Abstracts
BACKGROUND: Leg ulcers are characterized as tissue loss in the lower extremities, generally caused by vascular dysfunction. OBJECTIVES: Verify the clinical and epidemiological profiles of the population sample with leg ulcers treated at the health centers of Juiz de Fora (Brazil). MATERIAL AND METHODS: 124 leg-wound patients were evaluated between January 1999 and August 2001 and submitted to a clinical protocol. RESULTS: The mean age was 64 years, with females in the majority (65.3%). The mean family composition was 3.7 persons, and family income was around US$200.00 (86.8%). Venous insufficiency (90.3%), systemic arterial hypertension (54%), obesity (20.2%) and diabetes mellitus (16.1%) were the most frequent events associated with the ulcers. An association of venous insufficiency and arterial hypertension was frequent in 43.7% of the sample, and significant (p<0.01) to predisposition to the ulcers. These were classified as venous (79%), hypertensive (15.4%), mixed and other (5.6%). The ulcers were generally localized in the distal third of legs (90%) and considered large (5 cm) in about 90% of the sample, with means of 8.7 cm and 9.6 cm to vertical and horizontal axes, respectively. The ulcers were accompanied mainly by hyperpigmentation (92.7%), lipodermatosclerosis (68.5%) and varicose veins (66.9%), with a mean duration of 94.2 months and 50% of them recurrent. CONCLUSIONS: The data suggested that leg ulcer is an important chronic disease in the elderly and poor population of Juiz de Fora and region.
Aged; Income; Family income; Leg ulcers; Varicose veins
FUNDAMENTOS: Úlcera de perna (UP) caracteriza-se por perda do tegumento nas extremidades dos membros inferiores causada geralmente por disfunção vascular. OBJETIVOS: Caracterizar clínica e epidemiologicamente a amostra populacional com UP atendida nos centros de saúde de Juiz de Fora. PACIENTES E MÉTODOS: Submetidos ao protocolo clínico 124 pacientes com UP, de Juiz de Fora e região de janeiro/1999 a agosto/2001. RESULTADOS: A média de idade foi 64 anos, 65,3% do sexo feminino, média de 3,7 indivíduos/família e renda inferior a R$540,00 (86,8%). Associavam-se às úlceras insuficiência venosa (90,3%), hipertensão arterial sistêmica (54%), obesidade (20,2%) e diabetes mellitus (16,1%). A associação insuficiência venosa e hipertensão arterial foi freqüente (43,7%) e significante (p<0.01) para predisposição às úlceras. Foram classificadas como venosas (79%), hipertensivas (15,4%), mistas e outras(5,6%). Acometiam terço distal das pernas (90%), de tamanho grande (5cm) em cerca de 90% da amostra, com médias de 8,7cm e 9,6cm para os eixos vertical e horizontal, respectivamente. Estavam acompanhadas de hipercromia (92,7%), lipodermatoesclerose (68,5%) e varicosidades (66,9%), com duração média de 94,2 meses, e 50% das úlceras eram recidivantes. CONCLUSÕES: Os dados sugerem que a úlcera de perna seja doença crônica significativa na população idosa e de baixa renda de Juiz de Fora e região.
Idoso; Renda; Renda familiar; Úlcera da perna; Varizes
CLINICAL, EPIDEMIOLOGICAL, LABORATORY AND THERAPEUTIC INVESTIGATION
Leg ulcer: an observational study in Juiz de Fora, MG (Brazil) and region* * Work done at Dermatology Service, University Hospital of the Federal University of Juiz de Fora, Juiz de Fora, MG, Brazil.
Marco Andrey Cipriani FradeI; Igor Brum CursiII; Felipe Fortes AndradeII; Samara Casemiro SoaresII; Wendel S. RibeiroII; Sandro V. SantosII; Norma Tiraboschi FossIII
IMD, PhD. Professor, Dermatology Division, Department of Clinical Medicine, Ribeirao Preto Faculty of Medicine (USP/FAEPA) / Former Auxiliary Professor, Dermatology Service, Federal University of Juiz de Fora, MG
IIStudent of the Graduate studies in Medicine Program, Federal University of Juiz de Fora, MG
IIIMD, PhD, Associate Professor, Dermatology Sector, Clinical Medicine Department, Riberão Preto Faculty of Medicine (USP), SP
Correspondence Correspondence to Marco Andrey Cipriani Frade Divisão de Dermatologia - Hosp. das Clinicas FMRP/USP Av. Bandeirantes, 3900 - Bairro Monte Alegre Ribeirão Preto SP 14049-900 Tel/Fax: (16) 633-6695 E-mail: mandrey@fmrp.usp.br
ABSTRACT
BACKGROUND: Leg ulcers are characterized as tissue loss in the lower extremities, generally caused by vascular dysfunction.
