Abstracts
PURPOSE: To analyze mortality (7 days) or graft loss in liver transplantation (Tx) performed within the Awakening Protocol (AP) compared to sequential Tx. METHODS: Analysis of 243 liver tx (230 patients), divided into sequential tx or PD (early morning) to compare graft loss or death (7 days). Significant differences at p <0.05 RESULTS: The PD was adopted in 32.5% of tx. The cold ischemia time (p <0.01) and the interval until transplantation (p <0.01) were significantly different. Age of the donor and recipient, Donor Risk Index, MELD score, and donor base excess, sodium, creatinine and glucose were not different between groups. Previous abdominal surgery was a risk factor for early mortality, but was equally distributed between the groups. There was no difference in mortality or graft loss within 7 days (p = 0.521) CONCLUSION: The adoption of PD, to start tx the morning when harvesting occurs after 10p.m. did not result in worse patient and graft survival. Transplant patients with fulminant hepatic failure and high-risk grafts do not apply to this surgical tactics.
Liver transplantation; Surgical procedures; Operative; Organ transplantation; Liver transplantation; Method
OBJETIVO: Analisar a mortalidade (7 dias) ou perda do enxerto em tx de fígado realizado dentro do Protocolo Despertar (PD), em comparação ao tx realizado de maneira sequencial. MÉTODOS: Análise retrospectiva de 243 tx de fígado (230 pacientes), divididos em tx sequencial ou PD (inicio pela manhã). Foram comparados mortalidade ou perda do enxerto (7 dias). Diferenças significantes para p<0,05. RESULTADOS: O PD foi adotado em 32,5% dos tx. O TIF (p<0,01) e o intervalo até o início do transplante (p<0,01) foram significativamente diferentes. Idade do doador e do receptor, Donor Risk Index, escore MELD, Base excess do doador, sódio, creatinina e glicemia do doador não foram diferentes entre os grupos. Antecedentes cirúrgicos abdominais foram fatores de risco para mortalidade precoce, mas estavam distribuídos igualmente entre os grupos. Não houve diferença na mortalidade ou na perda do enxerto em até 7 dias (p=0,521) CONCLUSÃO: A adoção do PD, para inicio do tx pela manhã, quando a captação ocorre após 22:00 h não acarretou piora na sobrevida dos pacientes. Transplante de pacientes com hepatite fulminante e enxertos de alto risco não se aplicam a esta tática cirúrgica.
Transplante de fígado; Procedimentos cirúrgicos operatórios; Transplante de órgãos; Transplante de fígado; Técnica
13 - ORIGINAL ARTICLE
TRANSPLANTATION
Effect of "the Awakening Protocol" in the outcome of liver transplantation1, 1 Research performed at the Transplant Group, Alfa Institute of Gastroenterology. Clinics Hospital, Federal University of Minas Gerais. Belo Horizonte-MG, Brazil. 2 2 Winner of "Silvano Raia Prize", for best paper presented at the VII Congresso Brasileiro de Transplante de Fígado, Pâncreas e Intestino Delgado, 2012.
Efeito do "Protocolo Despertar" no resultado do transplante de fígado
Agnaldo Soares LimaI; Leandro Ricardo de Navarro AmadoII; Malvina Maria de Freitas DuarteIII; Marcelo Dias SanchesIV; Alexandre Prado de ResendeII; João Ricardo Miranda ZocratoII; Maria Eva Costa ZocratoII
IPhD, Associate Professor, Department of Surgery, Faculty of Medicine of Federal University of Minas Gerais (UFMG). Head of Liver Transplant Unit. Transplant Surgeon of the Alfa Institute of Gastroenterology (IAG), Hospital of Clinics /UFMG, Brazil. Conception, design, scientific content of the study, technical procedures, analysis and interpretation of data, manuscript writing
IITransplant Surgeon, IAG. Hospital of Clinics /UFMG. Involved in surgical procedures, acquisition and interpretation of data
IIIMSc, Coordinator of Nursing Transplant Team, IAG. Involved with technical procedures
IVPhD, Associate Professor, Department of Surgery, Faculty of Medicine of UFMG. Transplant Surgeon of the IAG, Hospital of Clinics /UFMG. Involved with technical procedures, acquisition and interpretation of data
Correspondence Correspondence Agnaldo Soares Lima Av. Alfredo Balena, 189/1405 30130-100 - Belo Horizonte, MG Tel/Fax: (55 31)3274-6852 agnaldo@gold.com.br
ABSTRACT
PURPOSE: To analyze mortality (7 days) or graft loss in liver transplantation (Tx) performed within the Awakening Protocol (AP) compared to sequential Tx.
