Abstract
Background:
The score is an effective instrument for the assessment of treatment adherence in users of oral anticoagulants and maintenance of INR (international normalized ratio) within the therapeutic range.
Objective:
To develop an adherence score for oral anticoagulant users for the maintenance of INR within the therapeutic range.
Methods:
This was an analytical, observational, cross-sectional study, with a quantitative approach, conducted in a public cardiology hospital. A total of 607 patients who met the inclusion criteria were evaluated. Variables with a significance level of 5% in the exploratory analysis and considered clinically relevant were included and subjected to a multiple logistic regression model. Predictive accuracy of the model was determined using the C statistic.
Results:
The variables with a significance level of 5% in the multivariate analysis were: education, family income, inadequate use of medications, drug-drug interactions, invasive procedures, food-drug interactions, physical activity, medical conditions, other factors, and complications related to oral anticoagulant therapy. The following prognostic variables were identified: family income, inadequate use of medications, invasive procedures, drug-drug interactions, dietary habits, medical conditions, other factors (stress, thinness, weight loss). C-statistic for adherence score was 0.94.
Conclusion:
The Simonetti adherence score proved to be easily applicable and feasible, with high predictive value for influencing factors, promoting the improvement of adherence and maintenance of INR in the ideal range. (Int J Cardiovasc Sci. 2018; [online].ahead print, PP.0-0)
Keywords:
Cardiovascular Diseases; Anticoagulants/therapy; Probability; Medication Adherence; Health Education
Resumo
Fundamento:
O escore é um instrumento eficaz na avaliação da adesão de usuários de anticoagulante oral e na manutenção do RNI (razão normalizada internacional) na faixa terapêutica segundo recomendações americanas e europeias.
Objetivo:
Construir um escore de adesão aos usuários de Anticoagulante Oral para a manutenção na faixa terapêutica.
Métodos:
Estudo analítico, observacional, transversal e abordagem quantitativa, realizado em hospital público especializado em cardiologia. Foram avaliados 607 pacientes que atenderam aos critérios de inclusão. Consideram-se as variáveis que apresentaram nível de significância menor que 5% na análise exploratória ou que foram apreciadas de relevância clínica e submetidas a um modelo de regressão logística múltipla. A acurácia preditiva do modelo foi determinada pelo C statistic.
Resultados:
As variáveis com nível de significância menor que 5% na análise multivariada: escolaridade, renda familiar, uso inadequado, interação medicamentosa, procedimentos invasivos, interações alimentar, atividade física, condições clínicas, outros fatores e complicações próprias do uso do anticoagulante oral. Foram identificadas variáveis prognósticas: renda familiar, uso inadequado, procedimento invasivo, interação medicamentosa, hábitos alimentares, condições clínicas, outros fatores (estresse, emagrecimento, perda de peso). O C Statistic para o Escore de Adesão foi de 0,94.
Conclusão:
O escore de adesão Simonetti mostrou-se de aplicabilidade fácil e exequível, com alto valor preditivo mediante os fatores intervenientes, facilitando a melhoria da adesão e manutenção do RNI na faixa ideal. (Int J Cardiovasc Sci. 2018; [online].ahead print, PP.0-0)
Palavras-chave:
Doenças Cardiovasculares; Anticoagulantes/terapia; Probabilidade; Adesão à Medicação; Educação em Saúde
Introduction
Health promotion is a key strategy for prevention of thromboembolic events in patients on oral anticoagulant therapy (OAC-T) in addition to other aspects related to the assistance of this population. In this context, health professionals, nurses and physicians play the role of educators, particularly in providing clear guidance on risk factors and possible signs and symptoms and related complications associated with a OAC-T.11 Freitas D, Ribeiro K, Oliveira JL, Matos FG, Carvalho AR, Ross C, et al. Diagnósticos de enfermagem entre usuários de anticoagulante oral acompanhados em ambulatório. Rev baiana enferm.2017;31(3):e20356
Stability of OAC-T is associated with treatment adherence, in addition to other factors including age, concomitant use of other drugs, comorbidities, irregular use of vitamin K, inadequate use of the drug, and hereditary polymorphism.22 Ávila CW, Aliti GB, Feijó MKF, Rabelo ER. Adesão Farmacológica ao anticoagulante oral e os fatores que influenciam na estabilidade do índice de normatização internacional. Rev Latino-Am. Enfermagem.2011; 19(1): 1-8. Educational programs for outpatient management of patients on OAC-T have been crucial for the approach of drug and dietary interactions with coumarin derivatives, which may affect treatment adherence.22 Ávila CW, Aliti GB, Feijó MKF, Rabelo ER. Adesão Farmacológica ao anticoagulante oral e os fatores que influenciam na estabilidade do índice de normatização internacional. Rev Latino-Am. Enfermagem.2011; 19(1): 1-8.,33 Lustosa MA, Alcaires J, Costa JC. Adesão do paciente ao tratamento no hospital geral. Rev SBPH. 2011;14(2):27-49.