OBJECTIVES: Verify the clinical and epidemiological profiles of the population sample with leg ulcers treated at the health centers of Juiz de Fora (Brazil).
MATERIAL AND METHODS: 124 leg-wound patients were evaluated between January 1999 and August 2001 and submitted to a clinical protocol.
RESULTS: The mean age was 64 years, with females in the majority (65.3%). The mean family composition was 3.7 persons, and family income was around US$200.00 (86.8%). Venous insufficiency (90.3%), systemic arterial hypertension (54%), obesity (20.2%) and diabetes mellitus (16.1%) were the most frequent events associated with the ulcers. An association of venous insufficiency and arterial hypertension was frequent in 43.7% of the sample, and significant (p<0.01) to predisposition to the ulcers. These were classified as venous (79%), hypertensive (15.4%), mixed and other (5.6%). The ulcers were generally localized in the distal third of legs (90%) and considered large (>5 cm) in about 90% of the sample, with means of 8.7 cm and 9.6 cm to vertical and horizontal axes, respectively. The ulcers were accompanied mainly by hyperpigmentation (92.7%), lipodermatosclerosis (68.5%) and varicose veins (66.9%), with a mean duration of 94.2 months and 50% of them recurrent.
CONCLUSIONS: The data suggested that leg ulcer is an important chronic disease in the elderly and poor population of Juiz de Fora and region.
Keywords: Aged; Income; Family income; Leg ulcers/ epidemiology; Varicose veins.
INTRODUCTION
A leg ulcer is a syndrome characterized by circumscribed or irregular loss of tegument (dermis or epidermis), which may reach subcutaneous and subjacent tissues. It affects the extremities of the lower limbs. Its cause is usually related to the arterial or venous vascular system.1
The etiology of leg ulcers emerges from chronic venous insufficiency from 80 to 85% of the time, and arterial disease in 5 to 10% of cases. The rest are of neuropathic origin (usually diabetes) or mixed.2,3 They may be classified as venous, hypertensive, ischemic, anemic, diabetic foot and thromboangiitis obliterans.1
In spite of the rare epidemiological studies available on leg ulcers, they are commonly found in medical practice and absorb large sums of the health care funds earmarked for managing them. Their frequency has grown along with increased life expectancy in the world population. In the USA, 600,000 new leg ulcer cases occur yearly. In Sweden, four to 5% of the population over the age of 80 years presents with this pathology. The annual cost for treating leg ulcer patients is estimated at some $25 million.1,4
Juiz de Fora is a medium sized city located in the mid-region of the Mineira Forest Zone no. 3.112 (Mata Mineira Mesoregião). It has a population of 465,076 inhabitants.5 Health care services are rendered mainly at the UFJF University Hospital and cover the entire "Forest Zone" ("Zona da Mata"), in addition to a number of southern Minas Gerais and Rio de Janeiro state municipalities.
This study is bound to open new ground. At present, there are no reports available containing statistical data published on leg ulcers in the Juiz de Fora region, although cases are regularly treated at dermatology, angiology, and plastic surgery services. The treatment of leg ulcers always takes time and is difficult owing to diversity in etiologies and therapies.3,6,7
Despite the disease's relevance, little is known about its distribution in the country's population or even in different regions. Accordingly, we have sought to draw a clinical-epidemiological profile of a leg ulcer patient sample treated especially at specialized treatment units in the Juiz de Fora region. The most frequent types of ulcers, associated diseases and patients' socioeconomic profile are assessed. We hope this will help prompt further studies on this theme.
PATIENTS AND METHODS
The present study was based on surveying cases diagnosed as leg ulcers, which were occasionally collected during clinical treatment carried out by clinical physicians and/or dermatologists and trainee-students in the UFJF Medical School from January 1999 to August 2001. The cases were collected in two care units specialized in leg ulcers-the ambulatories of the UFJF University Hospital and PAM (the Juiz de Fora Municipality Medical Care Center)-in addition to four basic municipal health units belonging to the UFJF Medical School Community Medicine Training Program.
