ABSTRACT
Objective:
Although some previous data have suggested a high iodine intake in Brazil, the prevalence of antithyroperoxidase antibodies (TPOAb) in the country is compatible with rates from countries with adequate iodine intake. This observation emphasizes the importance of knowing the incidence of TPOAb in Brazil.
Materials and methods:
This prospective analysis included euthyroid participants with negative TPOAb at baseline and a thyroid function assessment at a 4-year follow-up. TPOAb was measured by electrochemiluminescence and considered positive when titers were ≥34 IU/mL. TSH and free T4 (FT4) levels were determined by a third-generation immunoenzymatic assay. The incidence of TPOAb is expressed in percentage per year or as a cumulative incidence within the 4-year follow-up period.
Results:
Of 8,922 euthyroid participants (mean age 51.1 years; 50.9% women) with a negative TPOAb test at baseline, 130 presented incident TPOAb at the 4-year follow-up, yielding an annual incidence of TPOAb of 0.38%/year (95% confidence interval [95% CI], 0.37-0.39%/year) and a cumulative incidence over 4 years of 1.46% (95% CI, 1.21-1.71%). In men, the annual incidence was 0.32% (95% CI, 0.31-0.33%), and the cumulative incidence over 4 years was 1.23% (95% CI, 0.90-1.56%). In women, the annual incidence was 0.43%/year (95% CI, 0.42-0.44%/year) and the cumulative incidence over 4 years was 1.67% (95% CI, 1.30-2.04%). The only factor associated with incident TPOAb was the occurrence of thyroid diseases at follow-up. No differences in TPOAb incidence were detected across ELSA-Brasil research centers.
Conclusion:
Based on the results of this study, the incidence of TPOAb per year and at a 4-year follow-up period are compatible with those of a country with adequate iodine intake.
Keywords
TPOAb; incidence; thyroid function; autoimmune thyroid disease; thyroid disease
INTRODUCTION
Thyroid disease is a global health problem with the potential of substantially impacting the health of the population. Overt and subclinical hypothyroidism due to autoimmune thyroiditis are the most common types of thyroid dysfunction in iodine-sufficient populations (11 Sgarbi JA, Maciel RMB. Pathogenesis of autoimmune thyroid diseases. Arq Bras Endocrinol Metabol. 2009;53(1):5-14.
2 Chiovato L, Lapi P, Fiore E, Tonacchera M, Pinchera A. Thyroid autoimmunity and female gender. J Endocrinol Invest. 1993;16(5):384-91.-33 Amouzegar A, Ghaemmaghami Z, Beigy M, Gharibzadeh S, Mehran L, Tohidi M, et al. Natural Course of Euthyroidism and Clues for Early Diagnosis of Thyroid Dysfunction: Tehran Thyroid Study. Thyroid. 2017;27(5):616-25.). In this context, the most important aspect for the diagnosis of autoimmune thyroid diseases is the presence of circulating antithyroperoxidase antibodies (TPOAb) (33 Amouzegar A, Ghaemmaghami Z, Beigy M, Gharibzadeh S, Mehran L, Tohidi M, et al. Natural Course of Euthyroidism and Clues for Early Diagnosis of Thyroid Dysfunction: Tehran Thyroid Study. Thyroid. 2017;27(5):616-25.
4 Hoogendoorn EH, Hermus AR, de Vegt F, Ross HA, Verbeek ALM, Kiemeney LALM, et al. Thyroid function and prevalence of anti-thyroperoxidase antibodies in a population with borderline sufficient iodine intake: influences of age and sex. Clin Chemistry. 2006;52(1):104-11.
5 Bjoro T, Holmen J, Kruger O, Midthjell K, Hunstad K, Schreiner T, et al. Prevalence of thyroid disease, thyroid dysfunction and thyroid peroxidase antibodies in a large, unselected population. The Health Study of Nord-Trondelag (HUNT). Eur J Endocrinol. 2000;143(5):639-47.-66 Amouzegar A, Gharibzadeh S, Kazemian E, Mehran L, Tohidi M, Azizi F. The Prevalence, Incidence and Natural Course of Positive Antithyroperoxidase Antibodies in a Population-Based Study: Tehran Thyroid Study. PLoS One. 2017;12(1):e0169283.).
Thyroid diseases are very common in Brazil (77 Olmos RD, Figueiredo RC, Aquino EM, Lotufo PA, Bensenor IM. Gender, race and socioeconomic influence on diagnosis and treatment of thyroid disorders in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Braz J Med Biol Res. 2015;48(8):751-8.
8 Benseñor IM, Goulart AC, Lotufo PA, Menezes PR, Scazufca M. Prevalence of thyroid disorders among older people: results from the São Paulo Ageing & Health Study. Cad Saude Publica. 2011;27(1):155-61.-99 Sichieri R, Baima J, Marante T, de Vasconcellos MT, Moura AS, Vaisman M. Low prevalence of hypothyroidism among black and Mulatto people in a population-based study of Brazilian women. Clin Endocrinol (Oxf). 2007;66(6):803-7.), a country considered to have one of the highest prevalences of hypothyroidism and hyperthyroidism worldwide (1010 Taylor PN, Albrecht D, Scholz A, Gutierrez-Buey G, Lazarus JH, Dayan CM, et al. Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol. 2018;14(5):301-6.). Although goiter was a common presentation of thyroid diseases in the past, the prevalence of this condition has decreased after compulsory salt iodination in the second half of the 20th century. A previous analysis with data from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) has shown that the prevalence of TPOAb positivity in Brazil was aligned with that of iodine-sufficient areas (1111 Janovsky CCPS, Bittencourt MS, Goulart AC, Santos IS, Almeida-Pititto B, Lotufo PA, et al. Prevalence of antithyroperoxidase antibodies in a multiethnic Brazilian population: The ELSA-Brasil Study. Arch Endocrinol Metab. 2019;63(4):351-7.), and was higher in women compared with men, with a women:men ratio of 2.2. Additionally, 60% of the individuals with positive TPOAb were white. The presence of positive TPOAb in women was associated with the entire spectrum of thyroid dysfunction, while in men, it was related only to the occurrence of overt thyroid disease (1111 Janovsky CCPS, Bittencourt MS, Goulart AC, Santos IS, Almeida-Pititto B, Lotufo PA, et al. Prevalence of antithyroperoxidase antibodies in a multiethnic Brazilian population: The ELSA-Brasil Study. Arch Endocrinol Metab. 2019;63(4):351-7.). To the best of our knowledge, no large studies have been published on the incidence of autoimmune thyroid diseases in Brazil.
