ABSTRACT
Introduction
The laryngeal cancer treatment causes significant changes in the quality of life.
Purpose
To assess and compare the vocal handicap and the coping strategies to deal with the vocal handicap resulting from supracricoid and total laryngectomy.
Methods
Analytical, prospective observational study of groups of subjects with the same disease. Seventeen subjects were assessed and divided in two groups; the first with eight male subjects submitted to supracricoid partial laryngectomy, with cricohyoidoepiglottopexy, mean age of 67,5; and a second group with nine subjects, two women and seven men, submitted to total laryngectomy, mean age of 64,3. All subjects answered the Vocal Handicap Index-10 (VHI-10) and the Coping Strategies in Dysphonia Protocol (PEED-27).
Results
The mean values of raw scores obtained with the VHI-10 by the two groups did not reveal significant differences, matching studies involving dysphonic patients. Both groups use an elevated number of coping strategies for vocal problems: the first group presented mean raw scores of 65,75 and the second group, 59,22.
Conclusion
The comparison between subjects submitted to supracricoid laryngectomy and total laryngectomy does not evidence differences concerning the self-assessment of voice, vocal handicap and coping strategies to deal with vocal problems. Both groups use more than the double of coping strategies for vocal problems, with a predominant focus on emotion.
Voice; Dysphonia; Quality of life; Laryngectomy; Self concept
RESUMO
Introdução
O tratamento para o câncer de laringe acarreta mudanças significativas na qualidade de vida.
Objetivo
Avaliar e comparar a desvantagem vocal e as estratégias de enfrentamento para lidar com o comprometimento vocal resultante de laringectomias supracricoide e total.
Métodos
Foram avaliados 17 sujeitos, divididos em dois grupos, sendo um com oito sujeitos, todos do gênero masculino, que se submeteram à laringectomia parcial supracricoide, com cricohioidoepiglotopexia, média de idade 67,5 anos, e um segundo grupo com nove sujeitos, sendo duas mulheres e sete homens, que se submeteram à laringectomia total, média de idade 64,3 anos. Todos responderam às questões do protocolo Índice de Desvantagem Vocal-10 (IDV-10) e do Protocolo de Estratégias de Enfrentamento na Disfonia (PEED-27).
Resultados
Os valores médios dos escores brutos obtidos no IDV-10, nos dois grupos, não revelaram diferenças, sendo os índices de desvantagem compatíveis com estudos de vozes disfônicas de diferentes tipos. Ambos os grupos utilizavam um número elevado de estratégias de enfrentamento do problema de voz. O primeiro grupo apresentou 65,75 como média de escores brutos e o segundo, 59,22.
Conclusão
A comparação entre sujeitos que se submeteram a laringectomia supracricoide e aqueles submetidos à laringectomia total não evidenciou diferenças, no que se refere à autoavaliação da voz, desvantagem vocal e estratégias de enfrentamento do problema de voz. Os dois grupos utilizavam mais que o dobro de estratégias de enfrentamento do problema de voz, com predomínio de foco na emoção.
Voz; Disfonia; Qualidade de vida; Laringectomia; Autopercepção
INTRODUCTION
Supracricoid partial laryngectomy (SCPL) has been pointed out as advantageous when compared to total laryngectomy (TL), especially considering that it aims to preserve part of the organ11. Gallo A, Manciocco V, Tropiano ML, Simonelli M, Marvaso V, D’Arcangelo E et al. Prognostic value of resection margins in supracricoid laryngectomy. Laryngoscope. 2004;114(4):616-21. https://doi.org/10.1097/00005537-200404000-00005.
https://doi.org/10.1097/00005537-2004040...
,22. Laudadio P, Presutti L, Dall’Olio D, Cunsolo E, Consalici R, Amorosa L et al. Supracricoid laryngectomies: long-term oncological and functional results. Acta Otolaryngol. 2006;126(6):640-9. https://doi.org/10.1080/00016480500469024
https://doi.org/10.1080/0001648050046902...
,33. Nakayama M, Okamoto M, Miyamoto S, Takeda M, Yokobori S, Masaki T et al. Supracricoid laryngectomy with cricohyoidoepiglotto-pexy or cricohyoido-pexy: experience on 32 patients. AurisNasus Larynx. 2008;35(1):77-82. https://doi.org/10.1016/j.anl.2007.04.018
https://doi.org/10.1016/j.anl.2007.04.01...
,44. Alicandri-Ciufelli M, Piccinini A, Bergamini G, Ruberto M, Ghidini A, Marchioni D et al. Atypical neoglottis after supracricoid laryngectomy: a morphological and functional analysis. Eur Arch Otorhinolaryngol. 2011;268(7):1029-34. https://doi.org/10.1007/s00405-011-1556-4
https://doi.org/10.1007/s00405-011-1556-...
,55. Szyfter W, Leszczynska M, Wierzbicka M. Outcome after supracricoid laryngectomies in the material of ENT Department, Poznan University of Medical Sciences. Eur Arch Otorhinolaryngol. 2011;268(6):879-83. https://doi.org/10.1007/s00405-011-1513-2
https://doi.org/10.1007/s00405-011-1513-...
,66. Castro A, Sanchez-Cuadrado I, Bernaldez R, Del Palacio A, Gavilan J. Laryngeal function preservation following supracricoid partial laryngectomy. Head Neck. 2012;34(2):162-7. https://doi.org/10.1002/hed.21703
https://doi.org/10.1002/hed.21703...
,77. Vincentiis M, De Virgilio A, Bussu F, Gallus R, Gallo A, Bastanza G et al. Oncologic results of the surgical salvage of recurrent laryngeal squamous cell carcinoma in a multicentric retrospective series: emerging role of supracricoid partial laryngectomy. Head Neck. 2015;37(1):84-91. https://doi.org/10.1002/hed.23563
https://doi.org/10.1002/hed.23563...
. Survival rates of SCPL are similar to the TL ones66. Castro A, Sanchez-Cuadrado I, Bernaldez R, Del Palacio A, Gavilan J. Laryngeal function preservation following supracricoid partial laryngectomy. Head Neck. 2012;34(2):162-7. https://doi.org/10.1002/hed.21703
https://doi.org/10.1002/hed.21703...
,88. Moyano JAM, Gutiérrez RS, Nogueras JR, Aumente PO, Villarejo PL. Calidad de vida em pacientes tratados mediante laringectomía parcial supracricoidea com cricohioidoepiglotopexia (CHEP). Acta Otorrinolaringol Esp. 2004;55(9):409-14. https://doi.org/10.1016/S0001-6519(04)78545-3
https://doi.org/10.1016/S0001-6519(04)78...
