Abstracts
PURPOSE: To compare curative effect of different treatments for hypertensive cerebral hemorrhage of 25 to 35ml. METHODS: In this study, 595 cases were enrolled and grouped regarding treatments including conservative treatment, evacuation with microinvasive craniopuncture technique within 6h and 6-48h after the attack. RESULTS: After follow up for three months after the attack, the assessment based on the Activity of Daily Living (ADL) indicated no significant difference among conservative treatment and surgical interventions (p>0.05). However, surgical interventions showed advantages of shorter hospitalization, quick removal of hematoma and obvious reduction of cost. CONCLUSION: The microinvasive craniopuncture technique to drain the hematoma within 6-48h may be a good way in treating hypertensive hemorrhage of basal ganglia region.
Intracranial Hypertension; Basal Ganglia Hemorrhage; Punctures
OBJETIVO: Comparar o efeito curativo de diferentes tratamentos da hemorragia hipertensiva cerebral de 25 a 35ml. MÉTODOS: Foram analisados 595 casos agrupados segundo tratamento conservador e evacuação com técnica de punção transcraniana dentro de 6h ou de 6 às 48h do início do quadro clínico. RESULTADOS: O seguimento após três meses e avaliado pelo Escore de Atividade de Vida Diário, indicou que não houve diferenças significantes entre os tratamentos conservador e cirúrgico (p>0.05) O tratamento cirúrgico mostrou vantagem com hospitalização mais curta e redução de custos. CONCLUSÃO: A técnica de punção transcraniana para drenagem de hematoma dos núcleos da base pode ser uma boa alternativa de tratamento.
Hipertensão Intracraniana; Hemorragia dos Gânglios da Base; Punções
10 - ORIGINAL ARTICLE
CLINICAL INVESTIGATION
Comparison on different strategies for treatments of hypertensive hemorrhage in the basal ganglia region with a volume of 25 to 35ml1 1 Research performed at Department of Neurosurgery, The Affiliated Hospital of Taishan Medical College, Taishan 271000, China.
Comparação de diferentes estratégias no tratamento da hemorragia hipertensiva da região dos gânglios da base com volume de 25 a 35ml
Wei ZhengI; Chunpu ZhangII; Dapeng HouIII; Chunguang CaoIV
IDoctor degree, Department of Neurosurgery, Affiliated Hospital of Taishan Medical College, China. Study design and manuscript preparation
IIMaster degree, Department of Neurosurgery, Affiliated Hospital of Taishan Medical College, China. Acquisition of data
IIIMaster degree, Intensive Care Unit, Affiliated Hospital of Taishan Medical College, China. Contributed as postoperative treatment
IVMaster degree, Department of Neurosurgery, Affiliated Hospital of Taishan Medical College, China. Contributed to follow up and surgical procedures
Correspondence Correspondence: Dr. Wei Zheng Department of Neurosurgery The Affiliated Hospital of Taishan Medical College Taishan 271000 China david200310@163.com
ABSTRACT
PURPOSE: To compare curative effect of different treatments for hypertensive cerebral hemorrhage of 25 to 35ml.
METHODS: In this study, 595 cases were enrolled and grouped regarding treatments including conservative treatment, evacuation with microinvasive craniopuncture technique within 6h and 6-48h after the attack.
RESULTS: After follow up for three months after the attack, the assessment based on the Activity of Daily Living (ADL) indicated no significant difference among conservative treatment and surgical interventions (p>0.05). However, surgical interventions showed advantages of shorter hospitalization, quick removal of hematoma and obvious reduction of cost.
CONCLUSION: The microinvasive craniopuncture technique to drain the hematoma within 6-48h may be a good way in treating hypertensive hemorrhage of basal ganglia region.
Key words: Intracranial Hypertension. Basal Ganglia Hemorrhage. Punctures.
RESUMO
OBJETIVO: Comparar o efeito curativo de diferentes tratamentos da hemorragia hipertensiva cerebral de 25 a 35ml.
MÉTODOS: Foram analisados 595 casos agrupados segundo tratamento conservador e evacuação com técnica de punção transcraniana dentro de 6h ou de 6 às 48h do início do quadro clínico.
RESULTADOS: O seguimento após três meses e avaliado pelo Escore de Atividade de Vida Diário, indicou que não houve diferenças significantes entre os tratamentos conservador e cirúrgico (p>0.05) O tratamento cirúrgico mostrou vantagem com hospitalização mais curta e redução de custos.
