OBJECTIVES:
To compare coronary artery bypass to stenting in our institution, and to compare the studied samples for major adverse cardiac and cerebrovascular outcomes.
METHOD:
An observational cohort study. We analyzed 202 patients undergoing coronary artery surgical revascularization versus stenting in our institution between January 17 and July 31, 2009; patients were stratified into: Group G1-STENT, patients who received stents; and Group G2-CABG, patients submitted to coronary artery by-pass grafting. A script containing 62 clinical, hemodynamic and surgical items was used for data collection from medical records.
RESULTS:
Womenmade up a higher percentage of G1-STENT 44%versus 26% in G2-CABG. Diabetics predominated in G2-CABG, 46% versus 29% in G1-STENT. Three or more coronary branches showed a higher percentage in G2- CABG, 55% vs, 9.0%; in G1-STENT, 64% had only one coronary branch involvement. Non-elective procedures were higher for G1-STENT (21%vs. 9%).Worse postoperative renal function occurred inG2-CABG (15% vs. 2%). G1-STENT patients had shorter hospital time. Recurrence of angina was higher in patients in G1-STENT (11% vs. 2%) with no significant difference in hospital mortality. Postoperative quality of life increased from 45% to 55% in G2-CABG.
CONCLUSIONS:
Surgical revascularization is the best procedure for patients with multi vessel coronary disease, especially in diabetic patients: it allows a significantly more complete revascularization, reduces the number of readmissions due to cardiac causes, reduces the recurrence of angina and improves quality of life after surgery, with hospital and late mortality rates similar to those obtained through stenting.
KEYWORDS:
Coronary Artery Bypass; Coronary Artery Bypass, Off-Pump; Myocardial Revascularization; Stents
RESUMO
OBJETIVOS:
Comparar a cirurgia de revascularização versus implante de stent em nossa instituição, e comparar as amostras estudadas para eventos cardíacos e cerebrovasculares adversos.
MÉTODO:
Um estudo observacional de coorte. Foram analisados 202 pacientes submetidos a revascularização miocárdica em nossa instituição entre 17 de janeiro e 31 de julho de 2009. Os pacientes foram estratificados em: Grupo G1-stent, os pacientes que receberam stents; e Grupo G2-operatório de CRM, os pacientes submetidos a revascularização do miocárdio por by-pass. Um script contendo 62 itens clínicos, hemodinâmicos e cirúrgicos foi usado para a coleta de dados dos prontuários médicos.
RESULTADOS:
As mulheres representaram um percentual maior de G1-stent versus G2-Revascularização (44% versus 26%), diabéticos predominaram no G2-Revascularização, 46% versus 29% no G1-stent. Três ou mais ramos coronarianos apresentaram maior percentual em G2-Revascularização, 55% vs, 9.0%; no grupo G1-stent, 64% apresentavam apenas envolvimento de uma artéria coronária. Procedimentos não eletivos foram mais frequentes para G1-stent (21% contra 9%). A função renal no pós-operatório apresentou-se pior no grupo G2-Revascularização (15% contra 2%). Pacientes G1-stent tiveram menor tempo hospitalização. A recorrência de angina foi maior nos pacientes do G1-stent (11% contra 2%), sem diferença significativa na mortalidade hospitalar. A qualidade de vida no pós-operatório aumentou de 45% para 55% em G2-Revascularização.
CONCLUSÃO:
A revascularização cirúrgica é o melhor procedimento para pacientes com doença coronariana múltipla, especialmente em pacientes diabéticos: permite a revascularização significativamente mais completa, reduz o número de reinternações por causas cardíacas, reduzindo o retorno da angina e melhora a qualidade de vida após cirurgia, com taxas hospitalares e de mortalidade tardia semelhantes aos obtidos por meio de implante de stent.