The present study aimed to analyze the incidence of autoimmune thyroiditis considering all participants who had negative TPOAb levels and no thyroid dysfunction at baseline (2008-2010) and were followed up during 4 years (2012-2014). The incidence of TPOAb along the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) is presented according to the baseline sociodemographic and clinical characteristics of the participants.
MATERIALS AND METHODS
This was a prospective analysis based on a 4-year follow-up period of the ELSA-Brasil. The design and cohort profile of the ELSA-Brasil study have been previously published elsewhere (1212 Aquino EML, Barreto SM, Bensenor IM, Carvalho MS, Chor D, Duncan BB, et al. Brazilian Longitudinal Study of Adult Health (ELSA-Brasil): Objectives and Design. Am J Epidemiol. 2012;175(4):315-24.
13 Schmidt MI, Duncan BB, Mill JG, Lotufo PA, Chor D, Barreto SM, et al. Cohort Profile: Longitudinal Study of Adult Health (ELSA-Brasil). Int J Epidemiol. 2015;44(1):68-75.-1414 Benseñor IM, Griep RH, Pinto KA, Faria CP, Felisbino-Mendes M, Caetano EI, et al. Routines of organization of clinical tests and interviews in the ELSA-Brasil investigation center]. Rev Saude Publica. 2013;47 Suppl 2:37-47.). Briefly, the ELSA-Brasil is a multicenter cohort study of 15,105 active and retired civil servant employees aged between 35 and 74 years at baseline and from six cities in Brazil (Salvador, Vitória, Belo Horizonte, Rio de Janeiro, São Paulo, and Porto Alegre). Information on sociodemographic data, personal and family history of previous diseases, lifestyle risk factors, mental health, cognitive status, and occupational exposure was assessed at baseline from 2008 to 2010 and after 4 years from 2012 to 2014.
The institutional ethics committee approved the protocol of the study, and written consent was obtained from all study participants (Plataforma Brasil CAAE number 08109612.7.1001.0076).
Participants
Thyroid function tests were assessed in frozen samples stored in nitrogen. The present analysis included all participants with stored baseline samples available at the moment of the analysis (n = 13,500). No differences regarding sociodemographic or clinical characteristics were detected among participants with and without frozen samples. After exclusion of all participants with abnormal thyroid function (n = 2,420) only participants with normal thyroid function remained in the study (n = 11,080). Of 11,080 participants with normal thyroid function at baseline, we excluded 1,045 with missing information about thyroid function at follow-up, 330 who were using medications that could interfere with thyroid function assessment (15,16), 773 with positive TPOAb at baseline, and 10 with missing information about TPOAb at the follow-up assessment. After these exclusions, the final analysis comprised 8,922 participants (Figure 1).
Thyroid function
Serum for biochemistry and hormone tests was obtained from venous blood samples drawn after an overnight fast and centrifuged at 2,500 g for 15 minutes. Serum TPOAb was measured by electrochemiluminescence (Roche Diagnostics, Mannheim, Germany) and was considered positive when ≥34 IU/mL. Serum levels of TSH and FT4 were determined using a third-generation immunoenzymatic assay (Roche, USA). Serum free triiodothyronine was measured by electrochemiluminescence immunoassay. Thyroid dysfunction was defined by serum TSH and FT4 levels or by the routine use of thyroid hormones (levothyroxine) or antithyroid medications such as propylthiouracil or methimazole. Reference ranges were 0.4-4.0 mIU/L for normal TSH levels and 0.93-1.7 ng/dL for normal FT4 levels. Based on their TSH and FT4 levels and use of medications to treat thyroid disorders, the participants were classified into one of the following categories of thyroid function: overt hyperthyroidism (low TSH, high FT4, or use of medications to treat hyperthyroidism), subclinical hyperthyroidism (low TSH, normal FT4, and no use of thyroid medication), euthyroidism (normal TSH with no use of thyroid medication), subclinical hypothyroidism (high TSH, normal FT4, and no use of thyroid medication), and overt hypothyroidism (high TSH, low FT4, or use of levothyroxine) (1717 Fedeli LG, Vidigal PG, Leite CM, Castilhos CD, Pimentel RA, Maniero VC, et al. Logistics of Collection and Transportation of Biological Samples and the Organization of the Central Laboratory in the ELSA-Brasil Rev Saude Publica. 2013;47(Suppl 2):63-71.).