, although it may benefit the patient by not using permanent tracheostomy. The vocal quality after SCPL is characterized as hoarse and breathy22. Laudadio P, Presutti L, Dall’Olio D, Cunsolo E, Consalici R, Amorosa L et al. Supracricoid laryngectomies: long-term oncological and functional results. Acta Otolaryngol. 2006;126(6):640-9. https://doi.org/10.1080/00016480500469024
https://doi.org/10.1080/0001648050046902...
, however intelligible, allowing the patient to keep an effective voice for his communication11. Gallo A, Manciocco V, Tropiano ML, Simonelli M, Marvaso V, D’Arcangelo E et al. Prognostic value of resection margins in supracricoid laryngectomy. Laryngoscope. 2004;114(4):616-21. https://doi.org/10.1097/00005537-200404000-00005.
https://doi.org/10.1097/00005537-2004040...
and has low impact on social activities, contributing for a better quality of life11. Gallo A, Manciocco V, Tropiano ML, Simonelli M, Marvaso V, D’Arcangelo E et al. Prognostic value of resection margins in supracricoid laryngectomy. Laryngoscope. 2004;114(4):616-21. https://doi.org/10.1097/00005537-200404000-00005.
https://doi.org/10.1097/00005537-2004040...
,33. Nakayama M, Okamoto M, Miyamoto S, Takeda M, Yokobori S, Masaki T et al. Supracricoid laryngectomy with cricohyoidoepiglotto-pexy or cricohyoido-pexy: experience on 32 patients. AurisNasus Larynx. 2008;35(1):77-82. https://doi.org/10.1016/j.anl.2007.04.018
https://doi.org/10.1016/j.anl.2007.04.01...
,44. Alicandri-Ciufelli M, Piccinini A, Bergamini G, Ruberto M, Ghidini A, Marchioni D et al. Atypical neoglottis after supracricoid laryngectomy: a morphological and functional analysis. Eur Arch Otorhinolaryngol. 2011;268(7):1029-34. https://doi.org/10.1007/s00405-011-1556-4
https://doi.org/10.1007/s00405-011-1556-...
,55. Szyfter W, Leszczynska M, Wierzbicka M. Outcome after supracricoid laryngectomies in the material of ENT Department, Poznan University of Medical Sciences. Eur Arch Otorhinolaryngol. 2011;268(6):879-83. https://doi.org/10.1007/s00405-011-1513-2
https://doi.org/10.1007/s00405-011-1513-...
,99. Decotte A, Woisard V, Percodani J, Pessey JJ, Serrano E, Vergez S. Respiratory complications after supracricoid partial laryngectomy. Eur Arch Otorhinolaryngol. 2010;267(9):1415-21. https://doi.org/10.1007/s00405-010-1238-7
https://doi.org/10.1007/s00405-010-1238-...
,1010. Kucuk H, Kurnaz SC, Kutlar G. Treatment expectations and quality of life outcomes of patients with laryngeal cancer based on different treatment methods. Eur Arch Otorhinolaryngol. 2015;272(5):1245-50. https://doi.org/10.1007/s00405-014-3066-7
https://doi.org/10.1007/s00405-014-3066-...
.
The TL, however, is still one of the main procedures in the treatment of laryngeal cancer and the patient needs to learn a new way of verbal communication and deal with breathing and swallowing changes, which will certainly interfere in his life1111. Eadie TL, Bowker BC. Coping and quality of life after total laryngectomy. Otolaryngol Head Neck Surg. 2012;146(6):959-65. https://doi.org/10.1177/0194599812437315
https://doi.org/10.1177/0194599812437315...
.
Regardless the chosen surgical modality, the larynx cancer treatment results in changes in patient’s daily life activities, significantly altering its quality1212. Vakharia KT, Ali MJ, Wang SJ. Quality-of-life impact of participation in a head and neck cancer support group. Otolaryngol Head Neck Surg. 2007;136(3): 405-10. https://doi.org/10.1016/j.otohns.2006.10.018
https://doi.org/10.1016/j.otohns.2006.10...
,1313. Moore KA, Ford PJ, Farah CS. ‘’I have quality of life…but…’’: exploring support need important to quality of life in head and neck cancer. Eur J OncolNurs. 2014;18(2):192-200. https://doi.org/10.1016/j.ejon.2013.10.010
https://doi.org/10.1016/j.ejon.2013.10.0...
and jeopardizing primordial functions of social life88. Moyano JAM, Gutiérrez RS, Nogueras JR, Aumente PO, Villarejo PL. Calidad de vida em pacientes tratados mediante laringectomía parcial supracricoidea com cricohioidoepiglotopexia (CHEP). Acta Otorrinolaringol Esp. 2004;55(9):409-14. https://doi.org/10.1016/S0001-6519(04)78545-3
https://doi.org/10.1016/S0001-6519(04)78...
,1313. Moore KA, Ford PJ, Farah CS. ‘’I have quality of life…but…’’: exploring support need important to quality of life in head and neck cancer. Eur J OncolNurs. 2014;18(2):192-200. https://doi.org/10.1016/j.ejon.2013.10.010
https://doi.org/10.1016/j.ejon.2013.10.0...
,1414. Campos RJDS, Leite ICG. Qualidade de vida e voz pós-radioterapia: repercussões para a fonoaudiologia. Rev CEFAC. 2010;12(4):671-77. https://doi.org/10.1590/S1516-18462010005000038
https://doi.org/10.1590/S1516-1846201000...
in which voice plays a prominent role.
The quality of life (QoL) may be considered as the way an individual deals satisfactory or unsatisfactory with several aspects of his daily life, considering his wellbeing, beliefs, personal and spiritual satisfactions1212. Vakharia KT, Ali MJ, Wang SJ. Quality-of-life impact of participation in a head and neck cancer support group. Otolaryngol Head Neck Surg. 2007;136(3): 405-10. https://doi.org/10.1016/j.otohns.2006.10.018
https://doi.org/10.1016/j.otohns.2006.10...
,1515. Rogers SN. Quality of life perspectives in patients with oral cancer. Oral Oncol. 2010;46(6):445-7. https://doi.org/10.1016/j.oraloncology.2010.02.021
https://doi.org/10.1016/j.oraloncology.2...
,1616. Melo Filho MR, Rocha BA, Pires MBO, Fonseca ES, Freitas EM, Martelli Jr H et al. Qualidade de vida de pacientes com carcinoma em cabeça e pescoço. Braz J Otorhinolaryngol. 2013;79(1):82-9. https://doi.org/10.5935/1808-8694.20130014
https://doi.org/10.5935/1808-8694.201300...
. The assessment process may involve four main domains: physical and psychological functioning, social interaction and symptoms related to the disease treatment1515. Rogers SN. Quality of life perspectives in patients with oral cancer. Oral Oncol. 2010;46(6):445-7. https://doi.org/10.1016/j.oraloncology.2010.02.021
https://doi.org/10.1016/j.oraloncology.2...
