Abstracts
BACKGROUND: Chronic actinic cheilitis is actinic keratosis located on the vermilion border. Treatment is essential because of the potential for malignant transformation. OBJECTIVE: To evaluate the aesthetic and functional results of vermilionectomy using the classic and Wplasty techniques in actinic cheilitis. In the classic technique, the scar is linear and in the W-plasty one, it is a broken line. METHODS: 32 patients with clinical and histopathological diagnosis of actinic cheilitis were treated. Out of the 32 patients, 15 underwent the W-plasty technique and 17 underwent the classic one. We evaluated parameters such as scar retraction and functional changes. RESULTS: A statistically significant association between the technique used and scar retraction was found, which was positive when using the classic technique (p = 0.01 with Yates' correction). The odds ratio was calculated at 11.25, i.e., there was a greater chance of retraction in patients undergoing the classic technique. Both techniques revealed no functional changes. We evaluated postoperative complications such as the presence of crusts, dry lips, paresthesia, and suture dehiscence. There was no statistically significant association between complications and the technique used (p = 0.69). CONCLUSION: We concluded that vermilionectomy using the W-plasty technique shows better cosmetic results and similar complication rates.
Cheilitis; Photosensitivity disorders; Precancerous conditions
FUNDAMENTO: A queilite actínica crônica é a ceratose actínica localizada no vermelhão labial. O tratamento é de crucial importância, devido ao potencial de transformação maligna. OBJETIVO: Avaliar os resultados estéticos e funcionais das vermelhectomias clássica e em W-plastia na queilite actínica. Na técnica clássica, a cicatriz é linear; na W-plastia, em linha quebrada. MÉTODOS: Foram tratados 32 pacientes com diagnóstico clínico e histopatológico de queilite actínica. Quinze deles foram submetidos à técnica em W-plastia e 17, à técnica clássica. Avaliaram-se parâmetros como retração cicatricial e alterações funcionais. RESULTADOS: Houve associação estatisticamente significativa entre a técnica utilizada e a presença de retração cicatricial, sendo a associação positiva com a clássica (p=0,01 com correção de Yates). O risco relativo (odds ratio - OR) calculado foi de 11,25, ou seja, houve maior chance de retração nos pacientes submetidos à técnica clássica. Nenhuma das técnicas apresentou alterações funcionais. Avaliaram-se complicações pós-operatórias como presença de crostas, lábios secos, parestesia e deiscência de sutura. Não houve associação estatisticamente significante entre as complicações e a técnica utilizada (p=0,69). CONCLUSÃO: Concluiu-se que a vermelhectomia em W-plastia oferece melhores resultados estéticos e índices de complicações semelhantes.
Lesões pré-cancerosas; Queilite; Transtornos de fotossensibilidade
INVESTIGATION
ISpecialist in Plastic Surgery - Plastic Surgeon at the Dermatology Service, Padre Bento Hospital Complex - Guarulhos (São Paulo), Brazil
IIMSc in Pathological Anatomy, Federal University of São Paulo (UNIFESP) - Dermatopathologist at the Dermatology Service, Padre Bento Hospital Complex - Guarulhos (São Paulo), Brazil
IIIPhD in Clinical Medicine from the São Paulo State-Civil-Servant Hospital (Hospital do Servidor Público Estadual de São Paulo) - Director of the Dermatology Service, São Paulo State-Civil-Servant Hospital - São Paulo (SP), Brazil
IVPhD in Clinical Medicine from the São Paulo State-Civil-Servant Hospital - Director of the Dermatology Service, Padre Bento Hospital Complex - Guarulhos, São Paulo (SP), Brazil
Mailing address
ABSTRACT
BACKGROUND: Chronic actinic cheilitis is actinic keratosis located on the vermilion border. Treatment is essential because of the potential for malignant transformation.
OBJECTIVE: To evaluate the aesthetic and functional results of vermilionectomy using the classic and Wplasty techniques in actinic cheilitis. In the classic technique, the scar is linear and in the W-plasty one, it is a broken line.
