedback strategies were proposed. In each session, the patient performed activities using an intraoral instrument, connected to a computer, which functioned as a joystick actuated by the tongue (Figure 2). This instrument was chosen aiming to include a challenge that would motivate the patient during the therapy.
The activities consisted of targets (fruits) that appeared in four regions of the computer screen (right, left, top and bottom) and should be reached when the patient performed a movement with the tongue and held it for a few seconds. In the first five sessions, 0.5 N force was required to move the joystick; in the 6th and 7th sessions, 1 N was needed; as of the 8th session, 2 N were required. Duration of muscle contraction began at 1 s and was gradually increased until 5 s for each strength level throughout the therapy. The patient performed twelve movements in each session, three in each direction. In the 6th, 7th and 10th sessions, the patient performed the activity more than once, as shown in Table 2. In the 8th and 12th sessions, the patient was reevaluated with regard to her performance in the game using the same set of parameters of the initial assessment, that is, 1 N force and 1 s muscle contraction duration.
Tongue strength and duration of tongue muscle contraction in the biofeedback activities throughout the SLP therapy
The patient was instructed to perform the following exercises at home three times a day: press the apex of the tongue against a spatula positioned between the maxillary and mandibular premolars in three series of 10 s; exaggerated tongue retraction in three series of 10 movements and tongue tapering in three series of 10 s; press the apex of the tongue against the palate in three series of 10 s; isotonic exercise touching the tongue on the upper and lower lips and right and left commissures, alternately and repeatedly, in ten series. The feedback on the exercises performed at home was visual, using a mirror. In the resistance tasks, the patient was asked to apply maximum pressure, without deformation of the anterior third of the tongue.
With respect to the other changes, the patient was instructed to eliminate inappropriate habits regarding tongue posture, and was referred to multidisciplinary evaluation specialized in TMJ. Concomitantly with myotherapy, during the sessions she performed strategies of myofunctional therapy with exercise of the articulatory positions of the altered phonemes.
Concerning tongue apex elevation, it improved 28.6% after eight sessions. As for tongue dorsum elevation, the improvement was of 7.1%. Regarding tongue protrusion, there was improvement of 123.5%. The values increased by 53.8 and 7.4% for lateralization to the left and right, respectively. After 12 sessions, we observed improvements of 35.7, 7.1, 164.7, 76.9 and 40.7% in relation to the initial assessment for apex and dorsum elevation, protrusion, and lateralization to the left and right, respectively. Table 1 shows the pressure measures obtained.
Despite the increase, the values recommended in the literature as normal for sex and age were not reached after 12 sessions (Figure 3). There was a clear improvement with respect to tongue contraction duration, and the patient was able to maintain tongue apex pressure on the palate without deformation (Figure 4), which was not possible at the initial assessment. Pressure of the cheeks remained virtually constant throughout the measurements, lower on left side.
Graph of tongue pressure measures throughout the SLP therapy and normality standard values(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009... ,1414 Gingrich LL, Stierwalt JAG, Hageman CF, LaPointe LL. Lingual propulsive pressures across consistencies generated by the anteromedian and posteromedian tongue by healthy young adults. J Speech Lang Hear Res. 2012;55(3):960-72. http://dx.doi.org/10.1044/1092-4388(2011/10-0357). PMid:22232400.
http://dx.doi.org/10.1044/1092-4388(2011... )
The patient's performance in the game was also noticeably improved. At the initial assessment, it took her of 23.9 s on average to reach the targets that required 0.5 N force and 1 s duration. Targets with the same levels of force and contraction duration were reached in only 1.9 and 2 s on average at the 2nd and 3rd evaluations, respectively.
After 12 sessions of SLP therapy, the patient showed improvement in all aspects compared with the initial assessment. There was considerable improvement in tongue mobility during mastication and speech, and the patient reported having less difficulty producing vibrating and lingual alveolar phonemes. She began to produce these phonemes with the apex of the tongue and correct articulatory position. Tongue mobility assessment in the MBGR showed a score of 0 out of 16. The signs and symptoms of TMJ changes disappeared, and the patient was discharged from SLP therapy.