A study44 Simonetti SH, Mancussi e Faro AC, Bianchi ERF. Adesão à terapia com anticoagulantes orais: revisão integrativa. Rev enferm UFPE. 2014;8(8): 2854-63. pointed out important considerations about adherence to OAC-T. First, knowledge about adherence to OAC-T is still a challenge among health professionals in national and international contexts. Second, the study provides data on instruments proposed by health professionals aimed at improving patients’ adherence and knowledge about the treatment, and on patients’ sociodemographic status. The authors also reported the scarcity of studies on factors that may influence therapy adherence. Studies have so far highlighted the importance of health education as an efficient strategic intervention to improve the use of oral anticoagulants (OACs) but have not provided enough evidence on instruments to measure adherence and non-adherence. Finally, the study support the emerging need for a medication adherence scale for this population.44 Simonetti SH, Mancussi e Faro AC, Bianchi ERF. Adesão à terapia com anticoagulantes orais: revisão integrativa. Rev enferm UFPE. 2014;8(8): 2854-63.
In light of this context and current recommendations, a need for the development of a score to assess adherence and non-adherence in users of OACs has emerged.
Methods
This was an analytical, observational, cross-sectional study, with a quantitative approach, conducted at the Oral Anticoagulation Center of a public, cardiology hospital associated to the São Paulo State Secretary of Health.
For sample calculation, we considered the prevalence of altered INR (international normalized ratio), i.e., 5% among patients without other conditions that may affect this parameter; 15% among patients with conditions that may affect this parameter, additionally to an alpha of 5% and power of 95%. Therefore, inclusion of 5 and 2 patients with and without factors known to affect INR, respectively, was considered, resulting in a sample size of 574. An additional 5% was considered for possible dropouts, yielding a sample of 607 patients on OAC-T that met eligibility criteria. Altered INR was used as outcome measure and the following predicting variables were assessed: drug handling, drug-drug and drug-food interactions, surgeries and other procedures, clinical condition, health problems, among other factors - stress, weight loss / gain, use of (generic or similar) warfarin, alcohol abuse and physical activity.
Data collection was performed in two stages - in phase I, general features of the sample were collected, and in phase II, clinical characteristics were collected. All patients signed an informed consent form before being included in the study. The study was approved by local ethics committee (approval number 4420; CAAE: 24118513.7.0000.5392).
Statistical analysis
Qualitative variables were expressed as absolute and relative frequency, and quantitative variables as mean and standard deviation. The chi-square test and Fisher’s exact test were used to assess associations between qualitative variables. Variables with p < 0.10 and/or with clinical significance for adherence and INR within recommended therapeutic range were analyzed by a multiple logistic regression model, followed by a stepwise backward analysis for the final model. C-statistic was calculated by the ROC (receiver operating characteristic) curve to evaluate the final model and final score. Significance level was set at 5%. Analysis was performed using the Statistical Package for Social Sciences (SPSS) version 19 (Armonk, NY: IBM Corp.) and the R Core Team 2016 software.