METHODS: 32 patients with clinical and histopathological diagnosis of actinic cheilitis were treated. Out of the 32 patients, 15 underwent the W-plasty technique and 17 underwent the classic one. We evaluated parameters such as scar retraction and functional changes.
RESULTS: A statistically significant association between the technique used and scar retraction was found, which was positive when using the classic technique (p = 0.01 with Yates' correction). The odds ratio was calculated at 11.25, i.e., there was a greater chance of retraction in patients undergoing the classic technique. Both techniques revealed no functional changes. We evaluated postoperative complications such as the presence of crusts, dry lips, paresthesia, and suture dehiscence. There was no statistically significant association between complications and the technique used (p = 0.69).
CONCLUSION: We concluded that vermilionectomy using the W-plasty technique shows better cosmetic results and similar complication rates.
Keywords: Cheilitis; Photosensitivity disorders; Precancerous conditions
INTRODUCTION
Actinic cheilitis is also known as actinic keratosis of the lip. Its similarity with actinic keratosis of the skin lies in the etiology of both diseases, exposure to solar radiation and the possibility of development of squamous cell carcinoma. It is manifested through desiccation, erosion and loss of the lower lip border, affecting mainly light-skinned people. The main risk factors are: chronic exposure to sunlight, smoking and poor oral hygiene. 1
The relationship between lip cancer and sun exposure was described in 1923 by Ayres. The estimated time for the development of lip cancer is 20 to 30 years, but this time is shorter for some patients. Patients at risk of developing lip cancer are usually fair-skinned smokers who are older than 50 and have a history of sun exposure.2,3 Although metastases of squamous cell carcinoma of the skin derived from actinic keratosis are rare, this tumor results in metastasis in approximately 11% of the cases when on the lip. 1
Squamous cell carcinoma of the lip almost always develops in pre-existing lesions of actinic cheilitis. It affects the lower lip in more than 90% of the cases. Some signs of malignancy are hardened area, ulcer, persistent erythema and hyperkeratotic areas. Any of these changes indicate the need for biopsy. 4 Squamous cell carcinoma is the most common malignant neoplasia of the lip and represents about 15% to 40% of the cases of oral cancer. 5
Actinic cheilitis must be treated because of the risk of developing squamous cell carcinoma and the consequent potential for causing metastasis. 6 While squamous cell carcinoma of the lip causes metastasis in approximately 11% of the cases, the chances that this same tumor of the skin when derived from actinic keratosis develops into metastasis are less than 1%. 7
We describe various forms of treatment of actinic cheilitis: application of 5-fluorouracil, peeling with trichloroacetic acid 50%, electrosurgery, photodynamic therapy, CO2 laser, vermilionectomy, cryosurgery, and dermabrasion. 8
Vermilionectomy is an excellent alternative for treatment of actinic cheilitis, since it is easy to perform it and since it provides satisfactory aesthetic results according to several authors. 9
According to Spira and Hardy (1964), vermilionectomy was initially described by Bernard and Huette in 1869. Kwapis and Gibson described vermilionectomy in 1956 as excision of all or part of the vermilion of the lip, with mucosal advancement and its suture to the skin for closure of the defect. 10
Vermilionectomy is performed under local anesthesia, the whole vermilion of the lower lip is resected, without touching the orbicularis muscle. The mucosa is advanced toward the skin to be sutured and thus close the defect. Some postoperative complications are hematoma, suture dehiscence and hypoesthesia. 10
In vermilionectomy using the conventional technique, the scar that results from resection of the vermilion border is linear, which can lead to scar retraction and consequent unaesthetic scar. In order to avoid scar retraction, FERNANDEZ VOZMEDIANO, 1989, proposed the use of vermilionectomy forming a broken line, a technique called W-plasty, having published three cases involving this technique. 11
We propose a comparative study between the two techniques employed in vermilionectomy: classic and W-plasty, assessing the aesthetic results of these procedures.
