Abstracts
Langerhans cell histiocytosis is a rare disease of unknown cause, characterized by the proliferation of histiocytic cells (Langerhans cells). Its diagnosis is especially difficult due to its wide clinical spectrum, ranging from a single lesion to a multisystemic disorder. Diagnosis may be confirmed by means of an immunohistochemical study. Treatment depends upon the severity of the disease, and systemic chemotherapy may be needed.
Histiocytes; Histiocytosis; Langerhans-Cell
Histiocitose de células de Langerhans é uma doença rara de causa desconhecida, caracterizada pela proliferação de células histiocitárias (células de Langerhans). Representa significativa dificuldade diagnóstica por apresentar amplo espectro clínico, variando desde uma lesão solitária até uma enfermidade multissistêmica. Pode ser confirmada por estudo imunoistoquímico. O tratamento depende da extensão do processo, podendo ser necessária quimioterapia sistêmica.
Células de Langerhans; Histiócitos; Histiocitose
WHAT IS YOUR DIAGNOSIS?
IResident Physician in Dermatology at Faculdade de Medicina de Jundiai - Jundiai (SP), Brazil
IIResident Physician in Dermatology at Faculdade de Medicina de Jundiai - Jundiai (SP), Brazil
IIIPhysician specialized in Dermatology - Jundiai (SP), Brazil
IVVisiting Professor at the Dermatology Service at Faculdade de Medicina de Jundiai - Jundiai (SP), Brazil
VAssociate Professor at Faculdade de Medicina, Universidade de São Paulo. Postgraduate degree at New York University - New York (NY), United States of America. Full Professor of Dermatology at Faculdade de Medicina de Jundiai - Jundiai (SP), Brazil
Mailing Address
ABSTRACT
Langerhans cell histiocytosis is a rare disease of unknown cause, characterized by the proliferation of histiocytic cells (Langerhans cells). Its diagnosis is especially difficult due to its wide clinical spectrum, ranging from a single lesion to a multisystemic disorder. Diagnosis may be confirmed by means of an immunohistochemical study. Treatment depends upon the severity of the disease, and systemic chemotherapy may be needed.
Keywords: Histiocytes; Histiocytosis; Langerhans-Cell
HISTORY OF THE DISEASE
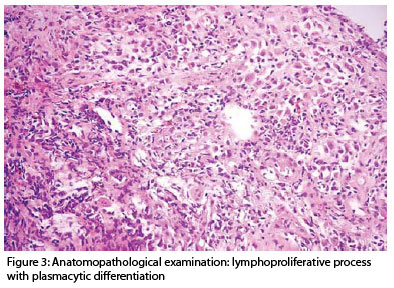
Male patient, 18 years old, smoker, with a history of painful wounds in the umbilical and anal region for eight months. The patient later noticed the appearance of new lesions in the oral cavity, ear, nose, and scalp. He also observed softening of teeth. Upon examination, the following were observed: erosions of hard palate (Figure 1) associated with periodontitis; exulcerated papules in the scalp, and erythematous exudative lesions in the external ear, right axilla, bilateral nasal fold, and anal region (Figure 2) with purulent exudate. Anatomopathological examination revealed a chronic suppurative inflammatory process, with fibrino leukocytic plug, plasmocytes, eosinophils, and histiocytic accumulation with discrete nuclear pleomorphism, suggesting lymphoproliferative process with plasmacytic differentiation (Figure 3). The immunohistochemical study was positive for protein S-100 and CD1a in neoplastic cells, being thus compatible with the standard pathology. Systemic disease investigation with a complete hemogram, hepatic function tests, abdominal ultrasonography, thoracic, cranial and mandibular radiography, and bone scintigraphy of the entire body did not show alterations. The patient initiated treatment with prednisone (80 mg/day) with partial improvement of lesions.
COMMENTARIES
Previously know as histiocytosis X, Langerhans cell histiocytosis (LCH) is classified today by the Histiocyte Society as class I histiocytosis, which is a group of clinical diseases characterized by reactive histiocytosis in which the predominant histiocytic cell type is of Langerhans cell phenotype. It is a reactive condition in which a population of cells with Langerhans phenotype accumulates in various tissues and causes damage. Its etiology is still unknown; however, several hypotheses have been considered, including immunological and viral etiology. Despite being a clonal process, most authors consider it a reactive, non-neoplastic disease. 1,2,4
Its incidence is estimated in 4-6/1000000, it rarely affects adults, and it is restricted to the skin. It can affect from one to several organs such as skin, bones and lymphonodes, with higher frequency. It may also affect the central nervous system, liver, spleen, lungs, gastrointestinal tract, thymus, endocrine glands, and bone marrow. The most characteristic presentation in the skin is the involvement of the scalp, being clinically similar to seborrheic dermatitis. In the trunk lesions can appear as yellowish or yellow-brown scaling papules and sometimes exposing areas of purpura. Lesions may become nodular, crostous or exulcerated. Ulcerations in folds, inguinal, perianal or vulvar region are common in adult patients.
Histologically, LCH is characterized by cells with irregular nuclei and abundant cytoplasm (Langerhans cells), and intense inflammatory cell infiltrate. The immunohistochemical study showed positivity for markers CD1a and S100 while electron microscopy indicated the presence of Birbeck granules, which are pathognomic.3
Prognosis varies according to the patient's age, extension of lesions, and failure of vital organ. Treatment depends upon the extension and severity of the disease. When restricted to the skin, treatment with nitrogenated mustard at 20% is effective.4 Oral administration of Psoralen combined with ultraviolet A radiation (PUVA) may be recommended in cases of failure or intolerance to topical nitrogenated mustard.5 New studies have shown positive results for treatment with Thalidomide. In multisystemic disease, with evidence of organic dysfunction, systemic chemotherapy is indicated.
REFERENCES
- 1. Aydogan K, Tunali S, Koran Karadogan S, Balaban Adim S, Turan H. Adult-onset Langerhans cell histiocytosis confined to the skin. J Eur Acad Dermatol Venereol. 2006;20:890-2.
- 2. Fabrini-Araújo PAF, Pimentel APS, Machado-Pinto J, Bueno-Neves L. Histiocitose de células de Langerhans - O papel do sistema imunológico na sua etiopatogenia. An Bras Dermatol. 1999;74:249-252.
- 3. Hashimoto K, Kagetsu N, Taniguchi Y, Weintraub R, Chapman-Winokur RL, Kasiborski A. Immunohistochemistry and electron microscopy in Langerhans cell histiocytosis confined to the skin. J Am Acad Dermatol. 1991;25:1044-53.
- 4. Wong E, Holden CA, Broadbent V, Atherton DJ. Histiocytosis X presenting as intertrigo and responding to topical nitrogen mustard. Clin Exp Dermatol. 1986;11:183-7.
- 5. Munn S, Chu AC. Langerhans cell histiocytosis of the skin. Hematol Oncol Clin North Am. 1998;12:269-86.
Case for diagnosis
Publication Dates
-
Publication in this collection
06 May 2010 -
Date of issue
Feb 2010