Results
Clinical profile of users of OACs
A total of 607 patients on OAC-T participated in the study. Fifty-two percent of patients were women, 57% married, 56% older than 60 years, 42% had some elementary school, in 55% the family income was between 1 and 3 minimum wage, and almost all of them (93%) came from Sao Paulo. Sociodemographic characteristics are described in Table 1.
Normal INR levels used as reference were: < 2 and > 3 for patients with thromboembolic events, and < 2.5 and > 3.5 for patients with mechanical prosthesis. Forty percent of patients (n = 247) had altered INR, whereas 60% (n = 360) had normal INR.
Most INR results were within the range from 2 to 3, whereas 119 participants (36%) with mechanical prosthesis had an INR < 2.5 and > 3.5. In addition, the presence of atrial fibrillation and/or atrial flutter was considered for patients with mechanical prosthesis. Most patients on OAC-T with INR < 2.0 were those with atrial fibrillation (n = 105, 54%) (Table 1).
For patients with INR > 2 (conditions with risk for thromboembolic events) and/or > 2.5 (mechanical prosthesis), atrial fibrillation was the most frequent disease and mechanical prosthesis was the main valvular prosthesis - mitral valve (n = 58; 26%) and aortic valve (n = 41; 18%).
With respect to participants’ diseases and indication for OAC, 30 types of heart diseases were identified, 51% (783) clinical conditions and 24% (360) of surgical type, as well as related comorbidities (364; 25%).
Multiple logistic regression model
The following variables were selected for the multiple logistic regression model: family income, educational attainment, inadequate doses, invasive procedures, drug interactions, eating habits, physical activity, health problems, OAC-related complications, among other factors (Table 2).
Since all predictive variables showed a significative response, seven logistic regression models were considered for analysis at first. However, the model adopted in the study included the variables described in Table 2, considering also the interactions between them.
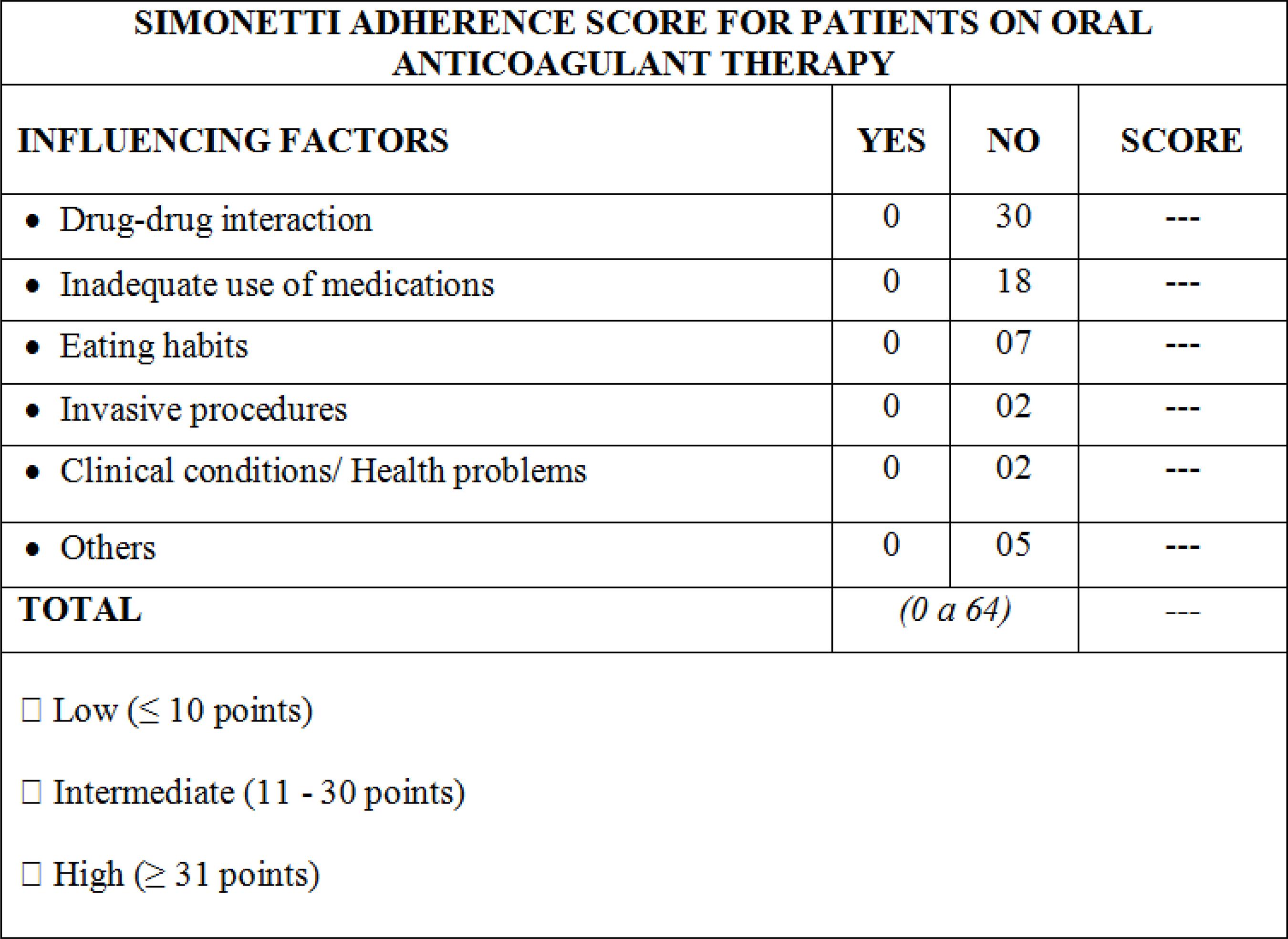
Simonetti medication adherence score
The variables used in the scores are shown in Table 3. First, the percentage of adherence was determined by Simonneti SH by multiplying the number of positive variables for adherence by the total number of predictive variables. A score was also developed to determine whether INR was within the normal range (Figure 1). The score was calculated by odds ratio.