After reading and signing the terms of consent, patients were submitted to a clinical and dermatological examination. A treatment protocol form was filled out covering the following data: regional health unit, personal data (age, sex, and color), family composition and income, associated diseases, medication use, systemic blood pressure, leg ulcer examination (type, localization, area, associated signs and symptoms, duration, history of recurrences).
The date were analyzed in accordance with the frequency (%) found in the sample.
RESULTS
One-hundred twenty-four patients were assessed. Yet not all of the protocol items were answered. Accordingly, the frequency analysis of the sample varies as a function of the number of protocols filled out for each specific variable.
The sample showed a mean age of 64 years, varying from 27 to 94 years (Table 1). As for sex, 34.7% were male and 65.3% female.
Among these patients, 86 (69.4%) came from the UH, 31 (25%) from the PAM, and seven (6%) from basic health units.
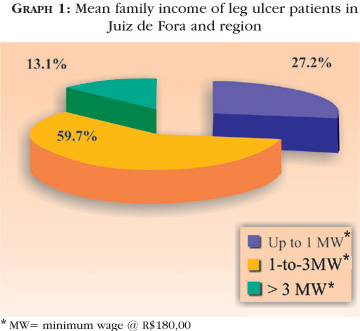
Only 114 patients agreed to provide information regarding family income (Graph 1).
The average family composition was 3.7 individuals per family (n=114). The figure for personal income was obtained by dividing mean family income by the number of each patient's family members. Therefore, by dividing the sum of the mean income values per person by the total amount of individuals in the sample, the mean income per person was determined to be R$ 95.00. Standard deviation was R$ 55.00, mean R$ 84.00 per person (95.00+55.00).
In relation to the patient's clinical history, diseases frequently associated with leg ulcers were investigated, such as venous insufficiency (present in 90.3%), systemic arterial hypertension (54%), obesity (20.2%), and diabetes (16.1%). The association of the chronic venous insufficiency with systemic arterial hypertension occurred in 54 patients (43.7%), becoming a predisponent factor to leg ulcers statistical significance (p<0.01, chi-square test).
As for medication use, 66%; of the sampled patients were observed to be taking some kind of drug, with oral antidiabetics (usually glibenclamide) and/or anti-hypertensive (generally inhibitors of the angiotensin converting-enzyme, methyldopa, furosemide) in order to control chronic diseases, such as systemic arterial hypertension and/or diabetes mellitus, in addition to treating the leg ulcer itself.
Patients' blood pressure, taken during the first consultation, presented with an average 151 mmHg systolic and 89.4 mmHg diastolic.
The classification of ulcers was based on clinical criteria that became evident during the initial examination, whose frequency is described in table 2.
In the evaluation of ulcer size, measurements of the largest wound axes were considered, that is, vertical and horizontal axes, due to surface irregularities rendering area and volume calculations difficult. When considering only the main lesions, or the largest ulcer among the cases with more than one lesion, 124 lesions were analyzed. They were assembled in categories (small, medium and large) in accordance with the aforementioned criteria (Table 2).
The local signs and symptoms associated with leg ulcers were assessed as shown in the results of table 3.
Most patients (107) presented with a lesion on only one of the lower limbs, which corresponded to 86% of cases. A single ulcer was observed in 65% of patients (81), two ulcers in 33% (42), and three lesions in only two patients (roughly 2%). If all lesions were considered, 169 ulcers would be assessed.
As for localization, the lower limb was divided into zones, as proposed by Baker et al. (1991),8 namely: Zone 1 (area corresponding to the foot), Zone 2 (area including the distal half of the leg and ankle) and Zone 3 (proximal half of the leg) (Figure 1). One hundred and sixty-nine ulcers were analyzed, with the medial and lateral faces for zones 2 and 3, and the dorsal and plantar regions for zone 1.
As for the surface of the ulcer-affected limb, it was observed that among the 169 lesions assessed, 152 (89.9%) were localized on the legs, 85 (50.3%) on the lateral face, and 67 (39.6%) on the medial face. All of the ulcers affecting the feet were localized on the dorsal aspect.
With respect to the duration of the leg ulcer, 34 patients were not able to answer. Of the 90 protocols that did provide answers, the average length of time was 94.2 months (94.2 + 127) and the median 36 months.
There was a recurrence of leg ulcers observed in 45 patients (50%), while the other half lived with the disease without interruption. Due to the variety of the ulcers' duration time, the authors chose to present the information in periods, as shown in table 4.