CONCLUSÃO: A técnica de punção transcraniana para drenagem de hematoma dos núcleos da base pode ser uma boa alternativa de tratamento.
Descritores: Hipertensão Intracraniana. Hemorragia dos Gânglios da Base. Punções.
Introduction
Hypertensive cerebral hemorrhage is a common critical disease in the neurosurgerical field and even may threaten patients' life. The large hematoma with the significant mass effect is generally treated with surgery and the small ones with the conservative modality. The risk of basal ganglia hemorrhage increases in patients with hypertension. However, a proportion of patients with BGH have underlying vascular abnormalities, and these patients may require a different treatment approach1. However, it is still inconclusive on the treatment modality and timing for hemorrhage in the critical volume (between 25ml to 35ml) with no definite operative indications. Patients with such hematoma in multiple hospitals were observed for their prognosis, quality of life, hematoma-eliminating time, hospital stays and costs from October 2004 to May 2009 and compared using the random and control method.
Methods
A total of 595 patients with hematoma between 25 to 35ml in volume (380 males and 215 females) were enrolled into this study with an average age of 57 years (range 27 to 75 years). All patients had hypertension histories and were treated with 3 methods: the conservative therapy (n=361), evacuation of the hematoma with the microinvasive craniopunture within 6 (n=89) or 6-48h (n=145) following attack.
Clinical manifestations
All patients experienced a sudden attack, manifesting with hemiplegia, aphasia, nausea, vomiting or slight conscious disturbance but no any brain hernia signs such as mydriasis.
Imaging examinations
CT confirmed the hemorrhage in the basal ganglia region and the supratentorial hematoma volume of 25-35ml (30±5ml) (calculated according to the Coniglobus formula). The hematoma was primarily located in the basal ganglia region but also broke into the ventricle in a few of patients without ventricular enlargement.
Selection of methods
All patients met the above criteria and following patients were excluded from this study: 1) with coagulation disturbance; 2) with long-term administration of anticoagulant agents; 3) in the dying situation which manifested with cerebral hernia and bilateral mydriasis; or 4) with bleeding inducing tumor, trauma, vascular malformation and aneurysm. Patients and their families were informed about advantages and disadvantages regarding conservative therapy and evacuation of the hematoma with the microinvasive craniopuncture within 6 or 6-48h following attack and they made the finial decision. The χ2 test showed no significant differences in general situation, disease condition and hematoma volume among the three groups (p>0.05).
Treatment modalities
1) Conservative therapy: all patients were treated by medication, including dehydration, hemostatis, neurotrophy and hypertensive agents. 2) Evacuation of the hematoma with the microinvasive craniopuncture: first of all, patients' or families' informed consents were provided. Evacuation of the hematoma with the microinvasive craniopuncture was conducted within 6 or 6-48h following attack. Local anesthesia single or in combination with intensified anesthesia was given. The prefrontal approach was adopted for bleeding in the anterior basal ganglia region while the puncture in the most superficial site of the hematoma for bleeding in the posterior part. To prevent injuries of cortical vessels in blind puncturing, the largest surface of the hematoma was selected on the basis of the accurate location. Firstly, around 2cm scalp was cut open; then, a hole was drilled in the cranium with a cranial drill; next, the dura was fulgerized and cut open. The cortex was punctured under direct vision and the puncturing depth was determined by the hematoma volume. The drainage tube was placed just in the middle of the hematoma and 1cm away from the inner wall of the hematoma cavity. During surgery, the blood needed no aspiration but naturally outflowed with cerebral pulsation to reduce the recurrent hemorrhage. Urokinase (10,000 units/5ml, per day) was injected into the hematoma cavity after 24h following attack, retained for 2 to 4h according to patients' tolerance and then opened. Cranial CT was reexamined two to six days later.
Assessment
1) Long-term efficacy: efficacy was analyzed using the Activity of Daily Living (ADL) scale. The prognosis was considered good if the ADL completely or partially recovered or patients could walk with the aid of other person. The prognosis was poor when patients seriously disabled in bed but kept conscious, were in vegetable status or died.
2) Hematoma disappearance: it was defined that the intracerebral hematoma decreased by more than 90%. For patients receiving conservative therapy with no complete hematoma absorption but meeting discharge criteria, the hematoma disappearing time was estimated via the hematoma absorbing speed (ml/day) by calculating the hematoma volume difference according to admission and discharge CT findings.
