ABSTRACT
Research on the genetics, epidemiology, and clinical manifestations of Fabry disease (FD) has increased significantly in recent years. However, some relevant clinical questions still need to be answered to develop better approaches to patient management. This review focuses on answering specific questions raised by Brazilian experts based on their experience in diagnosing and managing patients with FD. The questions are as follows: What is the role of globotriaosylsphingosine in diagnosis? How does one proceed with the diagnosis if there is a variant of unknown significance? What are the earliest and most reliable markers of renal, cardiac, and neurological impairment? What is the prevalence of FD in patients with cryptogenic stroke? What is the average delay in diagnosis in patients with FD? Based on these questions, our objective was to highlight epidemiological, diagnostic, and clinical aspects relating to the literature in the FD field.
Keywords:
Fabry disease; rare disease; diagnostic.
Introduction
Fabry disease (FD) is a rare X-linked inherited disorder of glycosphingolipid metabolism caused by absent or deficient lysosomal alpha-galactosidase A (α-Gal A)11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19.,22. Arends M, Wanner C, Hughes D, et al. Characterization of classical and nonclassical fabry disease: a multicenter study. J Am Soc Nephrol. 2017;28(5):1631-1641.. FD is characterized by the partial or complete inability of α-Gal A to catabolize lipids, mainly globotriaosylceramide (Gb3), also known as ceramide trihexoside, due to mutations in theGLAgene located on the X chromosome (Xq22.1)33. Bernardes TP, Foresto RD, Kirsztajn GM. Fabry disease: genetics, pathology, and treatment. Rev Assoc Med Bras. 2020;66(Suppl 1):10-16.. Morbidity and mortality are usually related to heart, kidney, and central nervous system (CNS)44. Germain DP, Fouilhoux A, Decramer S, et al. Consensus recommendations for diagnosis, management and treatment of Fabry disease in paediatric patients. Clin Genet. 2019;96(2):107-117. involvement that ensues for several years or decades11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19.. The deposition of Gb3 found in endothelial, renal, cardiac, and dorsal root ganglion neuronal cells promotes disturbances that can lead to sensitivity changes. Early clinical manifestations include neuropathic pain, anhidrosis, angiokeratoma, cornea verticillata, gastrointestinal symptoms, and albuminuria11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19.,55. Ries M, Mengel E, Kutschke G, et al. Use of gabapentin to reduce chronic neuropathic pain in Fabry disease. J Inherit Metab Dis. 2003;26(4):413-414..
The incidence of FD ranges from 1 in 476,000 to 1 in 117,000 live births66. Meikle PJ, Hopwood JJ, Clague AE, Carey WF. Prevalence of lysosomal storage disorders. JAMA. 1999;281(3):249-254.-99. Germain DP. Fabry disease. Orphanet J Rare Dis. 2010;5(1):30.. A study conducted in newborns in Italy reported an incidence of 1 in 3,100 for late-onset disease and 1 in 37,000 for the classical phenotype1010. Spada M, Pagliardini S, Yasuda M, et al. High incidence of later-onset Fabry disease revealed by newborn screening. Am J Hum Genet. 2006;79(1):31-40.. Among the Austrian population, the combined incidence was 1 in 2,315 births, with a mutation spectrum suggesting a high number of late-onset diseases1111. Mechtler TP, Stary S, Metz TF, et al. Neonatal screening for lysosomal storage disorders: feasibility and incidence from a nationwide study in Austria. Lancet. 2012;379(9813):335-341. Epidemiological data from newborn screening programs found a neonatal prevalence of up to 1 in 1,250 newborns, with a higher prevalence in males (ranging from 1 in 1,500 to 1 in 3,100)1010. Spada M, Pagliardini S, Yasuda M, et al. High incidence of later-onset Fabry disease revealed by newborn screening. Am J Hum Genet. 2006;79(1):31-40.,1212. Hwu W, Chien Y, Lee N, et al. Newborn screening for Fabry disease in Taiwan reveals a high incidence of the later‐onset GLA mutation c. 936+ 919G>A (IVS4+919G>A). Hum Mutat. 2009;30(10):1397-1405.. FD is classified into classical and nonclassical (late-onset) phenotypes. The prevalence of late-onset FD is markedly higher than that of classical FD1010. Spada M, Pagliardini S, Yasuda M, et al. High incidence of later-onset Fabry disease revealed by newborn screening. Am J Hum Genet. 2006;79(1):31-40.,1111. Mechtler TP, Stary S, Metz TF, et al. Neonatal screening for lysosomal storage disorders: feasibility and incidence from a nationwide study in Austria. Lancet. 2012;379(9813):335-341..
The natural course of the disease differs in men and women with classical or nonclassical phenotypes22. Arends M, Wanner C, Hughes D, et al. Characterization of classical and nonclassical fabry disease: a multicenter study. J Am Soc Nephrol. 2017;28(5):1631-1641.. Patients with the nonclassical phenotype have 2%-20% of normal residual α-Gal A activity, and compared with patients with the classical phenotype, those with the nonclassical phenotype have nearly 30-fold lower levels of globotriaosylsphingosine (lyso-Gb3), the deacetylated form of Gb322. Arends M, Wanner C, Hughes D, et al. Characterization of classical and nonclassical fabry disease: a multicenter study. J Am Soc Nephrol. 2017;28(5):1631-1641.,1010. Spada M, Pagliardini S, Yasuda M, et al. High incidence of later-onset Fabry disease revealed by newborn screening. Am J Hum Genet. 2006;79(1):31-40.,1313. Smid BE, van der Tol L, Biegstraaten M, Linthorst GE, Hollak CEM, Poorthuis BJHM. Plasma globotriaosylsphingosine in relation to phenotypes of fabry disease. J Med Genet. 2015;52(4):262-268.. Patients with the classical phenotype present with signs and symptoms in the fourth to sixth decades of life, with clinical manifestations usually confined to one organ system1414. Nakao S, Takenaka T, Maeda M, et al. An atypical variant of Fabry’s disease in men with left ventricular hypertrophy. N Engl J Med. 1995;333(5):288-293..
Men with classical FD show reduced or absent α-Gal A enzyme activity, have an increased risk of developing complications in several organs (ie, Fabry neuropathic pain, angiokeratoma, or cornea verticillata and severe cardiac and renal disease), and often present with symptoms in the first decade of life or late adolescence22. Arends M, Wanner C, Hughes D, et al. Characterization of classical and nonclassical fabry disease: a multicenter study. J Am Soc Nephrol. 2017;28(5):1631-1641.,1515. Oliveira JP, Ferreira S. Multiple phenotypic domains of Fabry disease and their relevance for establishing genotype - phenotype correlations. Appl Clin Genet. 2019;12:35-50.,1616. El Sayed M, Hirsch A, Boekholdt M, et al. Influence of sex and phenotype on cardiac outcomes in patients with Fabry disease. Heart. 2021;107(23):1889-1897. . In women with classical FD, the phenotype and the natural course of the disease are determined by the pattern of X-chromosome inactivation (XCI), in which the mutant GLA allele occurs at a ratio of 80:20 or higher among tissues1717. Echevarria L, Benistan K, Toussaint A, et al. X‐chromosome inactivation in female patients with Fabry disease. Clin Genet. 2016;89(1):44-54.. Women have a variable disease course ranging from asymptomatic to severely affected, similar to that in hemizygous men11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19..
In children with classical FD, pain is the most striking symptom, affecting 60%-80%99. Germain DP. Fabry disease. Orphanet J Rare Dis. 2010;5(1):30.,1818. Thomas AS, Mehta AB. Difficulties and barriers in diagnosing Fabry disease: what can be learnt from the literature? Expert Opin Med Diagn. 2013;7(6):589-599.,1919. Bugescu N, Naylor PE, Hudson K, Aoki CD, Cordova MJ, Packman W. The psychosocial impact of Fabry disease on pediatric patients. J Pediatr Genet. 2016;5(3):141-149.. Their overall quality of life (QoL) is often impacted by fatigue, anxiety, depression, and school absenteeism44. Germain DP, Fouilhoux A, Decramer S, et al. Consensus recommendations for diagnosis, management and treatment of Fabry disease in paediatric patients. Clin Genet. 2019;96(2):107-117.,1919. Bugescu N, Naylor PE, Hudson K, Aoki CD, Cordova MJ, Packman W. The psychosocial impact of Fabry disease on pediatric patients. J Pediatr Genet. 2016;5(3):141-149.. Symptoms can begin in infancy or early childhood44. Germain DP, Fouilhoux A, Decramer S, et al. Consensus recommendations for diagnosis, management and treatment of Fabry disease in paediatric patients. Clin Genet. 2019;96(2):107-117., with an average age at presentation of 6 years in boys and 7-8 years in girls2020. Ramaswami U, Najafian B, Schieppati A, Mauer M, Bichet DG. Assessment of renal pathology and dysfunction in children with Fabry disease. Clin J Am Soc Nephrol. 2010;5(2):365-370.. However, the primary features of the disease process are observed as early as the fetal stage of development2121. Popli S, Leehey DJ, Molnar Z, Nawab ZM, Ing TS. Demonstration of Fabry’s disease deposits in placenta. Am J Obstet Gynecol. 1990;162(2):464-465.,2222. Vedder AC, Strijland A, M A vd BW, Florquin S, Aerts J, Hollak CEM. Manifestations of Fabry disease in placental tissue. J Inherit Metab Dis. 2006;29(1):106-111.. Renal involvement is a core feature in FD and begins early in life, with possible detection of glycolipid deposits in kidney biopsies before the onset of albuminuria. Therefore, evaluation of renal function and monitoring for signs of podocyte loss in renal biopsy and podocyturia should be performed during the first years of life2323. Torra R. Renal manifestations in Fabry disease and therapeutic options. Kidney Int Suppl. 2008;74(111):S29-S32..
Adults may experience progressive renal failure, hypertrophic cardiomyopathy, and cerebrovascular disease, which contribute to morbidity and early mortality11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19.,44. Germain DP, Fouilhoux A, Decramer S, et al. Consensus recommendations for diagnosis, management and treatment of Fabry disease in paediatric patients. Clin Genet. 2019;96(2):107-117.,99. Germain DP. Fabry disease. Orphanet J Rare Dis. 2010;5(1):30.. Furthermore, if left untreated, FD could lead to a reduction in life expectancy of almost 20 years. The long delay between the onset of symptoms and diagnosis is a challenge, corroborating the idea that in several cases, FD remains undiagnosed and patients can also die of complications without the underlying cause being recognized1818. Thomas AS, Mehta AB. Difficulties and barriers in diagnosing Fabry disease: what can be learnt from the literature? Expert Opin Med Diagn. 2013;7(6):589-599..
Most cases of FD are hereditary; however, de novo disease-related variants have occasionally been reported33. Bernardes TP, Foresto RD, Kirsztajn GM. Fabry disease: genetics, pathology, and treatment. Rev Assoc Med Bras. 2020;66(Suppl 1):10-16.,99. Germain DP. Fabry disease. Orphanet J Rare Dis. 2010;5(1):30.. For example, in Japan, the frequency of de novo variants in FD was 6.8%, while in Spain, the frequency was 4.5%2424. Kobayashi M, Ohashi T, Iizuka S, et al. Frequency of de novo mutations in Japanese patients with Fabry disease. Mol Genet Metab Rep. 2014;1:283-287.,2525. Rodríguez-Marí A, Coll MJ, Chabás A. Molecular analysis in Fabry disease in Spain: fifteen novel GLA mutations and identification of a homozygous female. Hum Mutat. 2003;22(3):258.. In addition, the Human Gene Mutation Database has identified 1086 differentGLAvariants located on the Xq22 chromosome. However, only 843 of these variants cause FD2626. Germain DP, Oliveira JP, Bichet DG, et al. Use of a rare disease registry for establishing phenotypic classification of previously unassigned GLA variants: a consensus classification system by a multispecialty Fabry disease genotype-phenotype workgroup. J Med Genet. 2020;57(8):542-551.-2828. Human Gene Mutation Database. The Human Gene Mutation Database at the Institute of Medical Genetics in Cardiff. [Internet]. 2022 2021 July 15>. Available from: http://www.hgmd.cf.ac.uk/ac/index.php .
http://www.hgmd.cf.ac.uk/ac/index.php...