METHODS: Analysis of 243 liver tx (230 patients), divided into sequential tx or PD (early morning) to compare graft loss or death (7 days). Significant differences at p <0.05
RESULTS: The PD was adopted in 32.5% of tx. The cold ischemia time (p <0.01) and the interval until transplantation (p <0.01) were significantly different. Age of the donor and recipient, Donor Risk Index, MELD score, and donor base excess, sodium, creatinine and glucose were not different between groups. Previous abdominal surgery was a risk factor for early mortality, but was equally distributed between the groups. There was no difference in mortality or graft loss within 7 days (p = 0.521)
CONCLUSION: The adoption of PD, to start tx the morning when harvesting occurs after 10p.m. did not result in worse patient and graft survival. Transplant patients with fulminant hepatic failure and high-risk grafts do not apply to this surgical tactics.
Key words: Liver transplantation. Surgical procedures. Operative. Organ transplantation. Liver transplantation. Method.
RESUMO
OBJETIVO: Analisar a mortalidade (7 dias) ou perda do enxerto em tx de fígado realizado dentro do Protocolo Despertar (PD), em comparação ao tx realizado de maneira sequencial.
MÉTODOS: Análise retrospectiva de 243 tx de fígado (230 pacientes), divididos em tx sequencial ou PD (inicio pela manhã). Foram comparados mortalidade ou perda do enxerto (7 dias). Diferenças significantes para p<0,05.
RESULTADOS: O PD foi adotado em 32,5% dos tx. O TIF (p<0,01) e o intervalo até o início do transplante (p<0,01) foram significativamente diferentes. Idade do doador e do receptor, Donor Risk Index, escore MELD, Base excess do doador, sódio, creatinina e glicemia do doador não foram diferentes entre os grupos. Antecedentes cirúrgicos abdominais foram fatores de risco para mortalidade precoce, mas estavam distribuídos igualmente entre os grupos. Não houve diferença na mortalidade ou na perda do enxerto em até 7 dias (p=0,521)
CONCLUSÃO: A adoção do PD, para inicio do tx pela manhã, quando a captação ocorre após 22:00 h não acarretou piora na sobrevida dos pacientes. Transplante de pacientes com hepatite fulminante e enxertos de alto risco não se aplicam a esta tática cirúrgica.
Descritores: Transplante de fígado. Procedimentos cirúrgicos operatórios. Transplante de órgãos. Transplante de fígado. Técnica.
Introduction
Liver Transplantation (Tx) is a procedure performed on an emergency basis owing to the need to keep short the cold ischemia time (CIT). Until the late 1970s only the Collins and Euro-Collins solutions were available for hepatic graft preservation, which could not allow CIT longer than 4 to 6 hours. With the development of new preservation solutions suitable preservation could be guaranteed for CIT equal to or longer than 12 hours1,2. The extension of the CIT was beneficial to provide an appropriate length of time to prepare the institution for the transplant, to transport organs and candidates from great distances. The transformation of the transplant into a semi-elective procedure, scheduled to start in the morning, could be an additional gain from a prolonged CIT. The advantage associated with this tactic would be linked to better performance of the surgical team when it operates after a period of nightly resting. Furthermore, in most transplant institutions, infrastructure resource is largely available is during the day.
Prolonged cold ischemia time is associated to the risk of primary non-function or delayed graft function3. Graft impairment by steatosis or poor systemic condition of the donor may result in a worse outcome, even within a conventional period of ischemia4. Furthermore, recipient situations, such as fulminant hepatitis or the need for re-transplantation of a non-functioning graft, require intervention as soon as possible.
At the Hospital das Clínicas of Universidade Federal de Minas Gerais (UFMG), when graft harvesting starts after 10:00pm, the tx is scheduled to beginning the next day at 06:00am, constituting the so-called "Awakening Protocol". The present study analyzed the initial graft survival (first 7 postoperative days) of patients undergoing liver tx within the "Awakening Protocol", compared with patients whose operation was started sequentially.