Then, each condition known to affect INR was categorized into high (≤ 10 points), intermediate (11 - 30 points) and high (≥ 31 points) for normal INR (Figure 2).
The area under the ROC curve was determined based on the results of the variables proposed in the present study (Figure 3). For the logistic model, C-statistic was 0.940 (95% CI = 0.920 - 0.960; p < 0.001), indicating a satisfactory performance in detecting the occurrence of an event.
Areas under the ROC (Receiver Operating Characteristic) curves for medication adherence by the Simonetti score.
Discussion
The optimal dose of OAC is variable between individuals and should be adjusted to ensure that INR is maintained within the therapeutic range. In addition, it is known that the patient may reduce, discontinue (e.g. bleeding) or increase (e.g. double dose to make up for a missed dose) the dose of OAC.55 Crowther M, Crowther MA. Intensity of Warfarin Coagulation in the Antiphoslipid Syndrome. Curr Rheumatol Rep. 2010;12(1):64-9.
OAC-T-related complications may also be associated with the use of Marevan®, due to underdosing (risk of thrombus formation) or overdosing (bleeding), and the seek for medical care due to gum bleeding, hematuria, and other complications.66 Pelegrino FM, Bolela F, Corbi ISA, Carvalho ARS, Dantas RAS. Protocolo educativo para pacientes em uso de anticoagulante oral: construção e validação. Texto Contexto Enferm. 2014;23(3):799-806.
Therefore, the lack of appropriate instructions and recommendations for patients on OAC-T in the perioperative period of any clinical or surgical procedure may cause variability in routine practice and affect the maintenance of INR within therapeutic range. Nevertheless, evidence shows that changes in OAC-T are not required prior to tooth extraction for example, providing that INR is maintained between 2 and 4, and bleeding control measures are implemented in the perioperative period to prevent embolic events.77 Antonio N, Castro G, Ramos D, Machado A, Gonçalves L, Macedo T,et al. Controvérsias na anticoagulação oral: continuar ou interromper os anticoagulantes orais durante a Intervenção estomatológica? Rev Port Cardiol. 2008;27(4):531-44.