CASUISTRY
This protocol was submitted to the Research Ethics Committees and approved on December 27, 2005 and December 20, 2004.
We selected 33 patients with at least one of the following clinical criteria for actinic cheilitis: desquamation, severe keratosis, erythema, atrophy, erosion, loss of clear demarcation between the vermilion border and the skin and infiltration on palpation.3 Given the relative rarity of the disease, there was no calculus to determine the sample of patients for this study.
The research participants underwent biopsy of the lip for histopathological confirmation of actinic cheilitis, characterized by the presence of nuclear atypia (hyperchromasia, karyomegaly) and architectural atypia (breakdown in the arrangement of keratinocytes) observed in the basal layer of the squamous epithelium. Those who met the clinical and histopathological criteria for actinic cheilitis were eligible to participate in the study.
Patients were alternately divided into two groups for surgical treatment, that is, for vermilionectomy in its two variants: classic and W-plasty. While the resulting scar is linear in vermilionectomy using the classic technique, it is a broken line in vermilionectomy employing W-plasty. The vermilion of the lip is surgically removed up to the muscle plane and the internal mucosa is externally advanced and sutured to the skin.
Standard preoperative examinations of the Dermatology Service, such as CBC, coagulation, glucose, urea, creatinine, and electrocardiogram, were performed to evaluate the clinical status of the patients to be included in this study.
The criteria for inclusion of participants in the study were the following: patients of both genders at any age or race with clinical and histopathologic diag-nosis of actinic cheilitis who had agreed to participate in the study and signed a consent form.
Exclusion criteria were pregnancy, clinical or laboratory evidence of immunosuppression or use of immunosuppressive drugs, presence of squamous cell carcinoma in preoperative histopathological examination, allergy to any substance to be used in surgery, decompensated diabetes mellitus, use of anticoagulant or acetylsalicylic acid up to 15 days before surgery, presence of any drug that (according to the investigator) could interfere with results, outbreak of herpes labialis, heart disease or any medical condition that contraindicates surgery of this magnitude, failure to attend the postoperative visit.
After histopathological confirmation of actinic cheilitis, patients were instructed about the need for treatment of this condition. Several forms of treatment available in the hospital were presented to the patients and surgical treatment was offered as an option, including the possibility of participating in this study.
We gave to those who agreed to participate in the study the forms for informed consent (IC) and photograph authorization (PA), explaining the objective of the study, risks and discomforts of the surgery and confidentiality of results. All of the patients who agreed to participate signed the IC and PA forms.
Data on history, histopathological and physical examination and laboratory results were recorded on standardized medical report forms (age, gender, race, occupation, history of sun exposure, skin type according to Fitzpatrick classification, tobacco use, used technique, duration of surgery, immediate or late postoperative complications). All of the participants had standardized detailed photos taken of their lips in the preoperative and postoperative periods of at least three months.
Outpatient surgeries were performed under local anesthesia using lidocaine hydrochloride 2% with adrenaline, absorbable 4-0 catgut sutures and antisepsis with povidone-iodine solution. Duration of the surgery was timed from the start of incision until the completion of the last suture in order to compare the two techniques.
In the classic technique with resulting linear scar, an ellipse with linear borders of the entire vermilion is marked. Resection of the vermilion of the lip is performed up to the muscles and sutured after careful hemostasis. The final suture and scar result in a straight line that runs the length of the lower lip (Figures 1 and 2). In the W-plasty technique, the anesthetic process is the same as the one used in the classic technique, however, the way the lip is previously marked is different. The lower lip is marked in the shape of an ellipse which runs the entire length of the lower lip, but with jagged edges. Resection of the ellipse of the vermilion also follows up to the muscles. This way, the resulting scar will be a broken line, a procedure called W-plasty (Figures 3 and 4).
