ABSTRACT
BACKGROUND AND OBJECTIVES:
Walking is described as one of the abilities most affected by chronic low back pain. This study aimed to determine if chronic nonspecific low back pain and walking speed affect the spatiotemporal parameters (stride length, swing time, contact time, stride time, stride frequency and walking ratio) and the coefficients of variation of stride length and contact time.
METHODS:
Ten participants with chronic nonspecific low back pain (low back pain - LG) and ten healthy participants in the control group (CG) walked on the treadmill at preferred self-selected speed, slower and faster than the preferred speed. Spatiotemporal parameters and coefficients of variation were determined by kinematic analysis. Main effects (group and speed) and their interactions were tested using generalized estimating equations method.
RESULTS:
Our results showed that there were no significant differences between groups or significant interaction between group and speed factors. There was a speed effect. Stride frequency and length increased while contact and stride time decreased as the speed increased. The walking ratio (stride length/stride frequency) was relatively consistent across speeds (~1.6 m·stride-1.s) without statistical differences. The coefficients of variation were below 5%.
CONCLUSION:
The chronic nonspecific low back pain did not affect the gait spatiotemporal profile, at least for those patients classified as chronic nonspecific low back pain according to the signs and symptoms criteria. Although the preferred speed has affected the spatiotemporal parameters, both groups patients were able to adjust their kinematic parameters to each task demand.
Keywords:
Gait; Biomechanical phenomena; Locomotion; Spine
RESUMO
JUSTIFICATIVA E OBJETIVOS:
A caminhada é descrita como uma das habilidades mais afetadas pela dor lombar crônica. Este estudo objetivou determinar se a dor lombar crônica não específica e a velocidade de caminhada afetam os parâmetros espaço-temporais (comprimento da passada, tempo de balanço, tempo de contato, tempo da passada, frequência da passada e razão de caminhada) e os coeficientes de variação do comprimento da passada e do tempo de contato.
MÉTODOS:
Dez participantes com dor lombar crônica não específica (grupo dor lombar GL) e 10 participantes saudáveis (grupo controle - GC) caminharam na esteira na velocidade preferida autosselecionada, e em velocidades mais lenta e mais rápida que a velocidade preferida. Parâmetros espaço-temporais e coeficientes de variação foram determinados por cinemetria. Os efeitos principais (grupo e velocidade) e as suas interações foram testadas pelo método de equações de Estimativas Generalizadas.
RESULTADOS:
Não houve diferenças entre os grupos ou interação entre os fatores (grupo e velocidade). Houve efeito da velocidade. A frequência e o comprimento de passada aumentaram, enquanto o tempo de contato e de passada diminuíram à medida que a velocidade aumentou. A razão de caminhada (comprimento da passada/frequência da passada) foi relativamente consistente entre as velocidades (~1,6 m·passada-1·s) sem diferenças estatísticas. Os coeficientes de variação ficaram abaixo dos 5%.
CONCLUSÃO:
A dor lombar crônica não específica não afetou os parâmetros espaço-temporais da caminhada, pelo menos para os pacientes classificados com dor lombar crônica não específica pelos critérios de sinais e sintomas. Embora a velocidade preferida tenha afetado os parâmetros espaço-temporais, os pacientes de ambos os grupos foram hábeis para ajustar seus parâmetros cinemáticos às demandas da tarefa.
Descritores:
Coluna vertebral; Fenômenos biomecânicos; Locomoção; Marcha
INTRODUCTION
Low back pain (LBP) is a syndrome-based condition with high prevalence in the world population. The global prevalence of LBP was reported as ranging from 5 to 65%11 Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8-20.. In Brazil, the prevalence of chronic low back pain (CLBP) is 3.9 to 25.4%, and the prevalence in individuals aged between 20 and 59 years is around 19,6%22 Meucci RD, Fassa AG, Faria NM. Prevalence of chronic low back pain: systematic review. Rev Saude Publica. 2015;49. pii: S0034-89102015000100408.. Although the specific causes of LBP can be identified, the specific diagnosis is not possible in most cases, and a nonspecific cause is frequently accepted as the diagnosis33 Negrini S, Fusco C, Atanasio S, Romano M, Zaina F. Low back pain: state of art. Eur J Pain Suppl. 2008;2(Supp 1):52-6..