3) Hospital costs: the average cost was the cost for evacuation of the hematoma with the microinvasive craniopuncture within 6h following attack and the ratio of individual's costs to the average cost was calculated.
4) Discharge criteria: vital signs were stable and blood pressure could be well controlled with oral agents. Patients receiving no surgery showed a hematoma absorption proportion of above 60%-70%, no midline structure displacement and alleviating peripheral edema. For patients with surgery, the hematoma disappeared without significant peripheral edema and cranial knife edge healed well with the stitch removal.
Statistical analysis
SPSS12.0 was used for statistical analysis. Group comparison was conducted using the χ2 test. Measurement data were analyzed with the t test. p<0.05 was considered statistically different.
Results
Long-term efficacy
Patients were followed up for three months following surgery. A good prognosis was observed in 335 of patients with conservative therapy (92.8%), 77 of patients with surgery within 6h following attack (86.5%) and 139 of patients with surgery within 6-24h following attack (95.8%). A significant difference was noted in surgery within 6h following attack as compared to surgery within 6-24h following attack and conservative therapy (p<0.05) (Table 1) but not noted between patients with conservative therapy and those with surgeries (p>0.05) (Table 2).
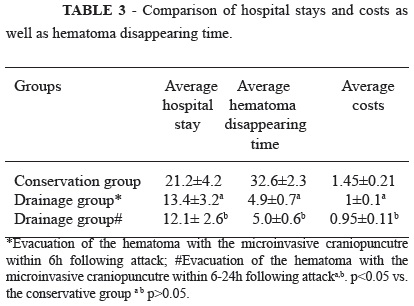
Comparison of hospital stays and costs as well as hematoma disappearing time
Evacuation of the hematoma with the microinvasive craniopuncutre could significantly reduce hospital stays and costs as well as hematoma disappearing time compared to the conservation therapy (p<0.05) (Table 3).
Discussion
Hypertensive cerebral hemorrhage usually occurs in the basal ganglia region, manifesting with the three deflective sign, and generally stops within 20 to 30 minutes1. However, there is still active or recurrent hemorrhage2, of which, most stops within 6h when the coagulation mechanism fully functions and the blood pressure is stable3. The hematoma can directly damage local nerve fibers, leading to the cerebral ischemia and hypoxia. Additionally, metabolites in the blood can produce the toxic effects on adjacent brain tissues, causing edema, degeneration, hemorrhage and necrosis of brain tissues and subsequent elevation of intracranial pressure to worse the cerebral ischemia and hypoxia4. Thus, the vicious circle formed. Surgical therapy aims to remove the hematoma, reduce the intracranial pressure, recover compressed and undamaged neurons and alleviate injuries secondary to hemorrhage. Hemorrhage of the basal ganglia region with the critical volume is associated with slight manifestations and there are conflicting opinions regarding treatment modalities. This study showed that the evacuation of the hematoma with the microinvasive craniopuncture and evacuation was comparable with the conservation therapy in the long-term efficacy but superior to it in the hematoma removal and hospital stays and costs. However, surgery within 6h following attack is associated with risks of hematoma enlargement (7/12) and other complications.
Neurosurgeons often give too much emphasis to the early hematoma removal5. Early ICH evacuation failed to improve the survival rates, as compared with best medical management6. In this study, evacuation of the hematoma with the microinvasive cranipuncture was conducted with the aid of the stereotactic technique or CT guidance, which allows for hematoma removal or minimal damage to brain tissues. The intracranial pressure is not very high and obtains certain buffer capacity in hematoma with the critical volume. Consequently, the hematoma can compress surrounding brain tissues and vessels, especially unstable or easily recurrently bleeding blood vessels, to prevent recurrent hemorrhage, which is proved by the fact that evacuation of the hematoma with the microinvasive craniopuncture within 6h following attack. Patients with spontaneous supratentorial intracerebral haemorrhage in neurosurgical units show no overall benefit from early surgery when compared with initial conservative treatment7.
