Keywords
Aortopulmonary Window/surgery; Heart Defects; Congenital/surgery; Infant
Clinical data: At 10 months of age, the patient underwent correction of a large aortopulmonary window and mitral valve regurgitation secondary to volume overload, which caused severe heart failure. The post-operative clinical outcome was favorable. Prior to operation, her clinical picture was of concern because of severe malnutrition (weight of 5,500 g), congestive heart failure (tachypnea of 60 bpm), hepatomegaly (liver palpable at 4 cm of the right costal margin), severe cardiomegaly, and increased pulmonary vasculature. Cardiovascular examination showed left ventricular (LV) enlargement; thrill and systolic murmur in the mitral area; accentuated S2; marked LV overload on electrocardiogram (ECG); mitral regurgitation due to incomplete leaflet coaptation; and pulmonary systolic pressure of 60 mmHg. At surgery, the 2-cm-diameter window between the pulmonary trunk and ascending aorta (Ao) was closed, and plication of the posterior ring of the mitral valve was performed. There was an immediate clinical response with hemodynamic stabilization, resolution of the heart murmur and heart failure, and subsequent normal weight gain. Medication for congestive heart failure was discontinued at 4 years of age, when the cardiac silhouette had returned to normal. To date, the patient tolerates routine exercises well and does not report any symptoms.
Physical examination: good general state of health, normal breathing, acyanotic, normal pulses. Weight: 53 kg; height: 165 cm; blood pressure on right arm (BPRA): 105/75 mmHg; heart rate (HR): 76 bpm. Aorta not palpable on the suprasternal notch.
The apical impulse was not palpable in the precordium, and there were no systolic impulses. Normal heart sounds, no heart murmurs. Liver not palpable.
Laboratory tests
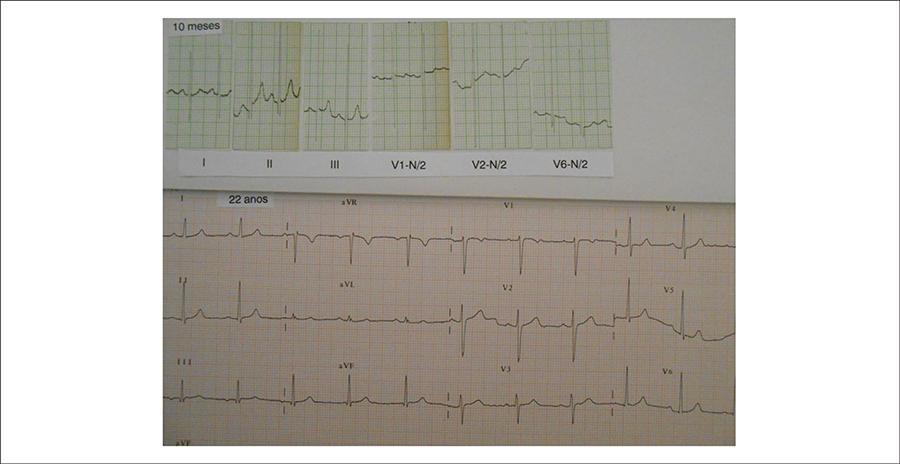
ECG (Figure 1) at 22 years of age showed normal sinus rhythm with no signs of overload, and normal ventricular repolarization. PA = +10º , QRSA = +50º , TA = +50º (lower tracing). ECG prior to operation, at 10 months of age (upper tracing), showed marked left ventricular overload, with QRSA = +70º , PA = +20º and TA = +80º ; RS morphology (amplitudes of 24 and 30 mm) from V1 to V3 and QRs (amplitudes of 10, 50 and 3 mm) from V4 to V6; Sokolow index of 90 mm; no ventricular repolarization abnormalities.
Electrocardiograms at two timepoints: in the preoperative period, at 10 months of age (upper tracing), and at late postoperative period at 22 years of age (lower tracing). These electrocardiograms show resolution of the left ventricular overload initially observed
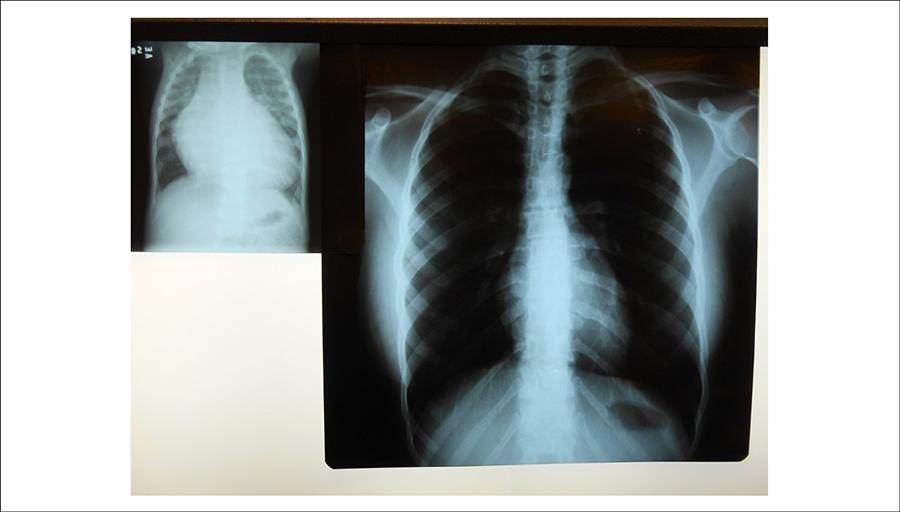
Chest radiograph showed normal cardiac silhouette (cardiothoracic ratio = 0.46) and pulmonary vasculature (Figure 2). In the image prior to surgery, these parameters were markedly increased, with a cardiothoracic ratio of 0.85 (Figure 2).