The recognition of the LBP etiology remains a challenge since there is still a poor correlation between anatomopathological and clinical presentation44 Welch E. Low back pain. InnovAiT. 2012;5(1):13-21.. Nevertheless, CLBP is usually associated with functional and psychosocial impairment55 Bertor WRR, Fracaro GA, Silva LI, Zílio M, Aragão FA, Carvalho AR. Subclassificação da lombalgia crônica e nível de incapacidade: efeito no desempenho funcional e força muscular. Conscientiae Saúde. 2013;12(4):563-71.,66 Fracaro GA, Bertor WR, Silva LI, Brandl L, Zanini GM, Zílio M, et al. Comparison of psycho-social and functional performance variables in a group of chronic low back pain patients. Rev Dor. 2013;14(2):119-23.. A study that identified the main activities performed with difficulty in patients with CLBP pointed out more than 60 types of activities. However, the most prevalent, around 56%, was a decrease in walking tolerance77 Andrew Walsh D, Jane Kelly S, Sebastian Johnson P, Rajkumar S, Bennetts K. Performance problems of patients with chronic low-back pain and the measurement of patient-centered outcome. Spine. 2004;29(1):87-93..
Walking is an activity of both clinical and functional relevance due to its impact on independence and quality of life, and is often an integral part of rehabilitation programs, including those directed to patients with CLBP. However, the repercussion of LBP on the walking parameters still needs further understanding, given the etiological complexity of this syndrome and the wide range of factors that can contribute to the loss of movement88 Simmonds MJ, Lee CE, Etnyre BR, Morris GS. The influence of pain distribution on walking velocity and horizontal ground reaction forces in patients with low back pain. Pain Res Treat. 2012;2012:214980..
Spatiotemporal parameters of gait, such as speed, stride length, stride frequency, contact, and balance time, are not unvarying. They interact in a coordinated manner to allow the displacement to be adequate to the task demands and environment and to ensure that it is performed effectively. Therefore, individuals tend to determine these spatiotemporal parameters freely, although dynamic and mechanical factors have a remarkable influence on this choice99 Saibene F, Minetti AE. Biomechanical and physiological aspects of legged locomotion in humans. Eur J Appl Physiol. 2003;88(4-5):297-316..
Some neurological diseases cause disturbance of gait spatiotemporal synchronism1010 Motl RW, Dlugonski D, Suh Y, Weikert M, Fernhall B, Goldman M. Accelerometry and its association with objective markers of walking limitations in ambulatory adults with multiple sclerosis. Arch Phys Med Rehabil. 2010;91(12):1942-7.,1111 Sibley KM, Tang A, Brooks D, McIlroy WE. Effects of extended effortful activity on spatio-temporal parameters of gait in individuals with stroke. Gait Posture. 2008;27(3):387-92.. In the major part of neurological impairments, the relation between the disease and motor disorders, although complex, is more apparent because the anatomopathological disease basis involves the recognized damage to the structures responsible for the generation and conduction of nerve stimuli1212 Belda-Lois JM, Mena-del Horno S, Bermejo-Bosch I, Moreno JC, Pons JL, Farina D, et al. Rehabilitation of gait after stroke: a review towards a top-down approach. J Neuroeng Rehabil. 2011;8(1):66.. Often, this framework does not apply to CLBP since the maintenance of the chronic condition may persist even when no physical reason justifies it1313 Shambrook J, Mcnee P, Harris EC, Kim M, Sampson M, Palmer KT, et al. Clinical presentation of low back pain and association with risk factors according to findings on magnetic resonance imaging. Pain. 2012;152(7):1659-65..
Nevertheless, a possible explanation for motor impairment in chronic pain conditions may be the deleterious changes in brain morphology. Recent studies have shown that individuals with symptoms of CLBP showed a loss in the volume and density of the gray matter of the dorsolateral prefrontal cortex, thalamus, somatosensory cortex, and midbrain1414 de Laat KF, Tuladhar AM, van Norden AGW, Norris DG, Zwiers MP, de Leeuw FE. Loss of white matter integrity is associated with gait disorders in cerebral small vessel disease. Brain. 2011;134(Pt 1):73-83.,1515 Wood PB. Variations in brain gray matter associated with chronic pain. Curr Rheumatol Rep. 2010;12(6):462-9..
Walking is described as one of the abilities most affected by CLBP. Considering the possibility of motor changes arising from central changes, identifying changes in walking kinematics in LBP becomes relevant. Therefore, the aim of this study was to determine if CLBP and walking speed (WS) affect the spatiotemporal parameters (stride length, swing time, contact time, stride time, stride frequency and walking ratio) and the coefficients of variation (CoV) of stride length and contact time.
The hypothesis of this study was that participants with CLBP are less able to adjust the spatiotemporal parameters as a result of speed variation, but especially in the preferred self-selected speeds because these patients tend to choose speed rates slower than healthy people, and as it has recently been demonstrated, at lower speeds the inter-strides variation is critical1616 Oliveira HB, Rosa RG, Gomeñuka NA, Peyré-Tartaruga LA. Estabilidade dinâmica da caminhada de indivíduos hemiparéticos: a influência da velocidade. Rev Educ Física/UEM. 2013;24(4):559-65.,1717 Hicks GE, Sions JM, Coyle PC, Pohlig RT. Altered spatiotemporal characteristics of gait in older adults with chronic low back pain. Gait Posture. 2017;55:172-6.. Based on this, it is expected that participants with CLBP have their dynamical stability impaired (assessed by inter-stride variation) at all speeds tested.