. Although FD is transmitted in an X-linked manner, it affects both men and women. However, a longer time for diagnosis in women arises in part from the broader heterogeneity of presentation44. Germain DP, Fouilhoux A, Decramer S, et al. Consensus recommendations for diagnosis, management and treatment of Fabry disease in paediatric patients. Clin Genet. 2019;96(2):107-117..
The diagnosis depends on the patient’s sex and age group. In general, diagnosis is based on the analysis of α-Gal A enzyme activity in dried blood spots (DBS) and plasma, leukocytes, or fibroblasts. Typical assays involve fluorometry and tandem mass spectrometry, with the latter being considered more precise11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19..
With regard to the specific characteristics of sex and age, the diagnosis in men is based on typical signs and symptoms, low levels of or absent α-Gal A activity, increased concentrations of Gb3 and lyso-Gb3 in plasma or urine, and molecular identification of disease-related variants11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19.. In women, enzyme activity depends on XCI and can vary from deficient to normal, as with Gb3 and lyso-Gb3 concentrations. Therefore, the diagnosis in women should be based on detecting a disease-related variant in the GLA gene by genetic testing11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19.. The diagnosis of FD in the prenatal period is feasible by determining α-Gal A activity in chorionic villus culture in the 10th week of pregnancy or amniotic cell culture in the 14th week of pregnancy11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19.,99. Germain DP. Fabry disease. Orphanet J Rare Dis. 2010;5(1):30..
Treatment for FD aims to minimize, control, and prevent symptoms and complications, halt disease progression, and provide better QoL11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19.. Currently approved therapies are based on enzyme replacement therapy (ERT) and the pharmacologic chaperone migalastat33. Bernardes TP, Foresto RD, Kirsztajn GM. Fabry disease: genetics, pathology, and treatment. Rev Assoc Med Bras. 2020;66(Suppl 1):10-16.,2929. Ishii S. Pharmacological chaperone therapy for Fabry disease. Proc Jpn Acad Ser B Phys Biol Sci. 2012;88(1):18-30.,3030. Germain DP, Hughes DA, Nicholls K, et al. Treatment of Fabry’s Disease with the Pharmacologic Chaperone Migalastat. N Engl J Med. 2016;375(6):545-555.. The objective is to avoid or remove deposits of Gb3 in plasma, urine, and tissues33. Bernardes TP, Foresto RD, Kirsztajn GM. Fabry disease: genetics, pathology, and treatment. Rev Assoc Med Bras. 2020;66(Suppl 1):10-16.,3131. Sartori DJ, Leivas PGC, de Souza MV, Krug BC, Balbinotto G, Schwartz IVD. Judicialização do acesso ao tratamento de doenças genéticas raras: A doença de Fabry no Rio Grande do Sul. Cienc Saude Colet. 2012;17(10):2717-2728.. Enzyme-enhancing therapy with pharmacological chaperones is also possible for selected patients who have amenable variants2929. Ishii S. Pharmacological chaperone therapy for Fabry disease. Proc Jpn Acad Ser B Phys Biol Sci. 2012;88(1):18-30.. Adjunctive treatment includes angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, antiplatelet drugs, and pain modulators22. Arends M, Wanner C, Hughes D, et al. Characterization of classical and nonclassical fabry disease: a multicenter study. J Am Soc Nephrol. 2017;28(5):1631-1641.,33. Bernardes TP, Foresto RD, Kirsztajn GM. Fabry disease: genetics, pathology, and treatment. Rev Assoc Med Bras. 2020;66(Suppl 1):10-16..
Although research on the genetics, epidemiology, and clinical manifestations of FD has significantly increased in recent years, there remain clinical aspects that should be more deeply investigated to develop better approaches to patient management. This narrative literature review focuses on answering specific questions raised by experts based on their experience in diagnosing and managing patients with FD. Based on these questions, our objective was to highlight epidemiological, diagnostic, and clinical aspects relating to the literature in the FD field.
Methods
As a starting point, Brazilian experts in the field of FD and other rare diseases identified the most important issues (based on their clinical practice) to be answered and collated in a single document to share with specialists in FD. In light of the objective and the known limitations of studies on rare diseases, the authors considered a narrative review to be the most appropriate methodology for the current analysis.
This narrative literature review addressed the primary question “What are the epidemiological, diagnostic, and clinical aspects of patients with FD?”. This approach aimed to summarize and collate the main findings of the specific literature on FD. To accomplish this, the following five guiding questions were formulated:
-
What is the role of lyso-Gb3 in diagnosis? Is there any specific biomarker?
-
How does one proceed with the diagnosis if there is a variant of unknown significance (VUS)?
-
What are the earliest and most reliable markers of renal, cardiac, and neurological impairment?
-
What is the prevalence of FD in patients with cryptogenic stroke?
-
What is the average delay in diagnosis in patients with FD?
To address these questions, the scientific literature was mapped using both electronic and manual tracking. We began by searching the reference lists of key studies11. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci. 2014;344(1-2):5-19.-33. Bernardes TP, Foresto RD, Kirsztajn GM. Fabry disease: genetics, pathology, and treatment. Rev Assoc Med Bras. 2020;66(Suppl 1):10-16. by putting their titles into Google Scholar. We identified the articles that had cited them subsequently and manually screened these titles for relevance. We chose the “ancestry and snowballing” or “citation tracking” methods because initial database searching proved neither sensitive nor specific3232. Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: Audit of primary sources. BMJ. 2005;331(7524):1064-1065..
Based on this approach, the subsequent searches were conducted in the following databases: Virtual Health Library (VHL), SciELO (Scientific Electronic Library Online), Latin American and Caribbean Literature in Health Sciences (LILACS), PubMed (National Library of Medicine), and a preprint database (medRxiv). Additionally, essential data from official Brazilian websites (datasus.gov.br and conitec.gov.br) were searched.
The search strategy was guided by the five questions and included the following terms: "Fabry disease," "diagnostic," "biomarkers," "variant of unknown significance," "early signs," "prevalence," "cryptogenic stroke," "delay," “renal,” “cardiac,” and “neurologic,” combined with the AND, OR, and NOT Boolean operators. We searched for articles indexed from the first publication until January 31, 2021. The literature search was not limited to a specific study design, population age, or country. This is an essential method for literature searches involving rare diseases. However, we only included English, Spanish, and Portuguese studies and those conducted in humans. Articles that did not address data related to the guiding questions were excluded. The selection of the studies was performed independently by the authors (all authors performed the selection) according to the following processes: (1) identification of the research question, (2) literature search, (3) selection of the studies, (4) data evaluation, (5) synthesis of the data, and (6) presentation of the findings in this final narrative review.
Using these methods and terms, we identified 1595 studies. To answer the questions, we selected 52 studies, of which two were from Brazil3333. Rosa Neto NS, Bento JCDB, Pereira RMR. Higher rate of rheumatic manifestations and delay in diagnosis in Brazilian Fabry disease patients. Adv Rheumatol. 2020;60(1):1-8.,3434. Martins AM, Kyosen SO, Garrote J, et al. Demographic characterization of Brazilian patients enrolled in the Fabry Registry. Genet Mol Res. 2013;12(1):136-142..
Results
What is the role of lyso-Gb3 in diagnosis? Is there any specific biomarker?
Plasma lyso-Gb3 has gained importance as a screening and diagnostic biomarker for FD, enabling better distinction between patients with classical and nonclassical phenotypes and healthy subjects3535. Levstek T, Vujkovac B, Podkrajsek KT. Biomarkers of fabry nephropathy: Review and future perspective. Genes (Basel). 2020;11(9):1091.,3636. Togawa T, Kodama T, Suzuki T, et al. Plasma globotriaosylsphingosine as a biomarker of Fabry disease. Mol Genet Metab. 2010;100(3):257-261.. Lyso-Gb3 levels may correlate with the severity of clinical manifestations of FD in patients carrying different GLA disease-related variants3737. Auray-Blais C, Ntwari A, Clarke JTR, et al. How well does urinary lyso-Gb3 function as a biomarker in Fabry disease? Clin Chim Acta. 2010;411(23-24):1906-1914..
The first investigation to examine the role of lyso-Gb3 in diagnosis was conducted by Maruyama et al. (2013). They screened male patients with FD on dialysis using α-Gal A plasma activity as the primary biomarker and demonstrated that plasma lyso-Gb3 screening was effective for selecting candidates for genetic testing, revealing unrecognized cases, and reducing the number of unnecessary genetic analyses3838. Maruyama H, Takata T, Tsubata Y, et al. Screening of male dialysis patients for Fabry disease by plasma globotriaosylsphingosine. Clin J Am Soc Nephrol. 2013;8(4):629-636.. Nowak et al. (2017) demonstrated that the results of the lyso-Gb3 assay in DBS correlated well with tests performed in sera3939. Nowak A, Mechtler T, Kasper DC, Desnick RJ. Correlation of Lyso-Gb3 levels in dried blood spots and sera from patients with classic and Later-Onset Fabry disease. Mol Genet Metab. 2017;121(4):320-324.. Maruyama et al. (2019) found that lyso-Gb3 was effective as a primary screening biomarker for classical and late-onset FD male and female probands. Males with classical FD exhibited higher levels of lyso-Gb3 than those with late-onset FD. To classify naїve hemizygous patients with FD, a lyso-Gb3 value above 45 nmol/L predicts a diagnosis of classical FD in men. This method might exclude males with the p.E66Q variant.
In FD female probands, pedigree analyses showed that levels of lyso-Gb3 in asymptomatic women from families with class 1 disease-related variants did not exceed 2.0 ng/mL, making it challenging to define a lower limit for women (below 2 ng/mL). Lyso-Gb3 values in hemizygous relatives may help with the classification of female probands. The study also found 0.6% of men and 1.4% of women with positive screens for lyso-Gb3. Those with positive screens were subjected to GLA analysis. Thus, the analysis of plasma lyso-Gb3 may reveal patients at high risk for FD4040. Maruyama H, Miyata K, Mikame M, et al. Effectiveness of plasma lyso-Gb3 as a biomarker for selecting high-risk patients with Fabry disease from multispecialty clinics for genetic analysis. Genet Med. 2019;21(1):44-52.. Poorthuis et al. (2008) and Auray-Blais et al. (2010) argued that screening for FD with the lyso-Gb3 test in plasma or urine provides higher diagnostic performance and the ability to discriminate between affected and unaffected patients as well as the classical and nonclassical phenotypes3737. Auray-Blais C, Ntwari A, Clarke JTR, et al. How well does urinary lyso-Gb3 function as a biomarker in Fabry disease? Clin Chim Acta. 2010;411(23-24):1906-1914.,4141. Rossi F, L’Imperio V, Marti HP, et al. Proteomics for the study of new biomarkers in Fabry disease: State of the art. Mol Genet Metab. 2021;132(2):86-93.,4242. Poorthuis BJ, Groener JE, Ottenhoff R, Wijburg FA, Hollak CE, Aerts JM. Elevated globotriaosylsphingosine as a hallmark of Fabry disease. Chem Phys Lipids. 2008;154:S19-S20..