Other variables
Fasting plasma glucose was measured using a hexokinase method. The study questionnaire addressed sociodemographic factors including age (as continuous and categorical [age strata] values, i.e., 35-44, 45-54, 55-64, and 65-74 years), sex, educational level (less than high school, high school and some college, or complete college or more), self-reported race/skin color (white, mixed color, black, Asian descendant, or Brazilian indigenous), smoking status (never, past, or current), alcohol use (never, past, or current), hypertension (yes or no), diabetes (yes or no), and dyslipidemia (yes or no). All participants were asked about their use of prescription and nonprescription medications within 2 weeks from their visits to the research center (1818 Chor D, Alves MG, Giatti L, Cade NV, Nunes MA, Molina Mdel C, et al. Questionnaire development in ELSA-Brasil: challenges of a multidimensional instrument. Rev Saude Publica. 2013;47(Suppl2):27-36.).
Weight was measured with the participant wearing light clothes. Body mass index (BMI) was calculated as weight divided by squared height (kg/m2). Waist circumference was measured at the midpoint between the lower edge of the last rib and the iliac crest at the midaxillary line. Blood pressure was measured after a 5-minute rest; three measurements were taken at 1-minute intervals between each measurement, and the mean of the second and third measurement was considered as the participant’s casual blood pressure level. Participants who reported the use of medication to treat hypertension or had a systolic blood pressure ≥140 mmHg or a diastolic blood pressure ≥90 mmHg were considered to have hypertension. Those participants who reported a previous medical history of diabetes mellitus or use of medication to treat this condition, presented a fasting plasma glucose ≥126 mg/dL (measured only once) or a 2-hour plasma glucose ≥200 mg/dL after 75 g of oral anhydrous glucose, or had a level of glycated hemoglobin (HbA1c) level ≥6.5% were considered to have diabetes mellitus. Dyslipidemia was defined as an LDL-cholesterol level >130 mg/dL or the use of lowering cholesterol drugs.
Statistical analysis
Categorical variables were reported as proportions and compared using the chi-square test. Continuous parametric variables were reported as means (standard deviations [SD]) and compared using analysis of variance (ANOVA), while continuous nonparametric variables were reported as medians (interquartile ranges) and compared using nonparametric tests (Mann-Whitney or Kruskal-Wallis test, as appropriate). The variable “TPOAb” was log-transformed and compared using ANOVA across all ELSA-Brasil research centers, then back-transformed to their original values. The incidence of TPOAb is expressed in percentage/year or as a cumulative incidence over the 4-year follow-up period. A logistic regression model was constructed to analyze the association between the TPOAb incidence and thyroid function (using euthyroidism as a reference), and models were presented after adjustment for age, sex, education level, and race. All analyses were performed using the Statistical Package for Social Sciences version 25.0 (IBM SPSS Statistics). A p value < 0.05 was considered significant.
RESULTS
Of the 8,922 euthyroid participants (mean age 51.1 years; 50.9% women) who presented negative TPOAb at baseline, only 130 presented incident TPOAb at follow-up, yielding an annual incidence of TPOAb of 0.38%/year (95% confidence interval [95% CI], 0.37-0.39%/year) and a cumulative incidence over 4 years of 1.46% (95% CI, 1.21-1.71%). In men, the annual incidence was 0.32% (95% CI, 0.31-0.33%), and the cumulative incidence over 4 years was 1.23% (95% CI, 0.9-1.56%). In women, the annual incidence was 0.43%/year (95% CI, 0.42-0.44%/year) and the cumulative incidence over 4 years was 1.67% (95% CI, 1.30-2.04%) (Figure 1). The women:men ratio was 1.36.
No differences in TPOAb incidence were detected across the ELSA-Brasil research centers, but the median values of incident TPOAb were higher in Belo Horizonte compared with the other centers. The median TPOAb titers per ELSA-Brasil research center, from lowest to highest, were as follows: São Paulo, 49.7 IU/mL (36.6-81 IU/mL); Rio de Janeiro, 56.5 IU/mL (37.5-110.3 IU/mL); Salvador, 57.5 IU/mL (38-90 IU/mL), Porto Alegre, 58.7 IU/mL (37.3-102.5 IU/mL); and Belo Horizonte, 77.3 IU/mL (39.7-77.3 IU/mL). Since only 2 cases of incident TPOAb were identified in Vitória, this research center was excluded from the subanalysis comparing the median values of incident TPOAb across research centers.
Table 1 describes the baseline (2008-2010) sociodemographic and clinical characteristics of the ELSA-Brasil participants according to the occurrence or not of incident TPOAb at the 4-year follow-up assessment (2012-2014). The participants with incident TPOAb were younger and more frequently women compared with the participants with no incident TPOAb, although these differences were not statistically significant (p = 0.06 for age and p = 0.08 for sex). No differences in incident TPOAb were found in relation to age strata, self-declared race, education level, or status of current smoking or alcohol intake.