DISCUSSION
The University Hospital (UH) of the Federal University of Juiz de Fora is the institution of reference in the Minas Gerais Forest Zone (Zona da Mata), and attends to an average of 102,615 patients yearly. Dermatology at the UH is responsible for half of the 7,906 yearly treatments (data relative to the two year 1999-2000 period).
Of the 124 patients assessed, 6% came from basic health care units, and 94% from specialized services for treating leg ulcers (UH and PAM), which attests to the importance of these services in the region.
The average age of the sample studied was 64 years, with a predominance of the population exceeding 60 years of age (59%). These results were found to be below the average determined by Nelzen et al.9 (Switzerland), in whose sample 85% were over the age of 64 years with a mean age of 76 years for women and 78 for men. By contrast, the results were similar to Scott et al.10 These difference are justified by different techniques used to collect data, in addition to socioeconomic, cultural and geographic differences characteristic of each sample.
Roughly 1% of the UK population is subject to chronic cutaneous ulcers, with increased prevalence among the elderly.11 With the demographic changes that have occurred in the present day to population of the developed countries,11 as well as in Brazil, geriatric diseases are expected to be more frequent in the medical routine, and among them leg ulcers.
The ratio between men and women was 1:1.9 This result is above the 1:1.4 ratio established by Scott et al,10 1which is probably associated with a younger population. It has already been reported that below the age of 60 years, the incidence of leg ulcers is greater in men (1.4:1), while above that age it is 1:1.2.10
Furthermore, most patients were observed to have a very low monthly income (R$84.00) for a family with 3.7 persons on average, 87% of them receiving low monthly wages (lower than the sum of three minimal wages).
An important finding was the association between chronic venous insufficiency and systemic arterial hypertension in 43.7% (p<0.01), which consists of an important association in the midst of factors that are predisposed to the appearance of leg ulcers. Such an association shows just how important it is to control and/or treat chronic venous insufficiency, in addition to treating arterial hypertension, diabetes and obesity.
All patients assessed were undergoing community care (at home or in health care centers), which is characteristically slow and costly. According to the clinical presentation, the ulcers were divided in: venous (79%), when accompanied by edema, ochre dermatitis, lipodermatosclerosis, varicose veins, eczema and pruritus; hypertensive (15.3%), when superficial, painful, necrotic, with erythematous borders and without hairs, in addition to an association with decompensated SAH; mixed (4.8%) when associating with or added to diabetes or others (0.9%), like neoplasms or hanseniasis. No cases of neuropathic ulcers for diabetes alone were found.
These results are similar to those published by Nelzen et al,12 Philips et al.,2 Callam et al.,13 Douglas et al.,6 Nelzen et al.,9 Trott14 and Benchikhi et al.,15 who found leg ulcers with a venous etiology in percentages ranging from 75 to 90% of cases. In addition to the venous category, these authors classified ulcers etiologically as arterial, neuropathic, or mixed. In this study, no cases of arterial ulcers were reported, though the hypertensive classification was added (Martorell's ulcer), whose etiology lies in alterations of the arterial walls. This condition determines ischemic processes in the dermal vessels, which was diagnosed in 15.6% of the sample. Indeed, it is relevant to report that the data agree with the low rate of neuropathic ulcers for diabetes and other causes.
The classification of ulcers was essentially based on clinical parameters that did not use more sophisticated tests, like photopletismography, duplex-scan and flebography, which improve the assessment of the limbs' vascular territory. This is a fact that might influence the frequencies of venous and arterial ulcers.
The signs and symptoms found in association with the ulcers confirmed the classification found. Its frequency is greater than 60% of the sample, like for example hyperchromia, lipodermatosclerosis, varicosity and edema, in addition to pruritus and eczema. All of them were related to chronic venous insufficiency, as suggested by Burton.16
With respect to ulcer localization, the present authors chose to adopt the zone scheme introduced by Baker et al.8 The majority of ulcers (73%) involved zone 2 alone, which was a lower result than what the authors found (84%). By summing the number of ulcers that involve zone 2 alone and those associated with other zones, the frequency of involvement for zone 2 reached 90%, which comes close to Baker's findings (90.1%). The number of patients with ulcers involving zones 1 and 2 simultaneously corresponded to 15%. This was greater than what Baker observed (3%). It is important to bear in mind that in his study Baker only assessed chronic venous ulcers.8
Many authors report that venous ulcers are commonly located on the medial face of the leg and ankle, following the vena saphena magna. In the present study, despite the fact that most of the ulcers are classified as venous, their localization was generally on the lateral face of the limb. This may be related to the high index of IVC and SAH association (43.7%) among the patients involved.