Nevertheless, these biomarkers have some limitations, including undetectable results in plasma or urine for women with classical FD4343. Alharbi FJ, Baig S, Rambhatla SB, et al. The clinical utility of total concentration of urinary globotriaosylsphingosine plus its analogues in the diagnosis of Fabry disease. Clin Chim Acta. 2020;500:120-127.,4444. Svarstad E, Marti HP. The Changing Landscape of Fabry Disease. Clin J Am Soc Nephrol. 2020;15(4):569-576. and patients with nonclassical FD variants4545. Mitobe S, Togawa T, Tsukimura T, et al. Mutant α-galactosidase A with M296I does not cause elevation of the plasma globotriaosylsphingosine level. Mol Genet Metab. 2012;107(3):623-626., inability to predict kidney involvement3737. Auray-Blais C, Ntwari A, Clarke JTR, et al. How well does urinary lyso-Gb3 function as a biomarker in Fabry disease? Clin Chim Acta. 2010;411(23-24):1906-1914., lack of reliability as a biomarker of disease activity, and response to treatment in heterozygous women and renal allograft recipients4646. Whitfield PD, Calvin J, Hogg S, et al. Monitoring enzyme replacement therapy in Fabry disease - role of urine globotriaosylceramide. J Inherit Metab Dis. 2005;28(1):21-33.. The total concentration of lyso-Gb3 plus its analogs in urine is highly sensitive and specific to support FD diagnosis for both classical and nonclassical patients4343. Alharbi FJ, Baig S, Rambhatla SB, et al. The clinical utility of total concentration of urinary globotriaosylsphingosine plus its analogues in the diagnosis of Fabry disease. Clin Chim Acta. 2020;500:120-127.,4747. Sueoka H, Ichihara J, Tsukimura T, Togawa T, Sakuraba H. Nano-LC-MS/MS for quantification of lyso-Gb3 and its analogues reveals a useful biomarker for Fabry disease. PLoS One. 2015;10(5):e0127048.. Nevertheless, gender strongly influences the urinary concentration of lyso-Gb3 and its analogs in pediatric FD4343. Alharbi FJ, Baig S, Rambhatla SB, et al. The clinical utility of total concentration of urinary globotriaosylsphingosine plus its analogues in the diagnosis of Fabry disease. Clin Chim Acta. 2020;500:120-127., with females having lower urinary levels of all biomarkers4343. Alharbi FJ, Baig S, Rambhatla SB, et al. The clinical utility of total concentration of urinary globotriaosylsphingosine plus its analogues in the diagnosis of Fabry disease. Clin Chim Acta. 2020;500:120-127.,4747. Sueoka H, Ichihara J, Tsukimura T, Togawa T, Sakuraba H. Nano-LC-MS/MS for quantification of lyso-Gb3 and its analogues reveals a useful biomarker for Fabry disease. PLoS One. 2015;10(5):e0127048.,4848. Auray-Blais C, Blais CM, Ramaswami U, et al. Urinary biomarker investigation in children with Fabry disease using tandem mass spectrometry. Clin Chim Acta. 2014;438:195-204.. Distinct lyso-Gb3 and related analogs (lyso-Gb3 [+16 Da], lyso-Gb3 [+34 Da], lyso-Gb3 [-2 Da], lyso-Gb3 [+14 Da], and lyso-Gb3 [+50 Da]) were detected in the urine of males and females with classical and nonclassical phenotypes4343. Alharbi FJ, Baig S, Rambhatla SB, et al. The clinical utility of total concentration of urinary globotriaosylsphingosine plus its analogues in the diagnosis of Fabry disease. Clin Chim Acta. 2020;500:120-127.. Urinary concentrations of lyso-Gb3 and its related analogs in treated males with FD were similar to those in untreated and treated females with FD. These characteristics were observed in children and adults4848. Auray-Blais C, Blais CM, Ramaswami U, et al. Urinary biomarker investigation in children with Fabry disease using tandem mass spectrometry. Clin Chim Acta. 2014;438:195-204..
Lyso-Gb3 analogs have been considered markers of some FD complications. Concerning the specific cardiac phenotype, increased levels of lyso-Gb3 analogs at m/z 836 were found only in patients manifesting severe heart disease, suggesting that it might be an earlier biomarker of progressive heart disease but nonspecific to FD cardiomyopathy4949. Ferreira S, Auray-Blais C, Boutin M, et al. Variations in the GLA gene correlate with globotriaosylceramide and globotriaosylsphingosine analog levels in urine and plasma. Clin Chim Acta. 2015;447:96-104.. Plasma lyso-Gb3 and urine lyso-Gb3 in m/z (+16), (+34), and (+50) were positively associated with left ventricular hypertrophy (LHV) and the Mainz Severity Score Index in adults and children5050. Yamashita S, Saotome M, Satoh H, et al. Plasma globotriaosylsphingosine level as a primary screening target for Fabry disease in patients with left ventricular hypertrophy. Circ J. 2019;83(9):1901-1907.,5151. Auray-Blais C, Lavoie P, Boutin M, et al. Biomarkers associated with clinical manifestations in Fabry disease patients with a late-onset cardiac variant mutation. Clin Chim Acta. 2017;466:185-193..
Auray-Blais et al. (2017) studied pediatric and adult patients carrying the late-onset cardiac FD phenotype variant IVS4 and found that patients may present different biomarkers levels as well as disease severity according to sex (concerning zygosity) and age to sex (concerning zygosity) and age5151. Auray-Blais C, Lavoie P, Boutin M, et al. Biomarkers associated with clinical manifestations in Fabry disease patients with a late-onset cardiac variant mutation. Clin Chim Acta. 2017;466:185-193.. In pediatric patients with this variant, biomarker levels did not reveal the severity of cardiomyocyte damage. The authors concluded that analysis of Gb3, lyso-Gb3, and related analogs would not be appropriate for neonatal screening5151. Auray-Blais C, Lavoie P, Boutin M, et al. Biomarkers associated with clinical manifestations in Fabry disease patients with a late-onset cardiac variant mutation. Clin Chim Acta. 2017;466:185-193.; however, these biomarkers can be helpful in monitoring. In addition, in patients with genetic VUS, elevated values of lyso-Gb3 in plasma may suggest FD but do not provide information about the phenotypic or biochemical characteristics of classical FD5252. Politei J, Alberton V, Amoreo O, et al. Clinical parameters, lysoGb3, podocyturia, and kidney biopsy in children with Fabry disease: is a correlation possible? Pediatr Nephrol. 2018;33(11):2095-2101..
Summary
Elevated concentrations of lyso-Gb3 in plasma, urine, or DBS with concomitant meticulous clinical and additional complementary exams (blood tests or imaging) might be useful to support the diagnosis of FD and for biochemical monitoring.
How does one proceed with the diagnosis if there is a VUS?
Patients with FD with novel variants require accurate evaluations to generate unbiased data regarding their consequences5353. Liao HC, Hsu TR, Young L, et al. Functional and biological studies of α-galactosidase A variants with uncertain significance from newborn screening in Taiwan. Mol Genet Metab. 2018;123(2):140-147.,5454. Filoni C, Caciotti A, Carraresi L, et al. Functional studies of new GLA gene mutations leading to conformational Fabry disease. Biochim Biophys Acta. 2010;1802(2):247-252.. Analysis of plasma lyso-Gb3 levels proved to have significant diagnostic sensitivity, especially in heterozygous women and patients with nonclassical FD; in addition, these levels correlate with the severity of clinical manifestations in patients with different GLA variants3737. Auray-Blais C, Ntwari A, Clarke JTR, et al. How well does urinary lyso-Gb3 function as a biomarker in Fabry disease? Clin Chim Acta. 2010;411(23-24):1906-1914.,5353. Liao HC, Hsu TR, Young L, et al. Functional and biological studies of α-galactosidase A variants with uncertain significance from newborn screening in Taiwan. Mol Genet Metab. 2018;123(2):140-147.. Neonatal screening of FD demonstrated a high prevalence of VUS. Individuals with VUS generally do not clinically express the disease and may present with nonclassical FD or no FD at all5555. van der Tol L, Smid BE, Poorthuis BJHM, et al. A systematic review on screening for fabry disease: prevalence of individuals with genetic variants of unknown significance. J Med Genet. 2014;51(1):1-9.. A systematic review showed that in some cases, it was necessary to conduct biochemical analyses and imaging of the affected organ. In cases of uncertainty, a biopsy of the affected organ is indicated to demonstrate the accumulation of Gb3 using electron microscopy (EM)5555. van der Tol L, Smid BE, Poorthuis BJHM, et al. A systematic review on screening for fabry disease: prevalence of individuals with genetic variants of unknown significance. J Med Genet. 2014;51(1):1-9..
To investigate the pathogenicity of a specific VUS, Liao et al. (2018) identified 13 missense VUS in 42 Taiwanese newborns (primarily male; p.N53D, p.P60S, p.G104V, p.A108T, p.P210S, p.I232T, p.M296L, p.S304T, p.D322H, p.R356Q, p.G360C, p.P362T, and p.K391T) using genetic analysis (site-specific mutagenesis of wild-type GLA cDNA)5353. Liao HC, Hsu TR, Young L, et al. Functional and biological studies of α-galactosidase A variants with uncertain significance from newborn screening in Taiwan. Mol Genet Metab. 2018;123(2):140-147.. Thereafter the prevalence of these VUS in the Taiwanese population was investigated and in silico prediction was performed (Polymorphism Phenotyping version 2 [PolyPhen-2], Mutation Tester, Proven, and Sorting Intolerant From Tolerant [SIFT] prediction). The p.P60S, p.G104V, p.I232T, p.D322H, p.G360C, and p.P362T were identified as the disease-causing variants, while p.P210S, p.S304T, p.R356Q, and p.K391T were considered benign or tolerable (according to at least two prediction tools)5353. Liao HC, Hsu TR, Young L, et al. Functional and biological studies of α-galactosidase A variants with uncertain significance from newborn screening in Taiwan. Mol Genet Metab. 2018;123(2):140-147.. It is important to note that approximately 80% of the patients carried the IVS4+919 G>A variant, and 5% carried classical or nonclassical variants in addition to the variants that were not previously reported or clarified. In addition to the VUS identified by Liao et al., Germain et al. (2020) recognized an additional VUS, namely, p.Ala143Thr, in the Fabry Registry2626. Germain DP, Oliveira JP, Bichet DG, et al. Use of a rare disease registry for establishing phenotypic classification of previously unassigned GLA variants: a consensus classification system by a multispecialty Fabry disease genotype-phenotype workgroup. J Med Genet. 2020;57(8):542-551.. It is worth mentioning that in silico prediction software introduces limitations such as contradictory results, unlike enzyme activity or plasma lyso-Gb3 data5353. Liao HC, Hsu TR, Young L, et al. Functional and biological studies of α-galactosidase A variants with uncertain significance from newborn screening in Taiwan. Mol Genet Metab. 2018;123(2):140-147.; the former has low diagnostic specificity and is restricted to predicting the pathogenic splice sites of missense variants2626. Germain DP, Oliveira JP, Bichet DG, et al. Use of a rare disease registry for establishing phenotypic classification of previously unassigned GLA variants: a consensus classification system by a multispecialty Fabry disease genotype-phenotype workgroup. J Med Genet. 2020;57(8):542-551..
The establishment of genotype-phenotype correlations in FD requires evidence of alteration in α-Gal A-dependent glycosphingolipid homeostasis, particularly in patients with nonclassical clinical phenotypes or patients with a VUS. Thus, complete phenotyping, whenever possible in hemizygous men, is the key to classifying the severity of GLA variants1515. Oliveira JP, Ferreira S. Multiple phenotypic domains of Fabry disease and their relevance for establishing genotype - phenotype correlations. Appl Clin Genet. 2019;12:35-50.. In patients without additional conclusive evidence of FD (ie, significantly reduced α-Gal A activity or histopathological evidence of Gb3 accumulation), a typical result of GLA genotyping at the gDNA level excludes the diagnosis. The same hypothesis can be applied to mRNA in men. In women, a typical result of genotyping at the mRNA level is a false negative due to XCI and the type of GLAvariant. In this case, the expression of the pathogenic variant of the GLA can be hidden, and caution must be taken when using these data to exclude the diagnosis of FD. Therefore, genotyping GLA at the gDNA level is recommended. VUS detection requires complete phenotyping to investigate pathogenicity and to support decision-making processes1515. Oliveira JP, Ferreira S. Multiple phenotypic domains of Fabry disease and their relevance for establishing genotype - phenotype correlations. Appl Clin Genet. 2019;12:35-50..