DISCUSSION
This case report addresses a patient with idiopathic peripheral facial nerve palsy (formerly Bell’s palsy) on the left side. As consequences of facial paralysis, the literature reports unilateral mastication contralateral to the paralyzed side due to functional limitations resulting from flaccidity of the buccinator muscle and lip incompetence on the same side(1313 Goffi-Gomez MVS, Vasconcelos LGE, Bernardes DFF. Intervenção fonoaudiológica na paralisia facial. In: Ferreira LP, Befi-Lopes DM, Limongi SCO, organizadores. Tratado de fonoaudiologia. São Paulo: Roca; 2004. p. 512-26.,1515 Mory MR, Tessitore A, Pfeilsticker LN, Couto EB Jr, Paschoal JR. Mastication, deglutition and its adaptations in facial peripheral paralysis. Rev CEFAC. 2013;15(2):402-10. http://dx.doi.org/10.1590/S1516-18462012005000076.
http://dx.doi.org/10.1590/S1516-18462012...
), with this mastication pattern possibly being the triggering factor of TMJ dysfunction(1616 Alfaya TA, Tannure PN, Dip EC, Uemoto L, Barcelos R, Gouvêa CVD. Bell’s palsy and temporomandibular disorder association: clinical treatment. RFO UPF. 2012;17(2):222-7.).
Sassi et al.(1717 Sassi FC, Mangilli LD, Queiroz DP, Salomone R, Andrade CRF. Avaliação eletromiográfica e ultrassonográfica do músculo masseter em indivíduos com paralisia facial periférica unilateral. Arq Int Otorrinolaringol. 2011;15(4):478-85. http://dx.doi.org/10.1590/S1809-48722011000400012.
http://dx.doi.org/10.1590/S1809-48722011...
) verified reduction in the mandibular range of motion of individuals with facial palsy in the mouth opening, mandibular lateralization and protrusion tests, and suggested that TMJ functionality tests should be included in facial palsy assessments. Although the patient did not present unilateral mastication when reevaluated, this pattern was observed during facial palsy, and may have contributed to the TMJ-related findings. In contrast, the changes observed in the tongue assessments conducted with the patient (severe decrease in anterior third strength, movement incoordination, and lowered posture) cannot be explained by the facial palsy condition. The literature reports increased use of the tongue in individuals with facial palsy, especially for the paralyzed side, as compensation for residue removal in the oral vestibule(1515 Mory MR, Tessitore A, Pfeilsticker LN, Couto EB Jr, Paschoal JR. Mastication, deglutition and its adaptations in facial peripheral paralysis. Rev CEFAC. 2013;15(2):402-10. http://dx.doi.org/10.1590/S1516-18462012005000076.
http://dx.doi.org/10.1590/S1516-18462012...
). Moreover, the patient investigated did not present neurological or muscular disorders of degenerative or progressive nature that could explain the changes observed in the tongue.
In the tongue pressure task performed at the initial assessment, we observed reduced values in all directions(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
). Cheek force asymmetry was also verified, with the left side showing smaller pressure values probably as a consequence of peripheral facial nerve palsy.
In the present study, the patient presented gains in tongue pressure after eight and 12 weeks of SLP therapy using counter-resistance exercises, corroborating the literature. A study conducted with healthy elderly(1818 Robbins J, Gangnon RE, Shannon MT, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53(9):1483-9. http://dx.doi.org/10.1111/j.1532-5415.2005.53467.x. PMid:16137276.
http://dx.doi.org/10.1111/j.1532-5415.20...
) found significant increase in tongue pressure after eight weeks of therapy using counter-resistance exercises. In a subsequent research, Robbins et al.(1111 Robbins J, Kays SA, Gangnon RE, Hind JÁ, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88(2):150-8. http://dx.doi.org/10.1016/j.apmr.2006.11.002. PMid:17270511.
http://dx.doi.org/10.1016/j.apmr.2006.11...