General characteristics of the participants according to the occurrence or not of incident antithyroperoxidase antibodies (TPOAb) at follow-up
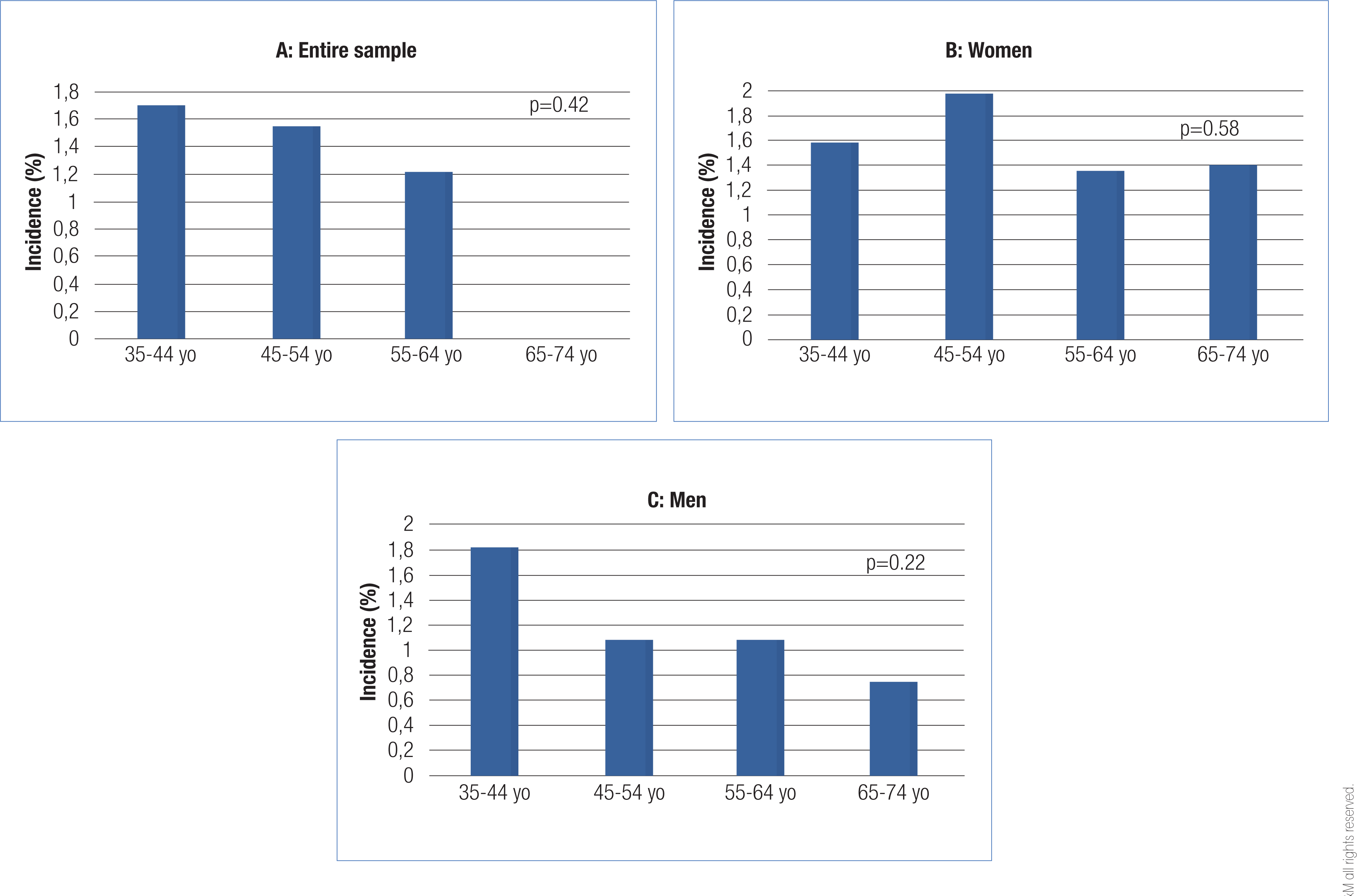
Figure 2 shows the cumulative incidence of TPOAb (percentage in a 4-year period) according to age strata and sex. There was a decline in TPOAb incidence by age strata in the entire sample and in women and men, but the differences were not statistically significant (p = 0.42, p = 0.58, and p = 0.22, respectively).
Cumulative incidence of antithyroperoxidase antibodies (TPOAb) according to age strata in: (A) Entire sample, (B) Mean and (C) Women.
The only factor associated with incident TPOAb was thyroid function at follow-up (p < 0.0001). Most incident cases occurred in participants with normal thyroid function at follow-up (88.5%), while the remaining cases were distributed according to incident thyroid diseases at follow-up as overt hyperthyroidism (1.5%), subclinical hyperthyroidism (3.1%), subclinical hypothyroidism (3.1%), and overt hypothyroidism (3.8%). In a logistic regression model adjusted by sex, age, and race and using euthyroidism as a reference, incident TPOAb was associated with overt hyperthyroidism (odds ratio [OR] 13.9; 95% CI, 3.0-64.9), subclinical hyperthyroidism (OR 8.4; 95% CI, 2.9-24.3), and overt hypothyroidism (OR 3.0; 95% CI, 1.2–7.5) but not with subclinical hypothyroidism (OR 1.0; 95% CI, 0.4-2.7).
Figure 3 shows the distribution of incident TPOAb according to the presence of thyroid diseases and age strata at follow-up for the entire sample and according to sex. All cases of overt hyperthyroidism in the entire sample (p = 0.002) and in women (p = 0.01) and men (with borderline significance, p = 0.05) are concentrated in the age strata of 35-44 years. Incident TPOAb was only associated with overt hypothyroidism in women in the younger age strata (35-44 years).
Distribution of incidence of anthyroperoxidase antibodies (TPOAb) according to thyroid function at follow-up, age strata an sex (A: Entire sample; B: Women; C: Men. (yo – years of age).
DISCUSSION
The results of the present study showed an annual incidence of TPOAb over a 4-year follow-up period that was compatible with previous studies in iodine-sufficient populations (3,5,6). The only factor associated with incident TPOAb was the presence at follow-up of thyroid dysfunction, except for subclinical hypothyroidism. The women:men ratio of incident TPOAb was 1.36. Incident TPOAb in overt hyperthyroidism was concentrated in the younger age strata in the entire sample and in women, but this observation was only borderline significant in men. Additionally, incident TPOAb was only associated with overt hypothyroidism in women in the younger age strata (35-54 years). We observed no differences in the incidence of TPOAb across ELSA-Brasil research centers, although the Belo Horizonte site had higher levels of incident TPOAb compared with the other centers (p < 0.0001). Incident TPOAb was not associated with age when analyzed as a continuous variable or with sex.