As previously demonstrated, the consensus was that in cases with an uncertain diagnosis of the nonclassical phenotype, enzymatic or genetic tests cannot always confirm an accurate diagnosis of FD. Regarding binomial LHV and VUS, histological analysis of cardiac muscle tissue should be considered the gold standard for diagnosis. In specific cases, such as in the absence of drugs known to induce a similar storage pattern, an endomyocardial biopsy exhibiting lamellar inclusion bodies characteristic of EM should be considered to support the diagnosis. It is important to note that similar deposits can be observed using medications such as amiodarone or chloroquine5656. Smid BE, van der Tol L, Cecchi F, et al. Uncertain diagnosis of Fabry disease : Consensus recommendation on diagnosis in adults with left ventricular hypertrophy and genetic variants of unknown significance. Int J Cardiol. 2014;177(2):400-408.. To detect characteristics of FD nephropathy, the Maltese cross sign and high urinary Gb3 have been described as “red flags” by Van der Tol et al. (2015)5757. van der Tol L, Svarstad E, Ortiz A, et al. Chronic kidney disease and an uncertain diagnosis of Fabry disease: approach to a correct diagnosis. Mol Genet Metab. 2015;114(2):242-247.. For patients with uncertain diagnoses, the absence of the classic pattern of disease manifestations, GLA (VUS), or chronic kidney disease (CKD), a renal biopsy with an EM assessment is strongly recommended to confirm or exclude the diagnosis of FD nephropathy5757. van der Tol L, Svarstad E, Ortiz A, et al. Chronic kidney disease and an uncertain diagnosis of Fabry disease: approach to a correct diagnosis. Mol Genet Metab. 2015;114(2):242-247.,5858. Curiati MA, Aranda CS, Kyosen SO, et al. The challenge of diagnosis and indication for treatment in fabry disease. J Inborn Errors Metab Screen. 2016;5:1-7..
Summary
Comprehensive multidomain phenotyping (ie, clinical, biochemical, and molecular genetic analyses) is necessary to investigate the severity of pathogenic GLA variants and to establish the pathogenicity of VUS to support decision-making processes in FD diagnosis. Histological analysis is still recommended in selected cases.
What are the earliest and most reliable markers of renal, cardiac, and neurological impairment?
Renal impairment
Nephropathy is a classic characteristic of FD. It is marked by disease progression with deposition of Gb3 in all types of cells, including podocytes and endothelial, mesangial, and tubular cells3535. Levstek T, Vujkovac B, Podkrajsek KT. Biomarkers of fabry nephropathy: Review and future perspective. Genes (Basel). 2020;11(9):1091.,5959. Abensur H, Reis MA Dos. Renal involvement in Fabry disease. J Bras Nefrol. 2016;38(2):245-254.,6060. Riccio E, Sabbatini M, Capuano I, Pisani A. Early biomarkers of fabry nephropathy: A review of the literature. Nephron. 2019;143(4):274-281.. Due to the absence of specific clinical markers, FD nephropathy may be associated with a delay in diagnosis of approximately 15 years, contributing to the overall burden of disease3535. Levstek T, Vujkovac B, Podkrajsek KT. Biomarkers of fabry nephropathy: Review and future perspective. Genes (Basel). 2020;11(9):1091.,6060. Riccio E, Sabbatini M, Capuano I, Pisani A. Early biomarkers of fabry nephropathy: A review of the literature. Nephron. 2019;143(4):274-281.. Currently, the approaches used in nephrology to diagnose patients with FD are kidney biopsy, high-risk population testing, and family screening3535. Levstek T, Vujkovac B, Podkrajsek KT. Biomarkers of fabry nephropathy: Review and future perspective. Genes (Basel). 2020;11(9):1091.. Albuminuria and reduced glomerular filtration rate are considered the gold-standard markers of renal dysfunction and significant predictors of kidney disease progression in patients with FD. However, renal impairment also occurs in a normoalbuminuric state (ie, in patients with podocyte injury)5959. Abensur H, Reis MA Dos. Renal involvement in Fabry disease. J Bras Nefrol. 2016;38(2):245-254., demonstrating a better correlation with estimated glomerular filtration rate (eGFR)3535. Levstek T, Vujkovac B, Podkrajsek KT. Biomarkers of fabry nephropathy: Review and future perspective. Genes (Basel). 2020;11(9):1091.,6060. Riccio E, Sabbatini M, Capuano I, Pisani A. Early biomarkers of fabry nephropathy: A review of the literature. Nephron. 2019;143(4):274-281.. Nevertheless, the main criteria for initiating ERT are renal biopsy findings in men, reduction in eGFR, or persistent proteinuria. Treatment is commonly delayed until proteinuria or evident organ involvement is detected, resulting in poor outcomes6060. Riccio E, Sabbatini M, Capuano I, Pisani A. Early biomarkers of fabry nephropathy: A review of the literature. Nephron. 2019;143(4):274-281..
To prevent poor outcomes, implementing strategies for earlier detection of FD nephropathy is paramount. For example, alternative biomarkers correlated to the earliest stages of kidney damage favored the diagnosis of preclinical renal involvement3535. Levstek T, Vujkovac B, Podkrajsek KT. Biomarkers of fabry nephropathy: Review and future perspective. Genes (Basel). 2020;11(9):1091.,6060. Riccio E, Sabbatini M, Capuano I, Pisani A. Early biomarkers of fabry nephropathy: A review of the literature. Nephron. 2019;143(4):274-281.. Some examples are podocyturia; glomerular hyperfiltration; cystatin C; urinary Gb3 and lyso-Gb3; glomerular (transferrin and type IV collagen) and tubular (α1-microglobulin, N-acetyl-β-glucosaminidase, and alanine aminopeptidase) dysfunction; bikunin (urinary trypsin inhibitor); parapelvic cysts; and approaches such as proteomics, genomics, transcriptomics, epigenomics, and metabolomics3535. Levstek T, Vujkovac B, Podkrajsek KT. Biomarkers of fabry nephropathy: Review and future perspective. Genes (Basel). 2020;11(9):1091.,6060. Riccio E, Sabbatini M, Capuano I, Pisani A. Early biomarkers of fabry nephropathy: A review of the literature. Nephron. 2019;143(4):274-281..
In children, proteinuria, microalbuminuria, increased serum creatinine, and reduced glomerular filtration rate showed low sensitivity for detecting early kidney damage, and abnormal results are often late signs of kidney disease. Renal biopsy studies in infants and children with the classical FD phenotype demonstrated that renal morphologic damage starts even before the detection of microalbuminuria/proteinuria or elevated serum creatinine6161. Najafian B, Mauer M, Hopkin RJ, Svarstad E. Renal complications of Fabry disease in children. Pediatr Nephrol. 2013;28(5):679-687. with segmental podocyte foot process effacement (evaluated through EM), a sign of podocyte injury in reaction to Gb3 deposits5252. Politei J, Alberton V, Amoreo O, et al. Clinical parameters, lysoGb3, podocyturia, and kidney biopsy in children with Fabry disease: is a correlation possible? Pediatr Nephrol. 2018;33(11):2095-2101.,6262. Tøndel C, Kanai T, Larsen KK, et al. Foot process effacement is an early marker of nephropathy in young classic fabry patients without albuminuria. Nephron. 2015;129(1):16-21.. In the pediatric population, few studies acknowledge that the prevention of or significant delay in the development of severe kidney disease in adulthood could be ensured by the initiation of ERT in childhood2020. Ramaswami U, Najafian B, Schieppati A, Mauer M, Bichet DG. Assessment of renal pathology and dysfunction in children with Fabry disease. Clin J Am Soc Nephrol. 2010;5(2):365-370..
Summary
Nephropathy begins early in childhood and, if not adequately treated, can progress to kidney failure in adolescence. Patient monitoring should be frequent, and renal biopsy should be performed if the patient presents increasing levels of lyso-Gb3 and a family history of FD nephropathy.
Cardiac impairment
Cardiac disease contributes to morbidity and mortality in patients with FD and can be the first manifestation in 10% of patients6363. Fernández A, Politei J. Cardiac manifestation of fabry disease: from hypertrophic cardiomyopathy to early diagnosis and treatment in patients without left ventricular hypertrophy. J Inborn Errors Metab Screen. 2016;4:1-9.. In the classical phenotype, patients usually show the first signs of cardiovascular impact between 30 and 40 years of age and then progress to heart failure with preserved ejection fraction6464. Yogasundaram H, Nikhanj A, Putko BN, et al. Elevated inflammatory plasma biomarkers in patients with fabry disease: a critical link to heart failure with preserved ejection fraction. J Am Heart Assoc. 2018;7(21):1-18.. Signs of cardiac involvement include LVH (concentric or asymmetrical), coronary disease, atrioventricular conduction disturbances, arrhythmia, valvular involvement, myocardial fibrosis, and functional impairment6363. Fernández A, Politei J. Cardiac manifestation of fabry disease: from hypertrophic cardiomyopathy to early diagnosis and treatment in patients without left ventricular hypertrophy. J Inborn Errors Metab Screen. 2016;4:1-9.,6565. Nordin S, Kozor R, Baig S, et al. Cardiac phenotype of prehypertrophic fabry disease. Circ Cardiovasc Imaging. 2018;11(6):e007168.. Although only 3% of the ventricular mass is due to Gb3 accumulation in FD cardiomyopathy, it activates oxidative stress and inflammatory pathways that lead to hypertrophy. Identification of lyso-Gb3 cell deposits contributed to the assessment of cardiac involvement6363. Fernández A, Politei J. Cardiac manifestation of fabry disease: from hypertrophic cardiomyopathy to early diagnosis and treatment in patients without left ventricular hypertrophy. J Inborn Errors Metab Screen. 2016;4:1-9..
Early signs of cardiac involvement can also be found before the appearance of myocardial hypertrophy. In this instance, it is advisable to conduct an electrocardiogram (ECG) to investigate ventricular repolarization disorders and conduction abnormalities demonstrated by the presence of a short PR interval and signs of left ventricular overload. Early signs of changes in myocardium velocities, microvascular dysfunction, and changes in diastolic function may also precede LVH6363. Fernández A, Politei J. Cardiac manifestation of fabry disease: from hypertrophic cardiomyopathy to early diagnosis and treatment in patients without left ventricular hypertrophy. J Inborn Errors Metab Screen. 2016;4:1-9.. These conditions can be assessed using echocardiography techniques, such as cardiac strain imaging with speckle-tracking echocardiography, that can identify signs preceding changes in ejection fraction6363. Fernández A, Politei J. Cardiac manifestation of fabry disease: from hypertrophic cardiomyopathy to early diagnosis and treatment in patients without left ventricular hypertrophy. J Inborn Errors Metab Screen. 2016;4:1-9.. Another sensitive and specific method for detecting early cardiac involvement in FD is magnetic resonance myocardial T1 mapping without contrast. This modality differentiates FD from other causes of LVH by reflecting glycosphingolipid deposits before the onset of LVH, identifying prehypertrophic cardiac involvement, and being associated with early diastolic and systolic dysfunction characteristics measured by echocardiography6363. Fernández A, Politei J. Cardiac manifestation of fabry disease: from hypertrophic cardiomyopathy to early diagnosis and treatment in patients without left ventricular hypertrophy. J Inborn Errors Metab Screen. 2016;4:1-9.,6666. Militaru S, Ginghin C, Popescu BA, Saftoiu A, Linhart A, Jurcut R. Multimodality imaging in Fabry cardiomyopathy: from early diagnosis to therapeutic targets. Eur Hear J Cardiovasc Imaging. 2018;19(12):1313-1322..
With regard to biomarkers, the N-terminal fragment of the pro-brain natriuretic peptide (NT-proBNP) is increased in patients with diastolic dysfunction in the absence of LVH and is related to the stage of cardiac involvement. However, these findings should be cautiously interpreted because elevated NT-proBNP can also be found in patients with FD with CKD6363. Fernández A, Politei J. Cardiac manifestation of fabry disease: from hypertrophic cardiomyopathy to early diagnosis and treatment in patients without left ventricular hypertrophy. J Inborn Errors Metab Screen. 2016;4:1-9..