Studies have suggested that patients on OAC-T may require parenteral anticoagulation in the perioperative period. The decision to discontinue anticoagulation and start an antithrombotic therapy is determined by the risk of bleeding, surgical treatment to which patients were submitted and the risk for thrombosis due to underlying diseases.88 Fernandes EO, Guerra EE, Pitrez FAB, Fernandes FM, Rosito GBA, Gonzáles HE, et al. Avaliação pré-operatório e cuidado em cirurgia eletiva: recomendações baseadas em evidências. Rev AMRIGS.2010;54(2):240-58. However, for patients at low risk of bleeding (skin biopsies, cataract or dental procedures), the use of OAC may be continued, providing that INR is maintained at lower values and control of local bleeding is successfully achieved.88 Fernandes EO, Guerra EE, Pitrez FAB, Fernandes FM, Rosito GBA, Gonzáles HE, et al. Avaliação pré-operatório e cuidado em cirurgia eletiva: recomendações baseadas em evidências. Rev AMRIGS.2010;54(2):240-58.
Due to the risk of bleeding, when management of patients on OAC-T includes major surgery, it is recommended88 Fernandes EO, Guerra EE, Pitrez FAB, Fernandes FM, Rosito GBA, Gonzáles HE, et al. Avaliação pré-operatório e cuidado em cirurgia eletiva: recomendações baseadas em evidências. Rev AMRIGS.2010;54(2):240-58. that these individuals are classified into patients at minimal risk (atrial fibrillation without history of venous thromboembolism), intermediate risk or high risk of thromboembolism.
In addition, one of the main factors that affect INR and treatment adherence is drug-drug interactions. Antonio et al.77 Antonio N, Castro G, Ramos D, Machado A, Gonçalves L, Macedo T,et al. Controvérsias na anticoagulação oral: continuar ou interromper os anticoagulantes orais durante a Intervenção estomatológica? Rev Port Cardiol. 2008;27(4):531-44. described the main drugs that interact with and potentiate the effect of OACs - allopurinol, amiodarone, cimetidine, cisapride, clofibrate and other fibrates, chloramphenicol, cotrimoxazole, erythromycin, fluconazole, isoniazid, metronidazole, miconazole, omeprazole, phenylbutazone, piroxicam, propafenone, propranolol, salicylate, phenylbutazone. These drugs may increase INR and cause bleeding. However, some drugs may inhibit the effects of OAC, including barbiturates, carbamazepine, chlordiazepoxide, cholestyramine, griseofulvin, nafcillin, rifampicin, sucralfate and trazodone. These drugs may decrease INR results, and hence, increase the risk for thromboembolic events.77 Antonio N, Castro G, Ramos D, Machado A, Gonçalves L, Macedo T,et al. Controvérsias na anticoagulação oral: continuar ou interromper os anticoagulantes orais durante a Intervenção estomatológica? Rev Port Cardiol. 2008;27(4):531-44.
Drug interactions related to OAC-T are of more or less importance, and are associated with processes that involve many pharmacodynamic and pharmacokinetic mechanisms - altered platelet function (clopidogrel, salicylic acid), gastrointestinal lesion (nonsteroidal anti-inflammatory drugs), impaired vitamin K synthesis in the gastrointestinal tract (antibiotics - amoxicillin, ampicillin, cephalosporin, metronidazole, clarithromycin, norfloxacin and trimethoprim/sulfamethoxazole), impaired warfarin metabolism (amiodarone, rifampicin, simvastatin, gemfibrozil), and impaired vitamin K metabolism (acetaminophen).99 Silva PM. Velhos e novos anticoagulantes orais. Perspectiva farmacológica. Rev Port Cardiol. 2012;31(Supl 1):6-16. In general, drug interactions reduce the therapeutic effects of OACs and increase the risk for clotting or potentiate such effects and increase the risk of bleeding.