The incidence of TPOAb was defined in percentage per year or cumulative incidence over a 4-year period. Since thyroid function was only measured at baseline and at the 4-year follow-up period and no information was available about thyroid function during the 4-year interval, we opted for not presenting the results in persons-year since the time interval was around 4 years for all participants.
Although several studies have evaluated the prevalence of TPOAb, only a small number of studies have evaluated the incidence of TPOAb or other antithyroid antibodies. To the best of our knowledge, this is the first large study investigating the incidence of TPOAb in Brazil. During a 20-year follow-up in the Whickham Study, 17.3% of the women and 6.6% of the men developed incident antithyroid antibodies (antithyroglobulin, antithyroid cytoplasmic antibodies, and antimicrosomal antibodies) (1919 Vanderpump WM, Brewis M, French JM, Appleton D, Bates F, Clark J, et al. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clin Endocrinol (Oxf). 1995;43(1):55-68.). In the recent Tehran Thyroid Study, in which a sample of 2,171 men and 2,849 women with negative TPOAb at baseline was evaluated after a median follow-up of 9.1 years, there were 77 cases of incident TPOAb in men and 223 in women, corresponding to an incidence of new cases of 0.66%/year (0.39%/year in men and 0.86%/year in women) (66 Amouzegar A, Gharibzadeh S, Kazemian E, Mehran L, Tohidi M, Azizi F. The Prevalence, Incidence and Natural Course of Positive Antithyroperoxidase Antibodies in a Population-Based Study: Tehran Thyroid Study. PLoS One. 2017;12(1):e0169283.). Additionally, Li and cols. have reported a 5-year incidence of TPOAb of around 2.8% (2020 Li Y, Teng D, Shan Z, Teng X, Guan H, Yu X, et al. Antithyroperoxidase and antithyroglobulin antibodies in a five-year follow-up survey of populations with different iodine intakes. J Clin Endocrinol Metab. 2008;93(5):1751-7.). Compared with these studies, the incidences per year and over a 4-year follow-up were lower in our study (6,18). We were unable to compare our data with those from the Whickham Study since the latter measured antimicrosomal antibodies. The women:men ratio of 2.2 in a study by Amouzegar and cols. was higher than the corresponding ratio found in our sample (1.36). This finding in our study is aligned with the results from a previous Brazilian population-based study that found a prevalence of TPOAb of 10.7% in women and 9.2% in men, with a women:men ratio of 1.2. (88 Benseñor IM, Goulart AC, Lotufo PA, Menezes PR, Scazufca M. Prevalence of thyroid disorders among older people: results from the São Paulo Ageing & Health Study. Cad Saude Publica. 2011;27(1):155-61.) This type of comparison across studies is very challenging since TPOAb may have been measured using different techniques, while in older studies, other types of antibodies were tested, as in the case of the Whickham Study (2121 Tunbridge WM, Brewis M, French JM, Appleton D, Bird F, Clark DC, et al. Natural history of autoimmune thyroiditis. Br Med J (Clin Res Ed). 1981;282(6260):258-62.). Additionally, the way that incidence has been reported in each study – percentage per year, cumulative incidence over a period, or persons-year – are additional challenges for establishing direct comparisons between the studies. Other sociodemographic risk factors and environmental characteristics related to iodine and intake of other micronutrients or even genetic differences among the study populations may also interfere with incidences obtained from different populations.
We found no association between incident TPOAb and sex or age. The Wickham Study found higher levels of antithyroid antibodies (2121 Tunbridge WM, Brewis M, French JM, Appleton D, Bird F, Clark DC, et al. Natural history of autoimmune thyroiditis. Br Med J (Clin Res Ed). 1981;282(6260):258-62.) in women compared with men and an association of positive antithyroid antibodies with age in women but not in men. Data from the National Health and Nutrition Examination Survey (NHANES III) showed an increasing prevalence of TPOAb with age in both men and women (2222 Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87(2):489-99.). In the present analysis, TPOAb levels increased only 4% from the first (35-44 years) to the fourth (65-74 years) age strata (1111 Janovsky CCPS, Bittencourt MS, Goulart AC, Santos IS, Almeida-Pititto B, Lotufo PA, et al. Prevalence of antithyroperoxidase antibodies in a multiethnic Brazilian population: The ELSA-Brasil Study. Arch Endocrinol Metab. 2019;63(4):351-7.). Another possible explanation for our results is that, due to the small number of cases of incident TPOAb, the study may not have had enough power to detect differences in incidence according to age. The ELSA-Brasil cohort comprises middle-aged men and women, and most of the cohort at baseline had a mean age below 55 years, which may also help explain our results. However, our results are aligned with those of a previous population-based study in older individuals in Brazil that also showed no differences in the prevalence of TPOAb according to age and sex (88 Benseñor IM, Goulart AC, Lotufo PA, Menezes PR, Scazufca M. Prevalence of thyroid disorders among older people: results from the São Paulo Ageing & Health Study. Cad Saude Publica. 2011;27(1):155-61.). In the study by Amouzegar and cols., performed in another low- and middle-income country, incident TPOAb was concentrated among younger individuals compared with middle-aged and older participants (66 Amouzegar A, Gharibzadeh S, Kazemian E, Mehran L, Tohidi M, Azizi F. The Prevalence, Incidence and Natural Course of Positive Antithyroperoxidase Antibodies in a Population-Based Study: Tehran Thyroid Study. PLoS One. 2017;12(1):e0169283.). In China, incident TPOAb had no association with sex (1818 Chor D, Alves MG, Giatti L, Cade NV, Nunes MA, Molina Mdel C, et al. Questionnaire development in ELSA-Brasil: challenges of a multidimensional instrument. Rev Saude Publica. 2013;47(Suppl2):27-36.). These results are more similar to ours and are probably explained by a higher early mortality rate in low- and middle-income countries compared with high-income ones. It was only when we analyzed incident TPOAb in relation to overt thyroid diseases at follow-up that we found an association in the lower age strata for overt hyperthyroidism (in the entire cohort and in women, with a borderline significance in men) and for overt hypothyroidism in women. An important aspect related to thyroid diseases in the present analysis was that despite the increased frequency of incident TPOAb in women compared with men, the women:men ratio was low not only for TPOAb incidence but also for overt hyperthyroidism and hypothyroidism. In our sample, the women:men ratio for thyroid diseases was 1.36, which is in accord with a previous study in which the reported ratio was 1.2 (88 Benseñor IM, Goulart AC, Lotufo PA, Menezes PR, Scazufca M. Prevalence of thyroid disorders among older people: results from the São Paulo Ageing & Health Study. Cad Saude Publica. 2011;27(1):155-61.) but different from the ratios reported in other classical studies (1919 Vanderpump WM, Brewis M, French JM, Appleton D, Bates F, Clark J, et al. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clin Endocrinol (Oxf). 1995;43(1):55-68.,2323 Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;160:526-34.) on thyroid diseases.