Children with FD may manifest early cardiac involvement. Wilson et al. (2017) conducted a cohort study in 26 individuals aged below 18 years and found that sinus bradycardia was an early sign of cardiac involvement, followed by ectopic atrial rhythm and premature atrial contractions6767. Wilson HC, Hopkin RJ, Madueme PC, et al. Arrhythmia and clinical cardiac findings in children with Anderson-Fabry disease. Am J Cardiol. 2017;120(2):251-255.. During follow-up, the most prevalent complaint in this population was chest pain and palpitations (detected using Holter monitors and exercise stress tests). A few patients experienced aortic root dilation and concurrent aortic insufficiency6767. Wilson HC, Hopkin RJ, Madueme PC, et al. Arrhythmia and clinical cardiac findings in children with Anderson-Fabry disease. Am J Cardiol. 2017;120(2):251-255.. Kampmann et al. (2008) measured increased values of left ventricular mass (LVM) indexed to height (LVM/h2.7) in children and adolescents with FD in comparison with healthy subjects. Interestingly, after an average of 26 months of follow-up, the LVM/h2.7 increased in 85.7% of patients6868. Kampmann C, Wiethoff CM, Whybra C, Baehner FA, Mengel E, Beck M. Cardiac manifestations of Anderson-Fabry disease in children and adolescents. Acta Paediatr. 2008;97(4):463-469..
Summary
Ventricular repolarization disorders and conduction abnormalities demonstrated by a short PR interval, sinus bradycardia, and signs of left ventricular overload in the ECG may suggest early signs of cardiac involvement in FD. Cardiac strain imaging and noncontrast myocardial T1 mapping can also detect early changes in the myocardium, microvascular dysfunction, and systolic and diastolic function.
Neurological impairment
Neurological impairment in patients with FD is manifested as an accumulation of Gb3 in Schwann cells, dorsal root ganglia, and CNS neurons, with consequent cerebrovasculopathy, cochlear nerve dysfunction, psychiatric and cognitive symptoms, autonomic dysfunction, and peripheral neuropathy6969. Brooks JBB, Fragoso YD. Neurological manifestations in Fabry disease. Neuroimmunol Neuroinflammation. 2016;3(10):228.-7272. Schiffmann R, Moore DF. Neurological manifestations of Fabry disease. In: Mehta A, Beck M, Sunder-Plassmann G, eds. Fabry Disease: Perspectives from 5 Years of FOS. Oxford: Oxford PharmaGenesis; 2006.. Neurological deficits include mild cognitive abnormalities, hemiparesis, vertigo/dizziness, diplopia, dysarthria, nystagmus, nausea/vomiting, headaches, hemiataxia, dysmetria, cerebellar gait ataxia, and (very rarely) cerebral hemorrhage. Hypohidrosis, psychiatric conditions, dementia, and other abnormalities associated with nervous system dysfunction are common in patients with FD7272. Schiffmann R, Moore DF. Neurological manifestations of Fabry disease. In: Mehta A, Beck M, Sunder-Plassmann G, eds. Fabry Disease: Perspectives from 5 Years of FOS. Oxford: Oxford PharmaGenesis; 2006..
Cerebrovascular complications are a major cause of morbidity and early mortality in patients with FD6969. Brooks JBB, Fragoso YD. Neurological manifestations in Fabry disease. Neuroimmunol Neuroinflammation. 2016;3(10):228.,7070. Kolodny E, Fellgiebel A, Hilz MJ, et al. Cerebrovascular involvement in fabry disease: Current status of knowledge. Stroke. 2015;46(1):302-313.. The prevalence of strokes described by the Fabry Registry was 6.9%-11.1% in males and 4.3%-15.7% in females. These data demonstrated that 1%-2% of all strokes identified in the general population aged 18-55 years were caused by neurological impairment related to FD7373. Marchesoni C, Cisneros E, Pfister P, et al. Brain MRI findings in children and adolescents with Fabry disease. J Neurol Sci. 2018;395:131-134.. It is essential to note that chronic white matter hyperintensities revealed by magnetic resonance imaging (MRI) are rarely associated with any neurological abnormalities and should be distinguished from white matter strokes7070. Kolodny E, Fellgiebel A, Hilz MJ, et al. Cerebrovascular involvement in fabry disease: Current status of knowledge. Stroke. 2015;46(1):302-313..
The cerebrovasculopathy of patients with FD is characterized as a small-vessel disease due to symptomatic stroke or vascular brain lesions, which can be identified in neuroimaging exams. These vascular abnormalities can be accurately detected on gradient echo (GRE) T2-weighted images or fluid-attenuated inversion recovery (FLAIR) MRI, mainly in the posterior periventricular and centrum semiovale regions of the white matter7070. Kolodny E, Fellgiebel A, Hilz MJ, et al. Cerebrovascular involvement in fabry disease: Current status of knowledge. Stroke. 2015;46(1):302-313.,7272. Schiffmann R, Moore DF. Neurological manifestations of Fabry disease. In: Mehta A, Beck M, Sunder-Plassmann G, eds. Fabry Disease: Perspectives from 5 Years of FOS. Oxford: Oxford PharmaGenesis; 2006.,7373. Marchesoni C, Cisneros E, Pfister P, et al. Brain MRI findings in children and adolescents with Fabry disease. J Neurol Sci. 2018;395:131-134..
Even in the absence of neurological symptoms, patients with FD may have significant abnormalities in various measures of brain function and circulation (eg, in the basilar artery diameter and basilar dolichoectasia and hyperexcitability in the primary motor cortex). To detect early signs of neurological involvement, brain MRI and functional transcranial Doppler sonography provide a more reliable picture of the natural history of white matter lesions (WML), microhemorrhagic lesions, vascular dysfunction, and abnormalities in the posterior cortical circulation, even without a prior history of stroke7070. Kolodny E, Fellgiebel A, Hilz MJ, et al. Cerebrovascular involvement in fabry disease: Current status of knowledge. Stroke. 2015;46(1):302-313.,7373. Marchesoni C, Cisneros E, Pfister P, et al. Brain MRI findings in children and adolescents with Fabry disease. J Neurol Sci. 2018;395:131-134..
Children and adolescents with FD almost never demonstrate early signs of brain lesions. Marchesoni et al. (2018) found subclinical evidence of asymptomatic WML (70% of the lesions were in the anterior circulation) on MRI scans of 15.9% of young patients with FD without a history of cerebrovascular accident. This result was observed mainly in heterozygous women. As asymptomatic lesions in young patients with FD are rarely investigated, the authors suggested possible selection bias through the inclusion of most symptomatic children and adolescents for neurological assessment7373. Marchesoni C, Cisneros E, Pfister P, et al. Brain MRI findings in children and adolescents with Fabry disease. J Neurol Sci. 2018;395:131-134..
In addition to these prior neurological impairments, small sensory nerve fiber activity is also affected in patients with FD7171. Burlina A, Politei J. The central nervous system involvement in fabry disease: A review. J Inborn Errors Metab Screen. 2016;4:1-7.,7474. Politei JM, Durand C, Schenone AB. Small fiber neuropathy in fabry disease: A review of pathophysiology and treatment. J Inborn Errors Metab Screen. 2016;4:1-5.. Consequently, a decrease in autonomic function of Aδ fibers occurs, causing thermal sensation deficits mainly in the feet and gradually progressing to more proximal parts. In the early stages, thermal stimulus impairment compromises the perception of cold, suggesting that finely myelinated Aδ fibers are more vulnerable to damage caused by Gb3 accumulation7171. Burlina A, Politei J. The central nervous system involvement in fabry disease: A review. J Inborn Errors Metab Screen. 2016;4:1-7.,7474. Politei JM, Durand C, Schenone AB. Small fiber neuropathy in fabry disease: A review of pathophysiology and treatment. J Inborn Errors Metab Screen. 2016;4:1-5..
Potential biomarkers of cardiac and renal involvement have been described previously; however, few have demonstrated any correlation with cerebrovascular involvement, including the lysosome-associated protein (1 and 2) found in phagocytes. Proteomic analysis of the peripheral blood mononuclear cells demonstrated upregulation of γ-enolase and galectin-1, suggesting possible cerebrovascular accidents and brain trauma and inflammatory processes7070. Kolodny E, Fellgiebel A, Hilz MJ, et al. Cerebrovascular involvement in fabry disease: Current status of knowledge. Stroke. 2015;46(1):302-313.. High levels of lyso-Gb3 in plasma may correlate with the development of cerebrovascular WML. The exposure to lyso-Gb3 may favor the risk for stroke through the increased intima-media vessel wall thickness in patients with FD. Nevertheless, it is essential to observe the limitations of this biomarker, particularly in female patients. Nevertheless, it is essential to observe the limitations of this biomarker, especially in females, considering the reported variations in lyso-Gb3 plasma concentrations among female patients7070. Kolodny E, Fellgiebel A, Hilz MJ, et al. Cerebrovascular involvement in fabry disease: Current status of knowledge. Stroke. 2015;46(1):302-313..
It is hypothesized that due to an increased endothelial inflammatory profile observed in patients with FD, serum biomarkers may be a more reliable indicator of stroke risk when compared with brain hemodynamic parameters. Research on potential biomarkers of endothelial dysfunction has revealed promising candidates, such as 3-nitrotyrosine, soluble vascular cell adhesion molecule-1, high-sensitivity C-reactive protein, tumor necrosis factor-α, and P-selectin7070. Kolodny E, Fellgiebel A, Hilz MJ, et al. Cerebrovascular involvement in fabry disease: Current status of knowledge. Stroke. 2015;46(1):302-313..
Finally, presymptomatic screening for these subtle indicators of cerebrovascular dysfunction and injury and autonomic function may facilitate early identification of patients at risk for neurological impairment and support treatment decision-making7373. Marchesoni C, Cisneros E, Pfister P, et al. Brain MRI findings in children and adolescents with Fabry disease. J Neurol Sci. 2018;395:131-134..
Summary
Neurological impairment in FD is characterized by central, peripheral, and autonomic systems. In children, neuropathic pain and dysautonomia are the most prevalent conditions, whereas in adults, cerebrovasculopathy is more common.
What is the prevalence of FD in patients presenting with cryptogenic stroke?
In the general population, ischemic strokes (IS) affect 5%-10% of young patients, and this proportion increases with age7575. Nacu A, Fromm A, Sand K, Thomassen L, Naess H. Age dependency of ischaemic stroke subtypes and vascular risk factors in western Norway: the Bergen Norwegian Stroke Cooperation Study. Acta Neurol Scand. 2016;133(3):202-207.. Nearly one-third of the young patients diagnosed with IS remain without a recognized pathogenesis and are characterized as having cryptogenic IS7575. Nacu A, Fromm A, Sand K, Thomassen L, Naess H. Age dependency of ischaemic stroke subtypes and vascular risk factors in western Norway: the Bergen Norwegian Stroke Cooperation Study. Acta Neurol Scand. 2016;133(3):202-207.. The prevalence of stroke is 12 times higher in patients with FD than in the normal population7676. Fellgiebel A, Müller MJ, Ginsberg L. CNS manifestations of Fabry’s disease. Lancet Neurol. 2006;5(9):791-795.. Due to its rarity and diagnostic complexity, FD may remain unidentified as a potential cause for IS.
Several studies have examined the prevalence of FD in patients with cryptogenic stroke. In Eurasian countries, a prevalence of 0.5%-4% of FD was observed in young patients with cryptogenic stroke7777. Rolfs A, Böttcher T, Zschiesche M, et al. Prevalence of Fabry disease in patients with cryptogenic stroke: A prospective study. Lancet. 2005;366(9499):1794-1796.-8080. Gündoğdu AA, Kotan D, Alemdar M. The frequency of Fabry disease among young cryptogenic stroke patients in the city of Sakarya. J Stroke Cerebrovasc Dis. 2017;26(6):1334-1340.. Further, the frequency of FD was found to be as high as 4% in 721 adults aged 18-55 years in a German cohort. The authors found that this result corresponds to nearly 1.2% of the general population of patients with stroke in the same age range, assuming that approximately 27% of all strokes in this age group are cryptogenic7777. Rolfs A, Böttcher T, Zschiesche M, et al. Prevalence of Fabry disease in patients with cryptogenic stroke: A prospective study. Lancet. 2005;366(9499):1794-1796.. Subsequently, Rolf et al. (2013) conducted a prospective study in 15 European countries in 5023 patients aged 18-55 years diagnosed with IS, hemorrhagic stroke, and transient ischemic attacks7878. Rolfs A, Fazekas F, Grittner U, et al. Acute cerebrovascular disease in the young: The stroke in young fabry patients study. Stroke. 2013;44(2):340-349.. This study reported 0.5% definite FD diagnoses and an additional 0.4% probable diagnoses confirmed by biochemical findings7878. Rolfs A, Fazekas F, Grittner U, et al. Acute cerebrovascular disease in the young: The stroke in young fabry patients study. Stroke. 2013;44(2):340-349.. The Lombardia GENS Registry identified monogenic disorders in 7% of the 209 young patients with cryptogenic stroke7979. Bersano A, Markus HS, Quaglini S, et al. Clinical pregenetic screening for stroke monogenic diseases: Results from lombardia GENS registry. Stroke. 2016;47(7):1702-1709.. Monogenic diseases were assessed using specific clinical and radiological diagnostic algorithms for the following five monogenic diseases: cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL), FD, mitochondrial encephalomyopathy, lactic acidosis, stroke-like episodes (MELAS), hereditary cerebral amyloid angiopathy (H-CAA), and Marfan syndrome. They found only 1 (0.5%) patient with FD evaluated using α-Gal A activity dosage and sequencing of all exons of GLA7979. Bersano A, Markus HS, Quaglini S, et al. Clinical pregenetic screening for stroke monogenic diseases: Results from lombardia GENS registry. Stroke. 2016;47(7):1702-1709.. A Turkish study with a young population with cryptogenic stroke demonstrated a prevalence of 3.7% of patients with FD with genetic analysis revealing c.680G>A (p.R227Q) VUS8080. Gündoğdu AA, Kotan D, Alemdar M. The frequency of Fabry disease among young cryptogenic stroke patients in the city of Sakarya. J Stroke Cerebrovasc Dis. 2017;26(6):1334-1340..