In the postoperative period, all patients received prophylactic antibiotics with cephalexin 500 mg every 6 hours for seven days, in addition to dipyrone analgesic, as established at the Dermatology Service. All patients were instructed not to eat hot food in the first 24 hours.
The surgical specimens were subjected to histopathological examination.
The postoperative complications analyzed were infection, crusting, necrosis, paresthesia, and suture dehiscence, besides functionality in terms of suction and smiling.
Postoperative photographs were taken at least three months after surgery, and parameters such as functionality and aesthetic aspects as scar retraction that showed scarring of worse quality were analyzed. Scar retraction was classified according to the following criteria:
0 - No retraction (Figure 5).
1 - Mild retraction: discrete scar (Figure 6).
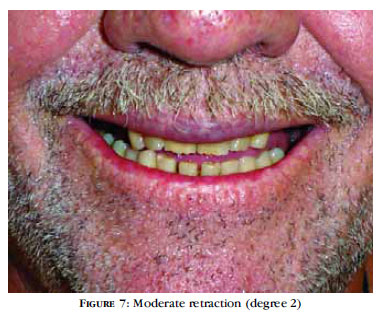
2 - Moderate retraction: clear scar (Figure 7).
3 - Severe retraction: scar showing contraction of surrounding tissues (Figure 8).
The results were analyzed using the program EPI INFO version 3.5.1.
The methods used were chi-square and Fisher's exact test. When a variable was less than 2, we used Fisher's exact test. Results were considered statistically significant if the p value was less than 0.05 (p <0.05).
RESULTS
Out of the 33 participants selected, 32 were analyzed and considered eligible for the study. One patient was excluded due to failure in the follow-up process. Of the 32 patients evaluated, 19 were female (59.4%) and 13 were male.
The distribution of the patients into W-plasty and classic groups was homogenous in relation to gender (p = 0.66 with Yates' correction).
The mean age of the participants was 63, with a median of 63.5 years old and mode of 65. The lowest age was 40 years old and the highest was 79. There was preponderance of patients in their 70s or 80s.
When we divided the patients into group undergoing W-plasty or group undergoing the classic technique, we observed no significant difference regarding age (p = 0.26, Fisher's exact test).
In relation to skin phototype, 31 patients (96%) out of 32 had skin phototype II, which prevented comparison between the two groups. Only one patient, who belonged to the W-plasty group, had skin phototype IV.
In terms of occupation, 18 patients were farmers (56.25%), followed by three construction workers (9.37%), three housewives (9.37%), a street vendor (3.12%), a cook (3.12%), a toolmaker (3.12%), a driver (3.12%), a clerk in the department of human resources (3.12%), a police officer (3.12%), a laundress (3.12%), and a security guard (3.12%).
Among the 32 patients evaluated, 17 (53.1%) reported being smokers, and their distribution was similar between the two groups.
The mean time of sun exposure was 30.78 years, a median of 30 years and mode of 30.
Regarding the results of the proposed treatment options, we chose to analyze the presence of scar retraction in the late postoperative period (more than three months later). Functional evaluation in relation to smiling and suction was also analyzed, but none of the groups showed any changes. Thus, the major differences found were those concerning degree of scar retraction in the late postoperative period. As shown in the methods section, retraction was classified into 4 degrees (Figures 5 to 8) to facilitate statistical analysis. In this respect, there was a predominance of moderate to severe retraction in the group that underwent surgery with the classic technique and no retraction to mild retraction in the group that underwent W-plasty (Table 1).
There was a statistically significant association between absence of retraction and W-plasty (p = 0.002).
For better statistical analysis, we divided the results into presence and absence of retraction, regardless of degree.
This way, we also found a statistically significant association between degree of scar retraction and technique used, with positive association with the classic technique (p = 0.01 with Yates' correction). The odds ratio (OR) was 11.25, that is, there was a greater chance of retraction in patients undergoing the classic technique (Table 2).
To evaluate the confounding variables, we analyzed the presence of retraction in relation to gender, age, smoking and sun exposure.