Our study found no association between subclinical hypothyroidism and positive TPOAb. The most likely explanations for this observation are that the incidence of TPOAb in the sample was not high, that some imbalance could have occurred across thyroid function categories, and that this finding could have occurred by chance. The small number of individuals with positive TPOAb among the participants with subclinical hypothyroidism could explain the lack of significance of this association. Further, the short follow-up (4 years) might also explain the low numbers of incident cases.
The World Health Organization (WHO) considers Brazil to be a country with sufficient iodine intake (2424 World Health Organization (WHO). 5ᵃ ed. Geneva: WHO; 2004.). However, results of the more recent PNAISAL survey have classified Brazil as a country with a more than adequate iodine intake (2525 Universidade Federal de Pelotas; Universidade Federal do Rio Grande. Pesquisa Nacional para Avaliação do Impacto da Iodação do Sal (PNAISAL) – Relatório Técnico Final. Available from: http://189.28.128.100/dab/docs/portaldab/documentos/pnaisal_relatorio_final.pdf. Accessed in: Feb 24, 2020.
http://189.28.128.100/dab/docs/portaldab...
). A recent meta-analysis of Brazilian studies has shown heterogeneous data with most of the studies located in the South and Southeast regions and without enough information from other areas of the country where insufficient iodine intake is still possible (2626 Campos RO, Barreto IS, Maia LR, Rebouças SC, Cerqueira TS, Oliveira CA, et al. Iodine nutritional status in Brazil: a meta-analysis of all studies performed in the country pinpoints to an insufficient evaluation and heterogeneity. Arch Endocrinol Metab. 2015;59(1):13-22.). Our previous analysis about the prevalence of TPOAb using data from the ELSA-Brasil cohort has reported a higher prevalence of TPOAb in Belo Horizonte. In this present analysis of incidence, we found no differences across ELSA-Brasil research centers (1111 Janovsky CCPS, Bittencourt MS, Goulart AC, Santos IS, Almeida-Pititto B, Lotufo PA, et al. Prevalence of antithyroperoxidase antibodies in a multiethnic Brazilian population: The ELSA-Brasil Study. Arch Endocrinol Metab. 2019;63(4):351-7.). Excessive iodine intake is associated with thyroid autoimmunity (11 Sgarbi JA, Maciel RMB. Pathogenesis of autoimmune thyroid diseases. Arq Bras Endocrinol Metabol. 2009;53(1):5-14.
2 Chiovato L, Lapi P, Fiore E, Tonacchera M, Pinchera A. Thyroid autoimmunity and female gender. J Endocrinol Invest. 1993;16(5):384-91.-33 Amouzegar A, Ghaemmaghami Z, Beigy M, Gharibzadeh S, Mehran L, Tohidi M, et al. Natural Course of Euthyroidism and Clues for Early Diagnosis of Thyroid Dysfunction: Tehran Thyroid Study. Thyroid. 2017;27(5):616-25.) and a likely effect on TPOAb levels, but such an effect was not observed in our sample. However, considering the results of the PNAISAL survey, increase in TPOAb titers in samples from Brazil is possible in the near future.