METHODS
After the sample calculation, which was determined for the variable “speed” (WinPepi version 11.18; power = 80%; significance level 5%; SD control group = 0.16; SD low back pain group = 0.21; difference to be detected = 0.3; at least n = 8 for each group), volunteers of both genders and aged over 25 years, with and without CLBP were recruited. The CG consisted of participants without systemic or musculoskeletal disorders in the lower limbs and spine, either chronic or acute, reported during the last year.
The chronic low back pain group (LG) consisted of volunteers with CLBP, from a local Rehabilitation Center, and with no musculoskeletal injuries in other joints on lower limbs and/or systemic illnesses which impairs the ability to walk. They were recruited intentionally and not probabilistically. The inclusion criteria for the LG followed the recommendations of original or review articles that focused on the diagnosis and treatment of LBP, according to the signs and symptoms indicated in the anamnesis and physical examination33 Negrini S, Fusco C, Atanasio S, Romano M, Zaina F. Low back pain: state of art. Eur J Pain Suppl. 2008;2(Supp 1):52-6.,1818 Chou R, Qaseem A, Snow V, Casey D, Cross TJ, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478-91.. Thus, volunteers should report LBP persisting for more than three months, without radiation to the lower limbs but with physical and clinical characteristics compatible with Category 1 pain (nonspecific low back pain) according to the guidelines for evaluation and treatment that are proposed by the American College of Physicians and the American Pain Society1818 Chou R, Qaseem A, Snow V, Casey D, Cross TJ, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478-91..
Volunteers, from both groups, were excluded if they did systematically and routinely engage in physical exercise, two or more times per week for at least 30 minutes; did show obvious differences in length of the lower limbs, postural misalignments and body mass indexes greater than 30.0kg.m-2. For data processing, videos with bad technical quality were excluded from the analysis.
Measures
The experimental design of this study involved the following steps: 1) screening; 2) preferred self-selected speed determination; 3) spatiotemporal assessment; 4) data analysis.
After the explanation about the procedures and objectives of the research, the volunteers underwent clinical screening to identify possible exclusion factors and collection of history and anthropometric data.
To determine the preferred self-selected speed (PS), the participant underwent a familiarization period, for five minutes, on the treadmill (Embrex 563-R3, Brusque, Brazil) and then the PS was determined. The PS was determined as follows: a) the volunteer was asked to choose the most comfortable speed, similar to the one used daily, that could be maintained over a long path; b) the treadmill speed was increased progressively up to a standard of 7 km.h-1 (or until before the volunteer felt insecure in walking) and then reduced in the same pattern so that the volunteer could choose his PS in each set; c) the PS of each patient was determined by calculating the mean of the PSs from two sets of recording1919 Dingwell JB, Marin LC. Kinematic variability and local dynamic stability of upper body motions when walking at different speeds. J Biomech. 2006;39(3):444-52..
A high-speed digital video camera (Casio High Speed - HS Exilim EX-FH25, Norderstedt, Germany) recorded the spatiotemporal parameters. Data acquisition occurred at a frequency of 240Hz. The camera was placed perpendicular to the treadmill with a focus on the lower limbs, especially on legs and feet.
The test battery was divided into three sections according to WS intensity as follows: PS, and slower and faster than the PS. Only three intensities were proposed to avoid overloading on the LG. In the first section, the participants walked at their PS. The order of the next two sections was randomly selected so that in one case, the volunteers walked 0.5 km·h-1 slower than the PS, and the other the volunteers walked 0.5 km·h-1 faster than the PS. In each section, the participants walked for five minutes. The images were captured in the last 30s of each section to minimize variability between steps2020 Zeni JA, Higginson JS. Gait parameters and stride-to-stride variability during familiarization to walking on a split-belt treadmill. Clin Biomech. 2010;25(4):383-6..
During the treadmill walking tests, minute by minute, the participants were asked to grade the pain experienced at that exact moment using the visual analogue scale (zero to 10, where zero represented absence of pain, and 10 the worst possible pain) making a total of six samples: from moment zero immediately before start walking until the moment five at the end of the last walking minute. The valid pain scores of each section for statistical analysis was the arithmetic average of all measures of that section.