.
The way the patient deals with the disease significantly influences the treatment and results1717. Oliveira G, Hirani SP, Epstein R, Yazigi L, Behlau M. Coping strategies in voice disorders of a Brazilian population. J Voice. 2012;26(2):205-13. https://doi.org/10.1016/j.jvoice.2010.10.023
https://doi.org/10.1016/j.jvoice.2010.10...
,1818. Zambon F, Moreti F, Behlau M. Coping strategies in teachers with vocal complaint. J Voice. 2014;28(3):341-8. https://doi.org/10.1016/j.jvoice.2013.11.008
https://doi.org/10.1016/j.jvoice.2013.11...
. He will have to deal with the laryngectomy impairments, requiring coping. It is vital that the patient makes an effort to face the situation in order to reestablish the appropriate psychic balance1919. Chaves EC, Cade NV, Montovani MF, Leite RCBO, Spire WC. Coping: significados, interferência no processo saúde-doença e relevância para a enfermagem. Rev Esc Enferm USP. 2000;34(4):370-5. https://doi.org/10.1590/S0080-62342000000400008
https://doi.org/10.1590/S0080-6234200000...
.
This study aimed to assess and compare the vocal handicap and coping strategies in two groups of patients, after supracricoid partial laryngectomy and after total laryngectomy.
METHODS
This analytical, descriptive, prospective open study assessed 17 subjects with the same disease divided in two groups. The first group comprised eight patients submitted to SCPL with cricohyoidoepiglottopexy (CHEP), all male ranging in age from 55 to 76 years, mean age of 67,5 years. The second group comprised nine subjects submitted to TL, seven men and two women, ranging in age from 59 to 82 years, mean age of 64,3 years. Two subjects of this group used tracheoesophageal prosthesis, two used esophageal speech and two used electrolarynx.
All subjects attended the Speech Language Services of the Head and Neck Surgery Ambulatory of a private school-hospital in Campinas city (SP). All participants were retired, literate, with an average schooling of elementary school, complete or not.
At the time of the study, subjects were in process of assisted discharged and were considered as presenting functional communication, which was an inclusion criteria for the study. The mean post-surgical time of subjects submitted to SCPL was two years and two months and the mean post-surgical time of subjects submitted to TL was three years and six months. Most of the patients had unilateral or bilateral cervical emptying (five SCPL and seven TL), however it was not the focus of the study to compare such situation.
Eligible subjects were included in the study if they met the following criteria: undergone SCPL or TL; willingness to participate in the study; general health under control at the time of the study; no cancer recurrence or other impairments or morbidities interfering with quality of life, considering only the limitations due to the surgery for laryngeal cancer; retired or not; absence of dysphagia or adapted swallowing; not in use of feeding probe.
Subjects from both groups answered the Voice Handicap Index-10 (VHI-10)2020. Costa T, Oliveira G, Behlau M. Validação do índice de Desvantagem Vocal: 10 (IDV-10) para o português brasileiro. CoDAS. 2013;25(5):482-5. https://doi.org/10.1590/S2317-17822013000500013
https://doi.org/10.1590/S2317-1782201300...
and the Dysphonia Coping Strategy Protocol (PEED-27)2121. Oliveira G, Hirani SP, Epstein R, Yazigi L, Behlau M. Validation of the Brazilian version of voice disability coping questionnaire. J Voice. 2016;30(2):247. https://doi.org/10.1016/j.jvoice.2015.01.004
https://doi.org/10.1016/j.jvoice.2015.01...
. All questions of the protocols were read by a researcher and subjects had to choose the answer according to his self-perception.
Material
The Vocal Handicap Index – 10 (VHI-10) is a shorter version of VHI, translated and adapted to Brazilian Portuguese2020. Costa T, Oliveira G, Behlau M. Validação do índice de Desvantagem Vocal: 10 (IDV-10) para o português brasileiro. CoDAS. 2013;25(5):482-5. https://doi.org/10.1590/S2317-17822013000500013
https://doi.org/10.1590/S2317-1782201300...
. VHI-10 was developed, maintaining the 10 most clinically relevant questions. The instrument produces a total single score arrived at by a summation of scores allocated to different responses to items/ questions that range from 0 to 40 points, with 0 indicating no disadvantage and 40 indicating maximum disadvantage. A study showed that the VHI-10 is a robust tool to evidence the impacts of dysphonia in the individual’s life2222. Rosen CA, Lee AS, Osborne J, Zullo T, Murry T. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114(9):1549-56. https://doi.org/10.1097/00005537-200409000-00009
https://doi.org/10.1097/00005537-2004090...
.
The Dysphonia Coping Strategy Protocol (PEED-27) was translated and into Brazilian Portuguese and validated1717. Oliveira G, Hirani SP, Epstein R, Yazigi L, Behlau M. Coping strategies in voice disorders of a Brazilian population. J Voice. 2012;26(2):205-13. https://doi.org/10.1016/j.jvoice.2010.10.023
https://doi.org/10.1016/j.jvoice.2010.10...
. It is a self-assessment instrument consisting of 27 items developed specifically to evaluating the strategies that people with voice disorders use to face their voice problem. The items are evaluated at a scale of 6 points that analyzes the frequency of use of the strategy. The score produced by the protocol can range from 0 to 135, with 0 indicating no use of strategies and 135, use of all strategies. The items of the questionnaire are categorized in two types of coping strategies, problem-focused and emotion-focused. Items 2, 4, 7, 8, 11, 13, 14, 24, 25 and 26 correspond to problem-focused strategies and are related to efforts used to modify the stress source. Emotion-focused strategies correspond to items 1, 3, 5, 6, 9, 10, 12, 15, 16, 17, 18, 19, 20, 21, 22, 23 and 27 and are attempts to regulate emotional stress caused by the stressing agent
Ethical aspects
The study was approved by the Research Ethics Committee with Human Beings of the Pontifícia Universidade Católica de Campinas, Nº 394.430, CAAE 17671513.1.0000.5481. All subjects were informed about the study details and, after understanding the procedures that would be performed, they signed the informed consent term and kept a copy of it.