In assessing the ulcer measurements, roughly 80% of them were observed to fall under the medium and large categories. This represents greater physical, economic and cosmetic inconveniences for the patient.
As for ulcer chronicity, the average time of duration for an ulcer was 94 months, with roughly 73% of the sample (n=90) presenting open ulcers for more than a year. In 50% of them, it was a first episode of ulceration, and in the other half it was recurrence. Such results prove to be much greater than the average found by Baker8 in an epidemiological study on venous ulcers, which was 26 weeks (6.5 months). In the same study, the author reported that 24.4% of the sample consisted of a first ulceration episode, whereas Callam et al.,13 reported 33%, which was lower than the present study's finding (50%) in spite of the mean duration time being greater. As such, it may be observed that the treatment of leg ulcers requires longer treatment, which incurs clinical, functional and cosmetic inconveniences in these patients' quality of life, in addition to representing high operational costs for both the individual and public health service.
CONCLUSION
Leg ulcers, mainly those of the venous type, constitute an important aggravation to health in the cases analyzed in Juiz de Fora and surrounding regions. It is an infirmity with a long course and is recurrent. It is usually associated with other chronic infirmities, and essentially affects the elderly in the low income bracket. q
ACKNOWLEDGEMENT
Funding: Scientific Initiation Grant, Federal University of Juiz de Fora.
REFERENCES
Received on October 03, 2003.
Approved by the Consultive Council and accepted for publication on December 17, 2004.
- 1. Frade MAC, Gamonal AC, Carvalho MTF, Bastos SMC. Úlceras de perna. In: Gamonal AC. Dermatologia elementar- compêndio de dermatologia. Juiz de Fora; 2000. p.115-7.
- 2. Phillips TJ. Chronic Cutaneus Ulcers: Etiology and Epidemiology. J Invest Dermatol 1994; 102(supl): 38-41.
- 3. Phillips TJ, Dover JS. Leg Ulcers. J Am Acad Dermatol. 1991; 25:965-87.
- 4. Arnold F, West D. Angiogenesis in wound healing. Pharmac Ther. 1991; 52: 407-22.
- 5. Ministério da Saúde [sitio na internet]. Brasília: Informações de saúde-Datasus, [acessado em 18 de Novembro de 2004]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/popmg.def 2001
- 6. Douglas WS, Simpson NB. Guidlines for management of chronic venous leg ulceration. Br J Dermatol. 1995; 132:445-52.
- 7. Frade MAC, Valverde RV, Violante MR, Netto JC, Foss NT. Chronic phlebopatic skin ulcer: a therapeutic proposal. Int J Dermatol. 2001;40:237-40.
- 8. Baker SR, Stacey MC, Jopp-McKay AG, Hoskin SE, Thompson PJ. Epidemiology of chronic venous ulcers. Br J Surg. 1991; 78:864-7.
- 9. Nelzen O, Bergqvist D, Lindhagen A, Hallbook T. Chronic leg ulcers: na underestimated problem in primary health care among elderly patients. J Epidemiol Community Health. 1991; 45:184-7.
- 10. Scott TE, LaMorte WW, Gorin DR, Menzoian JO. Risk factors for chronic venous insufficiency: A dual case-control study. J Vasc Surg. 1995; 22:622-8.
- 11. Skene AI, Smith JM, Dore CJ, Charlett A, Lewis JD. Venous leg ulcers: a prognostic index to predict time to healing. BMJ. 1992; 305:1121-3.
- 12. Nelzén O, Bergvist D, Lindhagen A, HallBok T. Chronic leg ulcers etiology - a cross-sectional population study. J Vasc Surg. 1991; 14:557-64.
- 13. Callam MJ, Ruckley CV, Harper DR, Dale JJ. Chronic ulceration of the leg: extend of the problem and provision of care. Br Med J. 1985; 290:1855-6.
- 14. Trott A. Chronic skin ulcers. Emerg Med Clin North Am. 1992; 10:823-45.
- 15. Benchikhi H, Chiheb S, Khadir K, Lakhdar H. Les ulcčres de jambe prédominent chez l' homme au maroc. Ann Dermatol Venereol. 1998; 125:339-40.
- 16. Burton CS. Management of chronic and problem lower extremity wounds. Wound Healing. 1993; 11: 767-73.
Publication Dates
-
Publication in this collection
25 Nov 2005 -
Date of issue
Feb 2005
History
-
Accepted
17 Dec 2004 -
Received
03 Oct 2003