Within 6 to 48h, patient's blood pressure and emotion are stable, hemorrhage had coagulated, the hematoma is in a relatively stable status, the cerebral edema is not severe, recurrent hemorrhage is less possible and patients are relatively safe. Cerebral hemorrhage is a relatively rapid process. It can immediately induce the displacement of brain tissues and rapid hematoma removal can cause reposition of these brain tissues, both damaging brain tissues. However, the damages can be avoided if the surgery is conducted in 6-48h later. In spite of a long course, absorption of hematoma with drugs is a relatively slow self-repair process, which can not induce additional injuries. Even though position is very accurate and the trauma is minimal, it is inevitable for nerve fibers and nuclei to injury, which may increase the incidence of complications. This side effect offset the benefit of the complete hematoma removal to a certain extent, which can be confirmed by causes why the micropuncture and evacuation cannot improve the long-term efficacy.
We also observed that evacuation of the hematoma with the microinvasive craniopuncture had significant benefits compared to the conservative therapy. In China, patients with hypertensive cerebral hemorrhage are primarily distributed in the rural areas. The surgery procedure is a favorable option for patients with economic difficulty and has the following advantages: 1) It is simple to operate and time-saving (around 40 minutes), especially suitable for primary hospitals. 2) The hematoma should be accurately positioned and for this, the stereotactic technique or CT guidance was used in this study. The drainage tube should be placed at the center of the hematoma to be beneficial for drainage. 3) Urokinase directly acts on the intrinsic fibrionlytic system to catalyze the conversion from plasminogen to plasmin and also can increase the activity of ADP enzyme, inhibit ADP-induced platelet aggregation and prevent thrombosis. Therefore, it shows a fast and good efficacy on the newly-formed thrombus. Additionally, this agent has significant antigenicity and allergic responses are rarely reported in clinical practice. This study proved that injection of urokinase into the hematoma was safe and effective without significant adverse reactions. The dose should not be too low. In this study, 10 units of urokinase were dissolved into 5 ml physical saline to administer once a day. The high dose has not been reported before. 4) It can be well tolerant by old and infirm patients, is convenient for nursing, shortens the disease course and reduces risks of the pulmonary infection, gastrointestinal bleeding and lower-limb deep venous thrombosis. 5) The blood coagulation is not complete within 6h following attack and micropuncture evacuation may cause rapid drop of intracranial pressure to induce recurrent hemorrhage. Therefore, evacuation of the hematoma with the microinvasive craniopuncture is suggested within 6-48h following attack.
Conclusions
The treatment modality for supratentorial hematoma with the critical volume should be determined according to patient's age, nerve functions, bleeding volume and site and concern of the patient and families. Risks of complications such as recurrent hemorrhage can be significantly increased when surgery is conducted within 6h following attack but not within 6-48h following attack. Therefore, the latter is considered the best option for hemorrhage of basal ganglia region with the critical volume.
Conflict of interest: none
Financial source: none
Received: May 25, 2012
Review: July 26, 2012
Accepted: August 27, 202
- 1. Zheng T, Wang S, Barras C, Davis S, Yan B. Vascular imaging adds value in investigation of basal ganglia hemorrhage. J Clin Neurosci. 2012;19(2):277-80.
- 2. Terzi M, Akkaya O, Onar M. Pure sensory stroke due to bilateral basal ganglion hemorrhage: a case report. Turk Neurosurg. 2010;20(3):406-8.
- 3. Wang JP, Chen DP, Li WF. Microinvasive and conservative treatments for hypertensive cerebral hemorrhage. Chin J Clin Neurosurg. 2006;11:629-36.
- 4. Clark JF, Loftspring M, Wurster WL, Beiler S, Beiler C, Wagner KR, Pyne-Geithman GJ. Bilirubin oxidation products, oxidative stress, and intracerebral hemorrhage. Acta Neurochir Suppl. 2008;105:7-12.
- 5. Nehls DG, Mendelow AD, Graham DI, Sinar EJ, Teasdale GM. Experimental introcerebral hemorrhage progression of hemodynamic changes after production of a spontaneous mass lesion. Neurosurgery. 1988;23:439-44.
- 6. Pantazis G, Tsitsopoulos P, Mihas C, Katsiva V, Stavrianos V, Zymaris S. Early surgical treatment vs conservative management for spontaneous supratentorial intracerebral hematomas: A prospective randomized study. Surg Neurol. 2006;66(5):492-501.
- 7. Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, Karimi A, Shaw MD, Barer DH; STICH investigators. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet. 2005;365(9457):387-97
Publication Dates
-
Publication in this collection
27 Sept 2012 -
Date of issue
Oct 2012
History
-
Received
25 May 2012 -
Accepted
27 Aug 2002 -
Reviewed
26 July 2012