RESULTS
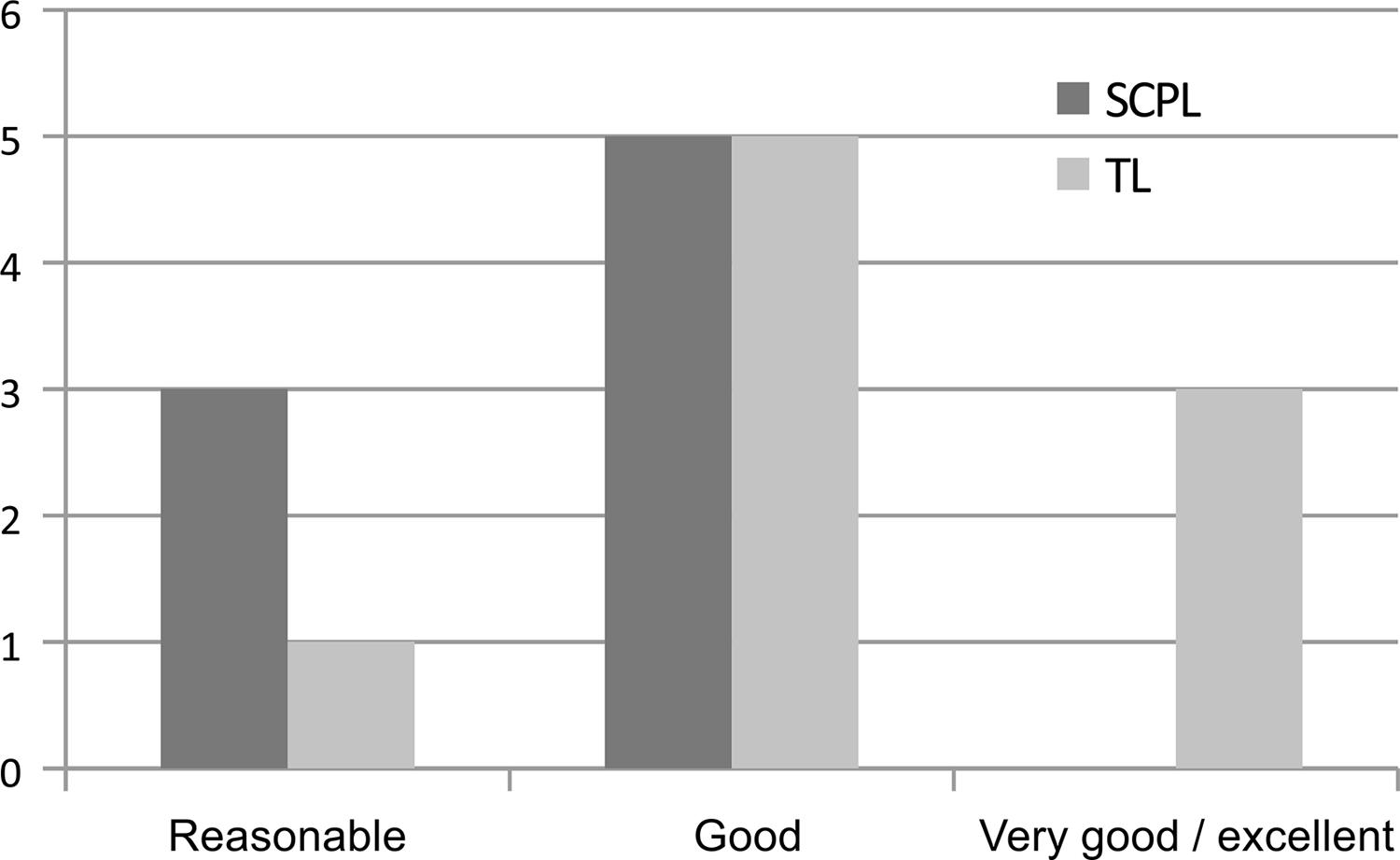
Subjects from the SCPL group evaluated their voices from reasonable to good, with predominance of good, and subjects from the TL group from reasonable to very good, also with predominance of good (Figure 1). The exact test of Fischer revealed p=0.385 in the comparison of both groups.
Self-assessment of vocal quality performed by groups supracricoid partial laryngectomy and total laryngectomy
The averages obtained by the two groups regarding VHI-10 questions with their respective p values are presented in Table 1.
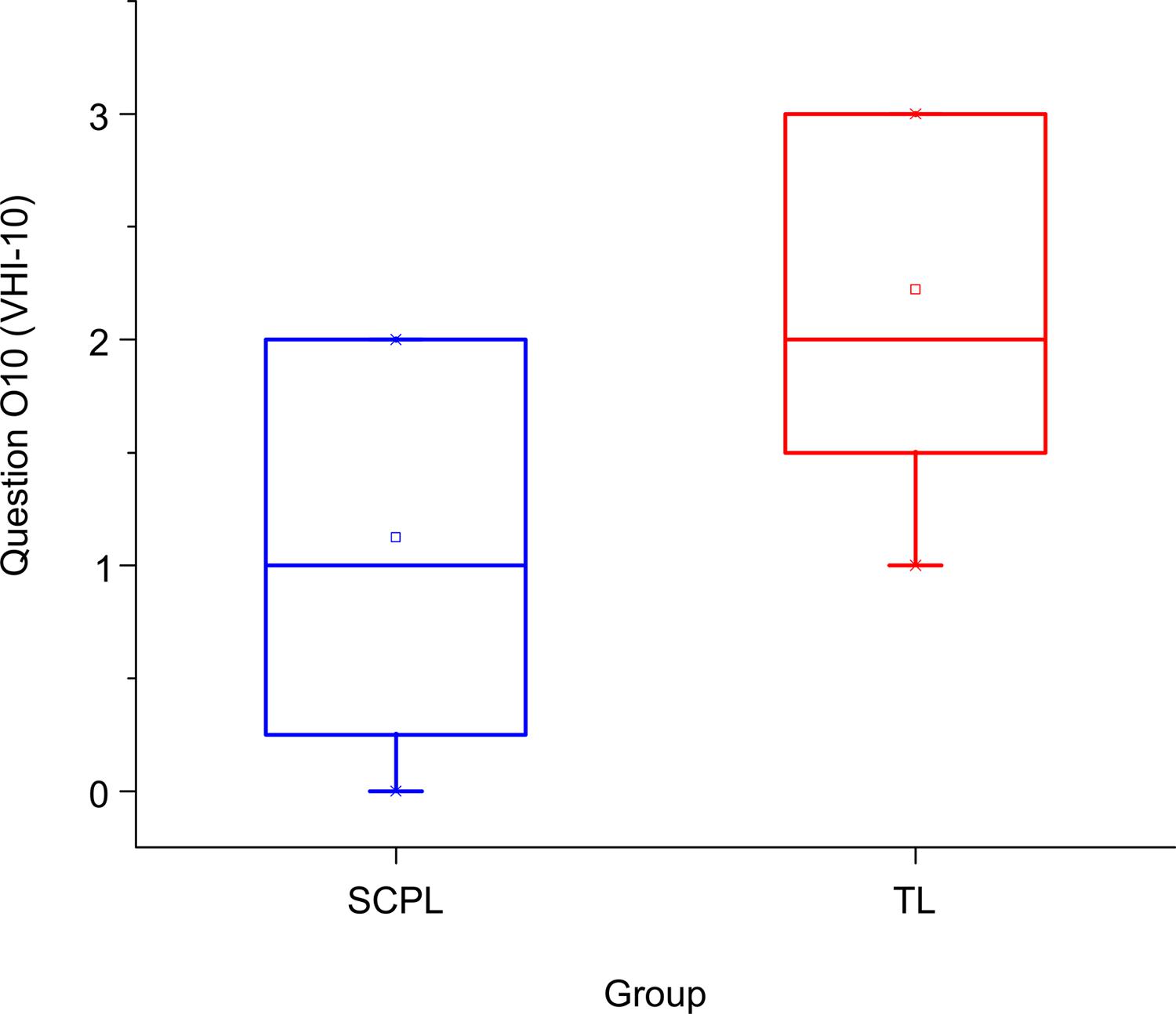
The average raw scores results of VHI-10 show that the SCPL group had average value of 9,0 and the TL group, 12,7 (Figure 2). Comparing the two groups regarding the raw average values of VHI-10, the Mann-Whitney/Wilcoxon test revealed p=0.175. Highlights to answers given to question O10 of the instrument -“People ask: what’s wrong with your voice?”, where p=0.024 (Figure 3).