INTRODUCTION
Percutaneous coronary intervention (PCI) is used on a large scale as a first-line treatment in patients with coronary artery disease (CAD),11 Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. SYNTAX Investigators. Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease. N Eng J Med. 2009;360(10):961-72. but the advantage of surgical revascularization (CABG) over this procedure is seen in patients with left coronary trunk disease, multivessel disease and those with diffuse involvement of the coronary arteries, resulting in lower rates of cardiac adverse clinical outcomes in the first year of follow-up.11 Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. SYNTAX Investigators. Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease. N Eng J Med. 2009;360(10):961-72.,22 Ito H. Optimal treatment for coronary artery disease in patients with diabetes: percutaneous coronary intervention, coronary artery bypass graft, and medications. Gen Thorac Cardiovasc Surg. 2011;59(1):6-13. Patients with multivessel disease, treatment using "stents" coated with drugs, when compared with surgical revascularization, show similar rates for mortality and concomitant clinical outcomes, but higher rates of redo-revascularization after five years of follow-up.33 Park DW, Kim YH, Song HG, Ahn JM, Oh J, Kim WJ, et al. Long-term comparison of drug-eluting stents and coronary artery bypass grafting for multivessel coronary revascularization 5-year outcomes from the Asan medical center-multivessel revascularization registry. J Am Coll Cardiol. 2011;57(2):128-37.
For patients with complex coronary artery disease, where complete revascularization cannot be obtained using the PCI, CABG is the alternative that can be offered; however, for patients with less complex disease, PCI represents a valid alternative even if revascularization cannot be fully obtained.44 Sarno G, Garg S, Onuma Y, Gutiérrez-Chico JL, van den Brand MJ, Rensing BJ, et al. ARTS-II Investigators. Impact of completeness of revascularization on the five-year outcome in percutaneous coronary intervention and coronary artery bypass graft patients (from the ARTS-II study). Am J Cardiol. 2010;106(10):1369-75.
The objective of this project was to analyze CABG versus stents and compare the studied populations with respect to clinical and major adverse cardiac and cerebrovascular outcomes.
The choice of the most appropriate method for myocardial revascularization in patients with obstructive coronary artery disease is subject to controversy. The information provided by this project aims to contribute to resolve this doubt within the Brazilian scenario.
METHODS AND PATIENTS
This is an observational study of a non-concurrent cohort involving 202 consecutive patients undergoing coronary artery bypass surgery or percutaneous coronary intervention at the Heart Institute, São Paulo University Medical College during the period between January 17 and July 31, 2009. During this period a total of 2,858 patients were operated upon, 478 of whom underwent coronary artery bypass grafting. The minimum size of the study sample was set at 90 patients per group using a significance level of 5% and a power of 80% in a two-tailed test. Patients who submitted to stenting received uncoated stents. The target population was stratified into two study samples. The first group (G1) was composed of 112 patients who underwent percutaneous coronary intervention - PCI, with placement of stents. The second group (G2) comprised 90 patients who were treated with CABG. A special script for data collection was prepared in advance and contained 62 clinical, hemodynamic and surgical items. Data were collected from medical records. The software used for the statistical analysis was SPSS 15.0 for Windows - Statistical Package for Social Sciences. The level of significance was set at 5%. The Ethics Committee of the Institution approved the project.
RESULTS
The two groups were very similar, with a significant percentage difference only relative to gender, with female predominance in G1-PCI, which had 44% versus 26% in G2-CABG as shown in Table 1.
Table 2 shows clinical conditions prevailing before the corrective procedures. There was a significantly higher percentage of diabetics in group G2-CABG, 46% vs. 29% in group G1-PCI. The other clinical conditions showed no statistical differences between groups.
Table 3 shows the number of injured coronary branches, where there was a significantly greater number of injured branches in G2 vs. G1 [3.0 (1-5) vs. 1.00 (1-4) p = 0.001]. This was reflected in the distribution of the number of stents placed and the amount of surgically treated coronary branches, which showed 72 G1 patients (64.3%) receiving only one stent, while in G2, the highest concentration of patients ranged from 2 -4 grafts.
Table 4 shows clinical conditions post-procedure; CABG was significantly associated with a transient, but significant, worsening of renal function, expressed by the percentage of serum creatinine levels higher than 2mg/dl in the postoperative period. There was no significant difference regarding the presence of congestive heart failure after hospital discharge. However, as was expected, the G2 group had a longer hospital stay [16.0 (7 - 65) versus 3.0 (0 - 101) days, p = 0.001], There was a higher incidence of hospital readmission for cardiac causes in the PCI group (table 4).
Table 5 shows that the recurrence of angina after the procedures is significantly higher in the group treated by percutaneous coronary intervention and also shows that hospital mortality is similar between the two groups of patients.