Studies in North and South America found a prevalence between 0.3% and 1.3% of FD in young patients with cryptogenic stroke8181. Lanthier S, Saposnik G, Lebovic G, Pope K, Selchen D, Moore DF. Prevalence of Fabry Disease and outcomes in young Canadian patients with cryptogenic ischemic cerebrovascular events. Stroke. 2017;48(7):1766-1772.-8383. Wozniak MA, Kittner SJ, Tuhrim S, et al. Frequency of unrecognized Fabry disease among young European-American and African-American men with first ischemic stroke. Stroke. 2010;41(1):78-81.. Lanthier et al. (2017) conducted a cohort study in young patients (aged 18-55 years) with cryptogenic stroke (365 patients with IS and 32 with transient ischemic attacks and speech or motor deficits) from across Canada and found a prevalence of 0.3% of FD in the sample (but considering the p.R118C variant as pathogenic)8181. Lanthier S, Saposnik G, Lebovic G, Pope K, Selchen D, Moore DF. Prevalence of Fabry Disease and outcomes in young Canadian patients with cryptogenic ischemic cerebrovascular events. Stroke. 2017;48(7):1766-1772.. The authors emphasized that the findings should be interpreted with caution as the diagnosis of FD was based on screening by α-GAL A gene sequencing and lyso-Gb3 plasma levels. Thus, false-positive results concerning female patients (45.1% of the sample was female) may occur, and underestimating FD prevalence is possible but probably minimal8181. Lanthier S, Saposnik G, Lebovic G, Pope K, Selchen D, Moore DF. Prevalence of Fabry Disease and outcomes in young Canadian patients with cryptogenic ischemic cerebrovascular events. Stroke. 2017;48(7):1766-1772..
The Stroke Prevention in Young Men study consisted of 154 young patients with cryptogenic stroke (aged 15-49 years) with a first cerebral infarction identified by discharge surveillance. Low plasma α-Gal A activity was observed in 10 patients (6.5%) but only two patients (1.3%) had GLA variants assessed by DNA sequencing8383. Wozniak MA, Kittner SJ, Tuhrim S, et al. Frequency of unrecognized Fabry disease among young European-American and African-American men with first ischemic stroke. Stroke. 2010;41(1):78-81.. The first Latin American multicenter study conducted by Reisin et al. (2018) found only one patient with FD, corresponding to 1% of the group with cryptogenic stroke (including patients with both strokes of undetermined etiology and an incomplete investigation). This patient exhibited the p.Met296Ile variant associated with late-onset FD, stroke, and angiokeratoma8282. Reisin RC, Mazziotti J, Cejas LL, et al. Prevalence of Fabry Disease in Young Patients with Stroke in Argentina. J Stroke Cerebrovasc Dis. 2018;27(3):575-582.. Ten additional oligosymptomatic patients in the family were identified, highlighting the value of screening programs in stroke patients7878. Rolfs A, Fazekas F, Grittner U, et al. Acute cerebrovascular disease in the young: The stroke in young fabry patients study. Stroke. 2013;44(2):340-349..
A meta-analysis of eight studies and 8148 patients demonstrated a prevalence of 4.5% and 3.4% of FD in men and women with cryptogenic stroke, respectively, and approximately 1% of all strokes occurred in young individuals8484. Shi Q, Chen J, Pongmoragot J, Lanthier S, Saposnik G. Prevalence of Fabry disease in stroke patients - a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2014;23(5):985-992.. These findings reinforce the relevance of screening for FD in patients with cryptogenic stroke or with clinical findings (ie, angiokeratoma and advanced atherosclerosis with vascular ectasia) to define the etiology and suggest therapy8181. Lanthier S, Saposnik G, Lebovic G, Pope K, Selchen D, Moore DF. Prevalence of Fabry Disease and outcomes in young Canadian patients with cryptogenic ischemic cerebrovascular events. Stroke. 2017;48(7):1766-1772.,8484. Shi Q, Chen J, Pongmoragot J, Lanthier S, Saposnik G. Prevalence of Fabry disease in stroke patients - a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2014;23(5):985-992.. Nevertheless, the limitations of FD diagnosis remain challenging because there are specific criteria for men and women8484. Shi Q, Chen J, Pongmoragot J, Lanthier S, Saposnik G. Prevalence of Fabry disease in stroke patients - a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2014;23(5):985-992. and systematic genetic screening is expensive8181. Lanthier S, Saposnik G, Lebovic G, Pope K, Selchen D, Moore DF. Prevalence of Fabry Disease and outcomes in young Canadian patients with cryptogenic ischemic cerebrovascular events. Stroke. 2017;48(7):1766-1772..
Summary
The data suggest that the prevalence of FD in patients presenting with cryptogenic stroke is 4.5% in men and 3.4% in women. Despite this relatively low prevalence in young patients, a careful differential diagnosis should be performed.
What is the average delay time for diagnosis in patients with FD?
Delays in FD symptom onset and accurate diagnosis can be explained by the high phenotypic variability1818. Thomas AS, Mehta AB. Difficulties and barriers in diagnosing Fabry disease: what can be learnt from the literature? Expert Opin Med Diagn. 2013;7(6):589-599.,8585. Reisin R, Perrin A, García-Pavía P. Time delays in the diagnosis and treatment of Fabry disease. Int J Clin Pract. 2017;71(1):1-8.. Patients report an average delay of >10 years between symptom onset and diagnosis1818. Thomas AS, Mehta AB. Difficulties and barriers in diagnosing Fabry disease: what can be learnt from the literature? Expert Opin Med Diagn. 2013;7(6):589-599.. Data from the Fabry Outcome Survey (FOS) database demonstrated little improvement in delay rates in recent years. In 2001, data from a cohort of 366 patients from 11 European countries found an average delay of 13.7 years in males and 16.3 years in females8686. Mehta A, Ricci R, Widmer U, et al. Fabry disease defined: Baseline clinical manifestations of 366 patients in the Fabry Outcome Survey. Eur J Clin Invest. 2004;34(3):236-242.. Delays of >20 years were common, and for some patients, there was a delay of >50 years8686. Mehta A, Ricci R, Widmer U, et al. Fabry disease defined: Baseline clinical manifestations of 366 patients in the Fabry Outcome Survey. Eur J Clin Invest. 2004;34(3):236-242.. Additionally, the database demonstrated the limitations of α-Gal A activity analysis to confirm the diagnosis of FD in women, where nearly half of the symptomatic women had enzyme levels within normal range. Another issue was the misdiagnosis of FD, particularly in the absence of affected family members8686. Mehta A, Ricci R, Widmer U, et al. Fabry disease defined: Baseline clinical manifestations of 366 patients in the Fabry Outcome Survey. Eur J Clin Invest. 2004;34(3):236-242.. An analysis of FOS data in 2005 (750 patients from 13 countries) showed subtle improvement compared with 2001 data: a delay of 12.2 years for males and 12.4 years for females8787. Mehta A, Beck M, Sunder-Plassmann G. Fabry disease: Perspectives from 5 years of FOS. In: Oxford: Oxford PharmaGenesis. Oxônia, UK: Oxford PharmaGenesis; 2006..
FOS data from 2007 to 2013 suggested a mean delay of 15.1 years for adult female patients and 14.7 years for adult male patients. The mean delay between diagnosis and treatment onset was 1.4 years in females and 1.1 years in males8585. Reisin R, Perrin A, García-Pavía P. Time delays in the diagnosis and treatment of Fabry disease. Int J Clin Pract. 2017;71(1):1-8.. Children showed a mean delay of 5.5 years in the 2001-2006 period and a slight decrease to 4.4 years in the 2007-2013 period from symptom onset to diagnosis. Indeed, a noticeable reduction in the mean delay between diagnosis and treatment onset was observed in children from 2001-2006 to 2007-2013 (4.4 years and 1.3 years, respectively). A possible explanation for the overall delay in diagnosis in patients with FD is the involvement of many specialists in the diagnosis, a lack of awareness of this rare disease, the later onset of LVH in cardiac variants, and end-stage renal disease in renal variants (without previous typical symptoms)8585. Reisin R, Perrin A, García-Pavía P. Time delays in the diagnosis and treatment of Fabry disease. Int J Clin Pract. 2017;71(1):1-8..
In agreement with the previous explanation, Marchesoni et al. (2010) assessed symptomatic patients with FD to identify the most frequent diagnostic errors according to the type of specialist consulted before diagnosis8888. Marchesoni CL, Roa N, Pardal AM, et al. Misdiagnosis in Fabry disease. J Pediatr. 2010;156(5):828-831.. They reported that internists and pediatricians were the most commonly consulted/seen specialists, with neuropathic pain being the most prevalent initial sign and rheumatic fever being the most prevalent misdiagnosis. An accurate diagnosis was provided after a mean of 15.3 years in males (range, 3 months to 32 years) and 24.7 years in females (range, 1-52 years), with a mean age at symptom onset of 9.8 years in males and 10.9 years in females8888. Marchesoni CL, Roa N, Pardal AM, et al. Misdiagnosis in Fabry disease. J Pediatr. 2010;156(5):828-831..
In a study using Brazilian data from 126 patients derived from the Fabry Registry by Martins et al (2013), the median age at diagnosis was found to be 31.9 years in males and 27.1 years in females. The median age at onset of symptoms was 9.8 years in males and 11.4 years in females. The median time between the onset of first symptoms and diagnosis was 20.3 years in males and 14.3 years in females, which was longer than that observed for the overall Fabry Registry population (ie,11 years for males and 11.4 years for females)3434. Martins AM, Kyosen SO, Garrote J, et al. Demographic characterization of Brazilian patients enrolled in the Fabry Registry. Genet Mol Res. 2013;12(1):136-142..
Recently, Rosa Neto et al. (2020) described a cohort in Brazil and investigated the misdiagnoses, time to correct diagnosis or determination of GLA status, and time to treatment initiation3333. Rosa Neto NS, Bento JCDB, Pereira RMR. Higher rate of rheumatic manifestations and delay in diagnosis in Brazilian Fabry disease patients. Adv Rheumatol. 2020;60(1):1-8.. Interestingly, a higher prevalence of misdiagnosis in males (68.8%) and females (61.9%) was observed. Many patients were diagnosed with one or more rheumatological conditions before the correct diagnosis. Women (17.9 years) had a significantly lower mean time to diagnosis after symptom onset than men (21.6 years) and a similar age at diagnosis (35.9 years for females and 35.5 years for males)3333. Rosa Neto NS, Bento JCDB, Pereira RMR. Higher rate of rheumatic manifestations and delay in diagnosis in Brazilian Fabry disease patients. Adv Rheumatol. 2020;60(1):1-8..