Results of the Vocal Handicap Index-10 raw scores averages obtained by the supracricoid partial laryngectomy and the total laryngectomy groups
Results of Question O10 of the Vocal Handicap Index-10: supracricoid partial laryngectomy and the total laryngectomy group averages
The average raw scores obtained by SCPL and TL groups concerning PEED-27 protocol were 65,75 and 59,22, respectively. Comparing those scores, the Mann-Whitney/Wilcoxon test revealed p=0.359. Concerning the problem-focused domain, the value was p=0.101 and concerning the emotion-focused domain it was p=0.923 (Table 2).
Results of the PEED-27 protocol regarding both, problem-focused and emotion-focused strategies, are described in Tables 3 and 4.
DISCUSSION
Results of this study showed that the SCPL group assessed their voices from reasonable to good, while in the TL group there were concepts of reasonable to very good. Attention is drawn to the tendency of both groups to make positive self-assessments, considering the extension of supracricoid partial laryngectomy, or even the total removal of the organ, which generates the laryngeal voice alaryngeal.
Previous studies confirmed the tendency of patients with dysphonia to assess their own voice as being of good quality after a partial laryngectomy2323. Oliveira IB, Augusti ACV, Siqueira DM. Avaliação de voz e qualidade de vida após laringectomia supracricóide. Audiol Commun Res. 2013;18(4):353-60. https://doi.org/10.1590/S2317-64312013000400018
https://doi.org/10.1590/S2317-6431201300...
. One must take into account other factors that may be influencing such self-concept since laryngectomy surgeries, partial and total, severely alter the laryngeal structure, or remove part of the organ, jeopardizing the vocal quality intensively, or leading patients to seek for substitutive phonation with esophageal speech, tracheoesophageal prosthesis, etc.
Studies show divergences of opinions concerning vocal quality, considering that communication goes beyond an impaired voice2424. Schindler A, Favero E, Nudo S, Albera R, Schindler O, Cavalot AL. Long-term voice and swallowing modificaitons after supracricoidlaryngectomy: objective, subjective, and self-assessment data. Am J Otolaryngol. 2006;27(6):378-83. https://doi.org/10.1016/j.amjoto.2006.01.010
https://doi.org/10.1016/j.amjoto.2006.01...
,2525. Schindler A, Mozzanica F, Ginocchio D, Invernizzi A, Peri A, Ottaviani F. Voice-related quality of life in patients after total and partial laryngectomy. Auris Nasus Larynx. 2012;39(1):77-83. https://doi.org/10.1016/j.anl.2011.03.009
https://doi.org/10.1016/j.anl.2011.03.00...
,2626. Saito K, Akari K, Ogawa K, Shiotani A. Laryngeal function after supracricoid laryngectomy. Otolaryngol Head Neck Surg. 2009;140(4):487-92. https://doi.org/10.1016/j.otohns.2008.12.036
https://doi.org/10.1016/j.otohns.2008.12...
. Some authors defended the patients’ satisfaction with their voice in the presence of an intelligible communication44. Alicandri-Ciufelli M, Piccinini A, Bergamini G, Ruberto M, Ghidini A, Marchioni D et al. Atypical neoglottis after supracricoid laryngectomy: a morphological and functional analysis. Eur Arch Otorhinolaryngol. 2011;268(7):1029-34. https://doi.org/10.1007/s00405-011-1556-4
https://doi.org/10.1007/s00405-011-1556-...
,2424. Schindler A, Favero E, Nudo S, Albera R, Schindler O, Cavalot AL. Long-term voice and swallowing modificaitons after supracricoidlaryngectomy: objective, subjective, and self-assessment data. Am J Otolaryngol. 2006;27(6):378-83. https://doi.org/10.1016/j.amjoto.2006.01.010
https://doi.org/10.1016/j.amjoto.2006.01...
,2727. Anchette D, Menezes MB, Nakay MY, Prandini B, Kikuchi W, Gonçalves AJ. Avaliação da qualidade de vida dos pacientes com câncer de laringe no pós-operatório tardio. Soc Bras Psico Oncol. 2009;4(3):1-6.. Others defended that the most affected aspect was communication, which is responsible for the worst impacts upon quality of life88. Moyano JAM, Gutiérrez RS, Nogueras JR, Aumente PO, Villarejo PL. Calidad de vida em pacientes tratados mediante laringectomía parcial supracricoidea com cricohioidoepiglotopexia (CHEP). Acta Otorrinolaringol Esp. 2004;55(9):409-14. https://doi.org/10.1016/S0001-6519(04)78545-3
https://doi.org/10.1016/S0001-6519(04)78...
. It is important to stress that, in this study, all patients had already gone through speech therapy, which may have contributed for adaptation strategies of the new voice and for a functional communication in both groups.
The HVI-10 average raw values obtained in both groups did not reveal difference, but showed compatibility with different types of voice impairment, corroborating a validation study of the HVI-102222. Rosen CA, Lee AS, Osborne J, Zullo T, Murry T. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114(9):1549-56. https://doi.org/10.1097/00005537-200409000-00009
https://doi.org/10.1097/00005537-2004090...
, in which the average values found for patients without vocal complaint were 1,0 and raw scores varying from 8,0 to 28,0 points for patients with functional dysphonia and vocal folds palsy. However, in the mentioned study there were no cases of dysphonia by larynx carcinoma and the scores found in the present study were lower than most of the dysphonia cases studied.