Data processing
For kinematic analysis, the ‘Kinovea’ software (V0.8.15; Kinovea open source project, www.kinovea.org) was used to determine the spatiotemporal parameters by visually identifying the total of frames, computing frame by frame, corresponding to the touching of the heel on the ground (landing) and the moment when a foot lost contact with the ground (toe-off) for 16 strides analyzed in that last 30s time. Each stride cycle comprised the interval between two consecutive take-offs of the same foot2121 Racic V, Pavic A, Brownjohn JMW. Experimental identification and analytical modelling of human walking forces: literature review. J Sound Vib. 2009;326(1-2):1-49.,2222 Thomas EE, De Vito G, Macaluso A. Physiological costs and temporo-spatial parameters of walking on a treadmill vary with body weight unloading and speed in both healthy young and older women. Eur J Appl Physiol. 2007;100(3):293-9..
The spatiotemporal parameters analyzed, and their respective measurement units and definitions are presented in table 1 2121 Racic V, Pavic A, Brownjohn JMW. Experimental identification and analytical modelling of human walking forces: literature review. J Sound Vib. 2009;326(1-2):1-49.,2222 Thomas EE, De Vito G, Macaluso A. Physiological costs and temporo-spatial parameters of walking on a treadmill vary with body weight unloading and speed in both healthy young and older women. Eur J Appl Physiol. 2007;100(3):293-9.. We also calculated the CoV of contact time and stride length, obtained by the ratio between standard deviation and by the average values arising from each step transformed into percentage values1616 Oliveira HB, Rosa RG, Gomeñuka NA, Peyré-Tartaruga LA. Estabilidade dinâmica da caminhada de indivíduos hemiparéticos: a influência da velocidade. Rev Educ Física/UEM. 2013;24(4):559-65.. The CoV is expressed in percentage values (CoV%).
List of the spatiotemporal parameters analyzed in the present study, their units and definitions
The present study was previously approved by the Research Review Board of the Universidade Estadual do Oeste do Paraná (Report 1433/2011), in accordance with resolution 466/12, and it was classified as observational, ex-post-facto, exploratory-descriptive, transversal study. All volunteers received clarification regarding the study aims and procedures before inclusion, and all provided formal consent to participate.
Statistical analysis
Regarding variable stride length, we considered only normalized values by lower limb length for statistical treatment. We tested the data normality by the Shapiro-Wilk test. For all statistical tests, we adopted α=0.05.
We compared the participants’ characteristics using the Mann-Whitney test (intergroup comparison). We verified if there was any difference in pain scores for LG between the speeds using the Friedman test. The verification of LBP effect (main group effect), walking speed effect (main effect of speed) and their interactions were made using the Generalized Estimating Equation (GEE) method. In post-tests, we applied the Bonferroni test.
RESULTS
In total, 20 volunteers were recruited, being five men and five women in each group. Statistical differences in age, PS, anthropometric characteristics were not observed between the groups, but we found differences in pain scores (Table 2). The pain scores were not different between the speeds for LG (p=0.8302).
Presentation of descriptive statistics (median, 25%, and 75% percentile) and intergroup comparison between the variables of sample characterization
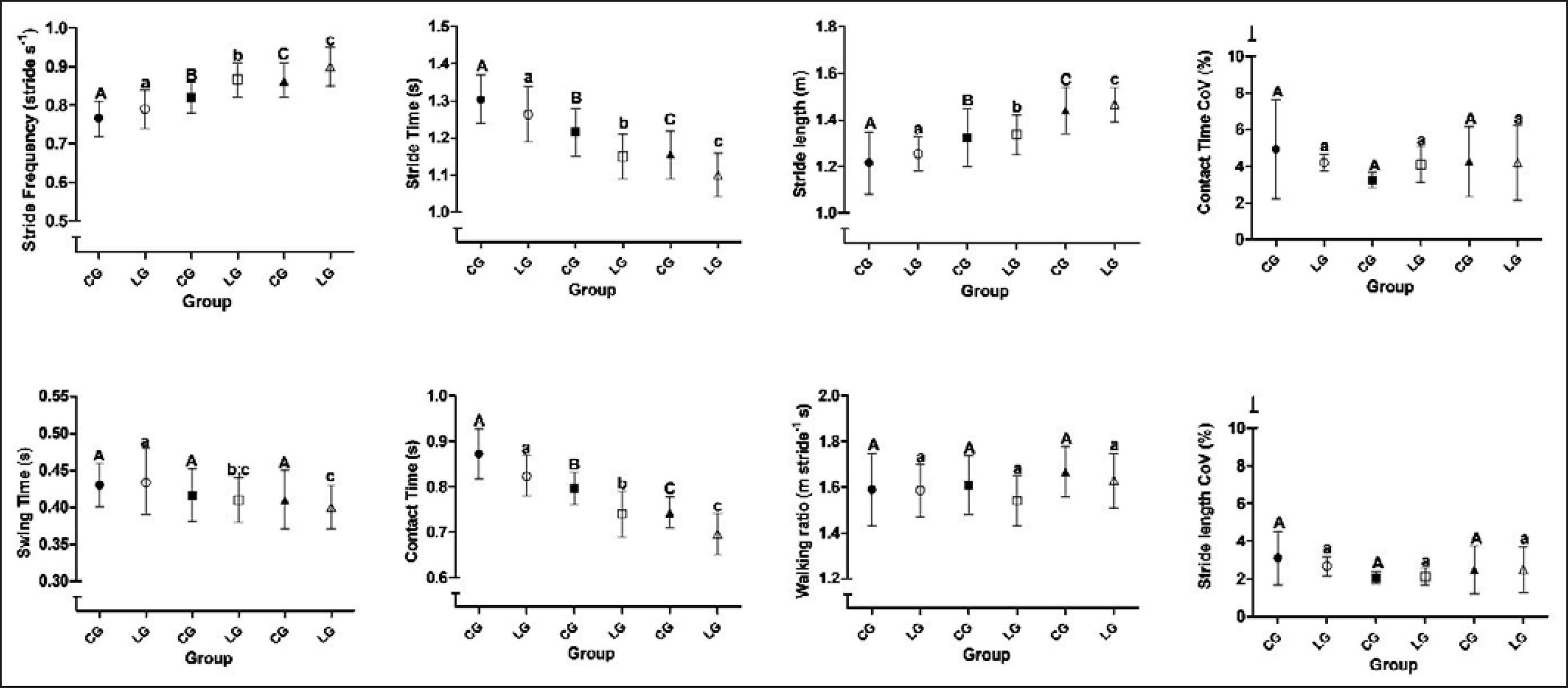
The descriptive statistic for the spatiotemporal variables is presented in figure 1. No main group effect was found as well as interactions between group and speed, but we found the effect of speed. It can be observed that stride frequency and stride length increased as the speed was higher. The contact time and stride time decreased as the speed was higher. We did not find effect of speed on the walking ratio. The CoVs were below 5%.