We found no association of incident TPOAb and self-declared race in our sample. Some studies have suggested that Hashimoto’s thyroiditis is associated with white race (99 Sichieri R, Baima J, Marante T, de Vasconcellos MT, Moura AS, Vaisman M. Low prevalence of hypothyroidism among black and Mulatto people in a population-based study of Brazilian women. Clin Endocrinol (Oxf). 2007;66(6):803-7.,2727 McLeod DS, Caturegli P, Cooper DS, Matos PG, Hutfless S. Variation in rates of autoimmune thyroid disease by race/ethnicity in US military personnel. JAMA. 2014;311(15):1563-5.) and that Graves’ disease is associated with black race (2727 McLeod DS, Caturegli P, Cooper DS, Matos PG, Hutfless S. Variation in rates of autoimmune thyroid disease by race/ethnicity in US military personnel. JAMA. 2014;311(15):1563-5.,2828 McLeod DS, Cooper DS, Ladenson PW, Whiteman DC, Jordan SJ. Race/Ethnicity and the prevalence of thyrotoxicosis in young Americans. Thyroid. 2015;25(6):621-8.) In the present analysis, we found no association between race and incident TPOAb. Although smoking is associated with decreased TPOAb levels (2929 Zhang Y, Shi L, Zhang Q, Peng N, Chen L, Lian X, et al. The association between cigarette smoking and serum thyroid stimulating hormone, thyroid peroxidase antibodies and thyroglobulin antibodies levels in Chinese residents: A cross-sectional study in 10 cities. PLoS One. 2019;14(11): e0225435.,3030 Jia M, Shi X, Gu X, Guan H, Teng X, Teng D, et al. Smoking is positively associated with antithyroperoxidase antibodies and antithyroglobulin antibodies in populations with mildly deficient iodine intake. Biol Trace Elem Res. 2019;187(2):383-91.), we found no association between smoking status and incident TPOAb in our sample. The small prevalence of current smoking in our sample may have influenced this result.
The present study has some strengths. The ELSA-Brasil is a multicenter cohort study in which repeated measurements of thyroid function allowed for a prospective analysis. The data were collected under strict quality control, and serum TSH, FT4, and TPOAb levels were measured using the same kits at both timepoints. The cohort includes a sample of apparently healthy individuals, and the blood samples were only taken if the participants had no clinical symptoms during their visits to the research center. In the presence of symptoms (e.g., fever), the blood collection was postponed. The study also has some limitations. Levels of thyroid hormones and TPOAb were only measured once in both visits. Since the incidence of TPOAb was not high in our sample, some imbalance across thyroid function categories was possible and caused by chance. This is the case of the absence of association of TPOAb and subclinical hypothyroidism, which may be explained by the low number of individuals with incident TPOAb among participants with subclinical hypothyroidism. The median follow-up of around 4 years was short, and there were only a small number of incident cases in the sample. Also, we have no information about antithyroglobulin antibodies – which is a relevant marker of iodine intake and may be related to TSH levels and Hashimoto’s thyroiditis – or about genetic variants at this moment of the study, which limits our ability to evaluate the risk factors associated with autoimmune thyroid diseases. Lastly, the study included only individuals aged 35-74 years.
In conclusion, our findings on incident TPOAb are aligned with those of a country with sufficient iodine intake. Still, monitoring the incidence of TPOAb over the next few years will be fundamental since the changes in iodine intake in Brazil – from “sufficient” to “more than adequate” – may have an effect on thyroid autoimmunity and TPOAb levels in the country in the near future.
-
Funding: the ELSA-Brasil baseline study and the 4-year follow-up were supported by the Brazilian Ministry of Health (Science and Technology Department) and the Brazilian Ministry of Science and Technology (Financiadora de Estudos e Projetos and CNPq National Research Council) (grants for the baseline study: 01 06 0010.00 RS, 01 06 0212.00 BA, 01 06 0300.00 ES, 01 06 0278.00 MG, 01 06 0115.00 SP, 01 06 0071.00 RJ; grants for the 4-year follow-up study: 01 10 0643-03 RS, 01 10 0742-00 BA, 01 12 0284-00 ES, 01 10 0746-00 MG, 01 10 0773-00 SP, 01 11 0093-01 RJ; grants for the follow-up study: 01 10 0643-03 RS; 01 10 0742-00 BA; 01 11 0093-01 RJ; 01 12 0284-00 ES; 01 10 0746-00 MG; 01 10 0773-00 SP). Fapesp – Fundação de Amparo à Pesquisa do Estado de São Paulo – 2015/17213-2
Acknowledgments:
the authors would like to thank the staff and the participants of the ELSA-Brasil Study for their important contributions.
REFERENCES
-
1Sgarbi JA, Maciel RMB. Pathogenesis of autoimmune thyroid diseases. Arq Bras Endocrinol Metabol. 2009;53(1):5-14.
-
2Chiovato L, Lapi P, Fiore E, Tonacchera M, Pinchera A. Thyroid autoimmunity and female gender. J Endocrinol Invest. 1993;16(5):384-91.
-
3Amouzegar A, Ghaemmaghami Z, Beigy M, Gharibzadeh S, Mehran L, Tohidi M, et al. Natural Course of Euthyroidism and Clues for Early Diagnosis of Thyroid Dysfunction: Tehran Thyroid Study. Thyroid. 2017;27(5):616-25.
-
4Hoogendoorn EH, Hermus AR, de Vegt F, Ross HA, Verbeek ALM, Kiemeney LALM, et al. Thyroid function and prevalence of anti-thyroperoxidase antibodies in a population with borderline sufficient iodine intake: influences of age and sex. Clin Chemistry. 2006;52(1):104-11.
-
5Bjoro T, Holmen J, Kruger O, Midthjell K, Hunstad K, Schreiner T, et al. Prevalence of thyroid disease, thyroid dysfunction and thyroid peroxidase antibodies in a large, unselected population. The Health Study of Nord-Trondelag (HUNT). Eur J Endocrinol. 2000;143(5):639-47.
-
6Amouzegar A, Gharibzadeh S, Kazemian E, Mehran L, Tohidi M, Azizi F. The Prevalence, Incidence and Natural Course of Positive Antithyroperoxidase Antibodies in a Population-Based Study: Tehran Thyroid Study. PLoS One. 2017;12(1):e0169283.
-
7Olmos RD, Figueiredo RC, Aquino EM, Lotufo PA, Bensenor IM. Gender, race and socioeconomic influence on diagnosis and treatment of thyroid disorders in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Braz J Med Biol Res. 2015;48(8):751-8.