Some factors, however, should be considered99 Silva PM. Velhos e novos anticoagulantes orais. Perspectiva farmacológica. Rev Port Cardiol. 2012;31(Supl 1):6-16. when the effects of OACs are decreased, such as inhibition of warfarin absorption by cholestyramine or by foods in the gastrointestinal tract; increased distribution volume and half-life reduction due to hypoproteinemia; increased metabolism caused by stimulation of CYP2C9 by other drugs (barbiturates); excess intake of vitamin K-rich foods. On the other hand, CYP2C9 inhibition by other drugs (fluoxetine, amiodarone, clopidogrel), protein binding displacement caused by diuretics and sodium valproate, as well as vitamin K deficiency may reduce vitamin K metabolism, and consequently increase its effect.1010 Rohrbacher I, Brum EP. Knowledge of warfarin users about their own treatment. Rev AMRIGS. 2013;57:285-9.
Amiodarone and simvastatin were the main drugs that significantly affected the required dose of OACs. Amiodarone is an antiarrhythmic that inhibits warfarin, due to its role as a potent cytochrome P450 inhibitor including CYP2C9, which is involved in S-warfarin metabolism.1010 Rohrbacher I, Brum EP. Knowledge of warfarin users about their own treatment. Rev AMRIGS. 2013;57:285-9. Amiodarone inhibits warfarin metabolism and increases its effect, and the concomitant use of both drugs also affects prothrombin time. Simvastatin potentiates the effect of warfarin by binding to plasma proteins, reduces platelet aggregation and promotes thrombus formation.1111 Krummenacher R, Lukas PS, Demarmels Biasiutti F, Begré S, Znoj H, Von Känel R. Relationship between psychological distress and endogenous anticoagulants in patients with a previous venous thromboembolic event. Clin Appl Thromb Hemost. 2011;17(2):171-80.
Besides, it is essential that patients on OAC-T are aware of the consumption of vitamin K-rich foods. Variations in the amount or in the frequency of consumption of these foods may change INR to values outside the therapeutic range.1010 Rohrbacher I, Brum EP. Knowledge of warfarin users about their own treatment. Rev AMRIGS. 2013;57:285-9.
In case of acute alcohol consumption, dehydrogenase pathway plays a key role in ethanol metabolism in the liver. Nevertheless, in case of chronic consumption, the microsomal ethanol oxidizing system, which requires the CYP2E1 enzyme, is used and increases ethanol metabolism by ten-fold.1010 Rohrbacher I, Brum EP. Knowledge of warfarin users about their own treatment. Rev AMRIGS. 2013;57:285-9. Therefore, in the pharmacokinetics of warfarin, there is an interaction between ethanol and the drug - in case of acute ethanol consumption, warfarin metabolism is decreased by enzymatic inhibition, resulting in increased OAC effect and increased risk of bleeding.1010 Rohrbacher I, Brum EP. Knowledge of warfarin users about their own treatment. Rev AMRIGS. 2013;57:285-9. In chronic alcohol consumption, enzymatic activity decreases, with consequent increase of warfarin metabolism, reduction of its half-life and pharmacological effect. In this case, a higher dose of warfarin is recommended to reach the therapeutic range.1010 Rohrbacher I, Brum EP. Knowledge of warfarin users about their own treatment. Rev AMRIGS. 2013;57:285-9.
In addition, psychological distress has been associated with a prothrombotic state. In patients with diagnosis of thromboembolism, decreased INR was associated with psychological distress, anger, depression and anxiety.1111 Krummenacher R, Lukas PS, Demarmels Biasiutti F, Begré S, Znoj H, Von Känel R. Relationship between psychological distress and endogenous anticoagulants in patients with a previous venous thromboembolic event. Clin Appl Thromb Hemost. 2011;17(2):171-80.,1212 Oldgren J, Wallentin L, Alexander JH, James S, Jönelid B, Steg G, et al. New oral anticoagulants in addition to single or dual antiplatelet therapy after an acute coronary syndrome: a systematic review and meta-analysis. Eur Heart J.2013; 34(22):1670-80.