) verified significant increase in maximal isometric pressure values measured with application of the IOPI in the anterior and posterior parts of the tongue, after four and eight weeks of therapy, using counter-resistance exercises in patients with dysphagia after stroke. In healthy individuals, increased tongue pressure was observed after a 9-week SLP therapy(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
).
This study shows greater gains in tongue pressure at the 9th week (28.6% for anterior elevation, 7.1% for dorsum elevation, 123.5% for protrusion, and 7.4 and 53.8% for lateralization to the right and left, respectively) than the findings described in the literature, probably due to the severe reduction in tongue strength found at the patient's initial assessment.
In a previous research(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
), the authors reported increases of 6, 13.4 and 26.6% in tongue elevation, protrusion and lateralization, respectively, after nine weeks of therapy. Another previous study(1919 Lazarus C, Logemann JA, Huang CF, Rademaker AW. Effects of two types of tongue strengthening exercises in young normals. Folia Phoniatr Logop. 2003;55(4):199-205. http://dx.doi.org/10.1159/000071019. PMid:12802092.
http://dx.doi.org/10.1159/000071019...
) verified a 12% increase in tongue elevation pressure in healthy young adults after a 4-week therapy using counter-resistance exercises. It is worth noting that these authors conducted their studies with healthy individuals with no tongue force impairments, thus the results cannot be directly compared. A study that reported tongue strength gain in patients with dysphagia after stroke found that the values increased by 63 and 76% for anterior and posterior elevation, respectively, after four weeks of therapy(1111 Robbins J, Kays SA, Gangnon RE, Hind JÁ, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88(2):150-8. http://dx.doi.org/10.1016/j.apmr.2006.11.002. PMid:17270511.
http://dx.doi.org/10.1016/j.apmr.2006.11...
), indicating that gains are greater in cases with more severe changes.
Another factor that differentiates the findings of the present research from those of studies that measured pre- and post-therapy tongue pressure was the frequency of exercise. Robbins et al.(1818 Robbins J, Gangnon RE, Shannon MT, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53(9):1483-9. http://dx.doi.org/10.1111/j.1532-5415.2005.53467.x. PMid:16137276.
http://dx.doi.org/10.1111/j.1532-5415.20...
) conducted a 30-exercise program performed three times daily, three days a week. Robbins et al.(1111 Robbins J, Kays SA, Gangnon RE, Hind JÁ, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88(2):150-8. http://dx.doi.org/10.1016/j.apmr.2006.11.002. PMid:17270511.
http://dx.doi.org/10.1016/j.apmr.2006.11...
) performed a training protocol with 10 exercise repetitions three times a day, three days a week. In the protocol used by Clark et al.(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
), the study participants performed three series of 10 exercise repetitions per day, seven days a week. In the survey conducted by Lazarus et al.(1919 Lazarus C, Logemann JA, Huang CF, Rademaker AW. Effects of two types of tongue strengthening exercises in young normals. Folia Phoniatr Logop. 2003;55(4):199-205. http://dx.doi.org/10.1159/000071019. PMid:12802092.
http://dx.doi.org/10.1159/000071019...
), the participants exercised five days a week. In contrast, in the present study, the participant performed the exercises daily three times a day, which may have contributed to the high tongue strength gain observed.
The cheek pressure measurements were not accompanied by muscle training and the results did not show any change over the course of therapy, even with motor learning, suggesting that the increased tongue pressure observed should not be attributed solely to the effect of motor learning by successive assessments. In the reassessment conducted six months after discharge from SLP therapy, we expected a decrease in tongue pressure values(33 Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062). PMid:19641080.
http://dx.doi.org/10.1044/1092-4388(2009...
). However, there was an increase in the pressure measures for anterior elevation and lateralization to the right and left, indicating that the patient, in addition to being able to maintain tongue tonus through adequacy of the functions, increased the values even more, although they still did not reach the normality standards reported in the literature.