Descriptive statistics (mean and 95% confidence interval) and inferential comparisons of the spatiotemporal variables by assessing the effect of speed
DISCUSSION
We aimed to determine if CLBP and WS affect the spatiotemporal parameters. The results of this study indicated that CLBP did not have a significant effect on the spatiotemporal parameters. However, the WS did affect them.
The effect of speed on the spatiotemporal parameters has been reported before, as speed is accompanied by changes in the kinematic parameters2323 Stoquart G, Detrembleur C, Lejeune T. Effect of speed on kinematic, kinetic, electromyographic and energetic reference values during treadmill walking. Clin Neurophysiol. 2008;38(2):105-16.. Likewise, it is emphasized that the walking speed is the product of stride length and frequency, but at the same time, these parameters are also determined by the speed, and this is a consequence of the complex interaction between mechanical parameters, task demand, and motor control2424 Osaki Y, Kunin M, Cohen B, Raphan T. Relative contribution of walking velocity and stepping frequency to the neural control of locomotion. Exp Brain Res. 2008;185(1):121-35.. It means that changes in the spatiotemporal parameters observed in this study, by the influence of the speed, are supported by the scientific and technical literature.
As the relation choice between stride length and stride frequency tends to be spontaneous at a self-selected speed, and even at different speeds2525 Danion F, Varraine E, Bonnard M, Pailhous J. Stride variability in human gait: the effect of stride frequency and stride length. Gait Posture. 2003;18(1):69-77., the walking ratio is considered as an index of the walking pattern which is independent of speed. Thus, a constant walking ratio at different speeds reveals a normal walking pattern2626 Sekiya N, Nagasaki H. Reproducibility of the walking patterns of normal young adults: test-retest reliability of the walk ratio (step-length / step-rate). Gait Posture. 1998;7(1):225-7.. As the walking ratio of the present study in both groups showed no statistical differences between the three intensities in speed and no significant group effect, we concluded that all the studied participants were skilled enough to adapt their kinematic parameters to each task demand.
Besides, the low values and the lack of statistical difference in the CoV index reinforce our findings, indicating stable gait characteristics. Variability of both stride time and length are closely related to the control of the rhythmic stepping mechanism associated with safe gait2727 Beauchet O, Allali G, Annweiler C, Bridenbaugh S, Assal F, Kressig RW, et al. Gait variability among healthy adults: low and high stride-to-stride Variability are both a reflection of gait stability. Gerontology. 2009;55(6):702-6.. Variability, represented by CoV, provides additional information about the behavior of the gait concerning average values of the kinematic variables and tends to be low in walks considered stable, being advocated percentage values for normal coefficient variation lower than 3% among young adults. Also, variability tends to be higher at lower speeds and, on the contrary, lower at higher speeds. The smaller the variability the greater the gait dynamic stability1616 Oliveira HB, Rosa RG, Gomeñuka NA, Peyré-Tartaruga LA. Estabilidade dinâmica da caminhada de indivíduos hemiparéticos: a influência da velocidade. Rev Educ Física/UEM. 2013;24(4):559-65.,2828 Beauchet O, Annweiler C, Lecordroch Y, Allali G, Dubost V, Herrmann FR, et al. Walking speed-related changes in stride time variability: effects of decreased speed. J Neuroeng Rehabil. 2009;6:32..