-
8Benseñor IM, Goulart AC, Lotufo PA, Menezes PR, Scazufca M. Prevalence of thyroid disorders among older people: results from the São Paulo Ageing & Health Study. Cad Saude Publica. 2011;27(1):155-61.
-
9Sichieri R, Baima J, Marante T, de Vasconcellos MT, Moura AS, Vaisman M. Low prevalence of hypothyroidism among black and Mulatto people in a population-based study of Brazilian women. Clin Endocrinol (Oxf). 2007;66(6):803-7.
-
10Taylor PN, Albrecht D, Scholz A, Gutierrez-Buey G, Lazarus JH, Dayan CM, et al. Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol. 2018;14(5):301-6.
-
11Janovsky CCPS, Bittencourt MS, Goulart AC, Santos IS, Almeida-Pititto B, Lotufo PA, et al. Prevalence of antithyroperoxidase antibodies in a multiethnic Brazilian population: The ELSA-Brasil Study. Arch Endocrinol Metab. 2019;63(4):351-7.
-
12Aquino EML, Barreto SM, Bensenor IM, Carvalho MS, Chor D, Duncan BB, et al. Brazilian Longitudinal Study of Adult Health (ELSA-Brasil): Objectives and Design. Am J Epidemiol. 2012;175(4):315-24.
-
13Schmidt MI, Duncan BB, Mill JG, Lotufo PA, Chor D, Barreto SM, et al. Cohort Profile: Longitudinal Study of Adult Health (ELSA-Brasil). Int J Epidemiol. 2015;44(1):68-75.
-
14Benseñor IM, Griep RH, Pinto KA, Faria CP, Felisbino-Mendes M, Caetano EI, et al. Routines of organization of clinical tests and interviews in the ELSA-Brasil investigation center]. Rev Saude Publica. 2013;47 Suppl 2:37-47.
-
15Lai EC, Yang YH, Lin SJ, Hsieh CY. Use of antiepileptic drugs and risk of hypothyroidism. Pharmacoepidemiol Drug Saf. 2013;22:1071-9.
-
16Dong BJ. How medications affect thyroid function. West J Med. 2000;172:102-6.
-
17Fedeli LG, Vidigal PG, Leite CM, Castilhos CD, Pimentel RA, Maniero VC, et al. Logistics of Collection and Transportation of Biological Samples and the Organization of the Central Laboratory in the ELSA-Brasil Rev Saude Publica. 2013;47(Suppl 2):63-71.
-
18Chor D, Alves MG, Giatti L, Cade NV, Nunes MA, Molina Mdel C, et al. Questionnaire development in ELSA-Brasil: challenges of a multidimensional instrument. Rev Saude Publica. 2013;47(Suppl2):27-36.
-
19Vanderpump WM, Brewis M, French JM, Appleton D, Bates F, Clark J, et al. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clin Endocrinol (Oxf). 1995;43(1):55-68.
-
20Li Y, Teng D, Shan Z, Teng X, Guan H, Yu X, et al. Antithyroperoxidase and antithyroglobulin antibodies in a five-year follow-up survey of populations with different iodine intakes. J Clin Endocrinol Metab. 2008;93(5):1751-7.
-
21Tunbridge WM, Brewis M, French JM, Appleton D, Bird F, Clark DC, et al. Natural history of autoimmune thyroiditis. Br Med J (Clin Res Ed). 1981;282(6260):258-62.
-
22Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87(2):489-99.
-
23Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;160:526-34.
-
24World Health Organization (WHO). 5ᵃ ed. Geneva: WHO; 2004.
-
25Universidade Federal de Pelotas; Universidade Federal do Rio Grande. Pesquisa Nacional para Avaliação do Impacto da Iodação do Sal (PNAISAL) – Relatório Técnico Final. Available from: http://189.28.128.100/dab/docs/portaldab/documentos/pnaisal_relatorio_final.pdf Accessed in: Feb 24, 2020.
» http://189.28.128.100/dab/docs/portaldab/documentos/pnaisal_relatorio_final.pdf -
26Campos RO, Barreto IS, Maia LR, Rebouças SC, Cerqueira TS, Oliveira CA, et al. Iodine nutritional status in Brazil: a meta-analysis of all studies performed in the country pinpoints to an insufficient evaluation and heterogeneity. Arch Endocrinol Metab. 2015;59(1):13-22.
-
27McLeod DS, Caturegli P, Cooper DS, Matos PG, Hutfless S. Variation in rates of autoimmune thyroid disease by race/ethnicity in US military personnel. JAMA. 2014;311(15):1563-5.
-
28McLeod DS, Cooper DS, Ladenson PW, Whiteman DC, Jordan SJ. Race/Ethnicity and the prevalence of thyrotoxicosis in young Americans. Thyroid. 2015;25(6):621-8.
-
29Zhang Y, Shi L, Zhang Q, Peng N, Chen L, Lian X, et al. The association between cigarette smoking and serum thyroid stimulating hormone, thyroid peroxidase antibodies and thyroglobulin antibodies levels in Chinese residents: A cross-sectional study in 10 cities. PLoS One. 2019;14(11): e0225435.
-
30Jia M, Shi X, Gu X, Guan H, Teng X, Teng D, et al. Smoking is positively associated with antithyroperoxidase antibodies and antithyroglobulin antibodies in populations with mildly deficient iodine intake. Biol Trace Elem Res. 2019;187(2):383-91.
Publication Dates
-
Publication in this collection
22 Nov 2021 -
Date of issue
Nov-Dec 2021
History
-
Received
24 May 2021 -
Accepted
07 Sept 2021