To minimize the risk of OAC-related complications, such as bleeding and thromboembolic events, the emergence of specialized clinics for the management of patients on OAC-T has become a common scenario worldwide. Besides, health professionals including pharmacists, nurses and physicians are responsible for implementing educational programs with oral and written instructions, videos, home visits, telephone follow-up and quality control indicators.66 Pelegrino FM, Bolela F, Corbi ISA, Carvalho ARS, Dantas RAS. Protocolo educativo para pacientes em uso de anticoagulante oral: construção e validação. Texto Contexto Enferm. 2014;23(3):799-806.
In this perspective, predisposing factors related to oral anticoagulant therapy as continuous use in treatment of thromboembolic diseases and cardiac valvar prosthesis have to be studied. Mundial recommendations are relevant and published by of the American Heart Association1313 January CT, Wann S, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, et al. 2014 AHA/ACC/HRS Guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Assosciation Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1-76. and European Society of Cardiology.1414 Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J (London).2016;37(38):2893-962.
Considering this assumption and the necessity to develop a medication adherence score for users of OACs, we adopted a complex, well-articulated and decisive methodological approach. This included the selection of predictive variables based on the clinical practice and also on researcher’s opinion, determined by practice-based evidence and current science.
Variables with statistical significance lower than 5% were selected for multiple logistic regression analysis, with adjustment for determinant factors and covariables of adherence. Variables related to adherence were then independently determined.
For adherence score development, variables known to affect INR were considered, including inadequate use of medication (higher or lower doses, missing doses), history of invasive or surgical procedures, drug-drug interaction, nutrient-drug interaction (particularly vitamin K), health problems or clinical conditions, other related factors such as considerable psychological distress, weight gain or loss and OAC-related complications. Thus, the score was developed using the variables of several models, classified and compared based on descriptive analysis of the independent variables, as well as interaction tests.
Then, a score model for a Brazilian population of patients in OAC-T was developed (Table 3); this was a simple instrument, easily applicable in the clinical setting of OAC-T. Results of the score were presented as odds ratio and respective 95% confidence interval and descriptive analysis.
The tests revealed the independent nature of the variables and the impartiality of the event occurrence. Therefore, a score that attributed the same weight for the variables was developed.
The proportion of the occurrence of an event will then be calculated by the number of positive variables for adherence and the number of predictive variables established in the model.
Simonetti adherence score had a c-statistic of 0.94, indicating satisfactory performance and applicability. Therefore, the score proposed in the present study will contribute to a more accurate evaluation and decision-making process. However, a long-term evaluation of the instrument should be performed in the clinical setting, like any stratification model, in order to evaluate the occurrence of new variables that may affect adherence.
Some limitations of the study should be considered. First, since the study was conducted in only one center, the model may not be reproducible in other settings. Second, since the score was not applied in an independent population for external validation, the performance of the instrument may not be satisfactory. It is worth pointing out, however, that our next step is to validate the instrument in another group of patients on OAC-T.
Despite these limitations, we successfully developed a medication adherence score using a model with good statistical performance. We believe that the score is of public interest and can contribute to the improvement of oral anticoagulation centers.
This study aimed to ensure and improve the provision of nursing services to patients on OAC-T in a specialized center, using a specific protocol. Although this characterized a limitation of the study, this would encourage different centers to revise their own protocols and to be informed of how treatment is being performed in other centers.
The proposed model of medication adherence score is in conformity with the significant and independent variables identified in the study. This ensures its accessibility and applicability. Using adequate statistical methods, we developed the Simonetti adherence score, and confirmed the hypothesis of this study.
Conclusion
The medication adherence score here proposed for patients on OAC-T was shown to be an easy-to-use instrument, with high predictive value and good performance. We successfully developed an instrument aimed at measuring and improving adherence of patients to OAC-T by means of the proposed methods and results obtained, confirming the hypothesis of the study.