In the present study, both groups were able to adjust their spatiotemporal parameters, and the LG reported low pain scores at all speeds without difference between them. We believe to be this the cause of the lack of statistical difference for PS between groups.
Our initial hypothesis was that participants with CLBP are less able to adjust the spatiotemporal parameters due to speed variation. This hypothesis was based on the findings of other authors2929 Newell D, van der Laan M. Measures of complexity during walking in chronic non-specific low back pain patients. Clin Chiropr. 2010;13(1):8-14.. In the medical literature, some investigators have highlighted the impairment in the walking pattern in people with CLBP as a synchronous movement between trunk and pelvis leading to “en bloc” style of walking, alteration of proprioceptive postural control, tendency to adopt ankle strategy for walking and slower speed gait than people without CLBP. In general, it is accepted that those adaptations might happen as a protective reaction to avoid pain3030 Carvalho AR, Andrade A, Peyré-Tartaruga LA. Possible changes in energy-minimizer mechanisms of locomotion due to chronic low back pain - a literature review. Rev Bras Reumatol. 2015;55(1):55-61.,3131 Henchoz Y, Soldini N, Peyrot N, Malatesta D. Energetics and mechanics of walking in patients with chronic low back pain and healthy matched controls. Eur J Appl Physiol. 2015;115(11):2433-43.. However, our data indicate the opposite, and they do not support the theory that patients with CLBP avoid moving due to the pain.
Despite some mechanical reasons to believe that the gait in CLBP patients could be changed, it is possible that the spatiotemporal features may not reflect the kinetics impaired. It is possible to speculate that one should consider other relevant features involved in the etiology of LBP syndrome for that spatiotemporal changes to be present.
Henchoz et al.3131 Henchoz Y, Soldini N, Peyrot N, Malatesta D. Energetics and mechanics of walking in patients with chronic low back pain and healthy matched controls. Eur J Appl Physiol. 2015;115(11):2433-43. did not observe differences in the spatiotemporal, mechanical, and metabolic variables in people with and without LBP, even with the self-selected speed for the lumbar group being slower than the control group. One of the arguments suggested to explain these outcomes was that peripheral musculoskeletal disorders, unlike central musculoskeletal disorders, may not be sufficiently large to cause a less efficient walking pattern.
One study suggested that CLBP patients seem to be more effective at slow speeds than fast speeds (speed effect), although there was no difference in free-pain participants3232 Carvalho AR, Ribeiro Bertor WR, Briani RV, Zanini GM, Silva LI, Andrade A, et al. Effect of nonspecific chronic low back pain on walking economy: an observational study. J Mot Behav. 2016;48(3):218-26.. The authors speculated that the repercussion of neurophysiological adjustments due to painful stimuli could explain the motor behavior in people with CLBP and consequently the metabolic parameters.
Indeed, the LBP is a syndrome-based condition, and the contribution of psychosocial and neuropsychological factors on the performance of motor tasks is still poorly understood and confusing in the context of CLBP. The contemporary classification system for this syndrome is yet not sensitive enough to include all etiological aspects. Probably, the physical classification systems for LBP do not consider relevant dimensions as pain characteristics, psychophysical, psychological, social, lifestyle, movement or comorbidities in an integrated manner to provide a diagnosis that allows recognizing single features in each case3333 Rabey M, Beales D, Slater H, O'Sullivan P. Multidimensional pain profiles in four cases of chronic non-specific axial low back pain: an examination of the limitations of contemporary classification systems. Man Ther. 2015;20(1):138-47..
Corroborating other papers, the researchers observed that patients with CLBP, although they had a lower level of strength on dorsal and lower limb muscles or in psychosocial variables, they did not show differences in the six-minute walk tests performance in comparison to healthy people55 Bertor WRR, Fracaro GA, Silva LI, Zílio M, Aragão FA, Carvalho AR. Subclassificação da lombalgia crônica e nível de incapacidade: efeito no desempenho funcional e força muscular. Conscientiae Saúde. 2013;12(4):563-71.,66 Fracaro GA, Bertor WR, Silva LI, Brandl L, Zanini GM, Zílio M, et al. Comparison of psycho-social and functional performance variables in a group of chronic low back pain patients. Rev Dor. 2013;14(2):119-23.. It is important to highlight that the speeds evaluated were self-selected.