The presence of scar retraction after surgery was not statistically associated with gender (p = 0.45, Fisher's exact test).
With regard to age, for purposes of statistical analysis, we separated the patients into two groups, that is, up to 60 years old and older, according to the Statute of the Elderly, Law No. 10741 of October 1, 2003, which considers 60 the age limit for appointment of the elderly in our country.
The presence of scar retraction after surgery was not statistically associated with age (p = 0.42, Fisher's exact test).
There was no association between smoking and presence of retraction (p = 0.79 with Yates's correction).
Due to the high variability found in both groups, it was not possible to analyze the relationship between duration of sun exposure and scar retraction.
The average duration of surgery with the classic technique was 19.6 minutes and 21.6 minutes with the W-plasty technique, which demonstrates that the use of W-plasty does not present technical difficulty statistically higher than that presented by the classic technique.
The histopathological results of the surgical specimens confirm the focal presence of squamous cell carcinoma superficially invasive in two cases (6.25%) and basal cell carcinoma in 1 case (3.12%), demonstrating the need for analysis of the complete surgical specimen for higher accuracy of diagnosis.
The complications analyzed were dry lips, paresthesia, crusts and suture dehiscence. Concerning the participants who underwent W-plasty, dry lip sensation was present in 2 cases (13.4%) and paresthesia was present in 5 cases (33.3%). In the classic technique, dry lips occurred in 2 cases (11.8%), paresthesia occurred in 4 cases (23.5%) and dehiscence was present in 2 (11.8%).
We also analyzed presence or absence of complications, regardless of the type, and presence or absence of retraction. We noted that there was no association between the technique used and presence of complications based on the chi-square method (p = 0.69).
With the exception of paresthesia, which tended to persist for long periods of time with both techniques, all other complications were completely resolved.
There was paresthesia in both groups (W-plasty, 5 cases; classic, 4 cases); this difference was not statistically significant when using the chi-square test (p = 0.69).
The duration of postoperative follow-up ranged from three to 42 months in both groups, with a mean of 19 months.
DISCUSSION
This study compared the functional and aesthetic results of vermilionectomy using the classic and W-plasty techniques. We evaluated the degree of scar retraction that showed scarring of worse quality and complications such as paresthesia, suture dehiscence, presence of crusts and dry lips.
Although various therapeutic techniques such as application of 5-fluorouracil, "peeling" with trichloroacetic acid, cryosurgery, electrodissection and curettage, dermabrasian, photodynamic therapy and CO2 laser have been described, 12, 13 they do not provide histopathological substrate for analysis of the whole surgical specimen. In addition to its high efficacy, complete removal of the lip vermilion facilitates the diagnosis of incipient squamous cell carcinoma.
We found a higher incidence of females (59.4%), which differed from most previous work, in which there was a predominance of males. 1, 2 However, AGUIAR (1995) and OLIVEIRA FILHO (1998) reported an equal incidence of the two genders, just like our study. This can be explained by the high number of women working in agriculture in our country. 3
The predominant age groups were the seventies and eighties. These data are similar to those found by OLIVEIRA FILHO (1998).
According to ZELICKSON, ROENIGK (1990), it takes actinic cheilitis 20 to 30 years to evolve into squamous cell carcinoma; this justifies the mean age in our sample. We consider time of sun exposure important for the development of actinic cheilitis.
As for skin phototype, 96% of the patients were phototype II in accordance with Fitzpatrick classification and only one was skin phototype IV, which is consistent with the literature. 14
The predominant occupation was farmer (56.25% of the cases), which corroborated the literature, according to which actinic cheilitis affects people who were exposed to solar radiation. 3, 12, 13, 15, 16, 17
Tobacco use was present in 53.1% of the cases in this study. In the literature, the data vary regarding the association of tobacco use and actinic cheilitis. In a study of 20 patients, OLIVEIRA FILHO (1998) found a similar incidence, 55%, which differs from Aguiar (1995), who found only 15.9%. Other authors have reported the association with smoking, but without mentioning percentages. 12, 18, 19 Since it is carcinogen, we believe that tobacco also contributes to the development of actinic cheilitis.
