Abstract
We describe a case of plantar interdigital cutaneous melanoma in a 22-year-old woman who reported changes in a pigmented lesion during pregnancy. Diagnosis was late and evolution unfavourable. The purpose of this report is to draw the attention of dermatologists to the need for careful regular examination of melanocytic lesions in pregnant women, not ignoring possible changes as always physiological.
Melanoma; Neoplastic metastasis; Nevi and melanomas; Pigmented nevus; Pregnancy; Skin Neoplasm
Cutaneous melanoma incidence has increased in the last few decades over the world, including in Brazil.11. Naser N. Cutaneous melanoma: a 30-year-long epidemiological study conducted in a city in southern Brazil, from 1980-2009. An Bras Dermatol. 2011;86:932-41. It is also considered the commonest malignant tumour found during pregnancy, corresponding to 31% of all diagnosed malignant neoplasms.22. Stensheim H, Møller B, van Dijk T, Fosså SD. Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: A registry-based cohort study. J Clin Oncol. 2009;27:45-51. Recent studies have reported an approximately 3.3% incidence of melanoma during pregnancy in women between 16 and 49 years old.22. Stensheim H, Møller B, van Dijk T, Fosså SD. Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: A registry-based cohort study. J Clin Oncol. 2009;27:45-51.
In the last 50 years, non-controlled studies have suggested that hormonal factors may influence melanoma development, and consequently pregnancy may represent a higher risk of tumour development as well as a factor for unfavourable prognosis.33. Driscoll MS, Grant-Kels JM.. Nevi and melanoma in pregnancy. Dermatol Clin. 2006;24:199-204, vi. Current evidence has not confirmed this. Controlled studies have shown that, until now, oral contraceptives and hormone replacement therapy do not increase the risk of developing melanomas, nor do endogenous hormones. For this reason, pregnancy does not seem to influence the development or prognosis of the disease (when corrected by tumour thickness and location factors).44. Gupta A, Driscoll MS. Do hormones influence melanoma? Facts and controversies. Clin Dermatol. 2010;28:287-92.
Another important aspect is the relationship between pregnancy and Breslow index. Breslow thickness is the main prognosis factor in patients diagnosed with melanoma. Some studies have suggested that women with melanoma diagnosed during pregnancy tend to present thicker tumours. Although there is the hypothesis of the involvement of hormonal changes and growth factors present in pregnancy, the most probable explanation would be a delay in its diagnosis.55. Travers RL, Sober AJ, Berwick M, Mihm MC Jr, Barnhill RL, Duncan LM. Increased thickness of pregnancy-associated melanoma. Br J Dermatol. 1995;132:876-83.
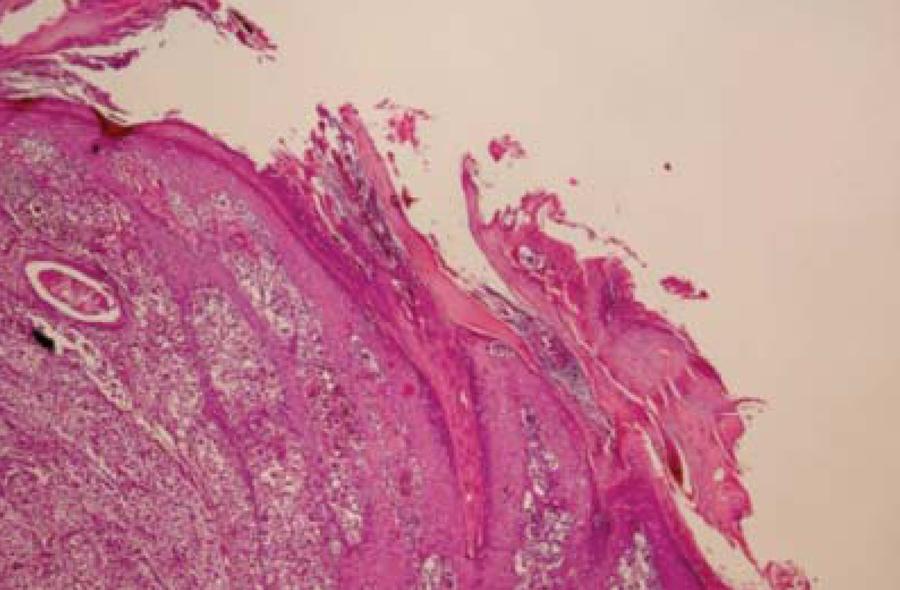
We describe a case of a 22 year old phototype II female, born and raised in São Paulo who reported a small dark brown mark in the third interdigital space of her right foot since birth. During her first pregnancy, she noted the mark increased in size and changed colour. At that time she was not examined for this dermatological complaint. Two years later, she sought dermatological evaluation, at which time an incisional biopsy was performed where the anatomical pathological findings were melanoma. At dermatological examination in our service, she presented a blackened plaque around the surgical ulceration (location of biopsy) in the third interdigital space