Only one question from the organic domain of the HVI-10 (O10) revealed difference between the two groups. The question “People ask: what’s wrong with your voice?” revealed greater disadvantage to the TL group, which may be justified if considering the significant voice modification for the listener. In the TL group, most of the subjects used the tracheoesophageal prosthesis which seals the tracheostomy digitally when speaking, raising people’s curiosity. The same may occur with the electronic larynx which also modifies the phonation source differing it from a laryngeal voice.
Concerning the elevated number of strategies used by both groups for coping with the vocal problem, results (Table 2) agree with those found in the study mentioned previously2222. Rosen CA, Lee AS, Osborne J, Zullo T, Murry T. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114(9):1549-56. https://doi.org/10.1097/00005537-200409000-00009
https://doi.org/10.1097/00005537-2004090...
. It may be emphasized that there were no differences between the average raw scores found in both groups, which is in agreement with a study that verified, using PEED-27, that subjects with vocal complaint used more than the double of coping strategies than the general population. According to the study, the average total score of the group with vocal complaint was 51,86 and of the general population it was 23,181717. Oliveira G, Hirani SP, Epstein R, Yazigi L, Behlau M. Coping strategies in voice disorders of a Brazilian population. J Voice. 2012;26(2):205-13. https://doi.org/10.1016/j.jvoice.2010.10.023
https://doi.org/10.1016/j.jvoice.2010.10...
.
Coping strategies are the result of cognitive and behavioral efforts used to manage internal and external demands under stressing circumstances, and the emotions caused by them2828. Folkaman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985;48(1):150-70. https://doi.org/10.1037/0022-3514.48.1.150
https://doi.org/10.1037/0022-3514.48.1.1...
. In other words, they are used by an individual to deal with a problem that causes stress, trying to overcome it somehow1717. Oliveira G, Hirani SP, Epstein R, Yazigi L, Behlau M. Coping strategies in voice disorders of a Brazilian population. J Voice. 2012;26(2):205-13. https://doi.org/10.1016/j.jvoice.2010.10.023
https://doi.org/10.1016/j.jvoice.2010.10...
,1919. Chaves EC, Cade NV, Montovani MF, Leite RCBO, Spire WC. Coping: significados, interferência no processo saúde-doença e relevância para a enfermagem. Rev Esc Enferm USP. 2000;34(4):370-5. https://doi.org/10.1590/S0080-62342000000400008
https://doi.org/10.1590/S0080-6234200000...
,2929. Antoniazzi AS, Dell’Aglio DD, Bandeira DR. O conceito de coping: uma revisão teórica. Estud Psicol. 1998;3(2):273-94. https://doi.org/10.1590/S1413-294X1998000200006
https://doi.org/10.1590/S1413-294X199800...
.
Coping strategies vary according to personal experiences and may be emotion-focused or problem-focused. In the first case, there is a search to decrease the internal emotional discomfort sensation, and is used predominantly when there is a permanent impairment. In the second case, there is a search for direct changes in the environment that generated the stress and it is more used in situation that are possible to be changed. Both strategies occur when there is an increase in stress and mutually influence one another2828. Folkaman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985;48(1):150-70. https://doi.org/10.1037/0022-3514.48.1.150
https://doi.org/10.1037/0022-3514.48.1.1...
,3030. Ravagnani LMB, Domingos NAM, Miyazaki MCOS. Qualidade de vida e estratégias de enfrentamento em pacientes submetidos a transplante renal. Estud Psicol. 2007;12(2):177-84..
In the present study, both groups used more emotion-focused strategies and there were no statistical differences between the average scores. Essentially, one can say that subjects from both groups used the double of emotion-focused strategies (average for SCPL 42,73 and for TL 42,2) when compared to problem-focused strategies. Literature pointed out that problem-focused strategies are, usually, used by people who go through a “temporary” problem. Considering the emotion-focused strategies, the reverse occurs2929. Antoniazzi AS, Dell’Aglio DD, Bandeira DR. O conceito de coping: uma revisão teórica. Estud Psicol. 1998;3(2):273-94. https://doi.org/10.1590/S1413-294X1998000200006
https://doi.org/10.1590/S1413-294X199800...
, which may have happened in the present study since, most likely, either the total or the partial larynx removal implicates in permanent loss of the organism’s structure and function.
Concerning certain questions of the problem-focused domain, some differences were observed between the groups regarding the search for knowledge about the disease. The SCPL group differed from the TL group in the following questions: “I try to find all available information about my vocal disorder”; “I find it is easier to cope with my vocal disorder trying to understand it better”; “I find it is easier to cope with my vocal disorder when I ask questions to the doctor”. Therefore, one may suppose a certain tendency of the SCPL group to search for strategies focused on efforts to manage or alter the problem1919. Chaves EC, Cade NV, Montovani MF, Leite RCBO, Spire WC. Coping: significados, interferência no processo saúde-doença e relevância para a enfermagem. Rev Esc Enferm USP. 2000;34(4):370-5. https://doi.org/10.1590/S0080-62342000000400008
https://doi.org/10.1590/S0080-6234200000...
.
Literature acknowledged that subjects use more problem-focused strategies in the presence of a “changeable” situation2828. Folkaman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985;48(1):150-70. https://doi.org/10.1037/0022-3514.48.1.150
https://doi.org/10.1037/0022-3514.48.1.1...
,3030. Ravagnani LMB, Domingos NAM, Miyazaki MCOS. Qualidade de vida e estratégias de enfrentamento em pacientes submetidos a transplante renal. Estud Psicol. 2007;12(2):177-84.. Although it was a punctual tendency, the propensity for using certain problem-focused strategies more expressively by the SCPL group than by the TL group may be justified by considering that SCPL subjects had more vocal adaptive possibilities than TL subjects, since the total larynx removal, the tracheostomy and the loss of vocal source are permanent.
Concerning questions related to emotion-focused coping strategies, the item “I find it easier to cope with my voice problem by joking about it” presented difference between the groups, being more used by the TL group. Many interpretations can be given to this fact. One may think that the unchangeable feature due to the total larynx removal, or even the communication ways (esophageal speech, electronic larynx or tracheoesophageal prosthesis), which are very different than the usual communication mode, make these individuals a constant target of social curiosity, leading them to develop this type of strategy.
According to literature, SCPL seems to be ideally suited to treat T1, T2 and T3 tumors and some selected T4 cases, when compared to TL. Its results have been satisfactory either for the preservation of the organ as for the functional benefits11. Gallo A, Manciocco V, Tropiano ML, Simonelli M, Marvaso V, D’Arcangelo E et al. Prognostic value of resection margins in supracricoid laryngectomy. Laryngoscope. 2004;114(4):616-21. https://doi.org/10.1097/00005537-200404000-00005.
https://doi.org/10.1097/00005537-2004040...