Methods
All liver transplants performed at the Hospital of UFMG, from January 2009 to July 2012, were included in this study in a retrospective assessment. Data on demographic characteristics of donors and recipients, and clinical, laboratory and outcome after transplantation were obtained electronically through the transplant management system Zeus. Data handling respected the confidentiality of patient information in accord with the Helsinki Declaration of 1975. The score of the Model for Endstage Liver Disease (MELD) and Donor Risk Index (DRI) were calculated from data of recipients and donors, respectively. All variables were tested as a risk factor for mortality within 7 days postoperatively. Then, patients were divided into two groups: transplantation sequentially, when transplantation was performed immediately after harvesting of the graft and "Awakening Protocol", when harvesting was performed at night after 10:00p.m. and transplantation started in the morning at 06:00a.m. The two groups were compared for the incidence of risk factors for mortality or graft loss within 7 days postoperatively. Statistical test of Mann-Whitney, Student's t, chi-square and Kaplan Meier were applied according to the characteristics of the variables analyzed. Differences were considered significant when the p value was <0.05
Results
Two hundred and forty-three donor-recipient pairs were included in the analysis. In thirteen, the operation was a re-transplantation. Donors were young (35.6 ± 14.1 years), and 59.3% male. Ethanolic cirrhosis (24.3%), virus C cirrhosis (18.9%) and cryptogenic cirrhosis (16.9%) were the main indications for transplantation. In 19.8% of cases there was association of diseases in transplant indication, the most frequent the combination of hepatocellular carcinoma on chronic hepatitis C viral infection (6.2%) or ethanolic cirrhosis (4.5%). Donors were victims of craniocerebral trauma (45.9%) and stroke (43.3%). The event that caused the brain death occurred four days before the removal of organs (between 1 and 33 days). The preservation solutions used in the perfusion of the grafts were Custodiol® (41.7%), Viaspan® (38.8%), Celsior® (12.7%) and IGL1® (6.8%).
In about 60% of the cases, organ harvesting occurred in a hospital in the same region of the transplant center. Donor operation occurred during the day (until 06:00p.m.) in 51.9% of cases and the transplant was daytime in 55.6% of cases. The median DRI was calculated at 1.32. During the donor operation the macroscopic appearance of the graft was judged by the surgeon as normal (77%), mildly steatotic (8.6%), moderately steatotic (9.5%) or severely steatotic (0.4%). The median time from onset of ischemic period and the beginning of transplant operation was 315.5 minutes. The median age of recipients was 52.5 years. Receivers were male in 67.5%. The matching for sex between donor and recipient showed frequency of 40.7% for the combination MM (male donor, male recipient), followed by combinations MF (26.7%), FM (18.5%) and FF (14%). The median MELD score was 20, ranging from 9 to 49. The general characteristics of the patients are shown in Table 1.
The Awakening Protocol was adopted in 79 cases (32.5%). In the other 164 cases (67.5%), transplantation was done sequentially, shortly after the liver harvesting from the donor.
Some transplant patients had previous surgery on the biliary tract (10.3%), for treatment of portal hypertension (11.5%), hepatectomy (9.1%) or cholecystectomy (16.5%). The occurrence of previous operations on the abdomen and the ischemia time longer than 12 hours were associated with higher mortality or early graft loss after transplantation. The organ procurement at distance did not influence early graft or patient survival (p = 0.481). However, the macroscopic appearance of the liver (judged by the surgeon) concerning the intensity of steatosis showed a trend (p = 0.054) to determine graft loss within 7 days. The adoption of the Awakening Protocol to determine the start of the transplantation procedure was not a determinant of early mortality or graft loss after transplantation. Univariate analysis of risk factors for mortality or loss of the transplanted liver within a week after surgery is shown in Table 2.
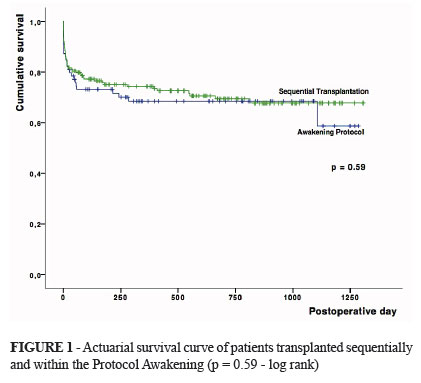
The incidence of factors identified as risk for graft loss or death within 7 days was compared in groups of sequential transplant and Awakening Protocol. The frequency of these factors was similar between the two groups (Table 3), The actuarial survival of the two groups is illustrated in Figure 1
Discussion
The surgical procedure for liver transplantation has undergone significant evolution over the years becoming a more simple operation than practiced in its beginnings. Nevertheless, the operation still remains one of the largest and most complex practiced in the abdominal cavity. The severity of the act lies in the set of massive resection in debilitated patients with portal hypertension and coagulopathy. Furthermore, resection of the diseased liver is followed by multiple anastomoses, including blood vessels and bile duct, all harboring a potential of serious complications.