of the right foot (Figures 1 and 2) and a painful palpable hardened mass on the root of right thigh measuring approximately 8 cm. Dermoscopy revealed a destructured lesion with areas of irregular multifocal pigmentation, coloured light brown, dark brown, black, and grey, as well as irregularly distributed brownish spots and globules and an amorphous grey-blue area. The centre presented a secondary scar area from a previous biopsy (Figure 3). Review of the slide confirmed diagnosis of superficial spreading melanoma with a nodular component, Breslow index 6.3mm, Clark level IV, presence of ulceration with 5.5 mm extension, 13 mitoses in 10 high power fields, angiolymphatic invasion, absence of regression, and vertical growth phase (Figures 4 and 5). Metastatic tracking in solid organs was negative. Their laboratory exams were normal (including lactate dehydrogenase). Its stage was IIIC in line with the American Joint Cancer Commission Staging of Melanoma.66. Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Atkins MB, Byrd DR, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27:6199-206. The lesion was treated surgically followed by local graft and draining of the right inguinal lymphatic chain. After 6 months, the patient evolved with cerebral and pulmonary metastases, quickly evolving to death.
Blackened plaque around the surgical ulcer in the third interdigital space of the right foot
Another angle of the lesion in the third interdigital space of the right foot, which gives a better view of the blackened area
Dermoscopy showing the destructured melanocytic lesion, irregular multifocal pigmentation with areas of light brown, dark brown, black, and grey, brown spots and globules with irregular distribution and an amorphous grey-blue area. The centre presents as an area of secondary scar tissue from a previous biopsy
Histology: superficial disseminative melanoma with a nodular component, noting in the epidermis adjacent to the nodule (to the right) epidermotropism until the granulosa layer. (HE 40x)
Histology: at higher magnification, note the intense nuclear atypia and mitotic figures. (HE 400x)
The relationship between pregnancy and melanocytic lesions has been discussed for many years. During pregnancy and exogenous hormone therapy, increased pigmentation is common in different areas of the body. Certain areas such as the mammary areole, armpits, genital region, and scar tissue are more prone to presenting increased pigmentation.77. Katz VL, Farmer RM, Dotters D. Focus on Primary Care: From Nevus to Neoplasm: Myths of Melanoma in Pregnancy. Obstet Gynecol Surv. 2002;57:112-9.
Although recent studies have shown that pregnancy does not seem to promote melanoma, some works indicated that melanocytic nevi can undergo changes during pregnancy.44. Gupta A, Driscoll MS. Do hormones influence melanoma? Facts and controversies. Clin Dermatol. 2010;28:287-92.,88. Gunduz K, Koltan S, Sahin MT, E Filiz E. Analysis of melanocytic naevi by dermoscopy during pregnancy. J Eur Acad Dermatol Venereol. 2003;17:349-51. For example, Zampino et al. followed melanocytic lesions in pregnant women and showed that during pregnancy some melanocytic nevi underwent dermoscopic changes. However, these changes were transitory and the pigmented lesions returned to their original colour after childbirth.99. Zampino MR, Corazza M, Costantino D, Mollica G, Virgili A. Are melanocytic nevi influenced by pregnancy? A dermoscopic evaluation. Dermatol Surg. 2006;32:1497-504.