The instrument used as a biofeedback in the therapy sessions proved to be an effective alternative for the patient, as it motivated her to exercise at home in order to succeed in the challenges with higher difficulty level at each session. The literature indicates that computer games are an important motivational resource for rehabilitation patients, and can be conducted with patients of any age. They have been increasingly explored in motor therapy programs(2020 Schimid M. Reinforcing motor re-training and rehabilitation through games: a machine-learning perspective. Front Neuroeng. 2009;2:1-2. http://dx.doi.org/10.3389/neuro.16.003.2009. PMid:19430596.
http://dx.doi.org/10.3389/neuro.16.003.2...
) because they increase patient adherence to treatment.
Importantly, in this study, the biofeedback instrument was used only during the SLP therapy sessions, thus the improvement in tongue strength is attributed to the daily traditional exercises performed by the patient at home. Nevertheless, the indirect role played by this instrument in motivation, with the possibility of quantifying improvement each week, was essential to the success achieved, as reported by the patient.
Results of this study show the effectiveness of orofacial myofunctional therapy. Myotherapy provided improvement in tongue tonus, which is important for maintaining an adequate habitual posture, whereas myofunctional therapy provided balance between the functions, which also contributes to maintain tongue tonus. However, as this is a case report, data cannot be generalized. The patient assessed in this study was assiduous and committed to treatment, which greatly contributed to the therapeutic success. A limitation of this study was the fact that the speech-language pathologist responsible for the initial assessment and reassessments also participated in the patient's rehabilitation process. Another limitation refers to the absence of studies conducted with individuals with the same diagnosis in the literature, which culminated in the use of data obtained from other populations for comparison.
CONCLUSION
It was clinically observed and proven, by pressure measurements, an evolution in tongue strength after a 12-week biofeedback therapy and myofunctional exercises.
-
Study conducted at Universidade Federal de Minas Gerais – UFMG - Belo Horizonte (MG), Brasil.
-
Financial support: nothing to declare.
REFERÊNCIAS
-
1Gilbert RJ, Napadow VJ, Gaige TA, Wedeen VJ. Anatomical basis of lingual hydrostatic deformation. J Exp Biol. 2007;210(23):4069-82. http://dx.doi.org/10.1242/jeb.007096 PMid:18025008.
» http://dx.doi.org/10.1242/jeb.007096 -
2Kier WM, Smith KK. Tongues, tentacles and trunks: the biomechanics and movement of muscular hydrostats. Zool J Linn Soc. 1985;83(4):307-24. http://dx.doi.org/10.1111/j.1096-3642.1985.tb01178.x
» http://dx.doi.org/10.1111/j.1096-3642.1985.tb01178.x -
3Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52(4):1034-47. http://dx.doi.org/10.1044/1092-4388(2009/08-0062) PMid:19641080.
» http://dx.doi.org/10.1044/1092-4388(2009/08-0062) -
4Pittman LJ, Bailey EF. Genioglossus and intrinsic electromyographic activities in impeded and unimpeded protrusion tasks. J Neurophysiol. 2009;101(1):276-82. http://dx.doi.org/10.1152/jn.91065.2008 PMid:18987117.
» http://dx.doi.org/10.1152/jn.91065.2008 -
5Marchesan IQ, Berretin-Félix G, Genaro KF. MBGR protocol of myofunctional evaluation with scores. Int J Orof Myol. 2012;38:38-77. PMid:23362752.
-
6SBFa: Sociedade Brasileira de Fonoaudiologia. Comitê de Motricidade Orafacial [Internet]. Vocabulário técnico - cientifico em motricidade orofacial [citado em 2018 Ago 5]. Disponível em: http://www.sbfa.org.br/portal/pdf/dicionario_mfo.pdf
» http://www.sbfa.org.br/portal/pdf/dicionario_mfo.pdf -
7Rezende BA, Furlan RMMM, Las Casas EB, Motta AR. Avaliação clínica da língua em adultos jovens. Rev CEFAC. 2016;18(3):559-67. http://dx.doi.org/10.1590/1982-021620161832516
» http://dx.doi.org/10.1590/1982-021620161832516 -
8Araújo TG, Rodrigues TM, Furlan RMMM, Las Casas EB, Motta AR. Avaliação da reprodutibilidade de um instrumento para medição da força axial da língua. CoDAS. 2018;30(3):1-7. http://dx.doi.org/10.1590/2317-1782/20182017191
» http://dx.doi.org/10.1590/2317-1782/20182017191 -
9Doebelin EO. Measurement systems, application and design. 5th ed. New York: McGraw Hill; 2004.