We selected vermilionectomy as the treatment option for actinic cheilitis because it is a rapid method, with short-term postoperative recovery, low complication rates and effective prophylaxis of lip squamous cell carcinoma, which can cause cervical metastasis in 11% of the cases.1,20
This procedure can be performed under local anesthesia in an outpatient manner and with very satisfactory aesthetic results. The operated area is closed through mucosal advancement toward the skin. 21 In our study, all vermilionectomies were performed in an outpatient setting under local anesthesia and with closure by advancement of the mucosa up to the skin, with good results.
The vermelionectomies were performed using two techniques: the classic, which leaves a linear scar and is more often described in the literature, and the W-plasty technique, which is described in only one study and involving a small number of individuals, whose resulting scar in a broken line offers superior aesthetic results compared to the technique previously described.9, 10, 11 ,21, 22, 23, 24, 25, 26 In accordance with Vozmediano and our opinion, this scar in a broken line is more distensible and thus does not affect the movement of the mouth. 11
The main result analyzed was presence of scar retraction in the late postoperative period (later than three months). Unaesthetic scars and paresthesias are the main criticisms of the use of vermilionectomy.16, 27 Other authors have described irritation of the upper lip, reversed growth of the beard of the lower lip, prolonged hematoma, swelling and erythema as complications of vermelionectomy. 15, 16 In our study, we did not find such complications. Despite varying degrees of scar retraction found in some of our patients, we believe that this is an excellent method for the treatment of actinic cheilitis, since it offers complete removal of the vermilion and histopathological examination of the surgical specimen, allowing the verification of the presence of malignancy.
In relation to the techniques used, moderate and severe scar retraction, accountable for results aesthetically inferior, were present mainly in the classic technique (12 patients, 70.6%, table 1). In W-plasty, scar retraction tended to be mild or absent, with moderate and severe retraction being less observed (1 patient, 6.6%, table 1). Thus, we observed that there was better tissue accommodation in W-plasty, with superior aesthetic results.
When we subdivided the patients into groups with or without scar retraction, regardless of degree, there was a statistically significant association between the technique used and presence of retraction, and the association with the classic technique was positive (p = 0.01 with Yates' correction, table 2). The odds ratio was calculated at 11.25, i.e., the chance of developing scar retraction in the classic technique was 11.25 times greater than that in W-plasty. Of the patients who underwent the W-plasty technique, 60% had invisible scar (no retraction), whereas only 11.8% had scars of this nature in the classic technique. We did not find any studies comparing the two techniques in the literature; only one author, FERNANDEZ VOZMEDIANO, 1989, described vermilionectomy using the W-plasty technique as an option to obtain better functional and aesthetic results. In the W-plasty technique, the resulting scar in a broken line allows the scar to become more distensible, avoiding scar retraction. In the classic technique, the scar in a straight line may cause retraction and difficulties in smiling and sucking. 11 This author studied only three patients and did not do a comparative study between the techniques. In our study, we did not find any patient with difficulty in smiling or sucking in any of the two groups, but the presence of scar retraction was greater with the classic technique.
SANCHEZ-CONEJO-MIR (1986) studied 52 patients with actinic cheilitis who were submitted to vermilionectomy using the classic technique. There was histopathological confirmation of squamous cell carcinoma in 13.4% of the cases, similar to our data of 6.25% of squamous cell carcinoma and 3.12% of basal cell carcinoma. We tried to correlate presence of scar retraction with other variables such as gender, age, tobacco use and time of sun exposure regardless of the technique.
There was no association between scar retraction and gender (p = 0.45, Fisher's exact test).
Regarding age, we separated the patients into two groups for purposes of statistical analysis: up to sixty and older. There was no association between presence of scar retraction and patients considered elderly or not, p = 0.42.