We suggest future papers to include other etiological dimensions in the analysis to compose groups functionally more homogeneous. The major limitation of this study is that we did not have a fixed speed aiming to compare both groups under similar mechanical conditions.
In general, one cause of concern about CLBP rehabilitation relates to the improvement of walking ability; mainly because these patients tend to walk slower. According to two systematic reviews, walking is a recommended strategy to be used in the management of CLBP to reduce pain and disability3434 Sitthipornvorakul E, Klinsophon T, Sihawong R, Janwantanakul P. The effects of walking intervention in patients with chronic low back pain: a meta-analysis of randomized controlled trials. Musculoskelet Sci Pract. 2018;34:38-46., although there is low-quality evidence to bespeak that walking is a strategy, in comparison with other non-pharmacological, and more effective, approaches3535 Lawford BJ, Walters J, Ferrar K. Does walking improve disability status, function, or quality of life in adults with chronic low back pain? A systematic review. Clin Rehabil. 2016;30(6):523-36..
Our results make us think if the strategies used in rehabilitation, aiming to correct the spatiotemporal parameter of gait for CLBP patients are necessary. The present findings show that the spatiotemporal profile of gait in this syndrome-based condition does not change across slow, middle, and high walking speeds. The gait variability is an indirect marker of dynamical stability and, though previous evidence shows a greater step width in people with LBP, these changes are not enough to impair the global stability parameters assessed here.
CONCLUSION
We conclude that CLBP does not affect the spatiotemporal parameters, at least for those patients classified as CLBP according to the signs and symptoms criteria. Although the WS has affected the spatiotemporal parameters, both LG and CG patients were able to adjust their kinematic parameters to each task demand sustaining a low variability of gait.
-
Sponsoring sources: Centro de Reabilitação Física da UNIOESTE e Centro de Ciências Biológicas e da Saúde - CCBS, UNIOESTE, Cascavel, PR, Brasil.
ACKNOWLEDGEMENTS
UNIOESTE Physical Rehabilitation Center and Biological and Health Sciences Center CCBS/UNIOESTE, Cascavel, PR, Brazil.
REFERENCES
-
1Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8-20.
-
2Meucci RD, Fassa AG, Faria NM. Prevalence of chronic low back pain: systematic review. Rev Saude Publica. 2015;49. pii: S0034-89102015000100408.
-
3Negrini S, Fusco C, Atanasio S, Romano M, Zaina F. Low back pain: state of art. Eur J Pain Suppl. 2008;2(Supp 1):52-6.
-
4Welch E. Low back pain. InnovAiT. 2012;5(1):13-21.
-
5Bertor WRR, Fracaro GA, Silva LI, Zílio M, Aragão FA, Carvalho AR. Subclassificação da lombalgia crônica e nível de incapacidade: efeito no desempenho funcional e força muscular. Conscientiae Saúde. 2013;12(4):563-71.
-
6Fracaro GA, Bertor WR, Silva LI, Brandl L, Zanini GM, Zílio M, et al. Comparison of psycho-social and functional performance variables in a group of chronic low back pain patients. Rev Dor. 2013;14(2):119-23.
-
7Andrew Walsh D, Jane Kelly S, Sebastian Johnson P, Rajkumar S, Bennetts K. Performance problems of patients with chronic low-back pain and the measurement of patient-centered outcome. Spine. 2004;29(1):87-93.
-
8Simmonds MJ, Lee CE, Etnyre BR, Morris GS. The influence of pain distribution on walking velocity and horizontal ground reaction forces in patients with low back pain. Pain Res Treat. 2012;2012:214980.
-
9Saibene F, Minetti AE. Biomechanical and physiological aspects of legged locomotion in humans. Eur J Appl Physiol. 2003;88(4-5):297-316.
-
10Motl RW, Dlugonski D, Suh Y, Weikert M, Fernhall B, Goldman M. Accelerometry and its association with objective markers of walking limitations in ambulatory adults with multiple sclerosis. Arch Phys Med Rehabil. 2010;91(12):1942-7.
-
11Sibley KM, Tang A, Brooks D, McIlroy WE. Effects of extended effortful activity on spatio-temporal parameters of gait in individuals with stroke. Gait Posture. 2008;27(3):387-92.
-
12Belda-Lois JM, Mena-del Horno S, Bermejo-Bosch I, Moreno JC, Pons JL, Farina D, et al. Rehabilitation of gait after stroke: a review towards a top-down approach. J Neuroeng Rehabil. 2011;8(1):66.
-
13Shambrook J, Mcnee P, Harris EC, Kim M, Sampson M, Palmer KT, et al. Clinical presentation of low back pain and association with risk factors according to findings on magnetic resonance imaging. Pain. 2012;152(7):1659-65.