Zalaudek et al. also showed that multiple dysplastic nevi (MDN) present alterations in diameter and colouration during pregnancy.1010. Zalaudek I, Wolf IH, Hofmann-Wellenhof R, Leinweber B, Di Stefani A, Argenziano G, et al. Dermatoscopic follow-up of a changing pigmented melanocytic skin lesion during pregnancy: from nevus to melanoma? Melanoma Res. 2004;14:323-5. However, the main question is whether these alterations correspond to a normal finding or to a condition which raises suspicion of a diagnosis of melanoma. For this reason, pregnant women who present MDN should receive clinical and dermoscopic follow up.1010. Zalaudek I, Wolf IH, Hofmann-Wellenhof R, Leinweber B, Di Stefani A, Argenziano G, et al. Dermatoscopic follow-up of a changing pigmented melanocytic skin lesion during pregnancy: from nevus to melanoma? Melanoma Res. 2004;14:323-5.
Probably in this case pregnancy may have precipitated the transformation of a congenital nevus into melanoma as the patient reported noticeable growth during pregnancy of a lesion present since birth.
The main objective of this report is to alert dermatologists to the need for careful examination of nevi and pigmented lesions during pregnancy. This case demonstrates that we must not interpret changes in these lesions as just being physiological. A biopsy should be immediately performed when a pigmented lesion changes dermoscopic character during pregnancy. This action could improve the early diagnosis and prognosis of primary cutaneous melanoma in these patients.
REFERENCES
-
1Naser N. Cutaneous melanoma: a 30-year-long epidemiological study conducted in a city in southern Brazil, from 1980-2009. An Bras Dermatol. 2011;86:932-41.
-
2Stensheim H, Møller B, van Dijk T, Fosså SD. Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: A registry-based cohort study. J Clin Oncol. 2009;27:45-51.
-
3Driscoll MS, Grant-Kels JM.. Nevi and melanoma in pregnancy. Dermatol Clin. 2006;24:199-204, vi.
-
4Gupta A, Driscoll MS. Do hormones influence melanoma? Facts and controversies. Clin Dermatol. 2010;28:287-92.
-
5Travers RL, Sober AJ, Berwick M, Mihm MC Jr, Barnhill RL, Duncan LM. Increased thickness of pregnancy-associated melanoma. Br J Dermatol. 1995;132:876-83.
-
6Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Atkins MB, Byrd DR, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27:6199-206.
-
7Katz VL, Farmer RM, Dotters D. Focus on Primary Care: From Nevus to Neoplasm: Myths of Melanoma in Pregnancy. Obstet Gynecol Surv. 2002;57:112-9.
-
8Gunduz K, Koltan S, Sahin MT, E Filiz E. Analysis of melanocytic naevi by dermoscopy during pregnancy. J Eur Acad Dermatol Venereol. 2003;17:349-51.
-
9Zampino MR, Corazza M, Costantino D, Mollica G, Virgili A. Are melanocytic nevi influenced by pregnancy? A dermoscopic evaluation. Dermatol Surg. 2006;32:1497-504.
-
10Zalaudek I, Wolf IH, Hofmann-Wellenhof R, Leinweber B, Di Stefani A, Argenziano G, et al. Dermatoscopic follow-up of a changing pigmented melanocytic skin lesion during pregnancy: from nevus to melanoma? Melanoma Res. 2004;14:323-5.
-
*
Work performed at the Department of Dermatology, Paulista School of Medicine - Federal University of São Paulo (EPM-UNIFESP) - São Paulo (SP), Brazil.
-
Financial funding: None
Publication Dates
-
Publication in this collection
Jan-Feb 2014
History
-
Received
11 Dec 2012 -
Accepted
04 Feb 2013