To improve physicians' knowledge regarding FD and reduce both diagnostic and therapeutic delays, Savary et al. (2017) conducted a study evaluating the efficiency of targeted information on FD screening and diagnosis for cardiologists8989. Savary AL, Morello R, Brasse-Lagnel C, Milliez P, Bekri S, Labombarda F. Enhancing the diagnosis of fabry disease in cardiology with a targeted information: A before-after control-impact study. Open Hear. 2017;4(1):e000567.. The information consisted of an educational booklet and oral information (a 10-minute presentation by a cardiologist specialist) and screening tools (kits for biochemical screening and genetic analysis). Initially, cardiologists answered a short questionnaire regarding the number of patients screened and diagnosed for FD in the past 3 years. After a 12-month study period, they assessed the targeted information on FD and retrospectively collected clinical data from the screened population. The study improved the cardiologists' knowledge of FD, favoring early recognition of cardiac involvement. These findings suggest that the cardiologists were qualified to provide the diagnosis and treatment before onset of renal or neurological damage8989. Savary AL, Morello R, Brasse-Lagnel C, Milliez P, Bekri S, Labombarda F. Enhancing the diagnosis of fabry disease in cardiology with a targeted information: A before-after control-impact study. Open Hear. 2017;4(1):e000567.. Poor recognition of the initial signs of FD (including neuropathic pain and gastrointestinal symptoms) leads to late diagnosis where heart, brain, or kidney involvement has already occurred8888. Marchesoni CL, Roa N, Pardal AM, et al. Misdiagnosis in Fabry disease. J Pediatr. 2010;156(5):828-831..
Summary
The average delay for diagnosis in patients with FD in Brazil is 20.3 years in males and 14.3 years in females, which is higher than in the Fabry Registry and FOS population.
Discussion and Conclusion
This narrative review summarized and collated current evidence concerning the epidemiological, clinical, and diagnostic aspects of patients with FD. The key points of these findings are shown in Figure 1. In this study, the epidemiological data demonstrated that the prevalence of cryptogenic stroke is 12 times higher in patients with FD compared with the general population and affects 4.5% of men and 3.4% of women with FD. Clinical and diagnostic data indicated the role of lyso-Gb3 in diagnosis of FD patients. The elevated concentrations of lyso-Gb3 in plasma, urine, or DBS with concomitant meticulous clinical and additional complementary exams might be used to support the diagnosis of FD and for biochemical monitoring. Regarding the diagnosis of VUS, a comprehensive multidomain phenotyping (ie, clinical, biochemical, molecular genetic, and histological [in selected cases] analysis) is essential to investigate the severity of pathogenic GLA variants and to establish the pathogenicity of VUS. To identify FD patients with renal, cardiac, and neurological impairment, the earliest and most reliable markers are renal biopsy, cardiac strain imaging and noncontrast myocardial T1 mapping, and brain MRI and functional transcranial Doppler sonography, respectively. Despite the availability of all these resources in Brazil, the average delay time for diagnosis of FD patients is 20.3 years in males and 14.3 years in females, highlighting the importance of recognizing the clinical signs and early and accurate diagnosis.
Acknowledgments
Medical writing and editorial assistance were provided by Ruth Bartelli Grigolon and Joana Balardin of Kantar Health Division, São Paulo, Brazil and funded by Takeda Pharmaceutical Company.
References
- 1. El-Abassi R, Singhal D, England JD. Fabry’s disease. J Neurol Sci 2014;344(1-2):5-19.
- 2. Arends M, Wanner C, Hughes D, et al Characterization of classical and nonclassical fabry disease: a multicenter study. J Am Soc Nephrol 2017;28(5):1631-1641.
- 3. Bernardes TP, Foresto RD, Kirsztajn GM. Fabry disease: genetics, pathology, and treatment. Rev Assoc Med Bras 2020;66(Suppl 1):10-16.
- 4. Germain DP, Fouilhoux A, Decramer S, et al Consensus recommendations for diagnosis, management and treatment of Fabry disease in paediatric patients. Clin Genet 2019;96(2):107-117.
- 5. Ries M, Mengel E, Kutschke G, et al Use of gabapentin to reduce chronic neuropathic pain in Fabry disease. J Inherit Metab Dis 2003;26(4):413-414.
- 6. Meikle PJ, Hopwood JJ, Clague AE, Carey WF. Prevalence of lysosomal storage disorders. JAMA 1999;281(3):249-254.
- 7. Poorthuis BJHM, Wevers RA, Kleijer WJ, et al The frequency of lysosomal storage diseases in The Netherlands. Hum Genet 1999;105(1-2):151-156.
- 8. Hoffmann B, Mayatepek E. Fabry disease - often seen, rarely diagnosed. Dtsch Arztebl Int 2009;106(26):440-447.
- 9. Germain DP. Fabry disease. Orphanet J Rare Dis 2010;5(1):30.
- 10. Spada M, Pagliardini S, Yasuda M, et al High incidence of later-onset Fabry disease revealed by newborn screening. Am J Hum Genet 2006;79(1):31-40.
- 11. Mechtler TP, Stary S, Metz TF, et al Neonatal screening for lysosomal storage disorders: feasibility and incidence from a nationwide study in Austria. Lancet 2012;379(9813):335-341.
- 12. Hwu W, Chien Y, Lee N, et al Newborn screening for Fabry disease in Taiwan reveals a high incidence of the later‐onset GLA mutation c. 936+ 919G>A (IVS4+919G>A). Hum Mutat 2009;30(10):1397-1405.
- 13. Smid BE, van der Tol L, Biegstraaten M, Linthorst GE, Hollak CEM, Poorthuis BJHM. Plasma globotriaosylsphingosine in relation to phenotypes of fabry disease. J Med Genet 2015;52(4):262-268.
- 14. Nakao S, Takenaka T, Maeda M, et al An atypical variant of Fabry’s disease in men with left ventricular hypertrophy. N Engl J Med 1995;333(5):288-293.
- 15. Oliveira JP, Ferreira S. Multiple phenotypic domains of Fabry disease and their relevance for establishing genotype - phenotype correlations. Appl Clin Genet 2019;12:35-50.
- 16. El Sayed M, Hirsch A, Boekholdt M, et al Influence of sex and phenotype on cardiac outcomes in patients with Fabry disease. Heart 2021;107(23):1889-1897.
- 17. Echevarria L, Benistan K, Toussaint A, et al X‐chromosome inactivation in female patients with Fabry disease. Clin Genet 2016;89(1):44-54.
- 18. Thomas AS, Mehta AB. Difficulties and barriers in diagnosing Fabry disease: what can be learnt from the literature? Expert Opin Med Diagn 2013;7(6):589-599.
- 19. Bugescu N, Naylor PE, Hudson K, Aoki CD, Cordova MJ, Packman W. The psychosocial impact of Fabry disease on pediatric patients. J Pediatr Genet 2016;5(3):141-149.
- 20. Ramaswami U, Najafian B, Schieppati A, Mauer M, Bichet DG. Assessment of renal pathology and dysfunction in children with Fabry disease. Clin J Am Soc Nephrol 2010;5(2):365-370.
- 21. Popli S, Leehey DJ, Molnar Z, Nawab ZM, Ing TS. Demonstration of Fabry’s disease deposits in placenta. Am J Obstet Gynecol 1990;162(2):464-465.
- 22. Vedder AC, Strijland A, M A vd BW, Florquin S, Aerts J, Hollak CEM. Manifestations of Fabry disease in placental tissue. J Inherit Metab Dis 2006;29(1):106-111.
- 23. Torra R. Renal manifestations in Fabry disease and therapeutic options. Kidney Int Suppl 2008;74(111):S29-S32.
- 24. Kobayashi M, Ohashi T, Iizuka S, et al Frequency of de novo mutations in Japanese patients with Fabry disease. Mol Genet Metab Rep 2014;1:283-287.
- 25. Rodríguez-Marí A, Coll MJ, Chabás A. Molecular analysis in Fabry disease in Spain: fifteen novel GLA mutations and identification of a homozygous female. Hum Mutat 2003;22(3):258.
- 26. Germain DP, Oliveira JP, Bichet DG, et al Use of a rare disease registry for establishing phenotypic classification of previously unassigned GLA variants: a consensus classification system by a multispecialty Fabry disease genotype-phenotype workgroup. J Med Genet 2020;57(8):542-551.
- 27. Koulousios K, Stylianou K, Pateinakis P, et al Fabry disease due to D313Y and novel GLA mutations. BMJ Open 2017;7(10):e017098.
- 28. Human Gene Mutation Database. The Human Gene Mutation Database at the Institute of Medical Genetics in Cardiff. [Internet]. 2022 2021 July 15>. Available from: http://www.hgmd.cf.ac.uk/ac/index.php
» http://www.hgmd.cf.ac.uk/ac/index.php - 29. Ishii S. Pharmacological chaperone therapy for Fabry disease. Proc Jpn Acad Ser B Phys Biol Sci 2012;88(1):18-30.
- 30. Germain DP, Hughes DA, Nicholls K, et al Treatment of Fabry’s Disease with the Pharmacologic Chaperone Migalastat. N Engl J Med 2016;375(6):545-555.
- 31. Sartori DJ, Leivas PGC, de Souza MV, Krug BC, Balbinotto G, Schwartz IVD. Judicialização do acesso ao tratamento de doenças genéticas raras: A doença de Fabry no Rio Grande do Sul. Cienc Saude Colet 2012;17(10):2717-2728.
- 32. Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: Audit of primary sources. BMJ 2005;331(7524):1064-1065.
- 33. Rosa Neto NS, Bento JCDB, Pereira RMR. Higher rate of rheumatic manifestations and delay in diagnosis in Brazilian Fabry disease patients. Adv Rheumatol 2020;60(1):1-8.
- 34. Martins AM, Kyosen SO, Garrote J, et al Demographic characterization of Brazilian patients enrolled in the Fabry Registry. Genet Mol Res 2013;12(1):136-142.
- 35. Levstek T, Vujkovac B, Podkrajsek KT. Biomarkers of fabry nephropathy: Review and future perspective. Genes (Basel) 2020;11(9):1091.
- 36. Togawa T, Kodama T, Suzuki T, et al Plasma globotriaosylsphingosine as a biomarker of Fabry disease. Mol Genet Metab 2010;100(3):257-261.
- 37. Auray-Blais C, Ntwari A, Clarke JTR, et al How well does urinary lyso-Gb3 function as a biomarker in Fabry disease? Clin Chim Acta 2010;411(23-24):1906-1914.
- 38. Maruyama H, Takata T, Tsubata Y, et al Screening of male dialysis patients for Fabry disease by plasma globotriaosylsphingosine. Clin J Am Soc Nephrol 2013;8(4):629-636.
- 39. Nowak A, Mechtler T, Kasper DC, Desnick RJ. Correlation of Lyso-Gb3 levels in dried blood spots and sera from patients with classic and Later-Onset Fabry disease. Mol Genet Metab 2017;121(4):320-324.
- 40. Maruyama H, Miyata K, Mikame M, et al Effectiveness of plasma lyso-Gb3 as a biomarker for selecting high-risk patients with Fabry disease from multispecialty clinics for genetic analysis. Genet Med 2019;21(1):44-52.
- 41. Rossi F, L’Imperio V, Marti HP, et al Proteomics for the study of new biomarkers in Fabry disease: State of the art. Mol Genet Metab 2021;132(2):86-93.
- 42. Poorthuis BJ, Groener JE, Ottenhoff R, Wijburg FA, Hollak CE, Aerts JM. Elevated globotriaosylsphingosine as a hallmark of Fabry disease. Chem Phys Lipids 2008;154:S19-S20.
- 43. Alharbi FJ, Baig S, Rambhatla SB, et al The clinical utility of total concentration of urinary globotriaosylsphingosine plus its analogues in the diagnosis of Fabry disease. Clin Chim Acta 2020;500:120-127.
- 44. Svarstad E, Marti HP. The Changing Landscape of Fabry Disease. Clin J Am Soc Nephrol 2020;15(4):569-576.
- 45. Mitobe S, Togawa T, Tsukimura T, et al Mutant α-galactosidase A with M296I does not cause elevation of the plasma globotriaosylsphingosine level. Mol Genet Metab 2012;107(3):623-626.