-
10Stierwalt JAG, Youmans SR. Tongue measures in individuals with normal and impaired swallowing. Am J Speech Lang Pathol. 2007;16(2):148-56. http://dx.doi.org/10.1044/1058-0360(2007/019) PMid:17456893.
» http://dx.doi.org/10.1044/1058-0360(2007/019) -
11Robbins J, Kays SA, Gangnon RE, Hind JÁ, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88(2):150-8. http://dx.doi.org/10.1016/j.apmr.2006.11.002 PMid:17270511.
» http://dx.doi.org/10.1016/j.apmr.2006.11.002 -
12Freitas GS, Mituuti CT, Furkim AM, Busanello-Stella AR, Stefani FM, Arone MMAS, et al. Electromyography biofeedback in the treatment of neurogenic orofacial disorders: systematic review of the literature. Audiol Commun Res. 2016;21:e1671. http://dx.doi.org/10.1590/2317-6431-2016-1671
» http://dx.doi.org/10.1590/2317-6431-2016-1671 -
13Goffi-Gomez MVS, Vasconcelos LGE, Bernardes DFF. Intervenção fonoaudiológica na paralisia facial. In: Ferreira LP, Befi-Lopes DM, Limongi SCO, organizadores. Tratado de fonoaudiologia. São Paulo: Roca; 2004. p. 512-26.
-
14Gingrich LL, Stierwalt JAG, Hageman CF, LaPointe LL. Lingual propulsive pressures across consistencies generated by the anteromedian and posteromedian tongue by healthy young adults. J Speech Lang Hear Res. 2012;55(3):960-72. http://dx.doi.org/10.1044/1092-4388(2011/10-0357) PMid:22232400.
» http://dx.doi.org/10.1044/1092-4388(2011/10-0357) -
15Mory MR, Tessitore A, Pfeilsticker LN, Couto EB Jr, Paschoal JR. Mastication, deglutition and its adaptations in facial peripheral paralysis. Rev CEFAC. 2013;15(2):402-10. http://dx.doi.org/10.1590/S1516-18462012005000076
» http://dx.doi.org/10.1590/S1516-18462012005000076 -
16Alfaya TA, Tannure PN, Dip EC, Uemoto L, Barcelos R, Gouvêa CVD. Bell’s palsy and temporomandibular disorder association: clinical treatment. RFO UPF. 2012;17(2):222-7.
-
17Sassi FC, Mangilli LD, Queiroz DP, Salomone R, Andrade CRF. Avaliação eletromiográfica e ultrassonográfica do músculo masseter em indivíduos com paralisia facial periférica unilateral. Arq Int Otorrinolaringol. 2011;15(4):478-85. http://dx.doi.org/10.1590/S1809-48722011000400012
» http://dx.doi.org/10.1590/S1809-48722011000400012 -
18Robbins J, Gangnon RE, Shannon MT, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53(9):1483-9. http://dx.doi.org/10.1111/j.1532-5415.2005.53467.x PMid:16137276.
» http://dx.doi.org/10.1111/j.1532-5415.2005.53467.x -
19Lazarus C, Logemann JA, Huang CF, Rademaker AW. Effects of two types of tongue strengthening exercises in young normals. Folia Phoniatr Logop. 2003;55(4):199-205. http://dx.doi.org/10.1159/000071019 PMid:12802092.
» http://dx.doi.org/10.1159/000071019 -
20Schimid M. Reinforcing motor re-training and rehabilitation through games: a machine-learning perspective. Front Neuroeng. 2009;2:1-2. http://dx.doi.org/10.3389/neuro.16.003.2009 PMid:19430596.
» http://dx.doi.org/10.3389/neuro.16.003.2009
Publication Dates
-
Publication in this collection
24 Oct 2019 -
Date of issue
2019
History
-
Received
01 Aug 2018 -
Accepted
10 Dec 2018