The percentage decline in quality of life was attributed to the fact that observation was performed in the first thirty days of the postoperative period. During this interval, patients do not yet feel the benefits of the intervention, due to the trauma of the procedure.
DISCUSSION
Our results show that CABG is a good method for the treatment of patients with coronary artery disease, especially those with diabetes, as it allows for a more complete revascularization, reduces the number of hospital readmissions due to cardiac causes, reduces the recurrence of angina after the procedure, and enhances the quality of life, with similar hospital mortality in comparison to that obtained by percutaneous revascularization by stents.
The results of the study confirm, in our institution, the superiority of surgery in relation to percutaneous treatment with stents and providing a subsidy to the cardiologist in choosing the most appropriate procedure for patients. Our finding is in agreement with the recommendations made by the ESC-EACTS,55 Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS), European Association for Percutaneous Cardiovascular Interventions (EAPCI), Kolh P, et al. Guidelines on myocardial revascularization. Eur J Cardiothorac Surg. 2010;38(Suppl):S1-52. ACCF/AHA66 Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al. Special Articles: 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Anesth Analg. 2012;114(1):11-45. and the STS,77 CABG vs. Stents, Know Your Options|STS. http://www.sts.org/patient-information/adult-cardiac-surgery/cabg-vs-stents-know-your-options (29/7/2014 08:30:07).
http://www.sts.org/patient-information/a...
,88 Taggart DP. Stents or surgery in coronary artery disease in 2013. Ann Cardiothorac Surg. 2013;2(4):431-4. for the treatment of obstructive coronary artery disease.
Our results are at a difference with Park et al33 Park DW, Kim YH, Song HG, Ahn JM, Oh J, Kim WJ, et al. Long-term comparison of drug-eluting stents and coronary artery bypass grafting for multivessel coronary revascularization 5-year outcomes from the Asan medical center-multivessel revascularization registry. J Am Coll Cardiol. 2011;57(2):128-37. when comparing CABG with stenting in patients with multivessel disease; their study concludes that treatment through the stents displays similar rate of mortality and clinical outcomes in five years follow-up. They claim an even greater benefit with respect to stenting in patients with two-vessel lesions although they do note a higher reintervention rate in this group. In a second report, Park et al99 Park SJ, Kim YH, Park DW, Yun SC, Ahn JM, Song HG, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011;364(18):1718-27. describe findings in a randomized study comparing two methods for myocardial revascularization in patients with left main coronary artery lesion. They conclude that percutaneous intervention by the stents is not worse than that obtained by surgery with regard to the following cardiovascular and cerebrovascular primary outcomes: death from any cause, myocardial infarction, cerebral ischemia or secondary to incomplete treatment of lesions in target vessel stroke in an observation period of one year. This is also not consistent with our results.
A limitation of our study is that even though it provides evidence regarding the best therapy for the treatment of coronary artery disease, our statement would be more robust if we had analyzed a larger number of patients.
To conclude this discussion, it is worth noting that the results analyzed in this study refer to surgical stent placement and coronary artery by-pass procedures performed in 2009. Figure 1 displays a historical series of mortality over the 30 year-period from 1984-2007. It can be seen that over these years mortality in the institution ranged between 2.7-7.3% with inter-year averages clustered around 4.3-4.8%, with no significant trend between over the period.1010 Lisboa LAF, Moreira LFP, Mejia OV, Dallan LAO, Pomerantzeff PMA, Costa R, et al. Evolution of cardiovascular surgery at the Instituto do Coraçáo: analysis of 71,305 surgeries. Arq. Bras. Cardiol. 2010;94(2):174-81. Even though Inter-year averages are steady, noteworthy upward deviations occurred during three specific years (1986, 1999, 2006).
Historical mortality series for the Heart Institute, Sa˜o Paulo, Brazil for the period 1984 – 2007. Modified from Lisboa et al.1010 Lisboa LAF, Moreira LFP, Mejia OV, Dallan LAO, Pomerantzeff PMA, Costa R, et al. Evolution of cardiovascular surgery at the Instituto do Coraçáo: analysis of 71,305 surgeries. Arq. Bras. Cardiol. 2010;94(2):174-81.