This instrument will help professionals in accurately dealing with and hence improving adherence of patients to OAC-T and consequently improve the quality of life of this population.
-
Sources of FundingThere were no external funding sources for this study.
-
Study AssociationThis article is part of the thesis of Doctoral submitted by Sérgio Henrique Simonetti, from USP Nursing School.
-
Ethics approval and consent to participateThis study was approved by the Ethics Committee of the Instituto Dante Pazzanese de Cardiologia do Estado de São Paulo under the protocol number 4420 e CAAE: 24118513.7.0000.5392. All the procedures in this study were in accordance with the 1975 Helsinki Declaration, updated in 2013. Informed consent was obtained from all participants included in the study.
References
-
1Freitas D, Ribeiro K, Oliveira JL, Matos FG, Carvalho AR, Ross C, et al. Diagnósticos de enfermagem entre usuários de anticoagulante oral acompanhados em ambulatório. Rev baiana enferm.2017;31(3):e20356
-
2Ávila CW, Aliti GB, Feijó MKF, Rabelo ER. Adesão Farmacológica ao anticoagulante oral e os fatores que influenciam na estabilidade do índice de normatização internacional. Rev Latino-Am. Enfermagem.2011; 19(1): 1-8.
-
3Lustosa MA, Alcaires J, Costa JC. Adesão do paciente ao tratamento no hospital geral. Rev SBPH. 2011;14(2):27-49.
-
4Simonetti SH, Mancussi e Faro AC, Bianchi ERF. Adesão à terapia com anticoagulantes orais: revisão integrativa. Rev enferm UFPE. 2014;8(8): 2854-63.
-
5Crowther M, Crowther MA. Intensity of Warfarin Coagulation in the Antiphoslipid Syndrome. Curr Rheumatol Rep. 2010;12(1):64-9.
-
6Pelegrino FM, Bolela F, Corbi ISA, Carvalho ARS, Dantas RAS. Protocolo educativo para pacientes em uso de anticoagulante oral: construção e validação. Texto Contexto Enferm. 2014;23(3):799-806.
-
7Antonio N, Castro G, Ramos D, Machado A, Gonçalves L, Macedo T,et al. Controvérsias na anticoagulação oral: continuar ou interromper os anticoagulantes orais durante a Intervenção estomatológica? Rev Port Cardiol. 2008;27(4):531-44.
-
8Fernandes EO, Guerra EE, Pitrez FAB, Fernandes FM, Rosito GBA, Gonzáles HE, et al. Avaliação pré-operatório e cuidado em cirurgia eletiva: recomendações baseadas em evidências. Rev AMRIGS.2010;54(2):240-58.
-
9Silva PM. Velhos e novos anticoagulantes orais. Perspectiva farmacológica. Rev Port Cardiol. 2012;31(Supl 1):6-16.
-
10Rohrbacher I, Brum EP. Knowledge of warfarin users about their own treatment. Rev AMRIGS. 2013;57:285-9.
-
11Krummenacher R, Lukas PS, Demarmels Biasiutti F, Begré S, Znoj H, Von Känel R. Relationship between psychological distress and endogenous anticoagulants in patients with a previous venous thromboembolic event. Clin Appl Thromb Hemost. 2011;17(2):171-80.
-
12Oldgren J, Wallentin L, Alexander JH, James S, Jönelid B, Steg G, et al. New oral anticoagulants in addition to single or dual antiplatelet therapy after an acute coronary syndrome: a systematic review and meta-analysis. Eur Heart J.2013; 34(22):1670-80.
-
13January CT, Wann S, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, et al. 2014 AHA/ACC/HRS Guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Assosciation Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1-76.
-
14Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J (London).2016;37(38):2893-962.
Publication Dates
-
Publication in this collection
11 June 2018 -
Date of issue
Jul-Aug 2018
History
-
Received
05 June 2017 -
Reviewed
21 Dec 2017 -
Accepted
15 Jan 2018