Smoking also showed no statistically significant association with scar retraction, p = 0.79. In the literature, smoking was associated with actinic cheilitis itself, and there are no reports regarding its influence on surgical results.
As for sun exposure, there was random distribution between time of sun exposure and scar retraction, which did not allow statistical analysis.
The average duration of surgery was 19.6 minutes in the classic technique and 21.6 minutes in the W-plasty one. There was no significant difference in terms of duration of surgery between the two techniques, which justifies the use of the W-plasty technique, since it offers better cosmetic results and the same rates of complications.
Distribution of complications between both techniques occurred at random. The main ones were presence of crusts, dry lips, paresthesia and suture dehiscence. There was no statistically significant association between presence of complications and the technique used, p = 0.69. With the exception of paresthesia, which tended to persist for long periods of time, all other complications were completely resolved. The presence of paresthesia was also not associated with the technique used, p = 0.69.
Actinic cheilitis is a premalignant skin condition that can develop into invasive squamous cell carcino-ma and cause metastasis of the cervical lymph nodes, and therefore, it should be treated in an incisive manner. Among the several different therapeutic alternatives found in the literature, such as application of 5fluorouracil, chemical peeling with trichloroacetic acid 50%, imiquimod 5%, cryosurgery, photodynamic therapy, and CO2 laser, we believe that vermilionectomy is the treatment of choice for allowing complete removal of the vermilion border and histopathological examination of surgical specimen. 28 Our comparative study of the two techniques employed in vermilionectomy, classic (with linear scar) and W-plasty (with scar in a broken line), showed that the latter has much better aesthetic results than the first. This technique can be performed under local anesthesia in an outpatient setting, with surgery duration and complication rates very similar to those observed in the classic technique.
CONCLUSION
The analysis of treatment of the 32 patients with actinic cheilitis who were submitted to vermilionectomy using the classic or W-plasty techniques showed:
1. There was a statistically significant association between the technique used and presence of scar retraction, with the association with the classic technique being positive (p = 0.01 with Yates' correction). The odds ratio (OR) was calculated at 11.25, i.e., there was a greater chance of retraction in patients undergoing the classic technique.
The odds ratio (OR) can lead to distortions due to incomplete sampling design, which is implicit in case-control studies. Thus, a limitation of this study was the estimate presented by the odds ratio (OR).
2. There was no statistically significant association between postoperative complications (presence of crusts, dry lips, paresthesia and suture dehiscence) and the technique used, p = 0.69.
3. The W-plasty technique offered superior cosmetic results compared to the classic one, with similar technical difficulty and complication rates.
4. There was no functional change in any of the techniques used.
REFERENCES
-
1Picascia DD, Robinson JK. Actinic cheilitis: A review of the etiology, differential diagnosis, and treatment. J Am Acad Dermatol. 1987;17:255-63.
-
2Cataldo E, Doku HC. Solar cheilitis. J Dermatol Surg Oncol. 1981;7:989-95.
-
3Aguiar SM. Contribuição ao estudo da queilite actínica: correlação anátomoclínica [Tese]. São Paulo: Faculdade de Medicina da Universidade de São Paulo; 1995.
-
4Main JHP, Pavone M. Actinic cheilitis and carcinoma of the lip. J Can Dent Assoc. 1994;60:113-6.
-
5Pires RF, Bueno RH, Alves FA, Almeida OP. Queilite actínica: Aspectos clínicos e preventivos. Rev Assoc Paul Cir Dent. 2001;55:200-3.
-
6Sanchez-Conejo-Mir J, Peres Bernal AM, Moreno-Gimenez JC, Camacho-Martinez F. Follow up of vemilionectomies: Evaluation of the technique . J Dermatol Surg Oncol. 1986;12:180-4.
-
7Robinson JK. Actinic cheilitis. A prospective study comparing four treatment methods. Arch Otolaryngol Head Neck Surg. 1989;115:848-52.