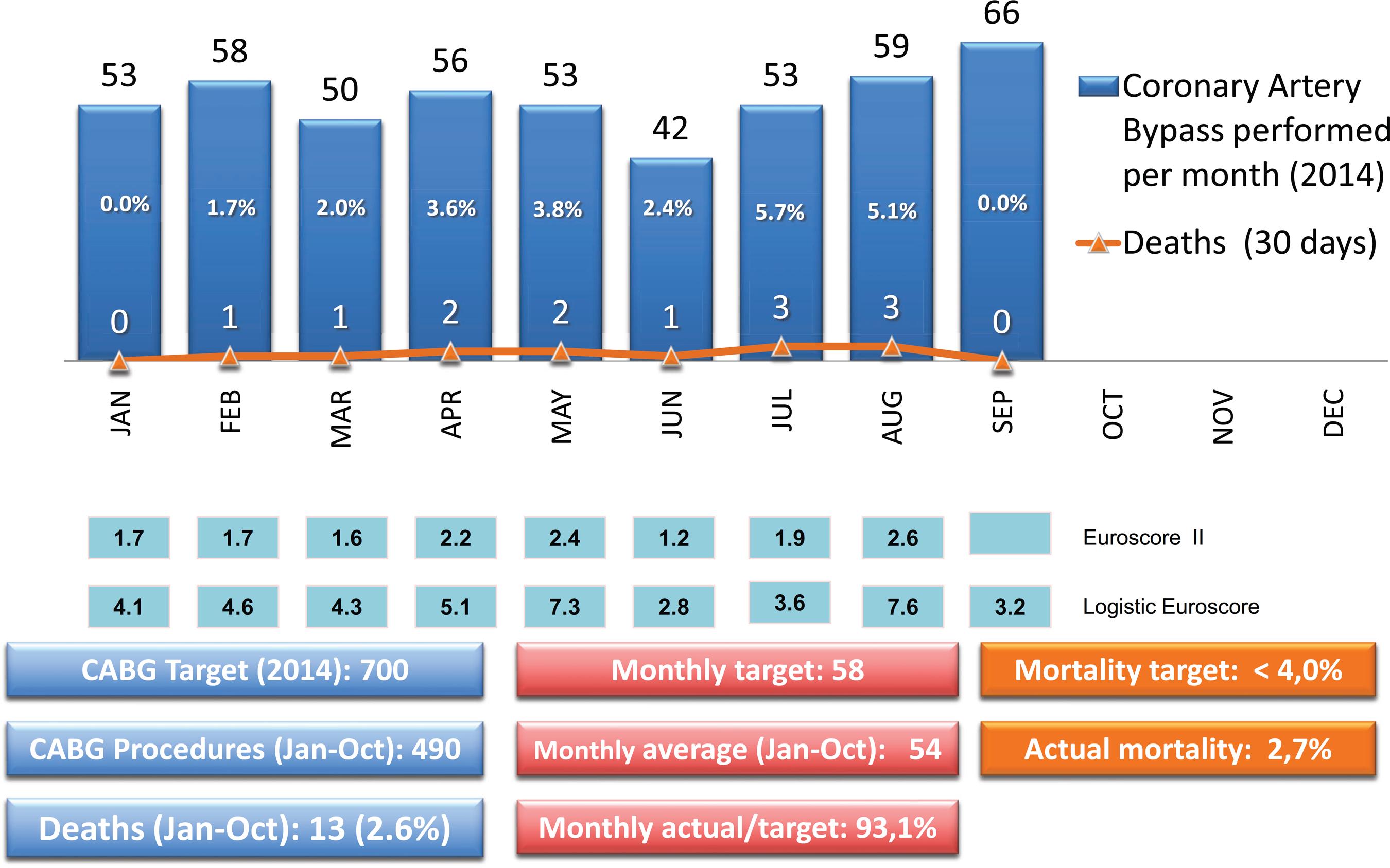
At the time of writing, improvements have been introduced under the auspices of the Director of the Surgical Division. These improvements involve a stricter quality control resulting in increased patient safety. As a consequence, mortality has decreased and is now equivalent to international high-grade centers. In this regard we quote from a report from the Duke Clinical Research Institute, which shows that unadjusted isolated coronary artery bypass operative mortality ranged between 1.8-2.6% over the period 2003-2012.1111 Grover FL, Shroyer LA, Hammermeister K, Edwards FH, Ferguson TB Jr, Dziuban SW Jr, A Decade's Experience with Quality Improvement in Cardiac Surgery Using the Veterans Affairs and Society of Thoracic Surgeons National Databases. Ann Surg. 2001;234(4):464-74. Figure 2 shows that as a consequence of these controls, average monthly mortality in our institution has dropped over the first nine months of 2014. It is presently 2.6% for a total population of 490 operated patients.