,22. Laudadio P, Presutti L, Dall’Olio D, Cunsolo E, Consalici R, Amorosa L et al. Supracricoid laryngectomies: long-term oncological and functional results. Acta Otolaryngol. 2006;126(6):640-9. https://doi.org/10.1080/00016480500469024
https://doi.org/10.1080/0001648050046902...
,33. Nakayama M, Okamoto M, Miyamoto S, Takeda M, Yokobori S, Masaki T et al. Supracricoid laryngectomy with cricohyoidoepiglotto-pexy or cricohyoido-pexy: experience on 32 patients. AurisNasus Larynx. 2008;35(1):77-82. https://doi.org/10.1016/j.anl.2007.04.018
https://doi.org/10.1016/j.anl.2007.04.01...
,44. Alicandri-Ciufelli M, Piccinini A, Bergamini G, Ruberto M, Ghidini A, Marchioni D et al. Atypical neoglottis after supracricoid laryngectomy: a morphological and functional analysis. Eur Arch Otorhinolaryngol. 2011;268(7):1029-34. https://doi.org/10.1007/s00405-011-1556-4
https://doi.org/10.1007/s00405-011-1556-...
,55. Szyfter W, Leszczynska M, Wierzbicka M. Outcome after supracricoid laryngectomies in the material of ENT Department, Poznan University of Medical Sciences. Eur Arch Otorhinolaryngol. 2011;268(6):879-83. https://doi.org/10.1007/s00405-011-1513-2
https://doi.org/10.1007/s00405-011-1513-...
,66. Castro A, Sanchez-Cuadrado I, Bernaldez R, Del Palacio A, Gavilan J. Laryngeal function preservation following supracricoid partial laryngectomy. Head Neck. 2012;34(2):162-7. https://doi.org/10.1002/hed.21703
https://doi.org/10.1002/hed.21703...
,77. Vincentiis M, De Virgilio A, Bussu F, Gallus R, Gallo A, Bastanza G et al. Oncologic results of the surgical salvage of recurrent laryngeal squamous cell carcinoma in a multicentric retrospective series: emerging role of supracricoid partial laryngectomy. Head Neck. 2015;37(1):84-91. https://doi.org/10.1002/hed.23563
https://doi.org/10.1002/hed.23563...
. However, despite such reports, the subjects’ vocal self-assessment and the analysis related to the vocal handicap did not reveal differences between both groups. The same happened regarding the vocal problem coping strategies.
CONCLUSION
The comparison of two groups of subjects submitted to supracricoid partial laryngectomy and total laryngectomy did not evidence difference regarding vocal self-assessment and vocal handicap aspects. Both groups used more than the double of vocal problem coping strategies when compared to the population without vocal complaint, with predominance of emotion-focused strategies. It is suggested that further studies should be developed to verify the impacts of both surgical resources.
REFERÊNCIAS
-
1Gallo A, Manciocco V, Tropiano ML, Simonelli M, Marvaso V, D’Arcangelo E et al. Prognostic value of resection margins in supracricoid laryngectomy. Laryngoscope. 2004;114(4):616-21. https://doi.org/10.1097/00005537-200404000-00005
» https://doi.org/10.1097/00005537-200404000-00005 -
2Laudadio P, Presutti L, Dall’Olio D, Cunsolo E, Consalici R, Amorosa L et al. Supracricoid laryngectomies: long-term oncological and functional results. Acta Otolaryngol. 2006;126(6):640-9. https://doi.org/10.1080/00016480500469024
» https://doi.org/10.1080/00016480500469024 -
3Nakayama M, Okamoto M, Miyamoto S, Takeda M, Yokobori S, Masaki T et al. Supracricoid laryngectomy with cricohyoidoepiglotto-pexy or cricohyoido-pexy: experience on 32 patients. AurisNasus Larynx. 2008;35(1):77-82. https://doi.org/10.1016/j.anl.2007.04.018
» https://doi.org/10.1016/j.anl.2007.04.018 -
4Alicandri-Ciufelli M, Piccinini A, Bergamini G, Ruberto M, Ghidini A, Marchioni D et al. Atypical neoglottis after supracricoid laryngectomy: a morphological and functional analysis. Eur Arch Otorhinolaryngol. 2011;268(7):1029-34. https://doi.org/10.1007/s00405-011-1556-4
» https://doi.org/10.1007/s00405-011-1556-4 -
5Szyfter W, Leszczynska M, Wierzbicka M. Outcome after supracricoid laryngectomies in the material of ENT Department, Poznan University of Medical Sciences. Eur Arch Otorhinolaryngol. 2011;268(6):879-83. https://doi.org/10.1007/s00405-011-1513-2
» https://doi.org/10.1007/s00405-011-1513-2 -
6Castro A, Sanchez-Cuadrado I, Bernaldez R, Del Palacio A, Gavilan J. Laryngeal function preservation following supracricoid partial laryngectomy. Head Neck. 2012;34(2):162-7. https://doi.org/10.1002/hed.21703
» https://doi.org/10.1002/hed.21703 -
7Vincentiis M, De Virgilio A, Bussu F, Gallus R, Gallo A, Bastanza G et al. Oncologic results of the surgical salvage of recurrent laryngeal squamous cell carcinoma in a multicentric retrospective series: emerging role of supracricoid partial laryngectomy. Head Neck. 2015;37(1):84-91. https://doi.org/10.1002/hed.23563
» https://doi.org/10.1002/hed.23563 -
8Moyano JAM, Gutiérrez RS, Nogueras JR, Aumente PO, Villarejo PL. Calidad de vida em pacientes tratados mediante laringectomía parcial supracricoidea com cricohioidoepiglotopexia (CHEP). Acta Otorrinolaringol Esp. 2004;55(9):409-14. https://doi.org/10.1016/S0001-6519(04)78545-3
» https://doi.org/10.1016/S0001-6519(04)78545-3 -
9Decotte A, Woisard V, Percodani J, Pessey JJ, Serrano E, Vergez S. Respiratory complications after supracricoid partial laryngectomy. Eur Arch Otorhinolaryngol. 2010;267(9):1415-21. https://doi.org/10.1007/s00405-010-1238-7
» https://doi.org/10.1007/s00405-010-1238-7 -
10Kucuk H, Kurnaz SC, Kutlar G. Treatment expectations and quality of life outcomes of patients with laryngeal cancer based on different treatment methods. Eur Arch Otorhinolaryngol. 2015;272(5):1245-50. https://doi.org/10.1007/s00405-014-3066-7
» https://doi.org/10.1007/s00405-014-3066-7 -
11Eadie TL, Bowker BC. Coping and quality of life after total laryngectomy. Otolaryngol Head Neck Surg. 2012;146(6):959-65. https://doi.org/10.1177/0194599812437315