Achieving success in liver transplant requires not only technical perfection, but also domain over factors related to the donor and the recipient. Some factors derogatory to the results of transplantation are associated with the liver disease that led to transplantation or to the systemic condition of the receiver. On the other hand, other important elements are dependent on the acceptance of donor characteristics, like age, biochemical profile, and morphological aspects of the graft or systemic condition of the donor. Among them, the age of the donor, the presence of macro vesicular steatosis in the graft and length of the cold ischemia time are those who find greater agreement in the literature on the subject 3.
The extension of the cold ischemia time may be needed to allow comfortable displacement of the recipient to the transplant center and its preparation, which includes laboratory tests, and matching of blood products. The improvement of preservation solutions that allow greater CIT represented an important development milestone for liver transplantation. It is discussed, in the present study, the extension of CIT to allow transplantation be performed in the mornings. The advantages of such a tactic would be to profit of the better functioning of hospital resources during the day, plus the best performance of the surgical team after resting overnight. However, no damage to the functioning of the graft can be justified by these benefits.
The decision to adopt the Awakening Protocol involves extracting the organ at night, with vascular clamping in the donor after 10:30p.m. The recipient is installed in the operating room at 05:00a.m. for monitoring and preparation, the procedure starting around 06:00a.m. Some circumstances require the immediate realization of transplantation, as in cases of fulminant hepatitis. In theses cases the use of Awakening Protocol is not indicated. Likewise, some steatotics marginal grafts can only be used in association with a short period of ischemia. Thus, the selection of cases to achieve the Protocol Awakening should not be random, but indicated in compliance with the criteria for inclusion and exclusion.
The comparison of the results of transplants performed in these two different protocols had involved initially, the ascertainment of factors associated with early mortality the recipient in order to avoid selection bias. The main factors identified - female donor, previous surgery on the bile ducts, previous surgery to treat portal hypertension, or hepatectomy and cholecystectomy - were equally distributed between the two groups. There was no difference in survival between patients transplanted sequentially and patients transplanted within the Awakening Protocol, without this having been a selection of the best recipients.
Xu et al. identified long CIT (10.65 ± 02.08 hours, approximately 699 ± 124.8 minutes) and presence of perioperative cardiac events as factors associated with a higher early mortality3. In our study, patients within the Awakening Protocol group had median CIT of 664 minutes, with no difference in survival compared to the others. Other authors, in a retrospective analysis of the OPTN database found lower survival in the association of CIT over 12 hours, with donors older than 45 years4. Moore et al, found a similar association between prolonged CIT and donor age greater than 60 years5.
Late biliary strictures, in patients with hepatic artery stenosis, were more frequent in grafts with prolonged CIT6. Late onset complications were not investigated in this study. So, it is important to note that although prolonged when compared to sequential transplantation, cold ischemia time in the Awakening Protocol was not long enough to complicate the immediate clinical course of transplanted patient.
Conclusion
Delaying the onset of non-urgent liver transplantation for the next morning following the removal of the graft, when vascular clamping occurs after 10:00p.m., does not cause damage to liver early function or patient survival.
Conflict of interest: none
Financial source: none
- 1. Southard JH, Belzer FO. Organ preservation. Annu Rev Med. 1995;46(1):235-47
- 2. Jamieson NV, Sundber G R, Lindell S et al. Successful 24-hour liver preservation: a preliminary report. Proceedings of the International Organ Transplant Forum. Pittsburgh. EUA. 1987;74.
- 3. Xu ZD, Xu HT, Yuan HB, Zhang H, Ji RH, Zou Z, Fu ZR, Shi XY. Postreperfusion syndrome during orthotopic liver transplantation: a single-center experience. Hepatobiliary Pancreat Dis Int. 2012;11:34-9
- 4. Reese PP, Sonawane SB, Thomasson A, Yeh H, Markmann JF. Donor age and cold ischemia interact to produce inferior 90-day liver allograft survival. Transplantation. 2008; 85(12):1737-44.
- 5. Moore DE, Feurer ID, Speroff T, Gorden DL, Wright JK, Chari RS, Pinson CW. Impact of donor, technical, and recipient risk factors on survival and quality of life after liver transplantation. Arch Surg. 2005; 140(3):273-7.
- 6. Dacha S, Barad A, Martin J, Levitsky J. Association of Hepatic Artery Stenosis and Biliary Strictures in Liver Transplant Recipients. Liver Transpl 17:849-854. 2011
Publication Dates
-
Publication in this collection
01 Feb 2013 -
Date of issue
2013