Monthly mortality (30 days) rates for January – September, 2014. The total number of deaths was 13 out of a population of 490 operated patients
CONCLUSIONS
The evidence allows us to claim that CABG is the best procedure to treat patients with multi-vessel coronary artery disease, especially diabetics, since it significantly allows for a more complete revascularization, reduces the number of readmissions due to cardiac causes, decreases the reappearance of angina and improves quality of life in the postoperative period, with similar percentages for hospital and late mortality. CABG is a safe and effective procedure with good prognosis. Not to offer it to bearers of obstructive coronary artery disease may represent a denial of the best treatment option to the patients; it may be argued that obtaining consent for percutaneous intervention may involve conflicts of interest; therefore these patients should be treated by a multidisciplinary team including a cardiovascular surgeon.
-
Iglezias JCR, Chi A, Dallan LAO, Moreira LFP, Jatene FB. Surgical myocardial revascularization versus stents. MEDICALEXPRESS. 2014;1(6):341-345.
ACKNOWLEDGEMENTS
This study was supported by a grant from Fundação de Amparo a Pesquisa do Estado de São Paulo (grant # 2010/00796-1). We sincerely thank the students of the Medical School of São Paulo University for the clinical follow-up of all patients included in this study.
REFERENCES
-
1Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. SYNTAX Investigators. Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease. N Eng J Med. 2009;360(10):961-72.
-
2Ito H. Optimal treatment for coronary artery disease in patients with diabetes: percutaneous coronary intervention, coronary artery bypass graft, and medications. Gen Thorac Cardiovasc Surg. 2011;59(1):6-13.
-
3Park DW, Kim YH, Song HG, Ahn JM, Oh J, Kim WJ, et al. Long-term comparison of drug-eluting stents and coronary artery bypass grafting for multivessel coronary revascularization 5-year outcomes from the Asan medical center-multivessel revascularization registry. J Am Coll Cardiol. 2011;57(2):128-37.
-
4Sarno G, Garg S, Onuma Y, Gutiérrez-Chico JL, van den Brand MJ, Rensing BJ, et al. ARTS-II Investigators. Impact of completeness of revascularization on the five-year outcome in percutaneous coronary intervention and coronary artery bypass graft patients (from the ARTS-II study). Am J Cardiol. 2010;106(10):1369-75.
-
5Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS), European Association for Percutaneous Cardiovascular Interventions (EAPCI), Kolh P, et al. Guidelines on myocardial revascularization. Eur J Cardiothorac Surg. 2010;38(Suppl):S1-52.
-
6Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al. Special Articles: 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Anesth Analg. 2012;114(1):11-45.
-
7CABG vs. Stents, Know Your Options|STS. http://www.sts.org/patient-information/adult-cardiac-surgery/cabg-vs-stents-know-your-options (29/7/2014 08:30:07).
» http://www.sts.org/patient-information/adult-cardiac-surgery/cabg-vs-stents-know-your-options -
8Taggart DP. Stents or surgery in coronary artery disease in 2013. Ann Cardiothorac Surg. 2013;2(4):431-4.
-
9Park SJ, Kim YH, Park DW, Yun SC, Ahn JM, Song HG, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011;364(18):1718-27.
-
10Lisboa LAF, Moreira LFP, Mejia OV, Dallan LAO, Pomerantzeff PMA, Costa R, et al. Evolution of cardiovascular surgery at the Instituto do Coraçáo: analysis of 71,305 surgeries. Arq. Bras. Cardiol. 2010;94(2):174-81.
-
11Grover FL, Shroyer LA, Hammermeister K, Edwards FH, Ferguson TB Jr, Dziuban SW Jr, A Decade's Experience with Quality Improvement in Cardiac Surgery Using the Veterans Affairs and Society of Thoracic Surgeons National Databases. Ann Surg. 2001;234(4):464-74.
Publication Dates
-
Publication in this collection
Dec 2014
History
-
Received
28 Aug 2014 -
Reviewed
12 Sept 2014 -
Accepted
15 Oct 2014