Chest radiographs in the preoperative period and later at 23 years of age, after surgical correction performed at 10 months of age, showing markedly enlarged and normal cardiac silhouette, respectively
Echocardiogram showed normal size cardiac chambers (Ao = 34; left atrium − LA = 36, right ventricle − RV = 13, LV = 49; ejection fraction − EF = 61%, septum = posterior wall = 8 mm); no mitral regurgitation. Echocardiogram prior to surgery showed enlargement of left chambers (LA = 37, Ao = 17 and LV = 42; RV = 10, septum = posterior wall = 5 mm; EF = 82%), with marked mitral regurgitation.
Clinical diagnosis: Aortopulmonary window with mitral regurgitation secondary to volume overload and severe heart failure resolved after surgical correction and favorable late outcome until adulthood.
Clinical reasoning: The postoperative clinical elements were consistent with normal cardiovascular parameters, unlike in the preoperative period, in which the overt manifestations of heart failure suggested the diagnosis of congenital heart defect expressed by signs of mitral regurgitation. On that occasion, the aortopulmonary window was diagnosed during surgery, and mitral regurgitation was secondary to and resulted from the volume overload caused by the defect. LV overload on ECG confirmed the magnitude of the volume overload, which predominated over the RV pressure overload.
Differential diagnosis: other defects accompanied by severe arterial left-to-right shunt, such as ductus arteriosus and arteriovenous fistulas, should be remembered in this context.
Management: In view of the marked consequences of the arterial shunt, the surgery for closure of the interarterial defect not only repaired the secondary dilatation of the mitral annulus, but also resulted in cure, thus surpassing the concern about pulmonary arterial hypertension at the time.
Commentaries: aortopulmonary window usually has important manifestations early in the first months of life, and cardiac surgery corrects the signs and symptoms of heart failure and associated defects such as those of secondary mitral regurgitation, which was present in the case reported11 Soares AM, Atik E, Cortêz TM, Albuquerque AM, Castro CP, Barbero-Marcial M, et al. Aortopulmonary window. Clinical and surgical assessment of 18 cases. Arq Bras Cardiol.1999;73(1):59-74.
2 Barnes ME, Mitchell ME, Tweddell JS Aortopulmonary window. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2011;14(1):67-74.
-
33 Atik E, Barbero-Marcial M, Andrade JL, Baucia JA, Iwahashi E, Aiello V, et al. [Clinical manifestation of aortopulmonary window as mitral regurgitation caused by secondary dilatation of the valvar anulus]. Arq Bras Cardiol. 1994;63 (6):493-5.. Generally, pulmonary arterial hypertension also subsides, and so does the secondary dilatation of the different correlate cardiac structures. This is encouraging, given the important implications of this defect, which should be corrected right after diagnosis. The return of anatomical and functional parameters to normal, in this case, becomes of great value as an example of outcome for similar cases in an early period of life.
References
-
1Soares AM, Atik E, Cortêz TM, Albuquerque AM, Castro CP, Barbero-Marcial M, et al. Aortopulmonary window. Clinical and surgical assessment of 18 cases. Arq Bras Cardiol.1999;73(1):59-74.
-
2Barnes ME, Mitchell ME, Tweddell JS Aortopulmonary window. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2011;14(1):67-74.
-
3Atik E, Barbero-Marcial M, Andrade JL, Baucia JA, Iwahashi E, Aiello V, et al. [Clinical manifestation of aortopulmonary window as mitral regurgitation caused by secondary dilatation of the valvar anulus]. Arq Bras Cardiol. 1994;63 (6):493-5.
Publication Dates
-
Publication in this collection
June 2015
History
-
Received
24 July 2014 -
Reviewed
06 Oct 2014 -
Accepted
06 Oct 2014