-
8Ishida CE, Ramos-e-Silva M. Cryosurgery in oral lesions. Int J Dermatol. 1998;37:283-5.
-
9Kurth ME. "Lip Shave" or vermilionectomy: Indications and technique. Br J Plast Surg. 1957;10:156-62.
-
10Spira M, Hardy B. Vermilionectomy. Review of cases with variations in technique. Plast Reconstr Surg. 1964;33:39-46.
-
11Fernandez Vozmediano JM, Romero Cabrera MA, Carrascosa Cerquero A. Vermilionectomy using the Wplasty technique. J Dermatol Oncol. 1989;15:627-9.
-
12Stanley RJ, Roenigk RK. Actinic cheilitis: Treatment with the carbon dioxide LASER. Mayo Clin Proc. 1988;63:230-5.
-
13Whitaker DC. Microscopically proven cure of actinic cheilitis by CO2 LASER. Lasers Surg Med. 1987;7:520-3.
-
14Oliveira Filho J. Queilite actínica: avaliação clínica, histopatológica e histoquímica do tratamento com LASER de CO2 [Tese]. São Paulo: Faculdade de Medicina da universidade de São Paulo; 1998.
-
15Zelickson BD, Roenigk RK. Actinic cheilitis. Treatment with the carbon dioxide LASER. Cancer. 1990;65:1307-11.
-
16Dufresne RG, Cruz AP, Zeikus P,Perlis C, Jellinek J. Dermabrasion for actinic cheilitis. Dermatol Surg. 2008;34:848-50.
-
17Cavalcante ASR, Anbinder AL, Carvalho YR. Actinic cheilitis: clinical and histological features. J Oral Maxillofac. 2008;3:498-503.
-
18Lindqvist C, Tempo L. Epidemiological evaluation of sunlight as a risk factor of lip cancer. Br J Cancer. 1978;37:983-9.
-
19Sheinberg RS. Carbon dioxide LASER treatment. Actinic cheilitis. West J Med. 1992;156:192-3.
-
20Johnson TM, Sebastien TS, Lowe L, Nelson BR. Carbon dioxide LASER treatment of actinic cheilitis. J Am Acad Dermatol. 1992;27:737-40.
-
21Kurul S, Uzunismail A, Kizir A. Total vermilionectomy; indications and technique. Euro J Surg Oncol. 1995;21:201-3.
-
22Burket J. Vemilionectomy for lower lip leucoplakia. Arch Derm. 1967;95:397-9.
-
23Marchac D, Dufourmentel C. Les états précancéreux du vermillon de la lèvre inférieure intérêt de la vermillonectomie préventive. J FR Otorhinolaryngol audiophonol chir maxill. 1971;20:1029-32.
-
24Rayner CR, Arscott GD. A new method of resurfacing the lip. Br J Plast Surg. 1987;40:454-8.
-
25Field LM. An improved design for vermilionectomy with a mucous-membrane advancement flap. J Dermatol Surg Oncol. 1991;17:833-4.
-
26Lustig J, Librus H, Neder A. Bipedicled myomucosal flap for reconstruction of the lip after vemilionectomy. Oral Surg Med Oral Pathol. 1994;77:594-7.
-
27Neder A, Nahlieli O, Kaplan I. CO2 Laser used in surgical treatment of actinic cheilitis. J Clin Laser Med Surg. 1992;10:373-5.
-
28Felício LBA, Ferreira J, Bently MVB, Bagnato VS, Tedesco CA, Souza CS. A terapia fotodinâmica com ácido 5 - aminolevulínico como modalidade de tratamento para neoplasias cutâneas não melanoma. An. Bras. Dermatol. 2008;83:309-16.
Actinic cheilitis: aesthetic and functional comparative evaluation of vermilionectomy using the classic and W-plasty techniques
Publication Dates
-
Publication in this collection
21 Mar 2011 -
Date of issue
Feb 2011
History
-
Received
11 Nov 2009 -
Accepted
16 Dec 2010