- 46. Whitfield PD, Calvin J, Hogg S, et al Monitoring enzyme replacement therapy in Fabry disease - role of urine globotriaosylceramide. J Inherit Metab Dis 2005;28(1):21-33.
- 47. Sueoka H, Ichihara J, Tsukimura T, Togawa T, Sakuraba H. Nano-LC-MS/MS for quantification of lyso-Gb3 and its analogues reveals a useful biomarker for Fabry disease. PLoS One 2015;10(5):e0127048.
- 48. Auray-Blais C, Blais CM, Ramaswami U, et al Urinary biomarker investigation in children with Fabry disease using tandem mass spectrometry. Clin Chim Acta 2014;438:195-204.
- 49. Ferreira S, Auray-Blais C, Boutin M, et al Variations in the GLA gene correlate with globotriaosylceramide and globotriaosylsphingosine analog levels in urine and plasma. Clin Chim Acta 2015;447:96-104.
- 50. Yamashita S, Saotome M, Satoh H, et al Plasma globotriaosylsphingosine level as a primary screening target for Fabry disease in patients with left ventricular hypertrophy. Circ J 2019;83(9):1901-1907.
- 51. Auray-Blais C, Lavoie P, Boutin M, et al Biomarkers associated with clinical manifestations in Fabry disease patients with a late-onset cardiac variant mutation. Clin Chim Acta 2017;466:185-193.
- 52. Politei J, Alberton V, Amoreo O, et al Clinical parameters, lysoGb3, podocyturia, and kidney biopsy in children with Fabry disease: is a correlation possible? Pediatr Nephrol 2018;33(11):2095-2101.
- 53. Liao HC, Hsu TR, Young L, et al Functional and biological studies of α-galactosidase A variants with uncertain significance from newborn screening in Taiwan. Mol Genet Metab 2018;123(2):140-147.
- 54. Filoni C, Caciotti A, Carraresi L, et al Functional studies of new GLA gene mutations leading to conformational Fabry disease. Biochim Biophys Acta 2010;1802(2):247-252.
- 55. van der Tol L, Smid BE, Poorthuis BJHM, et al A systematic review on screening for fabry disease: prevalence of individuals with genetic variants of unknown significance. J Med Genet 2014;51(1):1-9.
- 56. Smid BE, van der Tol L, Cecchi F, et al Uncertain diagnosis of Fabry disease : Consensus recommendation on diagnosis in adults with left ventricular hypertrophy and genetic variants of unknown significance. Int J Cardiol 2014;177(2):400-408.
- 57. van der Tol L, Svarstad E, Ortiz A, et al Chronic kidney disease and an uncertain diagnosis of Fabry disease: approach to a correct diagnosis. Mol Genet Metab 2015;114(2):242-247.
- 58. Curiati MA, Aranda CS, Kyosen SO, et al The challenge of diagnosis and indication for treatment in fabry disease. J Inborn Errors Metab Screen 2016;5:1-7.
- 59. Abensur H, Reis MA Dos. Renal involvement in Fabry disease. J Bras Nefrol 2016;38(2):245-254.
- 60. Riccio E, Sabbatini M, Capuano I, Pisani A. Early biomarkers of fabry nephropathy: A review of the literature. Nephron 2019;143(4):274-281.
- 61. Najafian B, Mauer M, Hopkin RJ, Svarstad E. Renal complications of Fabry disease in children. Pediatr Nephrol 2013;28(5):679-687.
- 62. Tøndel C, Kanai T, Larsen KK, et al Foot process effacement is an early marker of nephropathy in young classic fabry patients without albuminuria. Nephron 2015;129(1):16-21.
- 63. Fernández A, Politei J. Cardiac manifestation of fabry disease: from hypertrophic cardiomyopathy to early diagnosis and treatment in patients without left ventricular hypertrophy. J Inborn Errors Metab Screen 2016;4:1-9.
- 64. Yogasundaram H, Nikhanj A, Putko BN, et al Elevated inflammatory plasma biomarkers in patients with fabry disease: a critical link to heart failure with preserved ejection fraction. J Am Heart Assoc 2018;7(21):1-18.
- 65. Nordin S, Kozor R, Baig S, et al Cardiac phenotype of prehypertrophic fabry disease. Circ Cardiovasc Imaging 2018;11(6):e007168.
- 66. Militaru S, Ginghin C, Popescu BA, Saftoiu A, Linhart A, Jurcut R. Multimodality imaging in Fabry cardiomyopathy: from early diagnosis to therapeutic targets. Eur Hear J Cardiovasc Imaging 2018;19(12):1313-1322.
- 67. Wilson HC, Hopkin RJ, Madueme PC, et al Arrhythmia and clinical cardiac findings in children with Anderson-Fabry disease. Am J Cardiol 2017;120(2):251-255.
- 68. Kampmann C, Wiethoff CM, Whybra C, Baehner FA, Mengel E, Beck M. Cardiac manifestations of Anderson-Fabry disease in children and adolescents. Acta Paediatr 2008;97(4):463-469.
- 69. Brooks JBB, Fragoso YD. Neurological manifestations in Fabry disease. Neuroimmunol Neuroinflammation 2016;3(10):228.
- 70. Kolodny E, Fellgiebel A, Hilz MJ, et al Cerebrovascular involvement in fabry disease: Current status of knowledge. Stroke 2015;46(1):302-313.
- 71. Burlina A, Politei J. The central nervous system involvement in fabry disease: A review. J Inborn Errors Metab Screen 2016;4:1-7.
- 72. Schiffmann R, Moore DF. Neurological manifestations of Fabry disease. In: Mehta A, Beck M, Sunder-Plassmann G, eds. Fabry Disease: Perspectives from 5 Years of FOS Oxford: Oxford PharmaGenesis; 2006.
- 73. Marchesoni C, Cisneros E, Pfister P, et al Brain MRI findings in children and adolescents with Fabry disease. J Neurol Sci 2018;395:131-134.
- 74. Politei JM, Durand C, Schenone AB. Small fiber neuropathy in fabry disease: A review of pathophysiology and treatment. J Inborn Errors Metab Screen 2016;4:1-5.
- 75. Nacu A, Fromm A, Sand K, Thomassen L, Naess H. Age dependency of ischaemic stroke subtypes and vascular risk factors in western Norway: the Bergen Norwegian Stroke Cooperation Study. Acta Neurol Scand 2016;133(3):202-207.
- 76. Fellgiebel A, Müller MJ, Ginsberg L. CNS manifestations of Fabry’s disease. Lancet Neurol 2006;5(9):791-795.
- 77. Rolfs A, Böttcher T, Zschiesche M, et al Prevalence of Fabry disease in patients with cryptogenic stroke: A prospective study. Lancet 2005;366(9499):1794-1796.
- 78. Rolfs A, Fazekas F, Grittner U, et al Acute cerebrovascular disease in the young: The stroke in young fabry patients study. Stroke 2013;44(2):340-349.
- 79. Bersano A, Markus HS, Quaglini S, et al Clinical pregenetic screening for stroke monogenic diseases: Results from lombardia GENS registry. Stroke 2016;47(7):1702-1709.
- 80. Gündoğdu AA, Kotan D, Alemdar M. The frequency of Fabry disease among young cryptogenic stroke patients in the city of Sakarya. J Stroke Cerebrovasc Dis 2017;26(6):1334-1340.
- 81. Lanthier S, Saposnik G, Lebovic G, Pope K, Selchen D, Moore DF. Prevalence of Fabry Disease and outcomes in young Canadian patients with cryptogenic ischemic cerebrovascular events. Stroke 2017;48(7):1766-1772.
- 82. Reisin RC, Mazziotti J, Cejas LL, et al Prevalence of Fabry Disease in Young Patients with Stroke in Argentina. J Stroke Cerebrovasc Dis 2018;27(3):575-582.
- 83. Wozniak MA, Kittner SJ, Tuhrim S, et al Frequency of unrecognized Fabry disease among young European-American and African-American men with first ischemic stroke. Stroke 2010;41(1):78-81.
- 84. Shi Q, Chen J, Pongmoragot J, Lanthier S, Saposnik G. Prevalence of Fabry disease in stroke patients - a systematic review and meta-analysis. J Stroke Cerebrovasc Dis 2014;23(5):985-992.
- 85. Reisin R, Perrin A, García-Pavía P. Time delays in the diagnosis and treatment of Fabry disease. Int J Clin Pract 2017;71(1):1-8.
- 86. Mehta A, Ricci R, Widmer U, et al Fabry disease defined: Baseline clinical manifestations of 366 patients in the Fabry Outcome Survey. Eur J Clin Invest 2004;34(3):236-242.
- 87. Mehta A, Beck M, Sunder-Plassmann G. Fabry disease: Perspectives from 5 years of FOS. In: Oxford: Oxford PharmaGenesis. Oxônia, UK: Oxford PharmaGenesis; 2006.
- 88. Marchesoni CL, Roa N, Pardal AM, et al Misdiagnosis in Fabry disease. J Pediatr 2010;156(5):828-831.
- 89. Savary AL, Morello R, Brasse-Lagnel C, Milliez P, Bekri S, Labombarda F. Enhancing the diagnosis of fabry disease in cardiology with a targeted information: A before-after control-impact study. Open Hear 2017;4(1):e000567.
Publication Dates
-
Publication in this collection
07 Mar 2022 -
Date of issue
2022
History
-
Received
16 July 2021 -
Accepted
13 Jan 2022



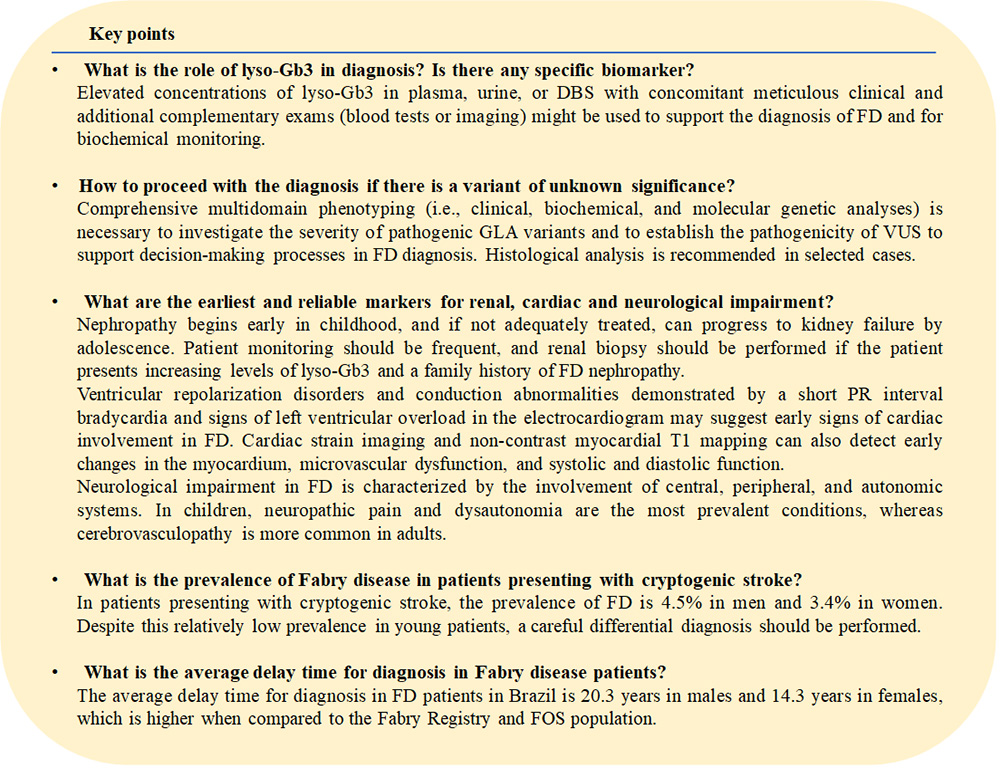 FD: Fabry disease; GLA: α-galactosidase A; VUS: variant of unknown significance; ECG: electrocardiogram; FOS: Fabry Outcome Survey.
FD: Fabry disease; GLA: α-galactosidase A; VUS: variant of unknown significance; ECG: electrocardiogram; FOS: Fabry Outcome Survey.