» https://doi.org/10.1177/0194599812437315 -
12Vakharia KT, Ali MJ, Wang SJ. Quality-of-life impact of participation in a head and neck cancer support group. Otolaryngol Head Neck Surg. 2007;136(3): 405-10. https://doi.org/10.1016/j.otohns.2006.10.018
» https://doi.org/10.1016/j.otohns.2006.10.018 -
13Moore KA, Ford PJ, Farah CS. ‘’I have quality of life…but…’’: exploring support need important to quality of life in head and neck cancer. Eur J OncolNurs. 2014;18(2):192-200. https://doi.org/10.1016/j.ejon.2013.10.010
» https://doi.org/10.1016/j.ejon.2013.10.010 -
14Campos RJDS, Leite ICG. Qualidade de vida e voz pós-radioterapia: repercussões para a fonoaudiologia. Rev CEFAC. 2010;12(4):671-77. https://doi.org/10.1590/S1516-18462010005000038
» https://doi.org/10.1590/S1516-18462010005000038 -
15Rogers SN. Quality of life perspectives in patients with oral cancer. Oral Oncol. 2010;46(6):445-7. https://doi.org/10.1016/j.oraloncology.2010.02.021
» https://doi.org/10.1016/j.oraloncology.2010.02.021 -
16Melo Filho MR, Rocha BA, Pires MBO, Fonseca ES, Freitas EM, Martelli Jr H et al. Qualidade de vida de pacientes com carcinoma em cabeça e pescoço. Braz J Otorhinolaryngol. 2013;79(1):82-9. https://doi.org/10.5935/1808-8694.20130014
» https://doi.org/10.5935/1808-8694.20130014 -
17Oliveira G, Hirani SP, Epstein R, Yazigi L, Behlau M. Coping strategies in voice disorders of a Brazilian population. J Voice. 2012;26(2):205-13. https://doi.org/10.1016/j.jvoice.2010.10.023
» https://doi.org/10.1016/j.jvoice.2010.10.023 -
18Zambon F, Moreti F, Behlau M. Coping strategies in teachers with vocal complaint. J Voice. 2014;28(3):341-8. https://doi.org/10.1016/j.jvoice.2013.11.008
» https://doi.org/10.1016/j.jvoice.2013.11.008 -
19Chaves EC, Cade NV, Montovani MF, Leite RCBO, Spire WC. Coping: significados, interferência no processo saúde-doença e relevância para a enfermagem. Rev Esc Enferm USP. 2000;34(4):370-5. https://doi.org/10.1590/S0080-62342000000400008
» https://doi.org/10.1590/S0080-62342000000400008 -
20Costa T, Oliveira G, Behlau M. Validação do índice de Desvantagem Vocal: 10 (IDV-10) para o português brasileiro. CoDAS. 2013;25(5):482-5. https://doi.org/10.1590/S2317-17822013000500013
» https://doi.org/10.1590/S2317-17822013000500013 -
21Oliveira G, Hirani SP, Epstein R, Yazigi L, Behlau M. Validation of the Brazilian version of voice disability coping questionnaire. J Voice. 2016;30(2):247. https://doi.org/10.1016/j.jvoice.2015.01.004
» https://doi.org/10.1016/j.jvoice.2015.01.004 -
22Rosen CA, Lee AS, Osborne J, Zullo T, Murry T. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114(9):1549-56. https://doi.org/10.1097/00005537-200409000-00009
» https://doi.org/10.1097/00005537-200409000-00009 -
23Oliveira IB, Augusti ACV, Siqueira DM. Avaliação de voz e qualidade de vida após laringectomia supracricóide. Audiol Commun Res. 2013;18(4):353-60. https://doi.org/10.1590/S2317-64312013000400018
» https://doi.org/10.1590/S2317-64312013000400018 -
24Schindler A, Favero E, Nudo S, Albera R, Schindler O, Cavalot AL. Long-term voice and swallowing modificaitons after supracricoidlaryngectomy: objective, subjective, and self-assessment data. Am J Otolaryngol. 2006;27(6):378-83. https://doi.org/10.1016/j.amjoto.2006.01.010
» https://doi.org/10.1016/j.amjoto.2006.01.010 -
25Schindler A, Mozzanica F, Ginocchio D, Invernizzi A, Peri A, Ottaviani F. Voice-related quality of life in patients after total and partial laryngectomy. Auris Nasus Larynx. 2012;39(1):77-83. https://doi.org/10.1016/j.anl.2011.03.009
» https://doi.org/10.1016/j.anl.2011.03.009 -
26Saito K, Akari K, Ogawa K, Shiotani A. Laryngeal function after supracricoid laryngectomy. Otolaryngol Head Neck Surg. 2009;140(4):487-92. https://doi.org/10.1016/j.otohns.2008.12.036
» https://doi.org/10.1016/j.otohns.2008.12.036 -
27Anchette D, Menezes MB, Nakay MY, Prandini B, Kikuchi W, Gonçalves AJ. Avaliação da qualidade de vida dos pacientes com câncer de laringe no pós-operatório tardio. Soc Bras Psico Oncol. 2009;4(3):1-6.
-
28Folkaman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985;48(1):150-70. https://doi.org/10.1037/0022-3514.48.1.150
» https://doi.org/10.1037/0022-3514.48.1.150 -
29Antoniazzi AS, Dell’Aglio DD, Bandeira DR. O conceito de coping: uma revisão teórica. Estud Psicol. 1998;3(2):273-94. https://doi.org/10.1590/S1413-294X1998000200006
» https://doi.org/10.1590/S1413-294X1998000200006 -
30Ravagnani LMB, Domingos NAM, Miyazaki MCOS. Qualidade de vida e estratégias de enfrentamento em pacientes submetidos a transplante renal. Estud Psicol. 2007;12(2):177-84.
Publication Dates
-
Publication in this collection
2017
History
-
Received
25 July 2016 -
Accepted
8 May 2017


 Subtitle: SCPL = Group of subjects submitted to supracricoid partial laryngectomy; TL = Group of subjects submitted to total laryngectomy
Subtitle: SCPL = Group of subjects submitted to supracricoid partial laryngectomy; TL = Group of subjects submitted to total laryngectomy
 Subtitle: SCPL = Group of subjects submitted to supracricoid partial laryngectomy; TL = Group of subjects submitted to total laryngectomy
Subtitle: SCPL = Group of subjects submitted to supracricoid partial laryngectomy; TL = Group of subjects submitted to total laryngectomy
 Subtitle: SCPL = Group of subjects submitted to supracricoid partial laryngectomy; TL = Group of subjects submitted to total laryngectomy
Subtitle: SCPL = Group of subjects submitted to supracricoid partial laryngectomy; TL = Group of subjects submitted to total laryngectomy