-
14de Laat KF, Tuladhar AM, van Norden AGW, Norris DG, Zwiers MP, de Leeuw FE. Loss of white matter integrity is associated with gait disorders in cerebral small vessel disease. Brain. 2011;134(Pt 1):73-83.
-
15Wood PB. Variations in brain gray matter associated with chronic pain. Curr Rheumatol Rep. 2010;12(6):462-9.
-
16Oliveira HB, Rosa RG, Gomeñuka NA, Peyré-Tartaruga LA. Estabilidade dinâmica da caminhada de indivíduos hemiparéticos: a influência da velocidade. Rev Educ Física/UEM. 2013;24(4):559-65.
-
17Hicks GE, Sions JM, Coyle PC, Pohlig RT. Altered spatiotemporal characteristics of gait in older adults with chronic low back pain. Gait Posture. 2017;55:172-6.
-
18Chou R, Qaseem A, Snow V, Casey D, Cross TJ, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478-91.
-
19Dingwell JB, Marin LC. Kinematic variability and local dynamic stability of upper body motions when walking at different speeds. J Biomech. 2006;39(3):444-52.
-
20Zeni JA, Higginson JS. Gait parameters and stride-to-stride variability during familiarization to walking on a split-belt treadmill. Clin Biomech. 2010;25(4):383-6.
-
21Racic V, Pavic A, Brownjohn JMW. Experimental identification and analytical modelling of human walking forces: literature review. J Sound Vib. 2009;326(1-2):1-49.
-
22Thomas EE, De Vito G, Macaluso A. Physiological costs and temporo-spatial parameters of walking on a treadmill vary with body weight unloading and speed in both healthy young and older women. Eur J Appl Physiol. 2007;100(3):293-9.
-
23Stoquart G, Detrembleur C, Lejeune T. Effect of speed on kinematic, kinetic, electromyographic and energetic reference values during treadmill walking. Clin Neurophysiol. 2008;38(2):105-16.
-
24Osaki Y, Kunin M, Cohen B, Raphan T. Relative contribution of walking velocity and stepping frequency to the neural control of locomotion. Exp Brain Res. 2008;185(1):121-35.
-
25Danion F, Varraine E, Bonnard M, Pailhous J. Stride variability in human gait: the effect of stride frequency and stride length. Gait Posture. 2003;18(1):69-77.
-
26Sekiya N, Nagasaki H. Reproducibility of the walking patterns of normal young adults: test-retest reliability of the walk ratio (step-length / step-rate). Gait Posture. 1998;7(1):225-7.
-
27Beauchet O, Allali G, Annweiler C, Bridenbaugh S, Assal F, Kressig RW, et al. Gait variability among healthy adults: low and high stride-to-stride Variability are both a reflection of gait stability. Gerontology. 2009;55(6):702-6.
-
28Beauchet O, Annweiler C, Lecordroch Y, Allali G, Dubost V, Herrmann FR, et al. Walking speed-related changes in stride time variability: effects of decreased speed. J Neuroeng Rehabil. 2009;6:32.
-
29Newell D, van der Laan M. Measures of complexity during walking in chronic non-specific low back pain patients. Clin Chiropr. 2010;13(1):8-14.
-
30Carvalho AR, Andrade A, Peyré-Tartaruga LA. Possible changes in energy-minimizer mechanisms of locomotion due to chronic low back pain - a literature review. Rev Bras Reumatol. 2015;55(1):55-61.
-
31Henchoz Y, Soldini N, Peyrot N, Malatesta D. Energetics and mechanics of walking in patients with chronic low back pain and healthy matched controls. Eur J Appl Physiol. 2015;115(11):2433-43.
-
32Carvalho AR, Ribeiro Bertor WR, Briani RV, Zanini GM, Silva LI, Andrade A, et al. Effect of nonspecific chronic low back pain on walking economy: an observational study. J Mot Behav. 2016;48(3):218-26.
-
33Rabey M, Beales D, Slater H, O'Sullivan P. Multidimensional pain profiles in four cases of chronic non-specific axial low back pain: an examination of the limitations of contemporary classification systems. Man Ther. 2015;20(1):138-47.
-
34Sitthipornvorakul E, Klinsophon T, Sihawong R, Janwantanakul P. The effects of walking intervention in patients with chronic low back pain: a meta-analysis of randomized controlled trials. Musculoskelet Sci Pract. 2018;34:38-46.
-
35Lawford BJ, Walters J, Ferrar K. Does walking improve disability status, function, or quality of life in adults with chronic low back pain? A systematic review. Clin Rehabil. 2016;30(6):523-36.
Publication Dates
-
Publication in this collection
02 Dec 2019 -
Date of issue
Oct-Dec 2019
History
-
Received
03 July 2019 -
Accepted
16 Sept 2019